Adapting the Healthy Eating Index 2010 for the Canadian Population: Evidence from the Canadian Community Health Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Dietary Intake Assessment
2.3. Anthropometric and Lifestyle Measurements
2.4. Developing HEI-C 2010: Adapting HEI-2010 to CFG 2007
2.5. Statistical Analyses
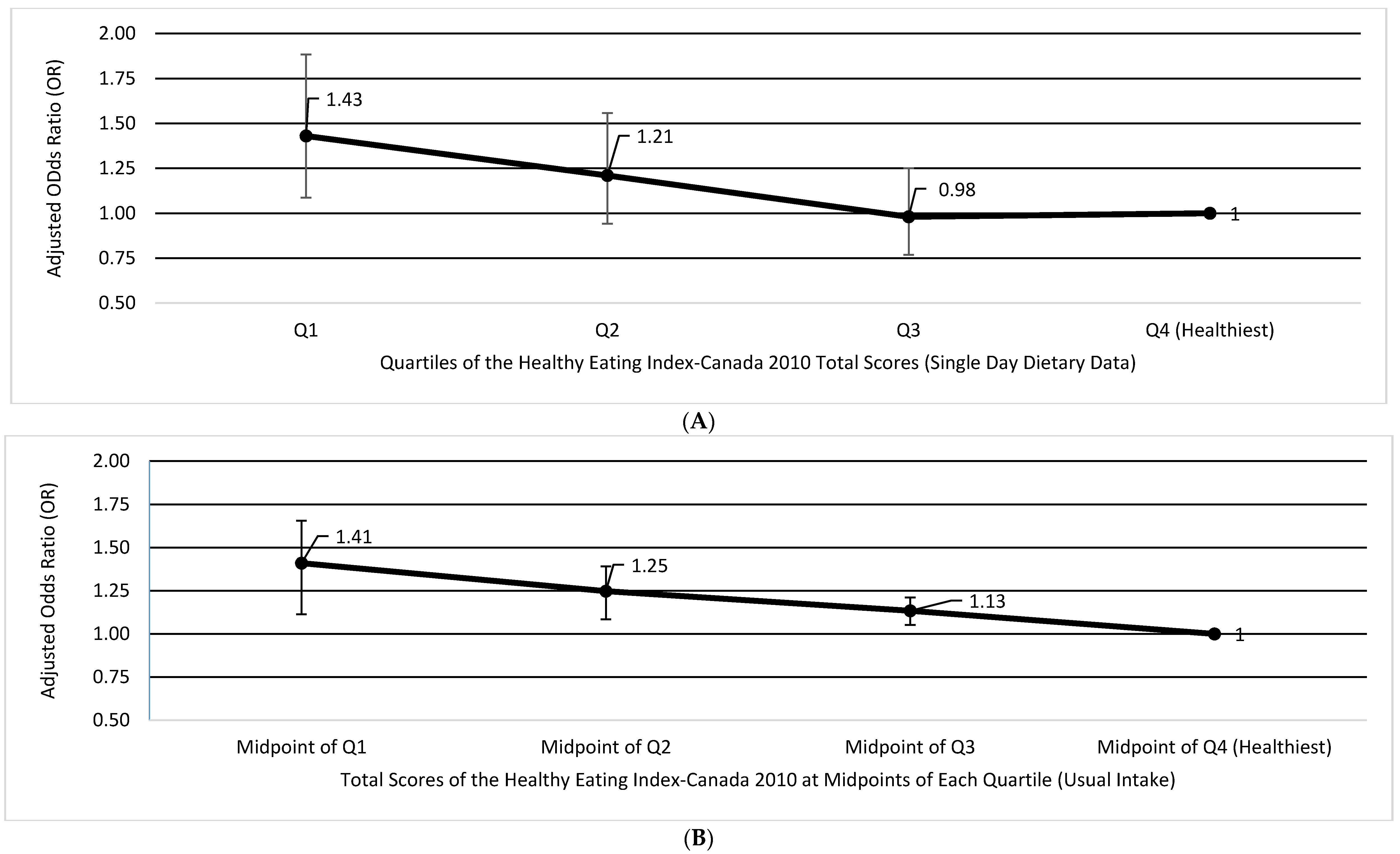
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Twells, L.K.; Gregory, D.M.; Reddigan, J.; Midodzi, W.K. Current and predicted prevalence of obesity in Canada: A trend analysis. CMAJ Open 2014, 2, E18–E26. [Google Scholar] [CrossRef] [PubMed]
- Ezzati, M.; Hoorn, S.V.; Rodgers, A.; Lopez, A.D.; Mathers, C.D.; Murray, C.J.L. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet 2003, 362, 271–280. [Google Scholar] [CrossRef]
- Lock, K.; Pomerleau, J.; Causer, L.; Altmann, D.R.; McKee, M. The global burden of disease attributable to low consumption of fruit and vegetables: Implications for the global strategy on diet. Bull. World Health Organ. 2005, 83, 100–108. [Google Scholar] [PubMed]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet 2013, 380, 2224–2260. [Google Scholar] [CrossRef]
- Kennedy, E.T.; Ohls, J.; Carlson, S.; Fleming, K. The healthy eating index: Design and applications. J. Am. Diet. Assoc. 1995, 95, 1103–1108. [Google Scholar] [CrossRef]
- Li, W.; Park, Y.; McGlynn, K.A.; Hollenbeck, A.R.; Taylor, P.R.; Goldstein, A.M.; Freedman, N.D. Index-based dietary patterns and risk of incident hepatocellular carcinoma and mortality from chronic liver disease in a prospective study. Hepatology 2014, 60, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Malagoli, C.; Malavolti, M.; Agnoli, C.; Crespi, C.M.; Fiorentini, C.; Farnetani, F.; Longo, C.; Ricci, C.; Albertini, G.; Lanzoni, A.; et al. Diet quality and risk of melanoma in an italian population. J. Nutr. 2015, 145, 1800–1807. [Google Scholar] [CrossRef] [PubMed]
