Multiparametric MRI in Era of Artificial Intelligence for Bladder Cancer Therapies
Abstract
:Simple Summary
Abstract
1. Introduction
2. Multiparametric (mp)MRI and VI-RADS Score in Bladder Cancer
2.1. Qualitative mpMRI
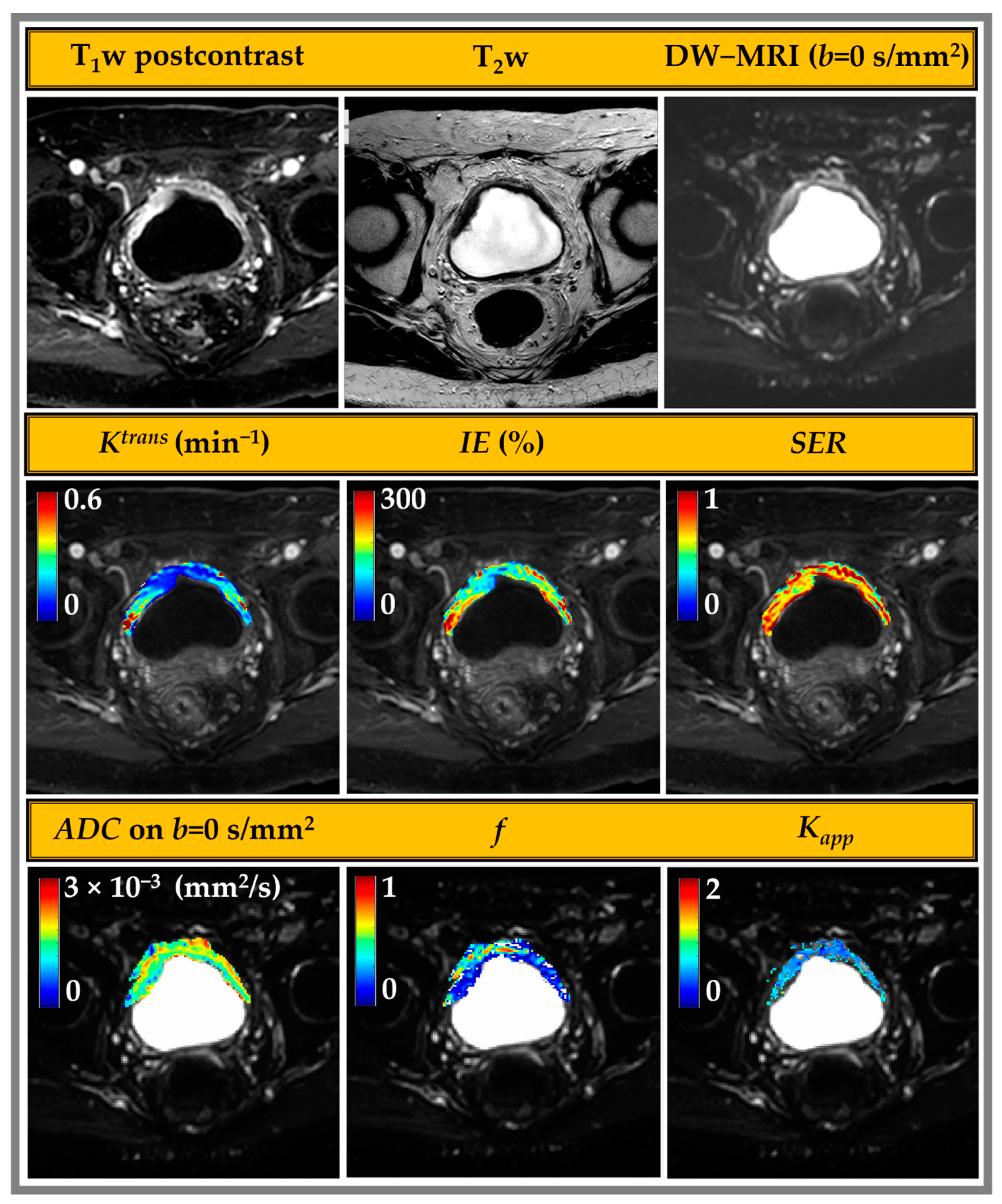
2.2. Quantitative (q)MRI
2.2.1. DW-MRI
| Parameter | T2w | DW | DCE |
|---|---|---|---|
| Field strength | 1.5 T/3 T | 1.5 T/3 T | 1.5 T/3 T |
| Sequence * | FSE | SS-EPI | FSPGR |
| Plane orientation | Multiplanar | Axial | Axial |
| FOV (mm) | 220–250 | 250–300 | 250–300 |
| TR (ms) | 4000–5000 | 4500–6000 | 3.5–4.5 |
| TE (ms) | 80–120 | 60–80 (minimum) | 1.2–2.2 |
| Acquisition matrix | 256 × 192–256 | 128 × 128 | 256 × 192–214 |
| Slice thickness/gap (mm) | 3–4/0 | 3–4/0 | 3–4/0 |
| Number of excitations | 1–2 | 4–12 + | 1 |
| Flip angles (FAs) (degree) | 90 | 90 | 15 |
| b-values (s/mm2) | NA | 0 and 800–1000, up to 2000 optional | NA |
2.2.2. DCE-MRI
2.2.3. Radiomics
3. mpMRI for Clinical Consideration
3.1. mpMRI for Staging, Characterization, and Prognosis in MIBC
3.2. mpMRI for Prediction of Treatment Response in MIBC
3.3. Artificial Intelligence in Bladder Cancer
| # | Application | Reference | Dataset | Methods | Conclusion |
|---|---|---|---|---|---|
| 1 | Segmentation | Dolz et al. (2018) [123] | 60 patients (training 40, validation 5, test 15) | U-Net yields precise segmentation of bladder walls and tumors on T2w. | Higher accuracy than standard CNN, especially for tumors. |
| 2 | Li et al. (2020) [122] | 1092 MR images | U-Net with priors is applied to segment bladder walls and tumors on T2w. | The method improved the accuracy of bladder wall segmentation. | |
| 3 | Yu et al. (2022) [126] | 245 patients (training 220, test 25) | Path augmentation U-Net segmentation for bladder walls and tumors on T2w. | It can precisely extract bladder structures, especially small tumors. | |
| 4 | Coroamă et al. (2023) [127] | 33 patients | A low-complexity 3D U-Net with less than five layers for segmentation of bladder walls and tumors on T2w. | System for automated diagnosis of bladder tumors that can lead to higher reporting accuracy. | |
| 5 | Moribata et al. (2023) [128] | 170 patients (training 140, test 30) | U-Net could segment bladder cancer, and robust high-order radiomics features were extracted from ADC maps. | The model performed accurate segmentation of bladder cancer, and the extracted radiomics exhibited high reproducibility. | |
| 6 | Classification | Zou et al. (2022) [130] | 468 patients | Inception V3, CNN on T2w, recognizes the position of bladder walls and tumors. | Reliable method that can be more focused on features from the surrounding area of the tumor. |
| 7 | Sevcenco et al. (2018) [131] | 51 patients (training 36, test 15) | A multilayer perceptron with one hidden layer on ADC maps. | Classifier model combining the ADC values with clinical–pathological information can identify patients at high risk for survival. | |
| 8 | Li et al. (2023) [133] | Multicenter cohort of 89 (121) patients (tumors), 61 (93) from center 1, and 28 (28) from center 2. Tumors for training 93, test 28 | 3D ResNet50 CNN on T2w as a multitask model exhibits good diagnostic performance in predicting MIBC. | The method was lesion-focused and more reliable for clinical decisions. | |
| 9 | Denoising | Taguchi et al. (2021) [124] | 68 patients | VI-RADS validation CNN, with denoising reconstruction on T2w, discriminates between NMIBC and MIBC. | Combining VI-RADS with denoising CNN might improve diagnostic accuracy. |
| 10 | Watanabe et al. (2022) [125] | 163 patients | VI-RADS validation CNN with denoising reconstruction on T2w and DW- predicts accurate MIBC without using DCE-MRI. | It achieved a comparable predictive accuracy for MIBC to that of conventional VI-RADS. |
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer statistics, 2023. CA A Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef] [PubMed]
- Shadab, R.; Nerli, R.B.; Bidi, S.R.; Ghagane, S.C. Risk Factors for Bladder Cancer: Results of a Survey of Hospital Patients. J. Cancer Allied Spec. 2023, 9, 485. [Google Scholar] [CrossRef] [PubMed]
- Saginala, K.; Barsouk, A.; Aluru, J.S.; Rawla, P.; Padala, S.A.; Barsouk, A. Epidemiology of Bladder Cancer. Med. Sci. 2020, 8, 15. [Google Scholar] [CrossRef] [PubMed]
- Hassan, O.; Murati Amador, B.; Lombardo, K.A.; Salles, D.; Cuello, F.; Marwaha, A.S.; Daniels, M.J.; Kates, M.; Bivalacqua, T.J.; Matoso, A. Clinical significance of urothelial carcinoma ambiguous for muscularis propria invasion on initial transurethral resection of bladder tumor. World J. Urol. 2020, 38, 389–395. [Google Scholar] [CrossRef]
- Robertson, A.G.; Kim, J.; Al-Ahmadie, H.; Bellmunt, J.; Guo, G.; Cherniack, A.D.; Hinoue, T.; Laird, P.W.; Hoadley, K.A.; Akbani, R. Comprehensive molecular characterization of muscle-invasive bladder cancer. Cell 2017, 171, 540–556.e525. [Google Scholar] [CrossRef]
- Pansadoro, V.; Emiliozzi, P. Bladder-sparing therapy for muscle-infiltrating bladder cancer. Nat. Clin. Pract. Urol. 2008, 5, 368–375. [Google Scholar] [CrossRef]
- Tholomier, C.; Souhami, L.; Kassouf, W. Bladder-sparing protocols in the treatment of muscle-invasive bladder cancer. Transl. Androl. Urol. 2020, 9, 2920–2937. [Google Scholar] [CrossRef]
- Tanaka, H.; Kijima, T.; Fujii, Y. Bladder preservation therapy in muscle-invasive bladder cancer: Current evidence and future perspectives. AME Med. J. 2020, 5, 16. [Google Scholar] [CrossRef]
- Babjuk, M.; Burger, M.; Zigeuner, R.; Shariat, S.F.; Van Rhijn, B.W.; Compérat, E.; Sylvester, R.J.; Kaasinen, E.; Böhle, A.; Redorta, J.P. EAU guidelines on non–muscle-invasive urothelial carcinoma of the bladder: Update 2013. Eur. Urol. 2013, 64, 639–653. [Google Scholar] [CrossRef]
