Eliminating Iodine Deficiency in China: Achievements, Challenges and Global Implications
Abstract
:1. Introduction
2. The Chinese Iodine Deficiency Disorder Elimination Programme
3. Achievements of the Programme
4. Challenges of the Programme
4.1. Achieving Optimal Iodine Nutrition for Both Women and Children through Salt Iodization
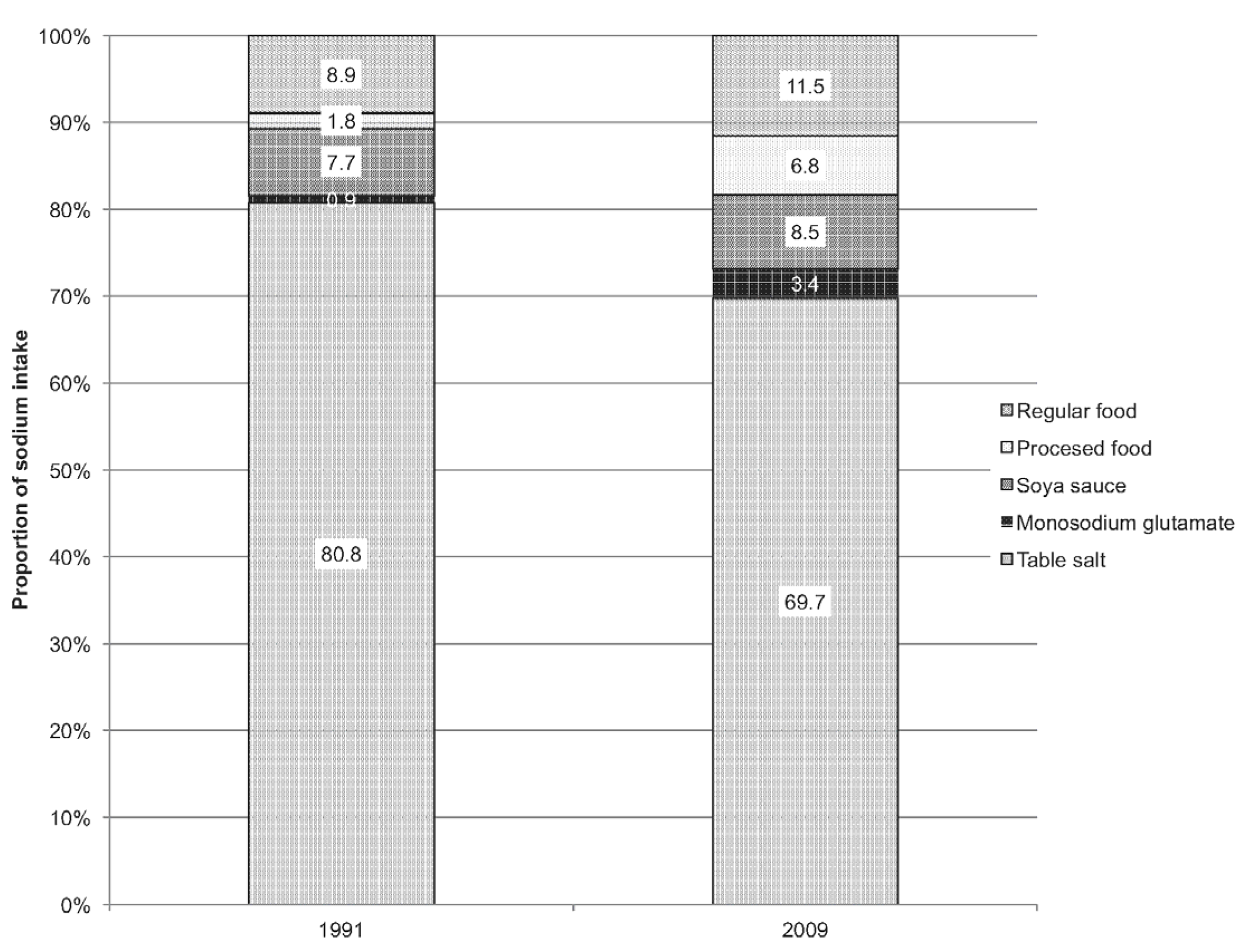
4.2. The Contribution of Processed Foods to Salt and Iodine Intake
4.3. Addressing the Problem of High Water Iodine Areas
4.4. Ensuring High Coverage of Adequately Iodized Salt in All Provinces
5. Implications for IDD Elimination Program Globally
5.1. Is It Possible for Salt Iodization to Ensure Adequate Iodine Intake in Pregnant Women without Causing Excess in School-Age Children?
5.2. Does Salt Used in Food Processing Need to Be Iodized in Order to Ensure Adequate Iodine Intakes in the General Population?