- Anic, G.M.; Park, Y.; Subar, A.F.; Schap, T.E.; Reedy, J. Index-based dietary patterns and risk of lung cancer in the NIH-AARP diet and health study. Eur. J. Clin. Nutr. 2016, 70, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Vargas, A.J.; Neuhouser, M.L.; George, S.M.; Thomson, C.A.; Ho, G.Y.F.; Rohan, T.E.; Kato, I.; Nassir, R.; Hou, L.; Manson, J.E. Diet quality and colorectal cancer risk in the women’s health initiative observational study. Am. J. Epidemiol. 2016, 184, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Drenowatz, C.; Shook, R.P.; Hand, G.A.; Hébert, J.R.; Blair, S.N. The independent association between diet quality and body composition. Sci. Rep. 2014. [Google Scholar] [CrossRef] [PubMed]
- An, R. Diet quality and physical activity in relation to childhood obesity. Int. J. Adolesc. Med. Health 2015, 29, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Harmon, B.E.; Boushey, C.J.; Shvetsov, Y.B.; Ettienne, R.; Reedy, J.; Wilkens, L.R.; Le Marchand, L.; Henderson, B.E.; Kolonel, L.N. Associations of key diet-quality indexes with mortality in the multiethnic cohort: The dietary patterns methods project. Am. J. Clin. Nutr. 2015, 101, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Glanville, N.T.; McIntyre, L. Diet quality of atlantic families headed by single mothers. Can. J. Diet. Pract. Res. 2006, 67, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, S.J.; Hanning, R.M. Development and implications of a revised Canadian Healthy Eating Index (HEIC-2009). Public Health Nutr. 2010, 13, 820–825. [Google Scholar] [CrossRef] [PubMed]
- Garriguet, D. Diet quality in Canada. Health Rep. 2009, 20, 41–52. [Google Scholar] [PubMed]
- Health Canada. Eating Well with Canada’s Food Guide (2007): Development of the Food Intake Pattern. Available online: http://www.hc-sc.gc.ca/fn-an/pubs/fd_int_pat-ela_mod_alim-eng.php (assessed on 9 May 2017).
- Health Canada. Canadian Community Health Survey, Cycle 2.2, Nutrition (2004): A Guide to Accessing and Interpreting the Data. Available online: http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/cchs_guide_escc-eng.php (assessed on 1 August 2016).
- United States Department of Agriculture Agricultural Research Service. USDA Automated Multiple-Pass Method. Available online: http://www.ars.usda.gov/Services/docs.htm?docid=7710 (accessed on 30 May 2016).
