An Assessment of the Potential Impact of Fortification of Staples and Condiments on Micronutrient Intake of Young Children and Women of Reproductive Age in Bangladesh †
Abstract
:1. Introduction
2. Experimental Section
2.1. Study Design
2.2. Population Sampling
2.3. Food Consumption Analysis
2.4. Socioeconomic Status
2.5. Fortification Levels
2.6. Data Management and Statistical Analysis
2.7. Ethical Issues
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Food and Agriculture Organization of the United Nations; World Food Programme; International Fund for Agricultural Development. The State of Food Insecurity in the World 2012: Economic Growth Is Necessary but Not Sufficient to Accelerate Reduction of Hunger and Malnutrition. Available online: http://www.fao.org/docrep/016/i3027e/i3027e.pdf (accessed on 24 September 2015).
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- World Bank. Bangladesh Development Update. Available online: http://www-wds.Worldbank.org/external/default/WDSContentServer/WDSP/IB/2015/08/10/090224b0828c33b0/1_0/Rendered/PDF/Bangladesh0development0update.pdf (accessed on 24 September 2015).
- National Institute of Population Research and Training; Mitra and Associates; MEASURE DHS; ICF International. Bangladesh Demographic and Health Survey 2011. Available online: http://dhsprogram.com/pubs/pdf/FR265/FR265.pdf (accessed on 24 September 2015).
- ICDDR,B; United Nations Children’s Fund; Bangladesh; Global Alliance for Improved Nutrition; Institute of Public Health and Nutrition. National Micronutrients Status Survey 2011–2012 Final Report. Available online: http://www.icddrb.org/publications/cat_view/10043-icddrb-documents/10058-icddrb-reports-and-working-papers/14275-survey-reports (accessed on 24 September 2015).
- World Health Organization; Food and Agriculture Organization of the United Nations. Guidelines on Food Fortification with Micronutrients. Available online: http://www.who.int/nutrition/publications/guide_food_fortification_micronutrients.pdf (accessed on 24 September 2015).
- Arsenault, J.E.; Yakes, E.A.; Islam, M.M.; Hossain, M.B.; Ahmed, T.; Hotz, C.; Lewis, B.; Rahman, A.S.; Jamil, K.M.; Brown, K.H. Very low adequacy of micronutrient intakes by young children and women in rural Bangladesh is primarily explained by low food intake and limited diversity. J. Nutr. 2013, 143, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, P.H.; Avula, R.; Ruel, M.T.; Saha, K.K.; Ali, D.; Tran, L.M.; Frongillo, E.A.; Menon, P.; Rawat, R. Maternal and child dietary diversity are associated in Bangladesh, Vietnam, and Ethiopia. J. Nutr. 2013, 143, 1176–1183. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Pramanik, M. Conversion Factors and Dietary Calculation; Institute of Nutrition and Food Science, University of Dhaka: Dhaka, Bangladesh, 1991; pp. 5–31. [Google Scholar]
- Islam, S.; Khan, N.; Akhtaruzzaman. Food Composition Tables and Database for Bangladesh with Special Reference to Selected Ethnic Foods; Institute of Nutrition and Food Science, University of Dhaka: Dhaka, Bangladesh, 2012. [Google Scholar]
- Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc (2000). Available online: http://www.nap.edu/download.php?record_id=10026# (accessed on 24 September 2014).
- Committee on Dietary Allowances, Food and Nutrition Board, Division of Biological Sciences, Assembly of Life Sciences. Recommended Dietary Allowances. Available online: http://www.nap.edu/download.php?record_id=1349# (accessed on 24 September 2015).
- Rutstein, S.O.; Johnson, K. DHS Comparative Reports No. 6: The DHS Wealth Index. Available online: http://www.childinfo.org/files/DHS_Wealth_Index(DHS_Comparative_Reports).pdf (accessed on 24 September 2015).
- World Health Organization. Recommendations on Wheat and Maize Flour Fortification Meeting Report: Interim Consensus Statement; WHO: Geneva, Switzerland, 2009. [Google Scholar]
- De Pee, S. Proposing nutrients and nutrient levels for rice fortification. Ann. N. Y. Acad. Sci. 2014, 1324, 55–66. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; Food and Agriculture Organization of the United Nations. Vitamin and Mineral Requirements in Human Nutrition, 2nd ed. Available online: http://apps.who.int/iris/bitstream/10665/42716/1/9241546123.pdf?ua=1 (accessed on 24 September 2015).