5.3. To What Extent Is Water an Important Source of Iodine and in What Conditions Is Iodized Salt Contraindicated?
5.4. Extrapolating China’s Lessons Learned on Monitoring the Status and Impact of Salt Iodization and IDD Elimination Efforts
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization; The United Nations Children’s Fund; The International Council for Control of Iodine Deficiency Disorders. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers, 2nd ed.; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Delange, F. The disorders induced by thyroid deficiency. Thyroid 1994, 4, 107–128. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, M.B.; Jooste, P.J.; Pandav, C.S. Iodine deficiency disorders. Lancet 2008, 372, 1251–1262. [Google Scholar] [CrossRef]
- World Health Organization. Micronutrient Deficiencies: Iodine Deficiency Disorders. Available online: http://www.who.int/nutrition/topics/idd/en/ (accessed on 1 February 2017).
- Qian, M.; Wang, D.; Watkins, W.; Gebski, V.; Yan, Y.Q.; Li, M.; Chen, Z. The effects of iodine on intelligence in children: A meta-analysis of studies conducted in China. Asia Pac. J. Clin. Nutr. 2005, 14, 32–42. [Google Scholar] [PubMed]
- Hynes, K.L.; Otahal, P.; Hay, I.; Burgess, J. Mild iodine deficiency during pregnancy is associated with reduction educational outcomes in the offspring: 9-year follow-up of the gestational iodine cohort. J. Clin. Endocrinol. Metab. 2013, 98, 1954–1962. [Google Scholar] [CrossRef] [PubMed]
- Bath, S.C.; Steer, C.D.; Golding, J.; Emmett, P.; Rayman, M.P. Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: Results from Avon Longitudinal Study of Parents and Children (ALSPC). Lancet 2013, 382, 331–337. [Google Scholar] [CrossRef]
- Universal Salt Iodization: Global Progress and Public Health Success Stories to Address IDD through USI, Key Programme Components, Lessons Learned at Country Level, and the Way Forward to Reach USI Globally. Available online: http://www.unsystem.org/scn/Publications/SCNNews/scnnews35.pdf (accessed on 1 February 2017).
- Laurberg, P.; Bulow Pedersen, I. Environmental iodine intake affects the nonmalignant thyroid disease. Thyroid 2001, 11, 457–469. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Guideline: Fortification of Food-Grade Salt with Iodine for the Prevention and Control of Iodine Deficiency Disorders; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- UNICEF. Fortifying our Future: A Snapshot Report on Food Fortification. September 2015. Available online: http://www.gainhealth.org/wp-content/uploads/2015/05/Fortifying-our-Future-A-SnapShot-Report-on-Food-Fortification1.pdf (accessed on 1 February 2017).
- Iodine Global Network. Legislation Database. Available online: http://www.ign.org/cm_data/Salt11X14.png (accessed on 30 January 2017).
- UNICEF. State of the World’s Children 2015. Available online: http://data.unicef.org/corecode/uploads/document6/uploaded_pdfs/corecode/SOWC_2015_Summary_and_Tables_210.pdf (accessed on 1 February 2017).
- Iodine Global Network. Global Scorecard 2016: Moving toward Optimal Iodine Status. Available online: http://www.ign.org/newsletter/idd_nov16_global_scorecard_2016.pdf (accessed on 1 February 2017).
- Abuto, N.J.; Abudou, M.; Candeias, V.; Wu, T. Effect and Safety of Salt Iodization to Prevent Iodine Deficiency Disorders: A Systematic Review with Meta-Analysis; WHO eLibrary of Evidence for Nutrition Actions; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Horton, S.; Mannar, V.; Wesley, A. Best Practice Paper: Micronutrient Fortification (Iron and Salt Iodization); Copenhagen Consensus: Copenhagen, Denmark, 2008. [Google Scholar]
- Wang, J.; Harris, M.; Amos, B.; Li, M.; Wang, X.; Zhang, J.; Chen, J. A ten year review of the Iodine Deficiency Disorders Program of the People’s Republic of China. J. Public Health Policy 1997, 18, 219–241. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y. Survey on iodine nutritional status of school-aged children in 10 cities in China. Chin. J. Control Endem. Dis. 1995, 10, 326–329. [Google Scholar]
- Chen, Z.; Dong, Z.; Lin, J. Achieving, and sustaining USI: Effective program development and management. Lessons learned from USI in China. SCN News 2007, 35, 33–36. [Google Scholar]
- Wang, L.; Qi, X.; Bai, H.; Sun, D. Meet the Challenge (To Commemorate the 10th Anniversary of Universal Salt Iodization, 1996–2006); Bureau of Disease Prevention and Control, Ministry of Health, People’ Republic of China: Beijing, China, 2006.