- Health Canada. The Canadian Nutrient File; Nutrition Research Division: Ottawa, ON, Canada, 2001. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids; National Academy Press: Washington, DC, USA, 2005. [Google Scholar]
- Jessri, M.; Lou, W.Y.; L’Abbé, M.R. Evaluation of different methods to handle misreporting in obesity research: Evidence from the Canadian national nutrition survey. Br. J. Nutr. 2016, 115, 147–159. [Google Scholar] [CrossRef] [PubMed]
- Garriguet, D. Impact of identifying plausible respondents on the under-reporting of energy intake in the Canadian Community Health Survey. Health Rep. 2008, 19, 47–55. [Google Scholar] [PubMed]
- Guenther, P.M.; Casavale, K.O.; Reedy, J.; Kirkpatrick, S.I.; Hiza, H.A.B.; Kuczynski, K.J.; Kahle, L.L.; Krebs-Smith, S.M. Update of the Healthy Eating Index: HEI-2010. J. Acad. Nutr. Diet. 2013, 113, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Brisbois, T.D.; Marsden, S.L.; Anderson, G.H.; Sievenpiper, J.L. Estimated intakes and sources of total and added sugars in the Canadian diet. Nutrients 2014, 6, 1899–1912. [Google Scholar] [CrossRef] [PubMed]
- Jessri, M.; Lou, W.Y.; L’Abbé, M.R. The 2015 dietary guidelines for Americans is associated with a more nutrient-dense diet and a lower risk of obesity. Am. J. Clin. Nutr. 2016, 104, 1378–1392. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada. Canadian Community Health Survey—Nutrition (CCHS). Available online: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=7498 (assessed on 9 May 2017).
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Tooze, J.A.; Midthune, D.; Dodd, K.W.; Freedman, L.S.; Krebs-Smith, S.M.; Subar, A.F.; Guenther, P.M.; Carroll, R.J.; Kipnis, V. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J. Am. Diet. Assoc. 2006, 106, 1575–1587. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute. Usual Dietary Intakes: SAS Macros for the NCI Method. Available online: https://epi.grants.cancer.gov/diet/usualintakes/macros.html (assessed on 9 May 2017).
- Kipnis, V.; Midthune, D.; Buckman, D.W.; Dodd, K.W.; Guenther, P.M.; Krebs-Smith, S.M.; Subar, A.F.; Tooze, J.A.; Carroll, R.J.; Freedman, L.S. Modelling data with excess zeros and measurement error: Application to evaluating relationships between episodically consumed foods and health outcomes. Biometrics 2009, 65, 1003–1010. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Liu, T.; Kuklina, E.V.; Flanders, W.D.; Hong, Y.; Gillespie, C.; Chang, M.H.; Gwinn, M.; Dowling, N.; Khoury, M.J.; et al. Sodium and potassium intake and mortality among US adults: Prospective data from the Third National Health and Nutrition Examination Survey. Arch. Intern. Med. 2011, 171, 1183–1191. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.; Gray, A.R.; Fleming, E.A.; Parnell, W.R. Characteristics of fast-food/takeaway-food and restaurant/café-food consumers among New Zealand adults. Public Health Nutr. 2014, 17, 2368–2377. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Appel, L.J.; Sacco, R.L.; Anderson, C.A.M.; Antman, E.M.; Campbell, N.; Dunbar, S.B.; Frohlich, E.D.; Hall, J.E.; Jessup, M.; et al. Sodium, blood pressure, and cardiovascular disease. Circulation 2012, 126, 2880–2889. [Google Scholar] [CrossRef] [PubMed]
- Jessri, M.; Nishi, S.K.; L’Abbé, M.R. Assessing the nutritional quality of diets of Canadian adults using the 2014 health Canada surveillance tool tier system. Nutrients 2015, 7, 10447–10468. [Google Scholar] [CrossRef] [PubMed]
- Jessri, M.; Nishi, S.K.; L’Abbe, M.R. Assessing the nutritional quality of diets of Canadian children and adolescents using the 2014 Health Canada Surveillance Tool Tier System. BMC Public Health 2016, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Jessri, M.; L’Abbe, M.R. The time for an updated Canadian Food Guide has arrived. Appl. Physiol. Nutr. Metab. 2015, 40, 854–857. [Google Scholar] [CrossRef] [PubMed]
- Bailey, B.W.; Perkins, A.; Tucker, L.A.; LeCheminant, J.D.; Tucker, J.M.; Moncur, B. Adherence to the 2010 Dietary Guidelines for Americans and the relationship to adiposity in young women. J. Nutr. Educ. Behav. 2015, 47, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Jessri, M.; Wolfinger, R.D.; Lou, W.Y.; L’Abbé, M.R. Identification of dietary patterns associated with obesity in a nationally representative survey of Canadian adults: Application of a priori, hybrid, and simplified dietary pattern techniques. Am. J. Clin. Nutr. 2017, 105, 669–684. [Google Scholar] [CrossRef] [PubMed]
- Schoeller, D.A.; Bandini, L.G.; Dietz, W.H. Inaccuracies in self-reported intake identified by comparison with the doubly labelled water method. Can. J. Physiol. Pharmacol. 1990, 68, 941–949. [Google Scholar] [CrossRef] [PubMed]
- Schoeller, D.A. Limitations in the assessment of dietary energy intake by self-report. Metabolism 1995, 44, 18–22. [Google Scholar] [CrossRef]
- Subar, A.F.; Kipnis, V.; Troiano, R.P.; Midthune, D.; Schoeller, D.A.; Bingham, S.; Sharbaugh, C.O.; Trabulsi, J.; Runswick, S.; Ballard-Barbash, R.; et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: The OPEN study. Am. J. Epidemiol. 2003, 158, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, M.B.E.; Black, A.E. Markers of the validity of reported energy intake. J. Nutr. 2003, 133, 895S–920S. [Google Scholar]


| HEI-C 2010 Quartile Category | p-Trend 3 | ||||
|---|---|---|---|---|---|
| Characteristics | 1 (Least Healthy) | 2 | 3 | 4 (Healthiest) | |
