Abstract
Anaplastic thyroid cancer (ATC) is a rare tumour but also one of the most lethal malignancies. Therapeutic modalities have usually been limited, but clinical trials with new drugs are now being implemented. The aims of this study were to analyse the clinical presentation, therapeutic modalities and independent prognostic factors for survival. We also reviewed the most recent literature on novel ATC therapies. We performed a retrospective analysis of 79 patients diagnosed between 2000 and 2018. Variables with impact on survival were identified using the Cox proportional-hazard regression model. At presentation, 6.3% had thyroid-confined disease, 30.4% evidenced extrathyroidal extension and 60.8% were already metastatic. Surgery was feasible in 41.8% and radiotherapy was applied to 35.4%, with those receiving >45 Gy having longer estimated survival (p = 0.020). Chemotherapy, either conventional or with tyrosine kinase inhibitors, was performed in 17.7% and 7.6%, respectively. Multimodality therapy with surgery, radiotherapy and chemotherapy/tyrosine kinase inhibitors (TKI) had the greatest impact on disease specific survival (DSS), providing a risk reduction of death of 96.9% (hazard ratio (HR) = 0.031, 0.005–0.210, p < 0.001). We concluded that most of these patients join reference centres at advanced stages of disease and multimodality treatment may offer the best chances for prolonging survival.
1. Introduction
Anaplastic thyroid cancer (ATC) is a rare tumour but accounts for more than 50% of all deaths attributable to thyroid tumours [1]. Undeniably, ATC is one of the most lethal malignancies in humans, as it portends a median survival of only three to four months and a disease-specific mortality at one year of nearly 100% [2]. ATC’s loco-regional invasiveness may cause compressive symptoms, like dysphagia, dyspnoea, stridor and pain, and makes it usually inoperable. Therefore, this disease must be promptly recognized, in order to be managed in a specialized centre, by a multidisciplinary team with expertise in ATC, including endocrinologists, oncologists, surgeons, radiotherapists and pathologists [3].
Given its aggressiveness, the American Joint Committee on Cancer (AJCC) classifies all cases of ATC as stage IV: IVA describes all the tumours that are confined to the gland, IVB represents ATC with gross extrathyroidal extension and in stage IVC the tumour has already spread to distant sites [4]. The American Thyroid Association (ATA) guidelines [4] consider multimodal therapy with surgery, radiotherapy and/or chemotherapy, when feasible, as a reasonable approach in these cases; however, a significant proportion of the patients arrive to the health care centres at an advanced stage of disease and, to most of them, palliative and symptomatic care represent the wisest attitude to take.
Different from well-differentiated thyroid cancers (WDTC), ATC cells do not produce thyroglobulin, so there is no tumour marker for these tumours, and they do not respond to thyroid-stimulating hormone (TSH) suppression; furthermore, ATC cells do not uptake iodine, so radioiodine is ineffective in these patients [3]. Given the rarity of ATC, the studies analysing the impact of different therapeutic approaches are small and usually of a retrospective nature or they only report isolated cases. ATC is generally refractory to standard therapies, which renders these patients excellent candidates for innovative adjuvant therapies, including drugs targeting specific oncogenic mutations, tyrosine kinase inhibitors (TKI) and immune-modulating approaches [3].
The purpose of this study was to analyse the clinical presentation, therapeutic modalities and its outcomes, as well as the prognostic factors influencing disease specific survival (DSS), in a homogenous population of ATC followed at a single institution. Furthermore, we also reviewed the most recent literature on novel ATC therapies.
2. Materials and Methods
We performed a retrospective analysis of patients’ clinical files with ATC diagnosed between 2000 and 2018 and followed at Instituto Português de Oncologia de Lisboa, Francisco Gentil, Lisboa, Portugal. ATC diagnosis was made from cytological or histological specimens and confirmed by experienced pathologists. Cases in which WDTC represented the main counterpart of the histological piece were excluded.
Patients were identified from the Endocrinology and Pathology database. Data regarding demographic characteristics, clinical presentation, therapeutic approaches and its outcomes, and survival were collected and registered with Microsoft Excel (Microsoft, Redmond, WA, USA).
DSS after ATC diagnosis was analysed using the Kaplan–Meier method and log-rank test. The independent prognostic factors were identified using the Cox proportional-hazard regression model. A p-value < 0.05 was considered statistically significant. The statistical analysis was performed with IBM SPSS Version 23.
This study was approved by the Ethics Committee of Instituto Português de Oncologia de Lisboa Francisco Gentil (project number 1056).
3. Results
We included 79 patients, 53 (67.1%) of which were women. The median age at diagnosis was 74 (interquartile range (IQR): 15 years). The main clinical characteristics and their impact on median survival are presented in Table 1. The incidence of new ATC diagnosis over the last two decades at our institution is represented in Figure 1.

Table 1.
Clinicopathological characteristics.