- The United Nations Children's Fund. Review of National Legislation for Universal Salt Iodization: South and East Asia and the Pacific; UNICEF East Asia and Pacific Regional Office: Geneva, Switzerland, 2015. [Google Scholar]
- Zheng, Q.; Xu, J.; Dong, H.; Wang, H.; Li, S.; Chen, Z. China IDD surveillance system and its role in the prevention and control of IDDs. Chin. J. Dis. Control Prev. 2010, 25, 428–430. (In Chinese) [Google Scholar]
- The Chinese Center for Disease Control and Prevention. Assessment Scheme for the Stage Goal Achievement of IDD Elimination (No. 58); CCDC: Beijing, China, 1999. (In Chinese)
- The State Council of the People’s Republic of China. Control Iodized Salt Management Regulations for IDD (No. 163); SCPRC: Beijing, China, 1994. (In Chinese)
- The State Council of the People’s Republic of China. The Salt Industry Management Regulations of the People’s Republic of China (No. 51); SCPRC: Beijing, China, 1990. (In Chinese)
- World Bank Operations Evaluation Department. An Analysis of Combating Iodine Deficiency: Case Studies of China, Indonesia, and Madagascar; OED Working Paper Series No. 18; The World Bank: Washington, DC, USA, 2001.
- Ministry of Health. GB14880-94 Hygienic Standard for the Use of Nutritional Fortification Substances in Foods. Available online: http://www.msckobe.com/links/food/gb14880_1994.pdf (accessed on 29 March 2017).
- Duan, D.; Chen, J.; Li, Z.; Xu, H. China IDD Surveillance in 1995; People’s Medical Publishing House: Beijing, China, July 1999. (In Chinese) [Google Scholar]
- Ministry of Health. GB 4561-2000 Edible Salt National Standards; National Environmental Protection Bureau: Beijing, China.
- Ministry of Health. GB 26878-2011: National Standard on Food Safety—Iodine Content of Edible Salt. Available online: http://www.shfda.gov.cn/spaqbz/GB26878-2011%20食用盐碘含量.pdf. (accessed on 1 February 2017).
- Sun, D.; Xiao, D.; Liu, S. The Monitoring of Iodine Deficiency Disorders of China in 2011; People’s Medical Publishing House: Beijing, China, 2011. [Google Scholar]
- Codling, K.; Rudert, C. Putting East Asia Back on Track towards Sustainable USI. IDD Newsletter. Available online: http://www.ign.org/newsletter/idd_aug16_east_asia_1.pdf (accessed on 1 February 2017).
- 735 Villages and Towns of 109 Counties Are High Water Iodine Areas in China. Available online: http://www.gov.cn/jrzg/2012-10/29/content_2252858.htm (accessed on 1 February 2017). (In Chinese).
- General Office of the Ministry of Health; General Office of the Ministry of Industry and Information Technology; The Chinese Center for Disease Control and Prevention. Notice on Further to Do Non-Iodized Salt Supply and Management Better (No.168); GOMH; GOMIIT; CCDC: Beijing, China, 2009. (In Chinese)
- Liu, P.; Liu, L.; Shen, H.; Jia, Q.; Wang, J.; Zheng, H.; Ma, J.; Zhou, D.; Liu, S.; Su, X. The standard intervention measures and health risk for high water iodine areas. PLoS ONE 2014, 9, e89608. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Su, X.; Yu, J.; Zhang, S.; Liu, P.; Ji, X.; Liu, S.; Sun, D. Analysis of field survey results for iodine deficiency disorders in high-risk areas of China. Chin. J. Endemiol. 2009, 2, 197–201. (In Chinese) [Google Scholar]
- Wu, Y.; Li, X.; Chang, S.; Liu, L.; Zou, S.; Hipgrave, D. Variable iodine intake persists in the context of universal salt iodization in China. J. Nutr. 2012. [Google Scholar] [CrossRef] [PubMed]
- Pandav, C.; Yadav, K.; Lakshmy, R.; Pandey, R.M.; Salve, H.R.; Chakrabarty, A.; Knowles, J.; Sankar, S.; Rah, J.H.; Ansari, M.A. Across India, Women Are Iodine Sufficient. Excerpt from National Iodine and Salt Intake Survey (NISI) 2014–2015: Executive Summary. Available online: http://www.ign.org/idd-newsletter-42015.htm (accessed on 1 February 2017).
- The World Bank. Repositioning Nutrition as Central to Development: A Strategy for Large Scale Action; The World Bank: Washington, DC, USA, 2006. [Google Scholar]
- The World Bank. Memorandum and Recommendation of the President of the International Bank for Reconstruction and Development and the International Development Association to the Executive Directors on a Proposed Loan in an Amount Equivalent to $7.0 Million and a Proposed Credit of SDR 12.7 Million to the People’s Republic of China for an Iodine Deficiency Disorders Control Project. 6 June 1995. Available online: http://documents.worldbank.org/curated/en/422711468261342795/text/multi0page.txt (accessed on 1 February 2017).
- Chang, S.; United Nations Children’s Fund, Beijing, China. Personal communication, 2017.