| HEI-C 2010, range | <0.23 | 40.23–50.7 | 50.71–61.5 | 61.5≥ | |
| HEI-C 2010 score, mean | 31.22 ± 0.25 | 45.7 ± 0.1 | 55.9 ± 0.11 | 70.1 ± 0.23 | <0.0001 |
| Adequacy sub-score, mean | 19.07 ± 0.31 | 26.04 ± 0.27 | 32.13 ± 0.26 | 40.5 ± 0.29 | <0.0001 |
| Moderation sub-score, mean | 12.15 ± 0.26 | 19.66 ± 0.29 | 23.77 ± 0.25 | 29.6 ± 0.28 | <0.0001 |
| Female, % | 39.37 ± 3.06 | 46.99 ± 2.88 | 56.2 ± 2.31 | 57.69 ± 3.46 | <0.0001 |
| Age, years | 41.79 ± 0.45 | 45.63 ± 0.5 | 47.55 ± 0.49 | 49.01 ± 0.58 | <0.0001 |
| BMI, kg/m2 | 27.78 ± 0.21 | 27.64 ± 0.21 | 27.12 ± 0.25 | 27.06 ± 0.19 | 0.0451 |
| BMI category, % | 0.0104 | ||||
| Normal weight | 34.48 ± 1.64 | 35.95 ± 1.77 | 39.05 ± 1.61 | 39.45 ± 1.48 | |
| Obese | 26.78 ± 1.53 | 25.54 ± 1.35 | 23.1 ± 1.42 | 22.8 ± 1.22 | |
| Misreporting status, % | 0.0146 | ||||
| Under-reporters of energy intake | 33.75 ± 2.26 | 34.65 ± 2.3 | 31.7 ± 1.6 | 27.93 ± 1.79 | |
| Over-reporters of energy intake | 9.80 ± 1.04 | 9.44 ± 0.97 | 10.65 ± 0.8 | 12.48 ± 1.14 | |
| Physical activity, % | <0.0001 | ||||
| Low-active | 64.74 ± 1.53 | 62.12 ± 2.18 | 54.17 ± 1.95 | 51.02 ± 2.01 | |
| Active | 13.61 ± 0.91 | 15 ± 1.12 | 19.67 ± 1.23 | 21.74 ± 1.16 | |
| Smoking status, % | <0.0001 | ||||
| Current daily smokers | 33.64 ± 1.49 | 20.01 ± 1.23 | 17.74 ± 0.99 | 14.06 ± 1.11 | |
| Never smoked | 30.17 ± 1.64 | 46.55 ± 2.01 | 50.39 ± 1.69 | 57.25 ± 1.84 | |
| Multivitamin users, % | 40.29 ± 1.92 | 38.35 ± 1.77 | 46.22 ± 1.74 | 49.55 ± 1.9 | <0.0001 |
| Model | HEI-C 2010 Quartile Category | p-Trend 3 | ||||
|---|---|---|---|---|---|---|
| 1 (Unhealthy) | 2 | 3 | 4 (Healthiest) | |||
| HEI-C 2010 range | <40.23 | 40.23–50.7 | 50.71–61.5 | 61.5≥ | ||
| Energy intake, kcal/day | a | 2024 ± 56 | 2037 ± 48 | 2106 ± 44 | 2175 ± 43 | 0.0665 |
| b | 2401 ± 28 | 2431 ± 22 | 2462 ± 29 | 2450 ± 27 | 0.1641 | |
| Carbohydrate, % energy | a | 47.91 ± 0.46 | 48.91 ± 0.51 | 49.49 ± 0.44 | 49.9 ± 0.47 | 0.0198 |
| b | 47.36 ± 0.51 | 48.33 ± 0.47 | 49.01 ± 0.5 | 49.56 ± 0.55 | 0.0062 | |
| Fiber density, kcal/g | a | 6.22 ± 0.12 | 7.83 ± 0.16 | 9.51 ± 0.19 | 11.68 ± 0.25 | <0.0001 |
| b | 6.01 ± 0.12 | 7.6 ± 0.15 | 9.35 ± 0.19 | 11.58 ± 0.26 | <0.0001 | |
| Added sugar, % 4 | a | 13.66 ± 0.34 | 10.03 ± 0.31 | 8.39 ± 0.27 | 6.88 ± 0.23 | <0.0001 |
| b | 13.55 ± 0.35 | 9.93 ± 0.32 | 8.22 ± 0.29 | 6.68 ± 0.24 | <0.0001 | |
| Total fat, % energy | a | 31.86 ± 039 | 31.96 ± 0.46 | 31.25 ± 0.31 | 31.21 ± 0.36 | 0.4131 |
| b | 32.36 ± 0.4 | 32.5 ± 0.43 | 31.66 ± 0.35 | 31.45 ± 0.39 | 0.1488 | |
| Saturated fat, % energy | a | 11.67 ± 0.23 | 10.78 ± 0.19 | 9.75 ± 0.13 | 8.93 ± 0.12 | <0.0001 |
| b | 11.84 ± 0.22 | 10.96 ± 0.18 | 9.89 ± 0.14 | 9.01 ± 0.13 | <0.0001 | |
