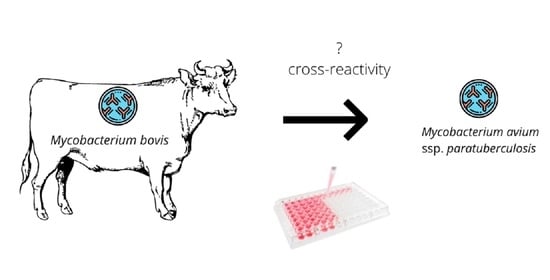
The Risk of False-Positive Serological Results for Paratuberculosis in Mycobacterium bovis-Infected Cattle
Abstract
:1. Introduction
2. Results
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Material
5.2. Serology
5.3. Mycobacterial Isolation
5.4. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Olea-Popelka, F.; Muwonge, A.; Perera, A.; Dean, A.S.; Mumford, E.; Erlacher-Vindel, E.; Forcella, S.; Silk, B.J.; Ditiu, L.; El Idrissi, A.; et al. Zoonotic tuberculosis in human beings caused by Mycobacterium bovis-a call for action. Lancet Infect. Dis. 2017, 17, e21–e25. [Google Scholar] [CrossRef] [Green Version]
- Over, K.; Crandall, P.G.; O’Bryan, C.A.; Ricke, S.C. Current perspectives on Mycobacterium avium subsp. paratuberculosis, Johne’s disease, and Crohn’s disease: A review. Crit. Rev. Microbiol. 2011, 37, 141–156. [Google Scholar] [CrossRef]
- Whittington, R.; Donat, K.; Weber, M.F.; Kelton, D.; Nielsen, S.S.; Eisenberg, S.; Arrigoni, N.; Juste, R.; Sáez, J.L.; Dhand, N.; et al. Control of paratuberculosis: Who, why and how. A review of 48 countries. BMC Vet. Res. 2019, 15, 198. [Google Scholar] [CrossRef] [Green Version]
- Griffa, N.; Moyano, R.D.; Canal, A.M.; Travería, G.E.; Santangelo, M.P.; Alonso, N.; Romano, M.I. Development and diagnostic validation of an ELISA based on an antigenic mixture for the detection of bovine tuberculosis. Vet. J. 2020, 256, 105426. [Google Scholar] [CrossRef]
- Palmer, M.V.; Thacker, T.C.; Rabideau, M.M.; Jones, G.J.; Kanipe, C.; Vordermeier, H.M.; Ray Waters, W. Biomarkers of cell-mediated immunity to bovine tuberculosis. Vet. Immunol. Immunopathol. 2020, 220, 109988. [Google Scholar] [CrossRef]
- Jenkins, A.O.; Gormley, E.; Gcebe, N.; Fosgate, G.T.; Conan, A.; Aagaard, C.; Michel, A.L.; Rutten, V.P.M.G. Cross reactive immune responses in cattle arising from exposure to Mycobacterium bovis and non-tuberculous mycobacteria. Prev. Vet. Med. 2018, 152, 16–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stringer, L.A.; Wilson, P.R.; Heuer, C.; Hunnam, J.C.; Mackintosh, C.G. Effect of vaccination and natural infection with Mycobacterium avium subsp. paratuberculosis on specificity of diagnostic tests for bovine tuberculosis in farmed red deer (Cervus elaphus). N. Z. Vet. J. 2011, 59, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Dunn, J.R.; Kaneene, J.B.; Grooms, D.L.; Bolin, S.R.; Bolin, C.A.; Bruning-Fann, C.S. Effects of positive results for Mycobacterium avium subsp paratuberculosis as determined by microbial culture of feces or antibody ELISA on results of caudal fold tuberculin test and interferon-gamma assay for tuberculosis in cattle. J. Am. Vet. Med. Assoc. 2005, 226, 429–435. [Google Scholar] [CrossRef]
- Gormley, E.; Doyle, M.; Duignan, A.; Good, M.; More, S.J.; Clegg, T.A. Identification of risk factors associated with disclosure of false positive bovine tuberculosis reactors using the gamma-interferon (IFNγ) assay. Vet. Res. 2013, 44, 117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bridges, N.; van Winden, S. The occurrence of Mycobacterium avium subspecies paratuberculosis positive milk antibody ELISA results in dairy cattle under varying time periods after skin testing for bovine tuberculosis. Animals 2021, 11, 1224. [Google Scholar] [CrossRef]