- Sun, D.; Shen, H. National Key Endemic Disease Monitoring (1990–2006); Beijing People’s Medical Publishing House: Beijing, China, 2009; pp. 118–144. (In Chinese) [Google Scholar]
- Shen, H. China iodine deficiency or excess hazard prevention and control situation and the countermeasures. Chin. J. Endemiol. 2012, 31, 239–240. (In Chinese) [Google Scholar]
- Sun, D.J.; Centre for Endemic Disease Control, Heilongjiang, China. Personal commuication, 2017.
- World Health Organization (WHO). Urinary Iodine Concentrations for Determining Iodine Status Deficiency in Populations. Vitamin and Mineral Nutrition Information System; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Zimmermann, M.B.; Aeberli, I.; Andersson, M.; Assey, V.; Yorg, J.A.; Jooste, P.; Jukić, T.; Kartono, D.; Kusić, Z.; Pretell, E.; et al. Thyroglobulin is a sensitive measure of both deficient and excess iodine intakes in children and indicates no adverse effects on thyroid function in the UIC range of 100–299 μg/L: A UNICEF/ICCIDD Study Group report. J. Clin. Endocrinol. Metab. 2013, 98, 1271–1280. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Higuchi, T.; Sawa, K.; Ohtaki, S.; Horiuchi, Y. “Endemic coast goitre” in Hokkaido, Japan. Acta Endocrinol. 1965, 50, 161–176. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Liu, D.R.; Qu, C.Y.; Zhang, P.Y.; Qian, Q.D.; Zhang, C.D.; Jia, Q.Z.; Wang, H.X.; Eastman, C.J.; Boyages, S.C. Endemic goitre in central China caused by excessive iodine intake. Lancet 1987, 2, 257–259. [Google Scholar] [PubMed]
- Zhao, J.; Chen, Z.; Maberly, G. Iodine-rich drinking water of natural origin in China. Lancet 1998, 352, 2024. [Google Scholar] [CrossRef]
- Li, W.H.; Dong, B.S.; Li, P.; Li, Y.F. Benefits and risks from the national strategy for improvement of iodine nutrition: A community-based epidemiologic survey in Chinese schoolchildren. Nutrition 2012, 28, 1142–1145. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Ito, Y.; Hess, S.Y.; Fujieda, K.; Molinari, L. High thyroid volume in children with excess dietary iodine intakes. Am. J. Clin. Nutr. 2005, 81, 840–844. [Google Scholar] [PubMed]
- Chen, W.; Li, X.; Wu, Y.; Bian, J.; Shen, J.; Jiang, W.; Tan, L.; Wang, X.; Wang, W.; Pearce, E.N.; et al. Associations between iodine intake, thyroid volume, and goiter rate in school-aged children from areas with high iodine drinking water concentrations. Am. J. Clin. Nutr. 2017, 105, 228–233. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2 years: Conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007, 10, 1606–1611. [Google Scholar]
- Xu, J.; Wang, J.-Q.; Zheng, Q.-S.; Gu, Y.-Y.; Wang, H.-Y.; Li, X.-W. Analysis of monitoring results of Chinese iodized salt surveillance in 2010. Chin. J. Endemiol. 2012, 5, 552–555. (In Chinese) [Google Scholar]
- Ghassabian, A.; Steenweg-de Graaff, J.; Peeters, R.P.; Ross, H.A.; Jaddoe, V.W.; Hofman, A.; VerHULST, F.C.; White, T.; Tiermeier, H.; et al. Maternal urinary iodine concentration in pregnancy and children’s cognition: Results from a population-based birth cohort in an iodine-sufficient area. BMJ Open 2014, 4, e005520. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Han, C.; Li, C.; Mao, J.; Wang, W.; Xie, X.; Li, C.; Xu, B.; Meng, T.; Du, J.; et al. Optimal and safe upper limits of iodine intake for early pregnancy in iodine sufficient regions: A cross-sectional study of 7190 pregnant women in China. J. Clin. Endocrinol. Metab. 2014. [Google Scholar] [CrossRef] [PubMed]
- Cui, J. Investigation report on iodized salt in China’s food processing industry. Chin. Salt Indus. 2012, 6, 11–14. [Google Scholar]
- Du, S.; Batis, C.; Wang, H.; Zhang, B.; Zhang, J.; Popkin, B.M. Understanding the patterns and trends of sodium intake, potassium intake and sodium to potassium ratio and their effect on hypertension in China. AJCN 2014, 99, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Hipgrave, D.; Chang, S.; Li, X.; Wu, Y. Salt and sodium intake in China. JAMA 2016, 315, 703–705. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.; Liu, S.; Sun, D.; Zhang, S.; Su, X.; Shen, Y.; Han, H. Geographical distribution of drinking water with high iodine level and association between high iodine level in drinking water and goitre: A Chinese national investigation. Br. J. Nutr. 2011, 106, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Wang, P.; Shang, L.; Sullivan, K.M.F.; Maberly, G. Endemic goitre associated with high iodine intake. Am. J. Public Health 2000, 90, 1633–1635. [Google Scholar] [PubMed]