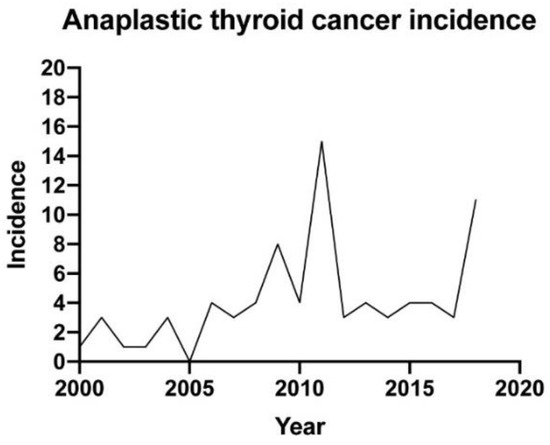
Figure 1.
Anaplastic thyroid cancer incidence.
The majority of patients (86.1%) presented compressive symptoms: 44 (55.7%) with dyspnoea, 32 (40.5%) with dysphagia, 20 (25.3%) with dysphonia and 25 (31.6%) complained of local pain; 31 (39.2%) patients had to be submitted to tracheostomy and 2 (2.5%) to tracheal prosthesis insertion; 8 (10.1%) needed a percutaneous endoscopic gastrostomy.
Almost half of the patients (37 (46.8%)) had a previous history of multinodular goiter. In the histological specimen, nine (11.4%) patients evidenced a WDTC area; three of these had been followed for a papillary thyroid cancer in the previous years and underwent subsequent dedifferentiation.
At presentation, more than 60% of the patients presented distant disease. The lungs were the most common site of metastases (45 (57.0%)), followed by bones (7 (14.3%)) and the brain (3 (4.0%)); in 39 patients (49%) only one tissue was affected.
The diagnostic approaches that were offered to our patients are presented in Table 1. Of the 33 (41.8%) patients who were submitted to surgery, resection margins were negative (R0) in 4 (12.5%), microscopic (R1) in 12 (37.5%) and macroscopic (R2) in 10 (31.3%). Surgical margins did not have impact on survival: estimated median survival for R0, R1 and R2 patients was 6.0, 8.0 and 3.0 months (p = 0.177), respectively (Figure 2). Radiotherapy was offered to 28 (35.4%) patients; median radiation dose was 28.8 (IQR: 46) Gy. Patients who received more than 45 Gy had longer estimated survival: 8.0 vs. 4.0 months, p = 0.020 (Figure 3). Additionally, seven (8.8%) patients were also submitted to radiosensitizing chemotherapy, yet although their estimated survival was higher, it did not reach statistical significance compared to radiotherapy alone (6.0 vs. 4.0 months, p = 0.085). Altogether, 14 (17.7%) patients were submitted to chemotherapy; the protocols included platin, taxane and/or anthracycline, as recommended by ATA guidelines [4], but the different regimens did not influence survival (p = 0.203). TKIs were offered to six (7.6%) patients: sorafenib to four, lenvatinib to one and sunitinib after progression with sorafenib to another patient.
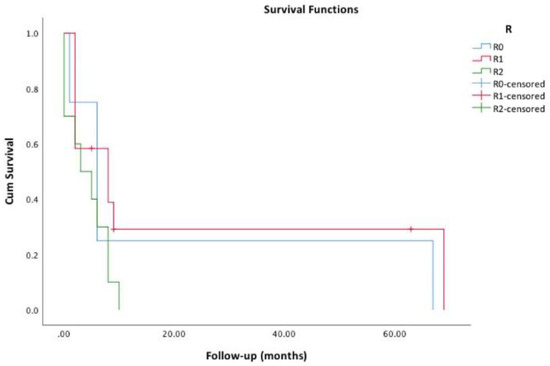
Figure 2.
Survival functions regarding surgical margins (R0 vs. R1 vs. R2).
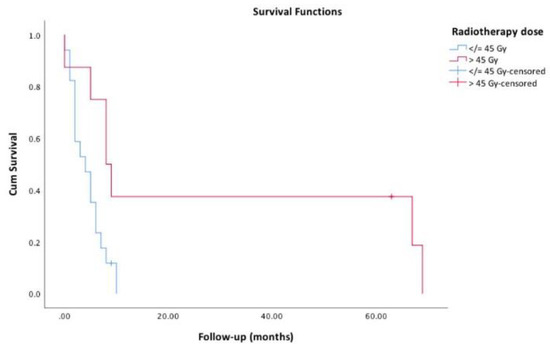
Figure 3.
Survival functions regarding radiotherapy dose (≤45 Gy vs. > 45 Gy).
Median estimate DSS was 2.0 months. However, four (5%) patients lived longer than one year. All of these were submitted to thyroidectomy with a multimodal approach. One patient remains alive, without evidence of disease, after 63 months of follow-up—he was 60 years old when he was submitted to thyroidectomy (surgery was R1), the tumour had well-differentiated areas, and he was also treated with adjuvant radiotherapy (total dose of 66 Gy) and chemotherapy with doxorubicin + docetaxel.
Multivariate analysis is shown in Table 2. Stage IVC, that is, metastatic disease, showed a tendency to influence survival. However, only the therapeutic approaches had a significant impact on overall survival: multimodality therapy with surgery, radiotherapy and chemotherapy/TKI had the greatest impact, providing a risk reduction of 96.9% of death for each month of follow-up, followed by surgery + radiotherapy, surgery + chemotherapy/TKI, surgery alone, and chemotherapy/TKI and/or radiotherapy, when comparing to isolated symptomatic care.