- Gilardoni, L.R.; Paolicchi, F.A.; Mundo, S.L. Bovine paratuberculosis: A review of the advantages and disadvantages of different diagnostic tests. Rev. Argent. Microbiol. 2012, 44, 201–215. [Google Scholar]
- Kennedy, A.E.; O’Mahony, J.; Byrne, N.; MacSharry, J.; Sayers, R.G. Is TB Testing Associated with Increased Blood Interferon-Gamma Levels? Front. Vet. Sci. 2017, 4, 176. [Google Scholar] [CrossRef] [Green Version]
- Byrne, A.W.; Graham, J.; Milne, G.; Guelbenzu-Gonzalo, M.; Strain, S. Is there a relationship between bovine tuberculosis (bTB) herd breakdown risk and Mycobacterium avium subsp. paratuberculosis status? An investigation in bTB chronically and non-chronically infected herds. Front. Vet. Sci. 2019, 6, 30. [Google Scholar] [CrossRef] [Green Version]
- Schiller, I.; Oesch, B.; Vordermeier, H.M.; Palmer, M.V.; Harris, B.N.; Orloski, K.A.; Buddle, B.M.; Thacker, T.C.; Lyashchenko, K.P.; Waters, W.R. Bovine tuberculosis: A review of current and emerging diagnostic techniques in view of their relevance for disease control and eradication. Transbound. Emerg. Dis. 2010, 57, 205–220. [Google Scholar] [CrossRef] [PubMed]
- Mosavari, N.; Geravand, M.M.; Tadayon, K.; Keshavarz, R. Mycobacterial coinfection and persisting bovine tuberculosis-Has the time arrived for a policy review? Int. J. Mycobacteriol. 2016, 5, S82–S83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCallan, L.; Brooks, C.; Couzens, C.; Young, F.; McNair, J.; Byrne, A.W. Assessment of serological tests for diagnosis of bovine tuberculosis. Vet. Rec. 2017, 181, 90. [Google Scholar] [CrossRef] [PubMed]
- Amadori, M.; Tagliabue, S.; Lauzi, S.; Finazzi, G.; Lombardi, G.; Teló, P.; Pacciarini, L.; Bonizzi, L. Diagnosis of Mycobacterium bovis infection in calves sensitized by mycobacteria of the avium/intracellulare group. J. Vet. Med. Ser. B 2002, 49, 89–96. [Google Scholar] [CrossRef]
- Raffo, E.; Steuer, P.; Tomckowiack, C.; Tejeda, C.; Collado, B.; Salgado, M. More insights about the interfering effect of Mycobacterium avium subsp. paratuberculosis (MAP) infection on Mycobacterium bovis (M. bovis) detection in dairy cattle. Trop. Anim. Health Prod. 2020, 52, 1479–1485. [Google Scholar] [CrossRef]
- Waters, W.R.; Nonnecke, B.J.; Palmer, M.V.; Robbe-Austermann, S.; Bannantine, J.P.; Stabel, J.R.; Whipple, D.L.; Payeur, J.B.; Estes, D.M.; Pitzer, J.E.; et al. Use of recombinant ESAT-6: CFP-10 fusion protein for differentiation of infections of cattle by Mycobacterium bovis and by M. avium subsp. avium and M. avium subsp. paratuberculosis. Clin. Diagn. Lab. Immunol. 2004, 11, 729–735. [Google Scholar] [CrossRef] [Green Version]
- Lyashchenko, K.P.; Grandison, A.; Keskinen, K.; Sikar-Gang, A.; Lambotte, P.; Esfandiari, J.; Ireton, G.C.; Vallur, A.; Reed, S.G.; Jones, G.; et al. Identification of novel antigens recognized by serum antibodies in bovine tuberculosis. Clin. Vaccine Immunol. 2017, 24, e00259-17. [Google Scholar] [CrossRef] [Green Version]
- Lyashchenko, K.P.; Sridhara, A.A.; Johnathan-Lee, A.; Sikar-Gang, A.; Lambotte, P.; Esfandiari, J.; Bernitz, N.; Kerr, T.J.; Miller, M.A.; Waters, W.R. Differential antigen recognition by serum antibodies from three bovid hosts of Mycobacterium bovis infection. Comp. Immunol. Microbiol. Infect. Dis. 2020, 69, 101424. [Google Scholar] [CrossRef] [PubMed]