- Lv, S.; Zhao, J.; Xu, D.; Rutherford, S. An epidemiological survey of children’s iodine nutrition and goitre status in regions with mildly excess iodine in drinking water in Hebei province, China. Public Health Nutr. 2012, 15, 1168–1173. [Google Scholar] [CrossRef] [PubMed]
- Lv, S.; Xu, D.; Wang, Y.; Chong, Z.; Du, Y.; Jia, L.; Zhao, J.; Ma, J. Goitre prevalence and epidemiological features in children living in areas with mildly excessive iodine in drinking water. Br. J. Nutr. 2014, 11, 86092. [Google Scholar] [CrossRef] [PubMed]
- Sui, H.; Li, J.W.; Mao, W.F.; Zhu, J.H.; He, Y.N.; Song, Y.; Ma, N.; Zhang, L.; Liu, S.N.; Liu, P.; et al. Dietary iodine intake in the Chinese population. Biomed. Environ. Sci. 2011, 24, 617–623. [Google Scholar] [PubMed]
- Liu, H.L.; Lam, L.T.; Zeng, Q.; Han, S.Q.; Fu, G.; Hou, C.C. Effects of drinking water with high iodine concentration on the intelligence of children in Tianjin, China. J. Public Nutr. 2008, 31, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Sang, Z.; Tan, L.; Zhang, S.; Dong, F.; Chu, Z.; Wei, W.; Zhao, N.; Zhang, G.; Yao, Z.; et al. Neonatal thyroid function born to mothers living with long-term excessive iodine intake from drinking water. Clin. Endocrinol. 2015, 83, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Lv, S.; Xu, D.; Wang, Y.; Jun, Z.; Jia, L.; Du, Y. Impact of removing iodized salt on children’s goitre status in areas with excessive iodine in drinking water. Br. J. Nutr. 2015, 113, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Hou, C.; Fu, G.; Zeng, Q.; Liu, H. Studies on the effect of changing water in high water-iodine area in Tianjin. Chin. J. Control Endem. Dis. 2010, 25, 444–450. (In Chinese) [Google Scholar]
- Wang, M.; Li, H.; Wang, M.; Li, J.; Li, X.; Li, J. Survey on the Residents’ Iodine Level in High Iodine Area after Taking Low Iodine Water in Shouguang City, 2009. Prev. Med. Tribune 2010, 16, 1010–1011. [Google Scholar]
- Wang, P.; Zhang, Q.; Shang, L.; Fei, Y.; Liu, C.; Chen, Y.; Liang, P. Children goiter rate change analysis before and after water source change in high water iodine area. Prim. Health Care 2005, 12, 61–62. (In Chinese) [Google Scholar]
- National Standards of People’s Republic of China. Standards for Drinking Water Quality. GB5749-2006. Available online: http://www.steriq.cn/pdf/34.pdf (accessed on 1 February 2017).
- Nima, C.; Gong, H.; Guo, M.; He, F.; Zhao, S.; Deji, Y. Tibet autonomous region iodized salt monitoring result analysis in 2011–2013. Tibet. J. Med. 2014, 4, 44–45. (In Chinese) [Google Scholar]
- Wang, F.; Li, X.; Ma, L.; PA, L.; Yi, L.; Ye, E.; Gu, L.; Mai, L; Hai, X.; Xu, Y. Distribution of non-iodized salt and related affecting factors in Xinjiang. Chin. J. Epidemiol. 2002, 23, 258–261. (In Chinese) [Google Scholar]
- Wang, Z.; Li, Y.; Xiong, C.; Zhou, Li. Qinghai province IDD prevention and treatment monitoring results and analysis in 1995. Bull. Dis. Control Prev. 1996, 11, 107–108. (In Chinese) [Google Scholar]
- Wang, H.; Su, Y.; Wu, L.; Yi, C. Iodized salt monitoring result analysis of Hainan province in 2004–2011. Chin. J. Endemiol. 2013, 32, 284–287. (In Chinese) [Google Scholar]
- Teng, W.; Shan, Z.; Teng, X.; Guan, H.; Li, Y.; Teng, D.; Jin, Y.; Yu, X.; Fan, C.; Chong, W.; et al. Effect of iodine intake on thyroid diseases in China. NEJM 2006, 354, 2783–2793. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Teng, W.; Shan, Z.; Guan, H.; Li, Y.; Jin, Y.; Hu, F.; Shi, X.; Tong, Y.; Chen, W.; et al. Epidemiological survey on the relationship between different iodine intakes and the prevalence of hyperthyroidism. Eur. J. Endocrinol. 2002, 146, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Teng, X.; Shan, Z.; Chen, Y.; Lai, Y.; Yu, J.; Shan, L.; Bai, X.; Li, Y.; Li, N.; Li, Z.; et al. More than adequate iodine intake may increase subclinical hypothyroidism and autoimmune thyroiditis: A cross sectional study based on two Chinese communities with different iodine intakes. Eur. J. Endocrinol. 2011, 164, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Shan, Z.; Chen, L.; Lian, X.; Liu, C.; Shi, B.; Shi, L.; Tong, N.; Wang, S.; Weng, J.; Zhao, J.; Teng, X.; et al. Iodine Status and Prevalence of Thyroid Disorders After Introduction of Mandatory Universal Salt Iodization for 16 Years in China: A Cross-Sectional Study in 10 Cities. Thyroid 2016, 26, 1125–1130. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Li, F.; Liu, Z.; He, Y.; Sui, H.; Mao, W.; Liu, S.; Yan, Y.; Li, N.; Chen, J. Assessment of Dietary Iodine Intake of Population in Non High-Iodine Areas in China. Available online: https://www.ncbi.nlm.nih.gov/m/pubmed/21560295/?i=1&from=liu,%20zhaoping,%20iodine (accessesd on 1 February 2017).