| Monounsaturated fatty acids, % energy | a | 12.41 ± 0.17 | 12.67 ± 0.23 | 12.58 ± 0.16 | 12.7 ± 0.2 | 0.633 |
| b | 12.65 ± 0.17 | 12.94 ± 0.21 | 12.78 ± 0.18 | 12.82 ± 0.21 | 0.7105 | |
| Polyunsaturated fatty acids, % energy | a | 4.87 ± 0.08 | 5.34 ± 0.1 | 5.76 ± 0.09 | 6.49 ± 0.12 | <0.0001 |
| b | 4.95 ± 0.1 | 5.24 ± 0.11 | 5.82 ± 0.1 | 6.52 ± 0.13 | <0.0001 | |
| Protein, % energy | a | 14.32 ± 0.21 | 16.32 ± 0.19 | 17.22 ± 0.29 | 17.66 ± 0.27 | <0.0001 |
| b | 14.29 ± 0.23 | 16.28 ± 0.21 | 17.25 ± 0.31 | 17.73 ± 0.29 | <0.0001 | |
| Alcohol, % energy | a | 5.91 ± 0.39 | 2.81 ± 0.22 | 2.03 ± 0.13 | 1.23 ± 0.1 | <0.0001 |
| b | 5.98 ± 0.43 | 2.89 ± 0.23 | 2.09 ± 0.17 | 1.26 ± 0.15 | <0.0001 | |
| Cholesterol density, mg/1000 kcal | a | 139.31 ± 4.03 | 150.34 ± 4.44 | 139.84 ± 4.6 | 128.66 ± 4.19 | 0.0044 |
| b | 139.17 ± 4.06 | 150.04 ± 4.57 | 140.31 ± 4.71 | 129.59 ± 4.63 | 0.0074 | |
| Calcium density, mg/1000 kcal | a | 377.18 ± 7.8 | 415.03 ± 6.97 | 436.63 ± 7.83 | 463.25 ± 7.86 | <0.0001 |
| b | 368.04 ± 7.75 | 405.42 ± 7.83 | 428.23 ± 8.1 | 456.98 ± 8.27 | <0.0001 | |
| Vitamin A density in RAE, μg/1000 kcal | a | 300.98 ± 10.56 | 348.54 ± 14.87 | 366.7 ± 10.68 | 448.83 ± 35.3 | <0.0001 |
| b | 291.82 ± 10.75 | 338.65 ± 15.5 | 359.35 ± 11.46 | 444.38 ± 31.59 | <0.0001 | |
| Vitamin D density, μg/1000 kcal | a | 2.29 ± 0.13 | 2.6 ± 0.08 | 2.98 ± 0.14 | 3.42 ± 0.17 | <0.0001 |
| b | 2.23 ± 0.16 | 2.64 ± 0.11 | 3.03 ± 0.18 | 3.46 ± 0.2 | <0.0001 | |
| Vitamin C density, mg/1000 kcal | a | 42.89 ± 1.8 | 59.35 ± 2.32 | 72.72 ± 2.43 | 82.56 ± 2.2 | <0.0001 |
| b | 40.01 ± 1.79 | 56.29 ± 2.16 | 70.23 ± 2.26 | 80.86 ± 2.3 | <0.0001 | |
| Sodium density, g/1000 kcal | a | 1588 ± 27 | 1594 ± 36 | 1560 ± 19 | 1448 ± 29 | 0.0012 |
| b | 1576 ± 27 | 1580 ± 38 | 1554 ± 22 | 1449 ± 30 | 0.0026 | |
| Naturally-occurring folate density, μg/1000 kcal 5 | a | 93.36 ± 2.72 | 109.5 ± 2.56 | 129.95 ± 2.93 | 147.8 ± 4.03 | <0.0001 |
| b | 89.54 ± 2.42 | 105.39 ± 2.31 | 126.83 ± 2.88 | 145.86 ± 3.96 | <0.0001 | |
| Folacin density from food sources, μg/1000 kcal 6 | a | 154.02 ± 3.41 | 176 ± 3.37 | 193.96 ± 3.22 | 198.06 ± 4.5 | <0.0001 |
| b | 150.63 ± 3.05 | 172.32 ± 3.06 | 191.27 ± 3.26 | 196.47 ± 4.72 | <0.0001 | |
| Phosphorus density, mg/1000 kcal | a | 565.97 ± 7.33 | 630.31 ± 6.09 | 685.43 ± 7.23 | 752.52 ± 8.83 | <0.0001 |
| b | 560.27 ± 7.43 | 623.95 ± 6.58 | 681.7 ± 7.75 | 751.17 ± 8.86 | <0.0001 | |
| Magnesium density, mg/1000 kcal | a | 137.24 ± 4.43 | 151.27 ± 1.72 | 173.57 ± 1.94 | 203.17 ± 3.21 | <0.0001 |
| b | 133.29 ± 3.97 | 146.95 ± 1.5 | 170.57 ± 1.89 | 201.53 ± 3.18 | <0.0001 | |
| Iron density, mg/1000 kcal | a | 6.21 ± 0.09 | 6.87 ± 0.08 | 7.29 ± 0.09 | 7.77 ± 0.1 | <0.0001 |