- Necchi, A.; Anichini, A.; Raggi, D.; Briganti, A.; Massa, S.; Lucianò, R.; Colecchia, M.; Giannatempo, P.; Mortarini, R.; Bianchi, M. Pembrolizumab as neoadjuvant therapy before radical cystectomy in patients with muscle-invasive urothelial bladder carcinoma (PURE-01): An open-label, single-arm, phase II study. J. Clin. Oncol. 2018, 36, 3353–3360. [Google Scholar] [CrossRef]
- Lattanzi, M.; Rosenberg, J.E. The emerging role of antibody-drug conjugates in urothelial carcinoma. Expert Rev. Anticancer Ther. 2020, 20, 551–561. [Google Scholar] [CrossRef] [PubMed]
- Powles, T.; Rosenberg, J.E.; Sonpavde, G.P.; Loriot, Y.; Durán, I.; Lee, J.L.; Matsubara, N.; Vulsteke, C.; Castellano, D.; Wu, C.; et al. Enfortumab Vedotin in Previously Treated Advanced Urothelial Carcinoma. N. Engl. J. Med. 2021, 384, 1125–1135. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, J.; Milowsky, M.; Ramamurthy, C.; Mar, N.; McKay, R.; Friedlander, T.; Ferrario, C.; Bracarda, S.; George, S.; Moon, H. LBA73 Study EV-103 Cohort K: Antitumor activity of enfortumab vedotin (EV) monotherapy or in combination with pembrolizumab (P) in previously untreated cisplatin-ineligible patients (pts) with locally advanced or metastatic urothelial cancer (la/mUC). Ann. Oncol. 2022, 33, S1441. [Google Scholar] [CrossRef]
- Juri, H.; Narumi, Y.; Panebianco, V.; Osuga, K. Staging of bladder cancer with multiparametric MRI. Br. J. Radiol. 2020, 93, 20200116. [Google Scholar] [CrossRef]
- Hiorns, M.P. Imaging of the urinary tract: The role of CT and MRI. Pediatr. Nephrol. 2011, 26, 59–68. [Google Scholar] [CrossRef]
- Ghafoori, M.; Shakiba, M.; Ghiasi, A.; Asvadi, N.; Hosseini, K.; Alavi, M. Value of MRI in local staging of bladder cancer. Urol. J. 2013, 10, 866–872. [Google Scholar]
- de Haas, R.J.; Steyvers, M.J.; Fütterer, J.J. Multiparametric MRI of the bladder: Ready for clinical routine? AJR Am. J. Roentgenol. 2014, 202, 1187–1195. [Google Scholar] [CrossRef]
- Li, Q.; Cao, B.; Tan, Q.; Liu, K.; Jiang, S.; Zhou, J. Prediction of muscle invasion of bladder cancer: A comparison between DKI and conventional DWI. Eur. J. Radiol. 2021, 136, 109522. [Google Scholar] [CrossRef]
- Donaldson, S.B.; Bonington, S.C.; Kershaw, L.E.; Cowan, R.; Lyons, J.; Elliott, T.; Carrington, B.M. Dynamic contrast-enhanced MRI in patients with muscle-invasive transitional cell carcinoma of the bladder can distinguish between residual tumour and post-chemotherapy effect. Eur. J. Radiol. 2013, 82, 2161–2168. [Google Scholar] [CrossRef]
- Panebianco, V.; Barchetti, F.; de Haas, R.J.; Pearson, R.A.; Kennish, S.J.; Giannarini, G.; Catto, J.W.F. Improving Staging in Bladder Cancer: The Increasing Role of Multiparametric Magnetic Resonance Imaging. Eur. Urol. Focus 2016, 2, 113–121. [Google Scholar] [CrossRef]
- Panebianco, V.; Narumi, Y.; Altun, E.; Bochner, B.H.; Efstathiou, J.A.; Hafeez, S.; Huddart, R.; Kennish, S.; Lerner, S.; Montironi, R.; et al. Multiparametric Magnetic Resonance Imaging for Bladder Cancer: Development of VI-RADS (Vesical Imaging-Reporting And Data System). Eur. Urol. 2018, 74, 294–306. [Google Scholar] [CrossRef]
- Panebianco, V.; Narumi, Y.; Barchetti, G.; Montironi, R.; Catto, J.W.F. Should We Perform Multiparametric Magnetic Resonance Imaging of the Bladder Before Transurethral Resection of Bladder? Time to Reconsider the Rules. Eur. Urol. 2019, 76, 57–58. [Google Scholar] [CrossRef] [PubMed]
- Panebianco, V.; Pecoraro, M.; Del Giudice, F.; Takeuchi, M.; Muglia, V.F.; Messina, E.; Cipollari, S.; Giannarini, G.; Catalano, C.; Narumi, Y. VI-RADS for Bladder Cancer: Current Applications and Future Developments. J. Magn. Reason. Imaging 2022, 55, 23–36. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.T.; Pohar, K.S.; Jia, G.; Shah, Z.K.; Mortazavi, A.; Zynger, D.L.; Wei, L.; Clark, D.; Yang, X.; Knopp, M.V. Improving bladder cancer imaging using 3-T functional dynamic contrast-enhanced magnetic resonance imaging. Investig. Radiol. 2014, 49, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.T.; Mortazavi, A.; Pohar, K.S.; Zynger, D.L.; Wei, L.; Shah, Z.K.; Jia, G.; Knopp, M.V. Quantitative Assessment of Heterogeneity in Bladder Tumor MRI Diffusivity: Can Response be Predicted Prior to Neoadjuvant Chemotherapy? Bladder Cancer 2017, 3, 237–244. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, Y.; Zhang, J.; Zhang, L.; Wang, S.; Chen, Y. Development of a MRI-Based Radiomics Nomogram for Prediction of Response of Patients With Muscle-Invasive Bladder Cancer to Neoadjuvant Chemotherapy. Front. Oncol. 2022, 12, 878499. [Google Scholar] [CrossRef]
- Yamada, Y.; Kobayashi, S.; Isoshima, S.; Arima, K.; Sakuma, H.; Sugimura, Y. The usefulness of diffusion-weighted magnetic resonance imaging in bladder cancer staging and functional analysis. J. Cancer Res. Ther. 2014, 10, 878–882. [Google Scholar] [CrossRef]
- Wang, F.; Jin, D.; Hua, X.L.; Zhao, Z.Z.; Wu, L.M.; Chen, W.B.; Wu, G.Y.; Chen, X.X.; Chen, H.G. Investigation of diffusion kurtosis imaging for discriminating tumors from inflammatory lesions after treatment for bladder cancer. J. Magn. Reason. Imaging 2018, 48, 259–265. [Google Scholar] [CrossRef]
- Li, Q.; Cao, B.; Liu, K.; Sun, H.; Ding, Y.; Yan, C.; Wu, P.Y.; Dai, C.; Rao, S.; Zeng, M.; et al. Detecting the muscle invasiveness of bladder cancer: An application of diffusion kurtosis imaging and tumor contact length. Eur. J. Radiol. 2022, 151, 110329. [Google Scholar] [CrossRef]