- Marassi, C.D.; McNair, J.; Pollock, J.; Ristow, P.; Fonseca, L.S.; Oelemann, W.M.; Lilenbaum, W. The use of MPB70 and MPB83 to distinguish between bovine tuberculosis and paratuberculosis. Comp. Immunol. Microbiol. Infect. Dis. 2010, 33, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Bannantine, J.P.; Campo, J.J.; Li, L.; Randall, A.; Pablo, J.; Praul, C.A.; Raygoza Garay, J.A.; Stabel, J.R.; Kapur, V. Identification of novel seroreactive antigens in Johne’s disease cattle by using the Mycobacterium tuberculosis Protein Array. Clin. Vaccine Immunol. 2017, 24, e00081-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Picasso-Risso, C.; Grau, A.; Bakker, D.; Nacar, J.; Mínguez, O.; Perez, A.; Alvarez, J. Association between results of diagnostic tests for bovine tuberculosis and Johne’s disease in cattle. Vet. Rec. 2019, 185, 693. [Google Scholar] [CrossRef] [PubMed]
- Szteyn, J.; Wiszniewska-Łaszczych, A. Seroprevalence of Mycobacterium avium subsp. paratuberculosis infection in dairy herds in Zuławy, Poland. Berl. Munch. Tierarztl. Wochenschr. 2012, 125, 397–400. [Google Scholar] [PubMed]
- Casal, C.; Infantes, J.A.; Risalde, M.A.; Díez-Guerrier, A.; Domínguez, M.; Moreno, I.; Romero, B.; de Juan, L.; Sáez, J.L.; Juste, R.; et al. Antibody detection tests improve the sensitivity of tuberculosis diagnosis in cattle. Res. Vet. Sci. 2017, 112, 214–221. [Google Scholar] [CrossRef]
- McCallan, L.; Brooks, C.; Barry, C.; Couzens, C.; Young, F.J.; McNair, J.; Byrne, A.W. Serological test performance for bovine tuberculosis in cattle from herds with evidence of on-going infection in Northern Ireland. PLoS ONE 2021, 16, e0245655. [Google Scholar] [CrossRef] [PubMed]
- Waters, W.R.; Palmer, M.V.; Stafne, M.R.; Bass, K.E.; Maggioli, M.F.; Thacker, T.C.; Linscott, R.; Lawrence, J.C.; Nelson, J.T.; Esfandiari, J.; et al. Effects of serial skin testing with purified protein derivative on the level and quality of antibodies to complex and defined antigens in Mycobacterium bovis-infected cattle. Clin. Vaccine Immunol. 2015, 22, 641–649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de la Rua-Domenech, R.; Goodchild, A.T.; Vordermeier, H.M.; Hewinson, R.G.; Christiansen, K.H.; Clifton-Hadley, R.S. Ante mortem diagnosis of tuberculosis in cattle: A review of the tuberculin tests, gamma-interferon assay and other ancillary diagnostic techniques. Res. Vet. Sci. 2006, 81, 190–210. [Google Scholar] [CrossRef]
- Kawaji, S.; Nagata, R.; Minegishi, Y.; Saruyama, Y.; Mita, A.; Kishizuka, S.; Saito, M.; Mori, Y. A Novel Real-Time PCR-Based screening test with pooled fecal samples for bovine Johne’s Disease. J. Clin. Microbiol. 2020, 58, e01761-20. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.S.; Toft, N. Ante mortem diagnosis of paratuberculosis: A review of accuracies of ELISA, interferon-gamma assay and faecal culture techniques. Vet. Microbiol. 