| b | 6.1 ± 0.09 | 6.75 ± 0.08 | 7.2 ± 0.09 | 7.72 ± 0.1 | <0.0001 | |
| Zinc density, mg/1000 kcal | a | 4.84 ± 0.08 | 5.5 ± 0.08 | 5.7 ± 0.08 | 6.124 ± 0.11 | <0.0001 |
| b | 4.81 ± 0.09 | 5.47 ± 0.09 | 5.7 ± 0.1 | 6.15 ± 0.12 | <0.0001 | |
| Potassium density, mg/1000 kcal | a | 1270 ± 17 | 1520 ± 28 | 1682 ± 19 | 1844 ± 24 | <0.0001 |
| b | 1236 ± 17 | 1482 ± 25 | 1656 ± 18 | 1831 ± 22 | <0.0001 | |
| Caffeine density, mg/1000 kcal | a | 166.19 ± 10.49 | 133.32 ± 5.08 | 124.91 ± 5.63 | 105.65 ± 4.83 | <0.0001 |
| b | 158.63 ± 9.77 | 124.93 ± 5.1 | 111.78 ± 5.53 | 103.56 ± 4.69 | <0.0001 | |
| Model | HEI-C 2010 Quartile Category | p-Trend 4 | ||||
|---|---|---|---|---|---|---|
| 1 (Unhealthy) | 2 | 3 | 4 (Healthiest) | |||
| HEI-C 2010, range | <40.23 | 40.23–50.7 | 50.71–61.5 | 61.5≥ | ||
| Total fruits and vegetables, (servings/day) | a | 3.08 ± 0.11 | 4.99 ± 0.17 | 6.1 ± 0.12 | 7.28 ± 0.18 | <0.0001 |
| b | 3.21 ± 0.13 | 5.13 ± 0.19 | 6.24 ± 0.17 | 7.42 ± 0.19 | <0.0001 | |
| Whole fruit, (servings/day) | a | 0.46 ± 0.12 | 1.05 ± 0.12 | 1.56 ± 0.1 | 2.25 ± 0.14 | <0.0001 |
| b | 0.46 ± 0.12 5 | 1.1 ± 0.29 | 1.6 ± 0.31 | 2.28 ± 0.31 | <0.0001 | |
| Greens and beans, (servings/day) | a | 0.17 ± 0.09 | 0.36 ± 0.08 | 0.64 ± 0.08 | 0.98 ± 0.07 | <0.0001 |
| b | 0.17 ± 0.09 5 | 0.36 ± 0.13 | 0.65 ± 0.14 | 0.98 ± 0.15 | <0.0001 | |
| Whole grains, (servings/day) | a | 0.07 ± 0.02 6 | 0.44 ± 0.14 | 0.95 ± 0.15 | 2.43 ± 0.12 | <0.0001 |
| b | 0.07 ± 0.02 6 | 0.39 ± 0.06 | 0.9 ± 0.07 | 2.38 ± 0.09 | <0.0001 | |
| Dairy, (servings/day) | a | 1.32 ± 0.09 | 1.62 ± 0.09 | 1.67 ± 0.1 | 1.77 ± 0.09 | <0.0001 |
| b | 1.28 ± 0.22 | 1.57 ± 0.23 | 1.63 ± 0.24 | 1.73 ± 0.23 | <0.0001 | |
| Total protein foods, (servings/day) | a | 1.86 ± 0.11 | 2.24 ± 0.11 | 2.37 ± 0.11 | 2.56 ± 0.1 | <0.0001 |
| b | 1.89 ± 0.25 | 2.27 ± 0.25 | 2.4 ± 0.25 | 2.59 ± 0.26 | <0.0001 | |
| Seafood and plant proteins, (servings/day) | a | 0.15 ± 0.07 | 0.28 ± 0.08 | 0.54 ± 0.07 | 0.98 ± 0.07 | <0.0001 |
| b | 0.15 ± 0.07 5 | 0.28 ± 0.08 5 | 0.54 ± 0.23 | 0.98 ± 0.23 | <0.0001 | |
| Fatty acids, ((PUFA + MUFA)/SFA) | a | 1.71 ± 0.06 | 1.88 ± 0.06 | 2.15 ± 0.07 | 2.38 ± 0.08 | <0.0001 |
| b | 1.7 ± 0.13 | 1.87 ± 0.14 | 2.14 ± 0.14 | 2.37 ± 0.14 | <0.0001 | |
| Refined grains, (servings/day) | a | 5.48 ± 0.2 | 5.64 ± 0.22 | 5.26 ± 0.2 | 3.54 ± 0.2 | <0.0001 |
| b | 5.64 ± 0.14 | 5.82 ± 0.14 | 5.44 ± 0.15 | 3.7 ± 0.18 | <0.0001 | |
| Sodium, (mg/day) | a | 3119 ± 47 | 3109 ± 50 | 3149 ± 45 | 2870 ± 75 | 0.0159 |
| b | 3109 ± 58 | 3098 ± 64 | 3139 ± 60 | 2861 ± 91 | 0.0162 | |
| Empty calories, (% energy) | a | 32.57 ± 0.46 | 18.39 ± 0.37 | 12.88 ± 0.31 | 9.11 ± 0.28 | <0.0001 |
| b | 32.38 ± 0.48 | 18.2 ± 0.43 | 12.66 ± 0.39 | 8.94 ± 0.35 | <0.0001 | |