- Yoshida, S.; Koga, F.; Kobayashi, S.; Ishii, C.; Tanaka, H.; Tanaka, H.; Komai, Y.; Saito, K.; Masuda, H.; Fujii, Y.; et al. Role of diffusion-weighted magnetic resonance imaging in predicting sensitivity to chemoradiotherapy in muscle-invasive bladder cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, e21–e27. [Google Scholar] [CrossRef]
- Hinsenveld, F.J.; Noordman, B.J.; Boormans, J.L.; Voortman, J.; van Leenders, G.J.L.H.; van der Pas, S.L.; van Beek, S.C.; Oprea-Lager, D.E.; Vis, A.N. Prediction of pathological response following neoadjuvant chemotherapy in patients with muscle-invasive bladder cancer: The PRE-PREVENCYS trial. BMC Cancer 2021, 21, 1161. [Google Scholar] [CrossRef] [PubMed]
- Hafeez, S.; Koh, M.; Jones, K.; El Ghzal, A.; D’Arcy, J.; Kumar, P.; Khoo, V.; Lalondrelle, S.; McDonald, F.; Thompson, A.; et al. Assessing Bladder Radiotherapy Response With Quantitative Diffusion-Weighted Magnetic Resonance Imaging Analysis. Clin. Oncol. 2022, 34, 630–641. [Google Scholar] [CrossRef]
- Naish, J.H.; McGrath, D.M.; Bains, L.J.; Passera, K.; Roberts, C.; Watson, Y.; Cheung, S.; Taylor, M.B.; Logue, J.P.; Buckley, D.L.; et al. Comparison of dynamic contrast-enhanced MRI and dynamic contrast-enhanced CT biomarkers in bladder cancer. Magn. Reson. Med. 2011, 66, 219–226. [Google Scholar] [CrossRef]
- Nguyen, H.T.; Jia, G.; Shah, Z.K.; Pohar, K.; Mortazavi, A.; Zynger, D.L.; Wei, L.; Yang, X.; Clark, D.; Knopp, M.V. Prediction of chemotherapeutic response in bladder cancer using K-means clustering of dynamic contrast-enhanced (DCE)-MRI pharmacokinetic parameters. J. Magn. Reson. Imaging 2015, 41, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Yuan, B.; Zhang, Y.; Zhuang, J.; Cai, L.; Wu, Q.; Cao, Q.; Li, P.; Lu, Q.; Sun, X. Quantitative multiparametric MRI as a promising tool for the assessment of early response to neoadjuvant chemotherapy in bladder cancer. Eur. J. Radiol. 2022, 157, 110587. [Google Scholar] [CrossRef]
- Park, J.J.; Park, B.K. The utility of CT and MRI in detecting male urethral recurrence after radical cystectomy. Abdom. Radiol. 2017, 42, 2521–2526. [Google Scholar] [CrossRef] [PubMed]
- Limkin, E.J.; Sun, R.; Dercle, L.; Zacharaki, E.I.; Robert, C.; Reuzé, S.; Schernberg, A.; Paragios, N.; Deutsch, E.; Ferté, C. Promises and challenges for the implementation of computational medical imaging (radiomics) in oncology. Ann. Oncol. 2017, 28, 1191–1206. [Google Scholar] [CrossRef] [PubMed]
- Parekh, V.; Jacobs, M.A. Radiomics: A new application from established techniques. Expert Rev. Precis Med. Drug Dev. 2016, 1, 207–226. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Song, M.; Zhao, Y.; Xu, S.; Sun, Q.; Zhai, G.; Liang, D.; Wu, G.; Li, Z.C. Radiomics nomogram for preoperative prediction of progression-free survival using diffusion-weighted imaging in patients with muscle-invasive bladder cancer. Eur. J. Radiol. 2020, 131, 109219. [Google Scholar] [CrossRef]
- Liu, S.; Chen, H.; Zheng, Z.; He, Y.; Yao, X. Development of a Molecular-Subtype-Associated Immune Prognostic Signature That Can Be Recognized by MRI Radiomics Features in Bladder Cancer. Bioengineering 2023, 10, 318. [Google Scholar] [CrossRef] [PubMed]
- Bera, K.; Braman, N.; Gupta, A.; Velcheti, V.; Madabhushi, A. Predicting cancer outcomes with radiomics and artificial intelligence in radiology. Nat. Rev. Clin. Oncol. 2022, 19, 132–146. [Google Scholar] [CrossRef]
- Caglic, I.; Panebianco, V.; Vargas, H.A.; Bura, V.; Woo, S.; Pecoraro, M.; Cipollari, S.; Sala, E.; Barrett, T. MRI of Bladder Cancer: Local and Nodal Staging. J. Magn. Reson. Imaging 2020, 52, 649–667. [Google Scholar] [CrossRef]
- Makboul, M.; Farghaly, S.; Abdelkawi, I.F. Multiparametric MRI in differentiation between muscle invasive and non-muscle invasive urinary bladder cancer with vesical imaging reporting and data system (VI-RADS) application. Br. J. Radiol. 2019, 92, 20190401. [Google Scholar] [CrossRef]
- Badawy, M.; Farg, H.; Gadelhak, B.; ElGhar, M.A.; Sadeq, A.G.; Borg, M. Diagnostic performance of 3-tesla multiparametric MRI for assessment of the bladder cancer T stage and histologic grade. Egypt. J. Radiol. Nucl. Med. 2020, 51, 225. [Google Scholar] [CrossRef]
- Woo, S.; Panebianco, V.; Narumi, Y.; Del Giudice, F.; Muglia, V.F.; Takeuchi, M.; Ghafoor, S.; Bochner, B.H.; Goh, A.C.; Hricak, H.; et al. Diagnostic Performance of Vesical Imaging Reporting and Data System for the Prediction of Muscle-invasive Bladder Cancer: A Systematic Review and Meta-analysis. Eur. Urol. Oncol. 2020, 3, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Das, J.P.; Woo, S.; Ghafoor, S.; Andrieu, P.I.C.; Ulaner, G.A.; Donahue, T.F.; Goh, A.C.; Vargas, H.A. Value of MRI in evaluating urachal carcinoma: A single center retrospective study. Urol. Oncol. 2022, 40, 345.e9–345.e17. [Google Scholar] [CrossRef]
- Yoshida, S.; Koga, F.; Masuda, H.; Fujii, Y.; Kihara, K. Role of diffusion-weighted magnetic resonance imaging as an imaging biomarker of urothelial carcinoma. Int. J. Urol. 2014, 21, 1190–1200. [Google Scholar] [CrossRef] [PubMed]
- Séguier, D.; Puech, P.; Kool, R.; Dernis, L.; Gabert, H.; Kassouf, W.; Villers, A.; Marcq, G. Multiparametric magnetic resonance imaging for bladder cancer: A comprehensive systematic review of the Vesical Imaging-Reporting and Data System (VI-RADS) performance and potential clinical applications. Ther. Adv. Urol. 2021, 13, 17562872211039583. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, M.; Sasaki, S.; Naiki, T.; Kawai, N.; Kohri, K.; Hara, M.; Shibamoto, Y. MR imaging of urinary bladder cancer for T-staging: A review and a pictorial essay of diffusion-weighted imaging. J. Magn. Reson. Imaging 2013, 38, 1299–1309. [Google Scholar] [CrossRef]
- Sim, K.C.; Sung, D.J. Role of magnetic resonance imaging in tumor staging and follow-up for bladder cancer. Transl. Androl. Urol. 2020, 9, 2890–2907. [Google Scholar] [CrossRef]