Table 2.
Multivariate analysis.
4. Discussion
ATC is an orphan disease that portends a very dismal prognosis. Multimodal approaches that include surgery have the largest impact in improving survival. At our institution, ATC diagnosis has shown a tendency to increase over the years and not to decrease (Figure 1), as observed by other authors [5,6]. We observed that our cases continue to be detected at later stages, since only 6.3% of the patients evidenced thyroid-confined disease at presentation. Accordingly, almost 90% had compressive symptoms, mainly dyspnoea. Furthermore, 60.8% had distant metastases at presentation. This is certainly due to the rapid growth typical of these tumours, but we cannot exclude a referral bias, since our hospital is a tertiary care centre. Furthermore, we also admit the unrecognition of the disease by primary and secondary care because almost half of our cohort had a previous history of a long-standing multinodular goiter, which represents a well-recognized risk factor for ATC, especially in elderly patients [3]. As verified by other authors [7,8], lungs were the primary sites of metastases (57%). Bone came as the second most common affected tissue (14.3%) which differs from other publications in which intrathoracic lymph nodes were the second most affected distant site. Six patients with IVC stage also showed coexistent well-differentiated areas at histology (data not shown), but we could not assess whether their metastases were from the well-differentiated or from the undifferentiated component.
In our cohort we identified, by univariate analysis, some characteristics that influenced survival: stage at diagnosis, leukocytosis, method of diagnosis, previous or coexistent WDTC and therapeutic approach. On multivariate analysis, despite the tendency for metastatic disease to influence overall survival, only the therapeutic approach had a strong statistical significance. Compared to isolated symptomatic care, surgery alone provided a risk reduction of death of 71.1%, but when combined with radiotherapy or chemotherapy/TKI this reduction was even greater (89.2% and 84.8%, respectively). The multimodality approach that included surgery plus radiotherapy and chemotherapy/TKI had the most beneficial impact on survival, portending a risk reduction of 96.9%. Interestingly, we verified that the amount of residual disease, either complete (R0 and R1) or incomplete (R2) surgery, did not affect survival. On the other hand, radiation dose of >45 Gy provided a longer survival. Neither the used regimens of chemotherapy nor the TKIs were associated with survival, but the number of patients who were submitted to these therapies was small, which hampered the analysis of their individual impact on prognosis. Different prognostic variables have been suggested in ATC. For instance, Glaser et al. [9] analysed the American National Cancer Database (NCDB) and identified total thyroidectomy and high-dose radiotherapy as independent prognostic factors in a cohort of 3552 patients. Lennon et al. [10] studied 64 Irish patients and recognised, as independent negative factors of survival, the presence of distance metastases and palliative care. In a smaller cohort, Machens et al. [11] reported that only nodal status influenced survival. Other authors [12] verified that age ≥70 years, presence of acute symptoms and leukocytosis at initial diagnosis, pT4b tumour, largest tumour dimension >5 cm and distant metastases, were all independent predictive factors of poorer survival. A multicentre German study that recently analysed a cohort of 100 ATC patients [13] reported similar demographic and clinicopathological characteristics to our patients; they found that radical surgery with sequential or simultaneous chemotherapy and radiotherapy was associated with survival in IVC patients (HR = 0.1, 0.03–0.31, p < 0.001). However, they noticed that surgery combined with either chemo or radiotherapy alone had no statistically significant benefit compared with surgery alone in their series of IVC patients. Also, in a cohort of 100 patients from Japan, Akaishi and colleagues [14] identified age ≥70 years, leukocytosis, extrathyroid invasion, distant metastases at diagnosis and, with greater impact, complete resection and radiotherapy ≥40 Gy, as independent prognostic factors, which is similar to our results. Haymart et al. [15] analysed the overall survival of 2742 ATC patients diagnosed between 1998 and 2008 and concluded that longer survival was associated with a more intensive and multimodal therapy. A study of 95 patients followed at Memorial Sloan-Kettering Cancer Centre [16] verified that in patients with locoregional disease, multimodality treatment with gross total surgical resection and postoperative radiotherapy with or without chemotherapy provided the best local control and had the greatest beneficial impact on DSS.
According to our results and to other reports [14,17,18,19], including a research by Pezzi and colleagues [17], that enrolled 1288 patients from the American NCDB, radiotherapy with cumulative doses of >40/45 Gy compared to lower dose regimens provided longer survival.
Only 17% of our patients were submitted to chemotherapy, making it difficult to draw any conclusion regarding the prognostic significance of this form of therapy. In general, chemotherapy response rates are very low in ATC (15–25%), bringing only a short period of benefit [20]. Ain et al. [21] reported a phase 2 clinical trial of a 96-h infusion of paclitaxel with the most satisfactory results, showing a total response rate of 53%. Chemotherapy in the neoadjuvant setting has only been evaluated in small studies (reviewed in [22]). One of these studies [23] investigated the effectiveness of weekly paclitaxel in stage IVB (n = 9) and observed a response rate of 33%.