2008, 129, 217–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weber, M.F.; Verhoeff, J.; van Schaik, G.; van Maanen, C. Evaluation of Ziehl-Neelsen stained faecal smear and ELISA as tools for surveillance of clinical paratuberculosis in cattle in the Netherlands. Prev. Vet. Med. 2009, 92, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Schwalm, A.K.; Metzger-Boddien, C.; Seemann, G.; Mandl, J.; Obiegala, A.; Pfeffer, M.; Sting, R. Field study on bovine paratuberculosis using real-time PCR and liquid culture for testing environmental and individual fecal samples implemented in dairy cow management. J. Dairy Sci. 2019, 102, 11260–11267. [Google Scholar] [CrossRef]
- Verdugo, C.; Cardemil, C.; Steuer, P.; Salgado, M. Bayesian latent class estimation of sensitivity and specificity parameters of the PMS-PCR test for the diagnosis of cattle sub-clinically infected with Mycobacterium avium subsp. paratuberculosis. Prev. Vet. Med. 2020, 182, 105076. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, I.; Kudi, C.A.; Abdulkadir, A.I.; Saidu, S.N.A. Occurrence and distribution of bovine TB pathology by age, sex, and breed of cattle slaughtered in Gusau Abattoir, Zamfara State Nigeria. Trop. Anim. Health Prod. 2017, 49, 583–589. [Google Scholar] [CrossRef]
- Vordermeier, M.; Ameni, G.; Berg, S.; Bishop, R.; Robertson, B.D.; Aseffa, A.; Hewinson, R.G.; Young, D.B. The influence of cattle breed on susceptibility to bovine tuberculosis in Ethiopia. Comp. Immunol. Microbiol. Infect. Dis. 2012, 35, 227–232. [Google Scholar] [CrossRef] [Green Version]
- Taylor, M.J.; Hughes, M.S.; Skuce, R.A.; Neill, S.D. Detection of Mycobacterium bovis in bovine clinical specimens using real-time fluorescence and fluorescence resonance energy transfer probe rapid-cycle PCR. J. Clin. Microbiol. 2001, 39, 1272–1278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norby, B.; Bartlett, P.C.; Fitzgerald, S.D.; Granger, L.M.; Bruning-Fann, C.S.; Whipple, D.L.; Payeur, J.B. The sensitivity of gross necropsy, caudal fold and comparative cervical tests for the diagnosis of bovine tuberculosis. J. Vet. Diagn. Investig. 2004, 16, 126–131. [Google Scholar] [CrossRef] [Green Version]
- Casal, C.; Díez-Guerrier, A.; Álvarez, J.; Rodriguez-Campos, S.; Mateos, A.; Linscott, R.; Martel, E.; Lawrence, J.C.; Whelan, C.; Clarke, J.; et al. Strategic use of serology for the diagnosis of bovine tuberculosis after intradermal skin testing. Vet. Microbiol. 2014, 170, 342–351. [Google Scholar] [CrossRef]
- Soares Filho, P.M.; Ramalho, A.K.; de Moura Silva, A.; Hodon, M.A.; de Azevedo Issa, M.; Fonseca Júnior, A.A.; Mota, P.M.P.C.; Silva, C.H.O.; Dos Reis, J.K.P.; Leite, R.C. Evaluation of post-mortem diagnostic tests’ sensitivity and specificity for bovine tuberculosis using Bayesian latent class analysis. Res. Vet. Sci. 2019, 125, 14–23. [Google Scholar] [CrossRef]
- Koni, A.; Juma, A.; Morini, M.; Nardelli, S.; Connor, R.; Koleci, X. Assessment of an ELISA method to support surveillance of bovine tuberculosis in Albania. Ir. Vet. J. 2016, 69, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cecchini, G.; Bekele, T.; Kasali, O.B. The effect of repeated freezing and thawing of serum on the activity of antibodies. Vet. Res. Commun. 1992, 16, 425–428. [Google Scholar] [CrossRef]
- Available online: www.ostrowmaz.piwet.net/instrukcje/instrukcja_gruzlica.pdf (accessed on 19 August 2021).