- Panebianco, V.; Del Giudice, F.; Leonardo, C.; Sciarra, A.; Catalano, C.; Catto, J.W.F. VI-RADS Scoring Criteria for Alternative Risk-adapted Strategies in the Management of Bladder Cancer During the COVID-19 Pandemic. Eur. Urol. 2020, 78, e18–e20. [Google Scholar] [CrossRef]
- Luo, C.; Huang, B.; Wu, Y.; Chen, J.; Chen, L. Use of Vesical Imaging-Reporting and Data System (VI-RADS) for detecting the muscle invasion of bladder cancer: A diagnostic meta-analysis. Eur. Radiol. 2020, 30, 4606–4614. [Google Scholar] [CrossRef] [PubMed]
- Arita, Y.; Yoshida, S.; Shigeta, K.; Kwee, T.C.; Edo, H.; Okawara, N.; Hashimoto, M.; Ishii, R.; Ueda, R.; Mikami, S.; et al. Diagnostic Value of the Vesical Imaging-Reporting and Data System in Bladder Urothelial Carcinoma with Variant Histology. Eur. Urol. Oncol. 2023, 6, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Malyarenko, D.I.; Swanson, S.D.; Konar, A.S.; LoCastro, E.; Paudyal, R.; Liu, M.Z.; Jambawalikar, S.R.; Schwartz, L.H.; Shukla-Dave, A.; Chenevert, T.L. Multicenter Repeatability Study of a Novel Quantitative Diffusion Kurtosis Imaging Phantom. Tomography 2019, 5, 36–43. [Google Scholar] [CrossRef]
- Keenan, K.E.; Biller, J.R.; Delfino, J.G.; Boss, M.A.; Does, M.D.; Evelhoch, J.L.; Griswold, M.A.; Gunter, J.L.; Hinks, R.S.; Hoffman, S.W. Recommendations towards standards for quantitative MRI (qMRI) and outstanding needs. J. Magn. Reson. Imaging JMRI 2019, 49, e26. [Google Scholar] [CrossRef] [PubMed]
- Shukla-Dave, A.; Obuchowski, N.A.; Chenevert, T.L.; Jambawalikar, S.; Schwartz, L.H.; Malyarenko, D.; Huang, W.; Noworolski, S.M.; Young, R.J.; Shiroishi, M.S.; et al. Quantitative imaging biomarkers alliance (QIBA) recommendations for improved precision of DWI and DCE-MRI derived biomarkers in multicenter oncology trials. J. Magn. Reson. Imaging 2019, 49, e101–e121. [Google Scholar] [CrossRef]
- Zwanenburg, A.; Vallières, M.; Abdalah, M.A.; Aerts, H.; Andrearczyk, V.; Apte, A.; Ashrafinia, S.; Bakas, S.; Beukinga, R.J.; Boellaard, R.; et al. The Image Biomarker Standardization Initiative: Standardized Quantitative Radiomics for High-Throughput Image-based Phenotyping. Radiology 2020, 295, 328–338. [Google Scholar] [CrossRef]
- Le Bihan, D.; Iima, M.; Federau, C.; Sigmund, E.E. Intravoxel Incoherent Motion (IVIM) MRI: Principles and Applications; CRC Press: Boca Raton, FL, USA, 2018. [Google Scholar]
- Le Bihan, D. What can we see with IVIM MRI? NeuroImage 2019, 187, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Stejskal, E.O.; Tanner, J.E. Spin diffusion measurements: Spin echoes in the presence of a time-dependent field gradient. J. Chem. Phys. 1965, 42, 288–292. [Google Scholar] [CrossRef]
- Chen, H.; Chen, L.; Liu, F.; Lu, J.; Xu, C.; Wang, L. Diffusion-weighted magnetic resonance imaging in bladder cancer: Comparison of readout-segmented and single-shot EPI techniques. Cancer Imaging 2019, 19, 59. [Google Scholar] [CrossRef] [PubMed]
- Holland, D.; Kuperman, J.M.; Dale, A.M. Efficient correction of inhomogeneous static magnetic field-induced distortion in Echo Planar Imaging. Neuroimage 2010, 50, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Skare, S.; Newbould, R.D.; Clayton, D.B.; Albers, G.W.; Nagle, S.; Bammer, R. Clinical multishot DW-EPI through parallel imaging with considerations of susceptibility, motion, and noise. Magn. Reson. Med. 2007, 57, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Jiang, Z.; Shen, W.; Liu, H. Deep learning in bladder cancer imaging: A review. Front. Oncol. 2022, 12, 930917. [Google Scholar] [CrossRef]
- Le Bihan, D.; Breton, E.; Lallemand, D.; Aubin, M.L.; Vignaud, J.; Laval-Jeantet, M. Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 1988, 168, 497–505. [Google Scholar] [CrossRef]
- Jansen, J.F.; Stambuk, H.E.; Koutcher, J.A.; Shukla-Dave, A. Non-gaussian analysis of diffusion-weighted MR imaging in head and neck squamous cell carcinoma: A feasibility study. AJNR Am. J. Neuroradiol. 2010, 31, 741–748. [Google Scholar] [CrossRef]
- Jensen, J.H.; Helpern, J.A.; Ramani, A.; Lu, H.; Kaczynski, K. Diffusional kurtosis imaging: The quantification of non-gaussian water diffusion by means of magnetic resonance imaging. Magn. Reson. Med. 2005, 53, 1432–1440. [Google Scholar] [CrossRef]
- Lu, Y.; Jansen, J.F.; Mazaheri, Y.; Stambuk, H.E.; Koutcher, J.A.; Shukla-Dave, A. Extension of the intravoxel incoherent motion model to non-gaussian diffusion in head and neck cancer. J. Magn. Reson. Imaging 2012, 36, 1088–1096. [Google Scholar] [CrossRef] [PubMed]
- Abd Elwahab, K.M.; Desky, E.A.E.; Eldery, M.S.; Mohammad, F.F.; Seleem, M.M.; El-Babouly, I.M. Apparent Diffusion Coefficient Value can Predict Poor Bacillus Calmette-Guérin Responders in T1HG/NMIBC: Prospective Cohort Study. Clin. Genitourin. Cancer 2021, 19, e248–e254. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, S.; Takahara, T.; Kwee, T.C.; Waseda, Y.; Kobayashi, S.; Fujii, Y. DWI as an Imaging Biomarker for Bladder Cancer. AJR Am. J. Roentgenol. 2017, 208, 1218–1228. [Google Scholar] [CrossRef]
- Jackson, A.; Li, K.L.; Zhu, X. Semi-quantitative parameter analysis of DCE-MRI revisited: Monte-carlo simulation, clinical comparisons, and clinical validation of measurement errors in patients with type 2 neurofibromatosis. PLoS ONE 2014, 9, e90300. [Google Scholar] [CrossRef] [PubMed]
- Sourbron, S.; Buckley, D.L. Tracer kinetic modelling in MRI: Estimating perfusion and capillary permeability. Phys. Med. Biol. 2011, 57, R1. [Google Scholar] [CrossRef] [PubMed]