- Chen, J. The Assessment of iodine status in Chinese residents. In Proceedings of the 2016 Iodine and Thyroid Disease Conference, Harbin, China, 19–20 October 2016. [Google Scholar]
- Pearce, E. Can USI achieve optimal iodine in all population groups: Preliminary results of SIMPLIFY: Salt Iodization: Meeting the needs of Pregnancy, Lactation and InFancY. A joint ETH/GAIN/UNICEF study. In Proceedings of the 2016 Iodine and Thyroid Disease Conference, Harbin, China, 19–20 October 2016. [Google Scholar]
- Sang, Z.; Peizhong, P. Exploration of the safe upper level of iodine intake in euthryroid Chinese adults: A randomized double-blind trial. Am. J. Clin. Nutr. 2011. [Google Scholar] [CrossRef]
- Ares, S.; Saenz-Rico, B.; Quero, J.; Morreale de Escobar, G. Chapter 30. Iodine and the effects on growth in premature newborns: A focus on the role of thyroid hormones in neurodevelopment and growth. In Handbook of Growth and Growth Monitoring in Health and Disease; Preedy, V.R., Ed.; Springer Science & Business Media: New York, NY, USA, 2012. [Google Scholar]
- Khan, N. Elimination of Iodine Deficiency in FIJI. IDD Newsletter. November 2009. Available online: http://www.ign.org/newsletter/idd_nl_nov09_fiji.pdf (accessed on 1 February 2017).
- Health Research Institute; Ministry of Health. Basic Health Research (RISKESDAS) 2013. Available online: http://www.depkes.go.id/resources/download/general/Hasil%20Riskesdas%202013.pdf (accessed on 1 February 2017).
- Mongolia Ministry of Health. Fourth National Nutrition Survey 2010 (Nutritional Status of Mongolian Population). Available online: http://ncph.gov.mn/userfiles/NNS%20IV%20last%20approved_eng.pdf. (accessed on 29 March 2017).
- Australia Institute of Health and Welfare. Monitoring the Health Impacts of Mandatory Folic Acid and Iodine Fortification. 2016. Available online: http://www.aihw.gov.au/publication-detail/?id=60129555435 (accessed on 1 February 2017).
- Skeaff, S.; Lonsdale-Cooper, E. Mandatory fortification of bread with iodized salt modestly improves iodine status in schoolchildren. BJN 2013, 109, 1109–1113. [Google Scholar] [CrossRef] [PubMed]
- Brough, L.; Jin, Y.; Shukri, N.H.; Wharemate, Z.R.; Weber, J.L.; Coad, J. Iodine intake and status during pregnancy and lactation before and after government initiatives to improve iodine status, in Palmerston North, New Zealand: A pilot study. Matern. Child Nutr. 2015, 11, 646–655. [Google Scholar] [CrossRef] [PubMed]
- Philippines Food and Nutrition Research Institute. National Nutrition Survey 2013. Available online: http://www.fnri.dost.gov.ph/images/sources/Iodine.pdf (accessed on 1 February 2017).
- Wong, E.M.; Sullivan, K.M.; Perrine, C.G.; Rogers, L.M.; Pena-Rosas, J.P. Comparison of median urinary iodine concentrations as an indicator of iodine status among pregnant women, school-age children, and non-pregnant women. Food Nutr. Bull. 2011, 32, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Gorstein, J.; University of Washington, Seattle, WA, USA; Zimmerman, M.; Swiss Federal Insitue of Technoclogy (ETH), Zurich, Switzerland. Personal communication. 5 November 2014. [Google Scholar]
- Rogers, L.M. WHO evidence and guidance for salt iodization & salt reduction. In Proceedings of the Achieving Universal Salt Iodization for Optimal Iodine Nutrition in the East Asia and Pacific Region, Bangkok, Thailand, 12–14 October 2015. [Google Scholar]
- Chang, S.; United Nations Children’s Fund, Beijing, China. Personal communication, 2016.