Precision Medicine in ATC: Target and Immune Modulation Therapies
As also observed in our cohort, ATC has been identified in coexistence with well-differentiated areas, suggesting that these tumours can develop from pre-existing WDTC cases. On the other hand, it has also been hypothesised that these tumours may arise de novo. It has been postulated that the presence of mutated RAS and BRAF in follicular thyroid cancer (FTC) and papillary thyroid cancer (PTC), respectively, in association with later acquired alterations in TP53 and mTOR pathway, might be responsible for this process of dedifferentiation [2,24,25]. Our group has studied the mutational profiles of genes involved in the most deregulated cellular processes and molecular pathways in poorly-differentiated thyroid cancer (PDTC) and ATC [26]. We found that most mutations were present in TP53 and RAS genes. Mutations in CDKs, PIK3CA and PTEN were also present. In a recent study, Kunstman et al. [27] performed whole-exome sequencing in 22 ATC and 4 cell lines, finding the majority of variants clustered in the MAPK, ErbB and RAS signalling pathways. Somatic mutations in established thyroid cancer related genes (e.g., BRAF, TP53, RAS, CDKI, PIK3CA) were detected in 64% of those tumours. In addition, mutations in genes not previously associated with thyroid tumourigenesis were also observed (e.g., mTOR, NF1, NF2, MLH1, MLH3, MSH5 and MSH6). Landa et al. [28] also performed next-generation sequencing (NGS) of 341 cancer genes from 117 patient-derived PDTC and ATC and analysed the transcriptome of a representative subset of 37 tumours and found a high prevalence of TP53, TERT promoter, PI3K/AKT/mTOR pathway effectors, SWI/SNF subunits, and histone methyltransferases, beyond the BRAF and RAS mutations, which were the predominant drivers. The knowledge of the genomic landscape of ATC is becoming very important in clinical practice given that techniques like NGS or liquid biopsies enable a complete somatic analysis in only a few days. Different TKIs that target the abovementioned pathways have been developed and studied in ATC patients.. The mechanisms of action underlying the therapeutic effects of these drugs have been previously reviewed by our group [29] (see Table 3).

Table 3.
Tyrosine kinase and immune checkpoint inhibitors studied in ATC.
Therapy with lenvatinib and sorafenib were approved in WDTC by the Food and Drug Administration (FDA) and by the European Medicines Agency (EMA); however, these TKIs are not currently authorized in ATC by these regulatory agencies. However, lenvatinib was approved in Japan for ATC treatment after a phase II trial (NCT01728623) [30]. In the last year, the FDA approved a BRAF inhibitor (dabrafenib) in combination with a MEK inhibitor (trametinib) for BRAF-mutated ATC, based on a phase II trial (NCT02034110) [31]. The rationale behind this association is that the MEK inhibition prevents the rebound activation of MEK and ERK pathway after BRAF inhibition; this combination results in enhancement of BRAF-MEK-ERK pathway inhibition and anti-tumour activity [32]. Table 3 shows the drugs that have been approved and studied in ATC patients.
Tumour-infiltrating immune cells are present in most solid tumours and can affect the response to therapy and thus clinical outcome. Advances in immune-mediated therapies have evidenced the importance of expanding our understanding of thyroid cancer progression from intrinsic oncogenic pathways to the whole tumour microenvironment. Recently, some studies analysed the presence of certain immune cells, like tumour-associated macrophages, which seem to be prognostic factors in ATC [33]. Chintakuntlawar et al. [34] also investigated the prognostic value of the immune checkpoints programmed death-1 (PD-1) and its ligand (PD-L1) in these tumours and verified that PD-1 and PD-L1 are both highly expressed in ATC and are associated with shorter progression-free survival and overall survival in multimodality-treated patients. Different authors have reported the outcomes of distinct immune checkpoint inhibitors on ATC treatment (see Table 4), including pembrolizumab, a monoclonal antibody against PD-1 receptor approved by the FDA in different types of cancer. For instance, Iyer et al. [35] described a cohort of 12 patients with ATC who were treated with pembrolizumab in combination with TKI at the time of progression on TKI; they observed that the addition of pembrolizumab enabled a median overall survival and progression-free survival of 6.93 and 2.96 months, respectively. One year earlier, Kollipara et al. [36] had reported a clinical case of an ATC patient that showed complete remission after treatment with vemurafenib plus nivolumab (therapeutic choices guided by NGS results).

Table 4.
Reported results of tyrosine kinase and immune checkpoint inhibitors in ATC.
The studies analysing the effects of TKI and immune checkpoint inhibitors either isolated or in association are presented in Table 4. In Table 5 we show the clinical trials with these therapies that are currently recruiting or ongoing (www.clinicaltrials.gov; www.clinicaltrialsregister.eu; accessed on 18 May 2019).

Table 5.
Currently recruiting and ongoing clinical trials of tyrosine kinase and immune checkpoint inhibitors in ATC.
5. Conclusions
The present study reflects the largest experience with ATC in the country and is one of the largest reported in Europe. One limitation is its retrospective nature, which makes it difficult to retrieve data not stated in clinical files, but this problem is similar to the majority of the studies reported with this type of cancer.