- Tofts, P.S.; Brix, G.; Buckley, D.L.; Evelhoch, J.L.; Henderson, E.; Knopp, M.V.; Larsson, H.B.; Lee, T.Y.; Mayr, N.A.; Parker, G.J. Estimating kinetic parameters from dynamic contrast-enhanced T1-weighted MRI of a diffusable tracer: Standardized quantities and symbols. J. Magn. Reson. Imaging Off. J. Int. Soc. Magn. Reson. Med. 1999, 10, 223–232. [Google Scholar] [CrossRef]
- Paudyal, R.; Grkovski, M.; Oh, J.H.; Schöder, H.; Nunez, D.A.; Hatzoglou, V.; Deasy, J.O.; Humm, J.L.; Lee, N.Y.; Shukla-Dave, A. Application of Community Detection Algorithm to Investigate the Correlation between Imaging Biomarkers of Tumor Metabolism, Hypoxia, Cellularity, and Perfusion for Precision Radiotherapy in Head and Neck Squamous Cell Carcinomas. Cancers 2021, 13, 3908. [Google Scholar] [CrossRef] [PubMed]
- Nath, K.; Paudyal, R.; Nelson, D.S.; Pickup, S.; Zhou, R.; Leeper, D.B.; Heitjan, D.F.; Springer, C.S.; Poptani, H.; Glickson, J.D. Acute changes in cellular-interstitial water exchange rate in DB-1 melanoma xenografts after lonidamine administration as a marker of tumor energetics and ion transport. Proc. Intl. Soc. Magn. Reson. Med. 2014, 22, 2757. [Google Scholar]
- Boca, B.; Caraiani, C.; Telecan, T.; Pintican, R.; Lebovici, A.; Andras, I.; Crisan, N.; Pavel, A.; Diosan, L.; Balint, Z.; et al. MRI-Based Radiomics in Bladder Cancer: A Systematic Review and Radiomics Quality Score Assessment. Diagnostics 2023, 13, 2300. [Google Scholar] [CrossRef]
- Kozikowski, M.; Suarez-Ibarrola, R.; Osiecki, R.; Bilski, K.; Gratzke, C.; Shariat, S.F.; Miernik, A.; Dobruch, J. Role of Radiomics in the Prediction of Muscle-invasive Bladder Cancer: A Systematic Review and Meta-analysis. Eur. Urol. Focus 2022, 8, 728–738. [Google Scholar] [CrossRef]
- Papanikolaou, N.; Matos, C.; Koh, D.M. How to develop a meaningful radiomic signature for clinical use in oncologic patients. Cancer Imaging 2020, 20, 33. [Google Scholar] [CrossRef] [PubMed]
- van Griethuysen, J.J.M.; Fedorov, A.; Parmar, C.; Hosny, A.; Aucoin, N.; Narayan, V.; Beets-Tan, R.G.H.; Fillion-Robin, J.C.; Pieper, S.; Aerts, H. Computational Radiomics System to Decode the Radiographic Phenotype. Cancer Res. 2017, 77, e104–e107. [Google Scholar] [CrossRef]
- Apte, A.P.; Iyer, A.; Crispin-Ortuzar, M.; Pandya, R.; van Dijk, L.V.; Spezi, E.; Thor, M.; Um, H.; Veeraraghavan, H.; Oh, J.H.; et al. Technical Note: Extension of CERR for computational radiomics: A comprehensive MATLAB platform for reproducible radiomics research. Med. Phys. 2018, 45, 3713–3720. [Google Scholar] [CrossRef]
- Nioche, C.; Orlhac, F.; Boughdad, S.; Reuzé, S.; Goya-Outi, J.; Robert, C.; Pellot-Barakat, C.; Soussan, M.; Frouin, F.; Buvat, I. LIFEx: A Freeware for Radiomic Feature Calculation in Multimodality Imaging to Accelerate Advances in the Characterization of Tumor Heterogeneity. Cancer Res. 2018, 78, 4786–4789. [Google Scholar] [CrossRef]
- Zhang, L.; Fried, D.V.; Fave, X.J.; Hunter, L.A.; Yang, J.; Court, L.E. IBEX: An open infrastructure software platform to facilitate collaborative work in radiomics. Med. Phys. 2015, 42, 1341–1353. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.H.; Lin, C.Y.; Shih, M.J.; Wang, H.M.; Ho, T.Y.; Liao, C.T.; Yen, T.C. Development and evaluation of an open-source software package "CGITA" for quantifying tumor heterogeneity with molecular images. Biomed. Res. Int. 2014, 2014, 248505. [Google Scholar] [CrossRef] [PubMed]
- Pfaehler, E.; Zwanenburg, A.; de Jong, J.R.; Boellaard, R. RaCaT: An open source and easy to use radiomics calculator tool. PLoS ONE 2019, 14, e0212223. [Google Scholar] [CrossRef] [PubMed]
- Bagher-Ebadian, H.; Chetty, I.J. Technical Note: ROdiomiX: A validated software for radiomics analysis of medical images in radiation oncology. Med. Phys. 2021, 48, 354–365. [Google Scholar] [CrossRef] [PubMed]
- El-Assmy, A.; Abou-El-Ghar, M.E.; Mosbah, A.; El-Nahas, A.R.; Refaie, H.F.; Hekal, I.A.; El-Diasty, T.; Ibrahiem, E.H. Bladder tumour staging: Comparison of diffusion- and T2-weighted MR imaging. Eur. Radiol. 2009, 19, 1575–1581. [Google Scholar] [CrossRef] [PubMed]
- Panebianco, V.; De Berardinis, E.; Barchetti, G.; Simone, G.; Leonardo, C.; Grompone, M.D.; Del Monte, M.; Carano, D.; Gallucci, M.; Catto, J.; et al. An evaluation of morphological and functional multi-parametric MRI sequences in classifying non-muscle and muscle invasive bladder cancer. Eur. Radiol. 2017, 27, 3759–3766. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.H.; Tan, C.H.; Faria, S.C.; Kundra, V. Role of Imaging in the Local Staging of Urothelial Carcinoma of the Bladder. AJR Am. J. Roentgenol. 2017, 208, 1193–1205. [Google Scholar] [CrossRef]
- Hugen, C.M.; Duddalwar, V.; Daneshmand, S. Preoperative Imaging for Clinical Staging Prior to Radical Cystectomy. Curr. Urol. Rep. 2016, 17, 62. [Google Scholar] [CrossRef]
- Tekes, A.; Kamel, I.; Imam, K.; Szarf, G.; Schoenberg, M.; Nasir, K.; Thompson, R.; Bluemke, D. Dynamic MRI of bladder cancer: Evaluation of staging accuracy. AJR Am. J. Roentgenol. 2005, 184, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.B.; Lee, N.K.; Kim, S.; Son, I.W.; Ha, H.K.; Ku, J.Y.; Kim, K.H.; Park, W.Y. Vesical Imaging-Reporting and Data System for Multiparametric MRI to Predict the Presence of Muscle Invasion for Bladder Cancer. J. Magn. Reson. Imaging 2020, 52, 1249–1256. [Google Scholar] [CrossRef]
- Green, D.A.; Durand, M.; Gumpeni, N.; Rink, M.; Cha, E.K.; Karakiewicz, P.I.; Scherr, D.S.; Shariat, S.F. Role of magnetic resonance imaging in bladder cancer: Current status and emerging techniques. BJU Int. 2012, 110, 1463–1470. [Google Scholar] [CrossRef] [PubMed]