- Krajewska-Wędzina, M.; Didkowska, A.; Sridhara, A.A.; Elahi, R.; Johnathan-Lee, A.; Radulski, Ł.; Lipiec, M.; Anusz, K.; Lyashchenko, K.P.; Miller, M.A.; et al. Transboundary tuberculosis: Importation of alpacas infected with Mycobacterium bovis from the United Kingdom to Poland and potential for serodiagnostic assays in detecting tuberculin skin test false-negative animals. Transbound. Emerg. Dis. 2020, 67, 1306–1314. [Google Scholar] [CrossRef] [PubMed]
- Nuñez-Garcia, J.; Downs, S.H.; Parry, J.E.; Abernethy, D.A.; Broughan, J.M.; Cameron, A.R.; Cook, A.J.; de la Rua-Domenech, R.; Goodchild, A.V.; Gunn, J.; et al. Meta-analyses of the sensitivity and specificity of ante-mortem and post-mortem diagnostic tests for bovine tuberculosis in the UK and Ireland. Prev. Vet. Med. 2018, 153, 94–107. [Google Scholar] [CrossRef] [PubMed]

| Reference Method | Compared Methods | |||||||
|---|---|---|---|---|---|---|---|---|
| Tuberculin Skin Test | TB-ELISA | ParaTB-ELISA | Gross Lesions | |||||
| MTBC isolation | − | + | − | + | − | + | − | + |
| − | 0 | 15 | 14 | 1 | 12 | 3 | 15 | 0 |
| + | 0 | 83 | 63 | 20 | 52 | 31 | 27 | 56 |
| Reference Method | ParaTB-ELISA | Logistic Regression Results | |
|---|---|---|---|
| TB-ELISA | − | + | Bvar = 2.03, (SE = 0.55), Wald χ2 = 13.622, p < 0.001, OR = 7.63 B0 = −2.27, (SE = 0.43), Wald χ2 = 27.986, p < 0.001, OR = 0.1 |
| − | 58 | 19 | |
| + | 6 | 15 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Didkowska, A.; Krajewska-Wędzina, M.; Klich, D.; Prolejko, K.; Orłowska, B.; Anusz, K. The Risk of False-Positive Serological Results for Paratuberculosis in Mycobacterium bovis-Infected Cattle. Pathogens 2021, 10, 1054. https://doi.org/10.3390/pathogens10081054
Didkowska A, Krajewska-Wędzina M, Klich D, Prolejko K, Orłowska B, Anusz K. The Risk of False-Positive Serological Results for Paratuberculosis in Mycobacterium bovis-Infected Cattle. Pathogens. 2021; 10(8):1054. https://doi.org/10.3390/pathogens10081054
Chicago/Turabian StyleDidkowska, Anna, Monika Krajewska-Wędzina, Daniel Klich, Kinga Prolejko, Blanka Orłowska, and Krzysztof Anusz. 2021. "The Risk of False-Positive Serological Results for Paratuberculosis in Mycobacterium bovis-Infected Cattle" Pathogens 10, no. 8: 1054. https://doi.org/10.3390/pathogens10081054