The major issue about ATC, apart from the lack of effective therapeutic options, is that the great majority of patients join the reference centres at an advanced stage of disease. Thus, it is urgent to improve and speed up the recognition and referral of these aggressive cases to tertiary or oncological centres so that they can be promptly managed by a multidisciplinary team that offers a multimodality treatment, which is often complex and needs to be held at an institution with expertise in ATC. Recently, Cabanillas et al. [53] implemented at their centre a new process flow for patients with ATC, allowing their immediate schedule, which resulted in a 98% decrease in referral to disposition time and led to a significant increase in ATC referrals to their institution.
In conclusion, ATC management is very challenging, and prospective trials are needed, with clinical criteria that may be adjusted to the real ATC patients, who are usually old and with an advanced stage of disease. Multimodality approach with surgery, radiotherapy and chemotherapy, either conventional or with the new agents, may offer the best chances for survival enhancement.
Author Contributions
J.S.-P. planned the study, collected the data, performed the statistical analysis and wrote the manuscript; R.C. collected the data and performed the statistical analysis; E.L. provided the collected ATC cases and reviewed the manuscript; V.L. planned and supervised the study and reviewed the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors are thankful for the collaboration of the Endocrinology and Pathology Departments, from Instituto Português de Oncologia de Lisboa Francisco Gentil (IPOLFG), Lisboa, Portugal.
Conflicts of Interest
The authors have no conflicts of interests.
References
- Ragazzi, M.; Ciarrocchi, A.; Sancisi, V.; Bisagni, A.; Piana, S. Update on anaplastic thyroid carcinoma: Morphological, molecular, and genetic features of the most aggressive thyroid cancer. Int. J. Endocrinol. 2014, 2014, 79083. [Google Scholar] [CrossRef] [PubMed]
- Smallridge, R.C.; Marlow, L.A.; Copland, J.A. Anaplastic thyroid cancer: Molecular pathogenesis and emerging therapies. Endocr. Relat. Cancer 2009, 16, 17–44. [Google Scholar] [CrossRef] [PubMed]
- Molinaro, E.; Romei, C.; Biagini, A.; Sabini, E.; Agate, L.; Mazzeo, S.; Materazzi, G.; Sellari-Franceschini, S.; Ribechini, A.; Torregrossa, L.; et al. Anplastic thyroid carcinoma: From clinicopathology to genetics and advanced therapies. Nat. Rev. Endocrinol. 2017, 13, 644–660. [Google Scholar] [CrossRef] [PubMed]
- Smallridge, R.C.; Ain, K.B.; Asa, S.L.; Bible, K.C.; Brierley, J.D.; Burman, K.D.; Kebebew, E.; Lee, N.Y.; Nikiforov, Y.E.; Shah, M.H.; et al. American Thyryoid Association Anaplastic Thyroid Cancer Guidelines Taskforce. American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid 2012, 22, 1104–1139. [Google Scholar] [CrossRef] [PubMed]
- Davies, L.; Welch, H.G. Increasing incidence of thyroid cancer in the United States, 1973–2002. J. Am. Med. Assoc. 2006, 295, 2164–2167. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, B.; Prichard, R.S.; Lee, A.; Kelly, L.M.; Smyth, P.P.; Crotty, T.; McDermott, E.W.; Hill, A.D.; O’Higgins, N. Changing patterns of thyroid carcinoma. Ir. J. Med. Sci. 2007, 176, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Besic, N.; Gazic, B. Sites of Metastases of Anaplastic Thyroid Carcinoma: Autopsy Findings in 45 Cases from a Single Institution. Thyroid 2013, 23, 709–713. [Google Scholar] [CrossRef]
- Ibanez, M.L.; Russell, W.O.; Albores-Saavedra, J.; Lampertico, P.; White, E.C.; Clark, R.L. Thyroid carcinoma—Biologic behavior and mortality. Postmortem findings in 42 cases, including 27 in which the disease was fatal. Cancer 1966, 19, 1039–1052. [Google Scholar] [CrossRef]
- Glaser, S.M.; Mandish, S.F.; Gill, B.S.; Balasubramani, G.K.; Clump, D.A.; Beriwal, S. Anaplastic thyroid cancer: Prognostic factors, patterns of care, and overall survival. Head Neck 2016, 38, E2083–E2090. [Google Scholar] [CrossRef]