- Al Johi, R.S.; Seifeldein, G.S.; Moeen, A.M.; Aboulhagag, N.A.; Moussa, E.M.; Hameed, D.A.; Imam, H.M. Diffusion weighted magnetic resonance imaging in bladder cancer, is it time to replace biopsy? Cent. Eur. J. Urol. 2018, 71, 31–37. [Google Scholar] [CrossRef]
- Gillies, R.J.; Kinahan, P.E.; Hricak, H. Radiomics: Images Are More than Pictures, They Are Data. Radiology 2016, 278, 563–577. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Yang, Z.; Zhang, G.; Cui, G.; Xiong, X.; Liang, Z.; Lu, H. Characterization of texture features of bladder carcinoma and the bladder wall on MRI: Initial experience. Acad. Radiol. 2013, 20, 930–938. [Google Scholar] [CrossRef]
- Xu, X.; Zhang, X.; Tian, Q.; Zhang, G.; Liu, Y.; Cui, G.; Meng, J.; Wu, Y.; Liu, T.; Yang, Z.; et al. Three-dimensional texture features from intensity and high-order derivative maps for the discrimination between bladder tumors and wall tissues via MRI. Int. J. Comput. Assist. Radiol. Surg. 2017, 12, 645–656. [Google Scholar] [CrossRef]
- Zhang, X.; Xu, X.; Tian, Q.; Li, B.; Wu, Y.; Yang, Z.; Liang, Z.; Liu, Y.; Cui, G.; Lu, H. Radiomics assessment of bladder cancer grade using texture features from diffusion-weighted imaging. J. Magn. Reson. Imaging 2017, 46, 1281–1288. [Google Scholar] [CrossRef] [PubMed]
- Clements, M.B.; Atkinson, T.M.; Dalbagni, G.M.; Li, Y.; Vickers, A.J.; Herr, H.W.; Donat, S.M.; Sandhu, J.S.; Sjoberg, D.S.; Tin, A.L.; et al. Health-related Quality of Life for Patients Undergoing Radical Cystectomy: Results of a Large Prospective Cohort. Eur. Urol. 2022, 81, 294–304. [Google Scholar] [CrossRef] [PubMed]
- Parmar, A.; Qazi, A.A.; Stundzia, A.; Sim, H.W.; Lewin, J.; Metser, U.; O’Malley, M.; Hansen, A.R. Development of a radiomic signature for predicting response to neoadjuvant chemotherapy in muscle-invasive bladder cancer. Can. Urol. Assoc. J. 2022, 16, E113–E119. [Google Scholar] [CrossRef] [PubMed]
- Darvin, P.; Toor, S.M.; Sasidharan Nair, V.; Elkord, E. Immune checkpoint inhibitors: Recent progress and potential biomarkers. Exp. Mol. Med. 2018, 50, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Onoi, K.; Chihara, Y.; Uchino, J.; Shimamoto, T.; Morimoto, Y.; Iwasaku, M.; Kaneko, Y.; Yamada, T.; Takayama, K. Immune Checkpoint Inhibitors for Lung Cancer Treatment: A Review. J. Clin. Med. 2020, 9, 1362. [Google Scholar] [CrossRef]
- Koufopoulou, M.; Miranda, P.A.P.; Kazmierska, P.; Deshpande, S.; Gaitonde, P. Clinical evidence for the first-line treatment of advanced urothelial carcinoma: Current paradigms and emerging treatment options. Cancer Treat. Rev. 2020, 89, 102072. [Google Scholar] [CrossRef]
- Rosenblatt, R.; Sherif, A.; Rintala, E.; Wahlqvist, R.; Ullén, A.; Nilsson, S.; Malmström, P.U. Pathologic downstaging is a surrogate marker for efficacy and increased survival following neoadjuvant chemotherapy and radical cystectomy for muscle-invasive urothelial bladder cancer. Eur. Urol. 2012, 61, 1229–1238. [Google Scholar] [CrossRef]
- Sharabi, A.B.; Lim, M.; DeWeese, T.L.; Drake, C.G. Radiation and checkpoint blockade immunotherapy: Radiosensitisation and potential mechanisms of synergy. Lancet Oncol. 2015, 16, e498–e509. [Google Scholar] [CrossRef] [PubMed]
- van Hattum, J.W.; de Ruiter, B.M.; Oddens, J.R.; Hulshof, M.; de Reijke, T.M.; Bins, A.D. Bladder-Sparing Chemoradiotherapy Combined with Immune Checkpoint Inhibition for Locally Advanced Urothelial Bladder Cancer—A Review. Cancers 2021, 14, 38. [Google Scholar] [CrossRef] [PubMed]
- de Ruiter, B.M.; van Hattum, J.W.; Lipman, D.; de Reijke, T.M.; van Moorselaar, R.J.A.; van Gennep, E.J.; Maartje Piet, A.H.; Donker, M.; van der Hulle, T.; Voortman, J.; et al. Phase 1 Study of Chemoradiotherapy Combined with Nivolumab ± Ipilimumab for the Curative Treatment of Muscle-invasive Bladder Cancer. Eur. Urol. 2022, 82, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.A.; Taher, M.G.A.; Ali, W.A.; Ebrahem, M. Diagnostic performance of contrast-enhanced dynamic and diffusion-weighted MR imaging in the assessment of tumor response to neoadjuvant therapy in muscle-invasive bladder cancer. Abdom. Radiol. 2021, 46, 2712–2721. [Google Scholar] [CrossRef]
- Necchi, A.; Bandini, M.; Calareso, G.; Raggi, D.; Pederzoli, F.; Farè, E.; Colecchia, M.; Marandino, L.; Bianchi, M.; Gallina, A.; et al. Multiparametric Magnetic Resonance Imaging as a Noninvasive Assessment of Tumor Response to Neoadjuvant Pembrolizumab in Muscle-invasive Bladder Cancer: Preliminary Findings from the PURE-01 Study. Eur. Urol. 2020, 77, 636–643. [Google Scholar] [CrossRef]
- Huang, X.; Wang, X.; Lan, X.; Deng, J.; Lei, Y.; Lin, F. The role of radiomics with machine learning in the prediction of muscle-invasive bladder cancer: A mini review. Front. Oncol. 2022, 12, 990176. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhang, J.; Zhe, X.; Chang, H.; Tang, M.; Lei, X.; Zhang, L.; Zhang, X. An MRI-based radiomics nomogram in predicting histologic grade of non-muscle-invasive bladder cancer. Front. Oncol. 2023, 13, 1025972. [Google Scholar] [CrossRef]
- Wang, H.; Xu, X.; Zhang, X.; Liu, Y.; Ouyang, L.; Du, P.; Li, S.; Tian, Q.; Ling, J.; Guo, Y.; et al. Elaboration of a multisequence MRI-based radiomics signature for the preoperative prediction of the muscle-invasive status of bladder cancer: A double-center study. Eur. Radiol. 2020, 30, 4816–4827. [Google Scholar] [CrossRef]
- Xu, X.; Wang, H.; Du, P.; Zhang, F.; Li, S.; Zhang, Z.; Yuan, J.; Liang, Z.; Zhang, X.; Guo, Y.; et al. A predictive nomogram for individualized recurrence stratification of bladder cancer using multiparametric MRI and clinical risk factors. J. Magn. Reson. Imaging 2019, 50, 1893–1904. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Z.; Gu, Z.; Xu, F.; Maskey, N.; He, Y.; Yan, Y.; Xu, T.; Liu, S.; Yao, X. Magnetic resonance imaging-based radiomics signature for preoperative prediction of Ki67 expression in bladder cancer. Cancer Imaging 2021, 21, 65. [Google Scholar] [CrossRef]