- Sun, D.J.; Centre for Endemic Disease Control, Heilongjiang, China. Personal communication, 2016.
- National Health and Medical Research Council Public Statement, Iodine Supplementation for Pregnant and Breastfeeding Women. January 2010. Available online: https://www.nhmrc.gov.au/guidelines-publications/new45 (accessed on 1 February 2017).
- Ministry of Health. Iodine Question and Answers. Available online: http://www.health.govt.nz/our-work/preventative-health-wellness/nutrition/iodine#iodine_supplements (accessed on 1 February 2017).
- Alexander, E.K.; Pearce, N.E.; Brent, G.A.; Brown, R.S.; Chen, H.; Dosiou, C.; Grobman, W.A; Lauberg, P.; Lazarus, J.H.; Mandel, S.J.; et al. 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease during Pregnancy and Postpartum. Thyroid 2016. [Google Scholar] [CrossRef] [PubMed]
- Notifications of the Thai Ministry of Public Health. Royal Gazette Book 127, Special Part 115, 1 October, B.E.2553 (2010) on Fish Sauce, Saline Seasoning and Seasoning from Fermented Soy Protein; Ministry of Public Health: Nonthaburi, Thailand, 2010.
- Sangsom, S.; Iodine Global Network, Bangkok, Thailand. Personal communication, 2015.
- Rajata, R.; Ministry of Public Health, Nonthaburi, Thailand. Personal communication, 2015.
- Ministry of Health & National Agency of Drug and Food Control, Indonesia, Clarity & GAIN. Usage of Iodized Salt in the Processed Food in Indonesia Industry. Available online: http://www.gainhealth.org/wp-content/uploads/2017/03/Final-Clarity-Salt-Report-March-2017.pdf (accessed on 29 March 2017).
- Nutrition Centre of the Philippines for GAIN. Survey of Food Processors Utilizing Iodized Salt and Salt Repackers. Available online: http://www.gainhealth.org/wp-content/uploads/2017/04/Survey-of-Food-Processors-Utilizing-Iodized-Salt-June-2015.pdf (accessed on 3 April 2017).
- The Health and Stroke Foundation; South Africa. Salt is killing South Africans and It Is Time to Take Action. Available online: http://www.heartfoundation.co.za/media-releases/salt-killing-south-africans-and-it-time-take-action (accessed on 1 February 2017).
- American Heart Association. Where Is All That Salt Coming From? Available online: http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyEating/Processed-Foods-Where-is-all-that-salt-coming-from_UCM_426950_Article.jsp (accessed on 1 February 2017).
- Ni Mhurchu, C.; Capelin, C.; Dunford, E.K.; Webster, J.L.; Neal, B.C.; Jebb, S.A. Sodium content of processed foods in the United Kingdom: Analysis of 44,000 foods purchased by 21,000 households. AJCN 2011, 93, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Szybinski, Z.; Delange, F.; Lewinski, A.; Podoba, J.; Rybakowa, M.; Wasik, R.; Szewczyk, L.; Huszno, B.; Golkowski, F.; Przybylik-Mazurek, E.; et al. A program of iodine supplementation using only iodized household salt is efficient—the case of Poland. Eur. J. Endocrinol. 2001, 144, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Jayatissa, R.; Gunathilaka, M. Third National Survey on Iodine Deficiency Status in Sri Lanka—2010. Available online: http://www.ign.org/cm_data/2017_Sri_Lanka.pdf (accessed on 3 April 2017).
- Centre for Applied Health Technology and Clinical Epidemiology; Indonesia Ministry of Health; UNICEF. Effect of Excess Iodine Intakes on Thyroid Function among School Children: Multicenter Study. Available online: http://www.ign.org/cm_data/2017_Indonesia_Multi-Center_study_report_final_report_version_2.pdf (accessed on 3 April 2017).