- Lennon, P.; Deady, S.; Healy, M.L.; Toner, M.; Kinsella, J.; Timon, C.I.; O’Neill, J.P. Anaplastic thyroid carcinoma: Failure of conventional therapy but hope of targeted therapy. Head Neck 2016, 38, E1122–E1129. [Google Scholar] [CrossRef]
- Machens, A.; Hinze, R.; Lautenschläger, C.; Thomusch, O.; Dunst, J.; Dralle, H. Extended surgery and early postoperative radiotherapy for undifferentiated thyroid carcinoma. Thyroid 2001, 11, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Sugitani, I.; Miyauchi, A.; Sugino, K.; Okamoto, T.; Yoshida, A.; Suzuki, S. Prognostic factors and treatment outcomes for anaplastic thyroid carcinoma: ATC Research Consortium of Japan cohort study of 677 patients. World J. Surg. 2012, 36, 1247–1254. [Google Scholar] [CrossRef] [PubMed]
- Wendler, J.; Kroiss, M.; Gast, K.; Kreissl, M.C.; Allelein, S.; Lichtenauer, U.; Blaser, R.; Spitzweg, C.; Fassnacht, M.; Schott, M.; et al. Clinical presentation, treatment and outcome of anaplastic thyroid carcinoma: Results of a multicentre study in Germany. Eur. J. Endocrinol. 2016, 175, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Akaishi, J.; Sugino, K.; Kitagawa, W.; Nagahama, M.; Kameyama, K.; Shimizu, K.; Ito, K. Prognostic factors and treatment outcomes of 100 cases of anaplastic thyroid carcinoma. Thyroid 2011, 21, 1183–1189. [Google Scholar] [CrossRef] [PubMed]
- Haymart, M.R.; Banerjee, M.; Yin, H.; Worden, F.; Griggs, J.J. Marginal treatment benefit in anaplastic thyroid cancer. Cancer 2013, 119, 3133–3139. [Google Scholar] [CrossRef]
- Mohebati, A.; Dilorenzo, M.; Palmer, F.; Patel, S.G.; Pfister, D.; Lee, N.; Tuttle, R.M.; Shaha, A.R.; Shah, J.P.; Ganly, I. Anaplastic thyroid carcinoma: A 25-year single-institution experience. Ann. Surg. Oncol. 2014, 21, 1665–1670. [Google Scholar] [CrossRef] [PubMed]
- Pezzi, T.A.; Mohamed, A.S.R.; Sheu, T.; Blanchard, P.; Sandulache, V.C.; Lai, S.Y.; Cabanillas, M.E.; Williams, M.D.; Pezzi, C.M.; Lu, C.; et al. Radiation therapy dose is associated with improved survival for unresected anaplastic thyroid carcinoma: Outcomes from the National CancerData Base. Cancer 2017, 123, 1653–1661. [Google Scholar] [CrossRef]
- Sun, C.; Li, Q.; Hu, Z.; He, J.; Li, C.; Li, G.; Tao, X.; Yang, A. Treatment and prognosis of anaplastic thyroid carcinoma: Experience from a single institution in China. PLoS ONE 2013, 8, e80011. [Google Scholar] [CrossRef]
- Dumke, A.K.; Pelz, T.; Vordermark, D. Long-term results of radiotherapy in anaplastic thyroid cancer. Radiat. Oncol. 2014, 9, 90. [Google Scholar] [CrossRef]
- Iyer, P.C.; Dadu, R.; Ferrarotto, R.; Busaidy, N.L.; Habra, M.A.; Zafereo, M.; Gross, N.; Hess, K.R.; Gule-Monroe, M.; Williams, M.D.; et al. Real-World Experience with Targeted Therapy for the Treatment of Anaplastic Thyroid Carcinoma. Thyroid 2018, 28, 79–87. [Google Scholar] [CrossRef]
- Ain, K.B.; Egorin, M.J.; DeSimone, P.A. Treatment of anaplastic thyroid carcinoma with Paclitaxel: Phase 2 trial using ninety-six-hour infusion. Thyroid 2000, 10, 587–594. [Google Scholar] [CrossRef] [PubMed]
- Cabanillas, M.E.; Zafereo, M.; Gunn, G.B.; Ferrarotto, R. Anaplastic Thyroid Carcinoma: Treatment in the Age of Molecular Targeted Therapy. J. Oncol. Pract. 2016, 12, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Higashiyama, T.; Ito, Y.; Hirokawa, M.; Fukushima, M.; Uruno, T.; Miya, A.; Matsuzuka, F.; Miyauchi, A. Induction chemotherapy with weekly paclitaxel administration for anaplastic thyroid carcinoma. Thyroid 2010, 20, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Kondo, T.; Ezzat, S.; Asa, S.L. Pathogenetic mechanisms in thyroid follicular-cell neoplasia. Nat. Rev. Cancer 2006, 6, 292–306. [Google Scholar] [CrossRef] [PubMed]
- Nikiforov, Y.E.; Nikiforova, M.N. Molecular genetics and diagnosis of thyroid cancer. Nat. Rev. Endocrinol. 2011, 7, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Pita, J.M.; Banito, A.; Cavaco, B.M.; Leite, V. Gene expression profiling associated with the progression to poorly differentiated thyroid carcinomas. Br. J. Cancer 2009, 101, 1782–1791. [Google Scholar] [CrossRef] [PubMed]