- Kimura, K.; Yoshida, S.; Tsuchiya, J.; Yamada, I.; Tanaka, H.; Yokoyama, M.; Matsuoka, Y.; Yoshimura, R.; Tateishi, U.; Fujii, Y. Usefulness of texture features of apparent diffusion coefficient maps in predicting chemoradiotherapy response in muscle-invasive bladder cancer. Eur. Radiol. 2022, 32, 671–679. [Google Scholar] [CrossRef]
- Borhani, S.; Borhani, R.; Kajdacsy-Balla, A. Artificial intelligence: A promising frontier in bladder cancer diagnosis and outcome prediction. Crit. Rev. Oncol. Hematol. 2022, 171, 103601. [Google Scholar] [CrossRef] [PubMed]
- Cha, K.H.; Hadjiiski, L.; Samala, R.K.; Chan, H.P.; Caoili, E.M.; Cohan, R.H. Urinary bladder segmentation in CT urography using deep-learning convolutional neural network and level sets. Med. Phys. 2016, 43, 1882. [Google Scholar] [CrossRef] [PubMed]
- Cha, K.H.; Hadjiiski, L.M.; Samala, R.K.; Chan, H.P.; Cohan, R.H.; Caoili, E.M.; Paramagul, C.; Alva, A.; Weizer, A.Z. Bladder Cancer Segmentation in CT for Treatment Response Assessment: Application of Deep-Learning Convolution Neural Network-A Pilot Study. Tomography 2016, 2, 421–429. [Google Scholar] [CrossRef]
- Cha, K.H.; Hadjiiski, L.M.; Cohan, R.H.; Chan, H.P.; Caoili, E.M.; Davenport, M.S.; Samala, R.K.; Weizer, A.Z.; Alva, A.; Kirova-Nedyalkova, G.; et al. Diagnostic Accuracy of CT for Prediction of Bladder Cancer Treatment Response with and without Computerized Decision Support. Acad. Radiol. 2019, 26, 1137–1145. [Google Scholar] [CrossRef]
- Ma, X.; Hadjiiski, L.M.; Wei, J.; Chan, H.P.; Cha, K.H.; Cohan, R.H.; Caoili, E.M.; Samala, R.; Zhou, C.; Lu, Y. U-Net based deep learning bladder segmentation in CT urography. Med. Phys. 2019, 46, 1752–1765. [Google Scholar] [CrossRef]
- Gordon, M.N.; Hadjiiski, L.M.; Cha, K.H.; Samala, R.K.; Chan, H.P.; Cohan, R.H.; Caoili, E.M. Deep-learning convolutional neural network: Inner and outer bladder wall segmentation in CT urography. Med. Phys. 2019, 46, 634–648. [Google Scholar] [CrossRef]
- Ahn, H.; Hwang, S.I.; Lee, H.J.; Choe, G.; Oh, J.J.; Jeong, S.J.; Byun, S.S.; Kim, J.K. Quantitation of bladder cancer for the prediction of muscle layer invasion as a complement to the vesical imaging-reporting and data system. Eur. Radiol. 2021, 31, 1656–1666. [Google Scholar] [CrossRef]
- Li, R.; Chen, H.; Gong, G.; Wang, L. Bladder Wall Segmentation in MRI Images via Deep Learning and Anatomical Constraints. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2020, 2020, 1629–1632. [Google Scholar] [CrossRef]
- Dolz, J.; Xu, X.; Rony, J.; Yuan, J.; Liu, Y.; Granger, E.; Desrosiers, C.; Zhang, X.; Ben Ayed, I.; Lu, H. Multiregion segmentation of bladder cancer structures in MRI with progressive dilated convolutional networks. Med. Phys. 2018, 45, 5482–5493. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, S.; Tambo, M.; Watanabe, M.; Machida, H.; Kariyasu, T.; Fukushima, K.; Shimizu, Y.; Okegawa, T.; Yokoyama, K.; Fukuhara, H. Prospective Validation of Vesical Imaging-Reporting and Data System Using a Next-Generation Magnetic Resonance Imaging Scanner-Is Denoising Deep Learning Reconstruction Useful? J. Urol. 2021, 205, 686–692. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.; Taguchi, S.; Machida, H.; Tambo, M.; Takeshita, Y.; Kariyasu, T.; Fukushima, K.; Shimizu, Y.; Okegawa, T.; Fukuhara, H.; et al. Clinical validity of non-contrast-enhanced VI-RADS: Prospective study using 3-T MRI with high-gradient magnetic field. Eur. Radiol. 2022, 32, 7513–7521. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Cai, L.; Chen, C.; Fu, X.; Wang, L.; Yuan, B.; Yang, X.; Lu, Q. Cascade Path Augmentation Unet for bladder cancer segmentation in MRI. Med. Phys. 2022, 49, 4622–4631. [Google Scholar] [CrossRef] [PubMed]
- Coroamă, D.M.; Dioșan, L.; Telecan, T.; Andras, I.; Crișan, N.; Medan, P.; Andreica, A.; Caraiani, C.; Lebovici, A.; Boca, B.; et al. Fully automated bladder tumor segmentation from T2 MRI images using 3D U-Net algorithm. Front. Oncol. 2023, 13, 1096136. [Google Scholar] [CrossRef]
- Moribata, Y.; Kurata, Y.; Nishio, M.; Kido, A.; Otani, S.; Himoto, Y.; Nishio, N.; Furuta, A.; Onishi, H.; Masui, K.; et al. Automatic segmentation of bladder cancer on MRI using a convolutional neural network and reproducibility of radiomics features: A two-center study. Sci. Rep. 2023, 13, 628. [Google Scholar] [CrossRef]
- Goisauf, M.; Cano Abadía, M. Ethics of AI in Radiology: A Review of Ethical and Societal Implications. Front. Big Data 2022, 5, 850383. [Google Scholar] [CrossRef]
- Zou, Y.; Cai, L.; Chen, C.; Shao, Q.; Fu, X.; Yu, J.; Wang, L.; Chen, Z.; Yang, X.; Yuan, B.; et al. Multi-task deep learning based on T2-Weighted Images for predicting Muscular-Invasive Bladder Cancer. Comput. Biol. Med. 2022, 151, 106219. [Google Scholar] [CrossRef]
- Sevcenco, S.; Maj-Hes, A.B.; Hruby, S.; Ponhold, L.; Heinz-Peer, G.; Rauchenwald, M.; Marszalek, M.; Klingler, H.C.; Polanec, S.; Baltzer, P.A.T. Apparent diffusion coefficient values obtained by unenhanced MRI predicts disease-specific survival in bladder cancer. Clin. Radiol. 2018, 73, 881–885. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, S. Editorial Comment from Dr Taguchi to Role of Vesical Imaging-Reporting and Data System in predicting muscle-invasive bladder cancer: A diagnostic meta-analysis. Int. J. Urol. 2022, 29, 195–196. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Qiu, Z.; Cao, K.; Deng, L.; Zhang, W.; Xie, C.; Yang, S.; Yue, P.; Zhong, J.; Lyu, J.; et al. Pre-dicting muscle invasion in bladder cancer based on MRI: A comparison of radiomics, and single-task and multi-task deep learning. Comput. Methods Programs Biomed. 2023, 233, 107466. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, S.; Koga, F.; Kawakami, S.; Ishii, C.; Tanaka, H.; Numao, N.; Sakai, Y.; Saito, K.; Masuda, H.; Fujii, Y.; et al. Initial experience of diffusion-weighted magnetic resonance imaging to assess therapeutic response to induction chemoradiotherapy against muscle-invasive bladder cancer. Urology 2010, 75, 387–391. [Google Scholar] [CrossRef]