| Components | Total Fruits and Vegetables | Whole Fruit | Greens and Beans | Whole Grains | Dairy | Total Protein Foods | Seafood and Plant Proteins | Refined Grains | Sodium | Empty Calories | Fatty Acids | Total HEI-C Score | Adequacy Score | Moderation Score | Energy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total fruits and vegetables | 1.00 | ||||||||||||||
| Whole fruit | 0.49 * | 1.00 | |||||||||||||
| Greens and beans | 0.27 * | 0.15 * | 1.00 | ||||||||||||
| Whole grains | 0.10 * | 0.16 * | 0.04 * | 1.00 | |||||||||||
| Dairy | 0.07 * | 0.08 * | 0.00 | 0.07 * | 1.00 | ||||||||||
| Total protein foods | 0.15 * | 0.01 | 0.22 * | 0.01 | 0.02 | 1.00 | |||||||||
| Seafood and plant proteins | 0.10 * | 0.13 * | 0.35 * | 0.09 * | −0.04 | 0.33 * | 1.00 | ||||||||
| Refined grains | 0.08 * | 0.13 * | 0.04 * | 0.84 * | 0.01 | −0.01 | 0.10 * | 1.00 | |||||||
| Sodium | −0.19 * | 0.01 | −0.08 * | −0.07 * | −0.29 * | −0.32 | −0.06 * | 0.10 * | 1.00 | ||||||
| Empty calories | 0.25 * | 0.23 * | 0.13 * | 0.16 * | 0.12 * | 0.09 * | 0.12 * | 0.13 * | 0.02 * | 1.00 | |||||
| Fatty acids | 0.08 * | 0.03 * | 0.13 * | 0.08 * | −0.35 * | 0.13 * | 0.26 * | 0.05 * | 0.00 | 0.12 * | 1.00 | ||||
| Total HEI-C score | 0.49 * | 0.48 * | 0.37 * | 0.59 * | 0.19 * | 0.21 * | 0.39 * | 0.59 * | 0.09 * | 0.68 * | 0.31 * | 1.00 | |||
| Adequacy score | 0.62 * | 0.53 * | 0.49 * | 0.50 * | 0.32 * | 0.38 * | 0.50 * | 0.39 * | −0.27 * | 0.34 * | 0.37 * | 0.83 * | 1.00 | ||
| Moderation score | 0.14 * | 0.22 * | 0.07 * | 0.46 * | −0.03 * | −0.07 * | 0.10 * | 0.57 * | 0.46 * | 0.78 * | 0.11 * | 0.78 * | 0.30 * | 1.00 | |
| Energy | 0.26 * | 0.04 * | 0.10 * | 0.06 * | 0.34 * | 0.39 * | 0.09 * | −0.12 * | −0.67 * | −0.13 * | 0.03 * | −0.01 | 0.36 * | −0.42 * | 1.00 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jessri, M.; Ng, A.P.; L’Abbé, M.R. Adapting the Healthy Eating Index 2010 for the Canadian Population: Evidence from the Canadian Community Health Survey. Nutrients 2017, 9, 910. https://doi.org/10.3390/nu9080910
Jessri M, Ng AP, L’Abbé MR. Adapting the Healthy Eating Index 2010 for the Canadian Population: Evidence from the Canadian Community Health Survey. Nutrients. 2017; 9(8):910. https://doi.org/10.3390/nu9080910
Chicago/Turabian StyleJessri, Mahsa, Alena Praneet Ng, and Mary R. L’Abbé. 2017. "Adapting the Healthy Eating Index 2010 for the Canadian Population: Evidence from the Canadian Community Health Survey" Nutrients 9, no. 8: 910. https://doi.org/10.3390/nu9080910
APA StyleJessri, M., Ng, A. P., & L’Abbé, M. R. (2017). Adapting the Healthy Eating Index 2010 for the Canadian Population: Evidence from the Canadian Community Health Survey. Nutrients, 9(8), 910. https://doi.org/10.3390/nu9080910