- Kunstman, J.W.; Juhlin, C.C.; Goh, G.; Brown, T.C.; Stenman, A.; Healy, J.M.; Rubinstein, J.C.; Choi, M.; Kiss, N.; Nelson-Williams, C.; et al. Characterization of the mutational landscape of anaplastic thyroid cancer via whole-exome sequencing. Hum. Mol. Genet. 2015, 24, 2318–2329. [Google Scholar] [CrossRef] [PubMed]
- Landa, I.; Ibrahimpasic, T.; Boucai, L.; Sinha, R.; Knauf, J.A.; Shah, R.H.; Dogan, S.; Ricarte-Filho, J.C.; Krishnamoorthy, G.P.; Xu, B.; et al. Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J. Clin. Investig. 2016, 126, 1052–1066. [Google Scholar] [CrossRef] [PubMed]
- Donato, S.; Santos, R.; Simões, H.; Leite, V. Novel therapies against aggressive differentiated thyroid carcinomas. Int. J. Endocr. Oncol. 2018, 5. [Google Scholar] [CrossRef]
- Tahara, M.; Kiyota, N.; Yamazaki, T.; Chayahara, N.; Nakano, K.; Inagaki, L.; Toda, K.; Enokida, T.; Minami, H.; Imamura, Y.; et al. Lenvatinib for Anaplastic Thyroid Cancer. Front. Oncol. 2017, 7, 25. [Google Scholar] [CrossRef] [PubMed]
- Subbiah, V.; Kreitman, R.J.; Wainberg, Z.A.; Cho, J.Y.; Schellens, J.H.M.; Soria, J.C.; Wen, P.Y.; Zielinski, C.; Cabanillas, M.E.; Urbanowitz, G.; et al. Dabrafenib and Trametinib Treatment in Patients with Locally Advanced or Metastatic BRAF V600–Mutant Anaplastic Thyroid Cancer. J. Clin. Oncol. 2017, 36, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Lito, P.; Pratilas, C.A.; Joseph, E.W.; Tadj, M.; Halilovic, E.; Zubrowski, M.; Huang, A.; Wong, W.L.; Callahan, M.K.; Merghoub, T.; et al. Relief of profound feedback inhibition of mitogenic signaling by RAF inhibitors attenuates their activity in BRAFV600E melanomas. Cancer Cell 2012, 22, 668–682. [Google Scholar] [CrossRef] [PubMed]
- Ryder, M.; Ghossein, R.A.; Ricarte-Filho, J.C.; Knauf, J.A.; Fagin, J.A. Increased density of tumor-associated macrophages is associated with decreased survival in advanced thyroid cancer. Endocr. Relat. Cancer 2008, 15, 1069–1074. [Google Scholar] [CrossRef] [PubMed]
- Chintakuntlawar, A.V.; Rumilla, K.M.; Smith, C.Y.; Jenkins, S.M.; Foote, R.L.; Kasperbauer, J.L.; Morris, J.C.; Ryder, M.; Alsidawi, S.; Hilger, C.; et al. Expression of PD-1 and PD-L1 in Anaplastic Thyroid Cancer Patients Treated with Multimodal Therapy: Results from a Retrospective Study. J. Clin. Endocrinol. Metab. 2017, 102, 1943–1950. [Google Scholar] [CrossRef] [PubMed]
- Iyer, P.C.; Dadu, R.; Gule-Monroe, M.; Busaidy, N.L.; Ferrarotto, R.; Habra, M.A.; Zafereo, M.; Williams, M.D.; Gunn, G.B.; Grosu, H.; et al. Salvage pembrolizumab added to kinase inhibitor therapy for the treatment of anaplastic thyroid carcinoma. J. Immunother. Cancer 2018, 11, 68. [Google Scholar] [CrossRef]
- Kollipara, R.; Schneider, B.; Radovich, M.; Babu, S.; Kiel, P.J. Exceptional Response with Immunotherapy in a Patient with Anaplastic Thyroid Cancer. Oncologist 2017, 22, 1149–1151. [Google Scholar] [CrossRef] [PubMed]
- Sherman, E.J.; Tsai, C.J.; Zhi, W.I.; Fetten, J.V.; Wu, V.; Ho, A.L.; Riaz, N.; Pfister, D.G.; Lee, N.Y. Pilot study combining PD-L1 antibody durvalumab (D) with CTLA-4 antibody tremelimumab (T) and stereotactic body radiotherapy (SBRT) to treat metastatic anaplastic thyroid cancer (ATC). J. Clin. Oncol. 2019, 37 (Suppl. S15). [Google Scholar] [CrossRef]
- Harris, E.J.; Hanna, G.J.; Chau, N.; Rabinowits, G.; Haddad, R.; Margalit, D.N.; Schoenfeld, J.; Tishler, R.B.; Barletta, J.A.; Nehs, M.; et al. Everolimus in Anaplastic Thyroid Cancer: A Case Series. Front. Oncol. 2019, 9, 106. [Google Scholar] [CrossRef] [PubMed]
- Wirth, L.J.E.E.; Capdevila, J.; Paz-Ares, L.G.; Lin, C.; Taylor, M.H.; Ramlau, R.; Butler, M.; Delord, J.P.; Horvath, Z.; Gelderblom, H.; et al. Phase I/II study of spartalizumab (PDR001), an anti-PD1 mAb, in patients with anaplastic thyroid cancer. J. Clin. Oncol. 2018, 36 (Suppl. S15). [Google Scholar] [CrossRef]