- Kobayashi, S.; Koga, F.; Kajino, K.; Yoshita, S.; Ishii, C.; Tanaka, H.; Saito, K.; Masuda, H.; Fujii, Y.; Yamada, T.; et al. Apparent diffusion coefficient value reflects invasive and proliferative potential of bladder cancer. J. Magn. Reson. Imaging 2014, 39, 172–178. [Google Scholar] [CrossRef]
- Sevcenco, S.; Ponhold, L.; Heinz-Peer, G.; Fajkovic, H.; Haitel, A.; Susani, M.; Shariat, S.F.; Szarvas, T.; Baltzer, P.A. Prospective evaluation of diffusion-weighted MRI of the bladder as a biomarker for prediction of bladder cancer aggressiveness. Urol. Oncol. 2014, 32, 1166–1171. [Google Scholar] [CrossRef]
- Hafeez, S.; Koh, M.; Jones, K.; Ghzal, A.E.; D’Arcy, J.; Kumar, P.; Khoo, V.; Lalondrelle, S.; McDonald, F.; Thompson, A.; et al. Diffusion-weighted MRI to determine response and long-term clinical outcomes in muscle-invasive bladder cancer following neoadjuvant chemotherapy. Front. Oncol. 2022, 12, 961393. [Google Scholar] [CrossRef]
- Zheng, Z.; Xu, F.; Gu, Z.; Yan, Y.; Xu, T.; Liu, S.; Yao, X. Combining Multiparametric MRI Radiomics Signature With the Vesical Imaging-Reporting and Data System (VI-RADS) Score to Preoperatively Differentiate Muscle Invasion of Bladder Cancer. Front. Oncol. 2021, 11, 619893. [Google Scholar] [CrossRef]
- Ahuja, A.S. The impact of artificial intelligence in medicine on the future role of the physician. PeerJ 2019, 7, e7702. [Google Scholar] [CrossRef]
- Liu, Z.; Wang, S.; Dong, D.; Wei, J.; Fang, C.; Zhou, X.; Sun, K.; Li, L.; Li, B.; Wang, M.; et al. The Applications of Radiomics in Precision Diagnosis and Treatment of Oncology: Opportunities and Challenges. Theranostics 2019, 9, 1303–1322. [Google Scholar] [CrossRef]



| VI-RADS Score | Inferences |
|---|---|
| 1 | Muscle invasion is highly unlikely |
| 2 | Muscle invasion is unlikely to be present |
| 3 | Presence of muscle invasion is equivocal |
| 4 | Muscle invasion is likely |
| 5 | Invasion of muscle and beyond the bladder is very likely |
| # | Reference | MRI/Segmentation/ Tools/Statistical Method | Dataset | Conclusion |
|---|---|---|---|---|
| 1 | Li et al. (2023) [110] | T2w and DW-MRI, manual, PyRadiomics, LASSO | 3148 features, first order, shape and size, texture, wavelet filter, and Laplacian of Gaussian filter in 169 patients (70% training, 30% test); 24 optimal features | Radiomics combined with monograms can differentiate low-from high-grade NMIBCs. |
| 2 | Zhang et al. (2022) [26] | T2w, DW- and DCE-MRI, manual, and PyRadiomics | 23,688 features, first order, shape, and grey levels (GLCM, GLRLM, GLSZM, GLDM, and NGTDM) in 342 patients (239 training, 68 validation); 43 optimal features | T2w, DW-MRI, and DCE-MRI radiomics models could effectively assess the state of muscular invasion. |
| 3 | Wang et al. (2020) [111] | T2w and DW-MRI, manual, LASSO, logistic regression, and SVM-RFE | 1404 features, histogram, co-occurrence matrices, run-length matrix, and grey levels (NGTDM and GLRSZM) in 106 patients (64 training, 42 validation), 36 optimal features | Features selected by SVM-RFE reflect the regional heterogeneity of tumor tissues and can better characterize tissue heterogeneity differences between NMIBC and MIBC. |
| 4 | Xu et al. (2019) [112] | T2w, DW- and DCE-MRI, manual, SVM-RFE and LASSO | 1872 features, histogram, co-occurrence matrices, run-length matrix, and grey levels (NGTDM and GLSZM) in 71 patients (50 training, 21 validation), 24 optimal features | The radiomics–clinical nomogram has potential in the preoperative prediction of the first two years after transurethral resection of the bladder tumor. |
| 5 | Zheng et al. (2021) [113] | T2w and DCE-MRI, manual, PyRadiomics, and SMOTE-LASSO | 2436 features, 179 patients (70% training, 30% validation), 10 optimal features | The applied model could predict the Ki67 expression status and was associated with survival outcomes. |
| 6 | Kimura et al. 2022 [114] | ADC maps, manual and LIFEx, LIFEX, RF, and SVM | 46 features: histogram, shape, grey levels (GLCM, GLRLM, GLZLM, and NGLDM) in 45 patients, | The radiomics model can predict the CRT response and serve as a novel imaging biomarker. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akin, O.; Lema-Dopico, A.; Paudyal, R.; Konar, A.S.; Chenevert, T.L.; Malyarenko, D.; Hadjiiski, L.; Al-Ahmadie, H.; Goh, A.C.; Bochner, B.; et al. Multiparametric MRI in Era of Artificial Intelligence for Bladder Cancer Therapies. Cancers 2023, 15, 5468. https://doi.org/10.3390/cancers15225468
Akin O, Lema-Dopico A, Paudyal R, Konar AS, Chenevert TL, Malyarenko D, Hadjiiski L, Al-Ahmadie H, Goh AC, Bochner B, et al. Multiparametric MRI in Era of Artificial Intelligence for Bladder Cancer Therapies. Cancers. 2023; 15(22):5468. https://doi.org/10.3390/cancers15225468
Chicago/Turabian StyleAkin, Oguz, Alfonso Lema-Dopico, Ramesh Paudyal, Amaresha Shridhar Konar, Thomas L. Chenevert, Dariya Malyarenko, Lubomir Hadjiiski, Hikmat Al-Ahmadie, Alvin C. Goh, Bernard Bochner, and et al. 2023. "Multiparametric MRI in Era of Artificial Intelligence for Bladder Cancer Therapies" Cancers 15, no. 22: 5468. https://doi.org/10.3390/cancers15225468