- Kassim, I.A.; Moloney, G.; Busili, A.; Nur, A.Y.; Paron, P.; Jooste, P.; Gadain, H.; Seal, A.J. Iodine intake in Somalia is excessive and associated with the source of household drinking water. J. Nutr. 2014, 144, 375–381. [Google Scholar] [CrossRef] [PubMed]
| Phase 1: 1993–1995 |
| Basic access of iodized salt across the country |
| (i) 75% national coverage of iodized salt |
| (ii) 85% coverage of iodized oil capsules among vulnerable groups in iodine-deficient areas |
| (iii) 50% of counties meet criteria to eliminate IDD |
| Phase 2: 1996–2000 |
| IDD eliminated at the national level: national coverage of iodized salt increased to 95% |
| Phase 3: 2001–2010 |
| IDD eliminated in all provinces and 95% of counties |
| Phase 4: 2010–2015 |
| Sustainably eliminate IDD |
| (i) above 90% of counties in Hainan, Tibet, Qinghai and Xinjiang eliminate IDD |
| (ii) 95% of counties in other provinces maintain IDD elimination |
| (iii) prevention of new cases of cretinism |
| (iv) maintain iodine nutrition of general population at adequate level |
| Categorization | Criteria |
|---|---|
| Yet to eliminate IDD | ● <90% coverage adequately iodized salt |
| OR | |
| ● MUIC of school-age children <100 μg/L | |
| Almost eliminated IDD | ● >90% coverage adequately iodized salt |
| ● >95% coverage iodized salt | |
| ● MUIC of school-age children >100 μg/L | |
| ● Goiter rate of school children <20% | |
| Eliminated IDD | ● >90% coverage adequately iodized salt |
| ● >95% coverage iodized salt | |
| ● MUIC of school-age children >100 μg/L | |
| ● Goiter rate of school children <10% |
| 2005 National IDD Survey [42] | 2011 National IDD Survey [31] | 2010 End-Line Evaluation [44] | |
|---|---|---|---|
| Global Targets for Sustainable IDD Elimination | |||
| >90% household use of salt with iodine content 15–40 ppm | 90.2% | 95.3% | |
| MUIC in general population 100–199 μg/L | 246 μg/L | 239 μg/L | |
| MUIC in pregnant women 150–249 μg/L | 184 μg/L | ||
| China National IDD Elimination Programme Targets | |||
| All provinces eliminated IDD | 28 out of 31 | ||
| 95% of counties eliminated IDD | 98% | ||
| Pregnant Women: <150 μg/L | Pregnant Women: 150–249 μg/L | Pregnant Women: ≥250 μg/L | No. of Provinces | |
|---|---|---|---|---|
| School age children: <100 μg/L | 0 | |||
| School age children: 100–199 μg/L | Tibet, Tianjin, Shanghai, Guangdong | Beijing, Xinjiang, Henan, Liaoning, Jilin, Shandong | 10 | |
| School age children: 200–299 μg/L | Fujian, Guanxi | Hainan, Heilongjiang, Gansu, Hebei, Qinghai, Ningxia, Xinjiang Corps, Zheijiang, Chongqing, Inner Mongolia, Hubei, Hunan, Yunan, Shaanxi, Sichuan | Shanxi | 18 |
| School age children: ≥300 μg/L | Guizhou, Jiangxi, Jiangsu, Anhui | 4 | ||
| No of provinces | 6 | 25 | 1 | 32 |
| Country (Year) | School-Age Children (μg/L) | Iodine Status [1] | Pregnant Women (μg/L) | Iodine Status [1] |
|---|---|---|---|---|
| Fiji (2009) [85] | 237 | Above requirements | 227 | Adequate |
| Indonesia (2013) [86] | 223 | Above requirements | 172 | Adequate |
| Mongolia (2011) [87] | 171 | Adequate | 1512 | Adequate |
| Australia (2016) [88] | 175 | Adequate | 116 | Insufficient |
| New Zealand (2011) [89,90] | 113 | Adequate | 85 | Insufficient |
| The Philippines (2013) [91] | 168 | Adequate | 105 | Insufficient |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, D.; Codling, K.; Chang, S.; Zhang, S.; Shen, H.; Su, X.; Chen, Z.; Scherpbier, R.W.; Yan, J. Eliminating Iodine Deficiency in China: Achievements, Challenges and Global Implications. Nutrients 2017, 9, 361. https://doi.org/10.3390/nu9040361
Sun D, Codling K, Chang S, Zhang S, Shen H, Su X, Chen Z, Scherpbier RW, Yan J. Eliminating Iodine Deficiency in China: Achievements, Challenges and Global Implications. Nutrients. 2017; 9(4):361. https://doi.org/10.3390/nu9040361
Chicago/Turabian StyleSun, Dianjun, Karen Codling, Suying Chang, Shubin Zhang, Hongmei Shen, Xiaohui Su, Zupei Chen, Robert W. Scherpbier, and Jun Yan. 2017. "Eliminating Iodine Deficiency in China: Achievements, Challenges and Global Implications" Nutrients 9, no. 4: 361. https://doi.org/10.3390/nu9040361
APA StyleSun, D., Codling, K., Chang, S., Zhang, S., Shen, H., Su, X., Chen, Z., Scherpbier, R. W., & Yan, J. (2017). Eliminating Iodine Deficiency in China: Achievements, Challenges and Global Implications. Nutrients, 9(4), 361. https://doi.org/10.3390/nu9040361