- Ito, Y.; Onoda, N.; Ito, K.; Sugitani, I.; Takahashi, S.; Yamaguchi, I.; Kabu, K.; Tsukada, K. Sorafenib in Japanese patients with locally advanced or metastatic medullary thyroid carcinoma and anaplastic thyroid carcinoma. Thyroid 2017, 27, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Ravaud, A.; De la Fouchardière, C.; Caron, P.; Doussau, A.; Do Cao, C.; Asselineau, J.; Rodien, P.; Pouessel, D.; Nicolli-Sire, P.; Klein, M.; et al. A multicenter phase II study of sunitinib in patients with locally advanced or metastatic differentiated, anaplastic or medullary thyroid carcinomas: Mature data from the THYSU study. Eur. J. Cancer 2017, 76, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Iniguez-Ariza, N.M.; Ryder, M.M.; Hilger, C.R.; Bible, K.C. Salvage Lenvatinib therapy in metastatic anaplastic thyroid Cancer. Thyroid 2017, 27, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Hyman, D.M.; Puzanov, I.; Subbiah, V.; Faris, J.E.; Chau, I.; Blay, J.Y.; Wolf, J.; Raje, N.S.; Diamond, E.L.; Hollebecque, A.; et al. Vemurafenib in multiple nonmelanoma cancers with BRAF V600 mutations. N. Engl. J. Med. 2015, 373, 726–736. [Google Scholar] [CrossRef] [PubMed]
- Godbert, Y.; Henriques de Figueiredo, B.; Bonichon, F.; Chibon, F.; Hostein, I.; Perot, G.; Dupin, C.; Daubech, A.; Belleannee, G.; Gros, A.; et al. Remarkable response to crizotinib in woman with anaplastic lymphoma kinase-rearranged anaplastic thyroid carcinoma. J. Clin. Oncol. 2015, 33, 84–87. [Google Scholar] [CrossRef] [PubMed]
- Marten, K.A.; Gudena, V.K. Use of vemurafenib in anaplastic thyroid carcinoma: A case report. Cancer Biol. Ther. 2015, 16, 1430–1433. [Google Scholar] [CrossRef] [PubMed]
- Wagle, N.; Grabiner, B.C.; Van Allen, E.M.; Amin-Mansour, A.; Taylor-Weiner, A.; Rosenberg, M.; Gray, N.; Barletta, J.A.; Guo, Y.; Swanson, S.J.; et al. Response and acquired resistance to everolimus in anaplastic thyroid cancer. N. Engl. J. Med. 2014, 371, 1426–1433. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.M.; Chang, H.; Yoon, M.J.; Hong, Y.K.; Kim, H.; Chung, W.Y.; Park, C.S.; Nam, K.H.; Kang, S.W.; Kim, M.K.; et al. A multicenter, phase II trial of everolimus in locally advanced or metastatic thyroid cancer of all histologic subtypes. Ann. Oncol. 2013, 24, 3089–3094. [Google Scholar] [CrossRef] [PubMed]
- Savvides, P.; Nagaiah, G.; Lavertu, P.; Fu, P.; Wright, J.J.; Chapman, R.; Wasman, J.; Dowlati, A.; Remick, S.C. Phase II trial of sorafenib in patients with advanced anaplastic carcinoma of the thyroid. Thyroid 2013, 23, 600–604. [Google Scholar] [CrossRef]
- Rosove, M.H.; Peddi, P.F.; Glaspy, J.A. BRAF V600E inhibition in anaplastic thyroid cancer. N. Engl. J. Med. 2013, 368, 684–685. [Google Scholar] [CrossRef]
- Bible, K.C.; Suman, V.J.; Menefee, M.E.; Smallridge, R.C.; Molina, J.R.; Maples, W.J.; Karlin, N.J.; Travnor, A.M.; Kumar, P.; Goh, B.C.; et al. Mayo Phase 2 Consortium; Mayo Clinic Endocrine Malignances Disease Oriented Group. A multiinstitutional phase 2 trial of pazopanib monotherapy in advanced anaplastic thyroid cancer. J. Clin. Endocrinol. Metab. 2012, 97, 3179–3184. [Google Scholar] [CrossRef]
- Ha, H.T.; Lee, J.S.; Urba, S.; Koenig, R.J.; Sisson, J.; Giordano, T.; Worden, F.P. A phase II study of imatinib in patients with advanced anaplastic thyroid cancer. Thyroid 2010, 20, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Pennell, N.A.; Daniels, G.H.; Haddad, R.I.; Ross, D.S.; Evans, T.; Wirth, L.J.; Fidias, P.H.; Temel, J.S.; Gurubhagavatula, S.; Heist, R.S.; et al. A phase II study of gefitinib in patients with advanced thyroid cancer. Thyroid 2008, 18, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Cabanillas, M.E.; Williams, M.D.; Gunn, G.B.; Weitzman, S.P.; Burke, L.; Busaidy, N.L.; Ying, A.K.; Yiin, Y.H.; William, W.N.; Lu, C.; et al. Facilitating anaplastic thyroid cancer specialized treatment: A model for improving access to multidisciplinary care for patients with anaplastic thyroid cancer. Head Neck 2017, 39, 1291–1295. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).