- Lozoff, B.; Beard, J.; Connor, J.; Felt, B.; Georgieff, M.; Schallert, T. Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutr. Rev. 2006, 64, S34–S91. [Google Scholar] [CrossRef] [PubMed]
- Lozoff, B.; Jimenez, E.; Hagen, J.; Mollen, E.; Wolf, A.W. Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy. Pediatrics 2000, 105, E51. [Google Scholar] [CrossRef] [PubMed]
- Casanueva, E.; Pfeffer, F.; Drijanski, A.; Fernandez-Gaxiola, A.C.; Gutierrez-Valenzuela, V.; Rothenberg, S.J. Iron and folate status before pregnancy and anemia during pregnancy. Ann. Nutr. Metab. 2003, 47, 60–63. [Google Scholar] [CrossRef]
- Allen, L.H. Multiple micronutrients in pregnancy and lactation: An overview. Am. J. Clin. Nutr. 2005, 81, 1206S–1212S. [Google Scholar] [PubMed]
- World Health Organization. Guideline: Vitamin A Supplementation in Postpartum Women; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Hurrell, R.F.; Reddy, M.; Cook, J.D. Inhibition of non-haem iron absorption in man by polyphenolic-containing beverages. Br. J. Nutr. 1999, 81, 289–295. [Google Scholar] [PubMed]
- Turnlund, J.R.; King, J.C.; Keyes, W.R.; Gong, B.; Michel, M.C. A stable isotope study of zinc absorption in young men: Effects of phytate and alpha-cellulose. Am. J. Clin. Nutr. 1984, 40, 1071–1077. [Google Scholar] [PubMed]
- Thorne-Lyman, A.L.; Valpiani, N.; Sun, K.; Semba, R.D.; Klotz, C.L.; Kraemer, K.; Akhter, N.; de Pee, S.; Moench-Planner, R.; Sari, M.; et al. Household dietary diversity and food expenditures are closely linked in rural Bangladesh, increasing the risk of malnutrition due to the financial crisis. J. Nutr. 2010, 140, 182S–188S. [Google Scholar] [CrossRef] [PubMed]
- Angeles-Agdeppa, I.; Capanzana, M.V.; Barba, C.V.; Florentino, R.F.; Takanashi, K. Efficacy of iron-fortified rice in reducing anemia among schoolchildren in the Philippines. Int. J. Vitam. Nutr. Res. 2008, 78, 74–86. [Google Scholar] [CrossRef] [PubMed]
- Hotz, C.; Porcayo, M.; Onofre, G.; Garcia-Guerra, A.; Elliott, T.; Jankowski, S.; Greiner, T. Efficacy of iron-fortified Ultra Rice in improving the iron status of women in Mexico. Food Nutr. Bull. 2008, 29, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Moretti, D.; Zimmermann, M.B.; Muthayya, S.; Thankachan, P.; Lee, T.C.; Kurpad, A.V.; Hurrell, R.F. Extruded rice fortified with micronized ground ferric pyrophosphate reduces iron deficiency in Indian schoolchildren: A double-blind randomized controlled trial. Am. J. Clin. Nutr. 2006, 84, 822–829. [Google Scholar] [PubMed]
- Piccoli, N.B.; Grede, N.; de Pee, S.; Singhkumarwong, A.; Roks, E.; Moench-Planner, R.; Bloem, M.W. Rice fortification: Its potential for improving micronutrient intake and steps required for implementation at scale. Food Nutr. Bull. 2012, 33, S360–S372. [Google Scholar] [CrossRef] [PubMed]
- Dary, O.; Mora, J.O.; International Vitamin A Consultative Group. Food fortification to reduce vitamin A deficiency: International Vitamin A Consultative Group recommendations. J. Nutr. 2002, 132, 2927S–2933S. [Google Scholar] [PubMed]
- Rahman, S.; Ahmed, T.; Rahman, A.S.; Alam, N.; Ahmed, A.S.; Ireen, S.; Chowdhury, I.A.; Chowdhury, F.P.; Rahman, S.M. Determinants of iron status and Hb in the Bangladesh population: The role of groundwater iron. Public Health Nutr. 2016, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Ahsan, H.; Parvez, F.; Howe, G.R. Validity of a food-frequency questionnaire for a large prospective cohort study in Bangladesh. Br. J. Nutr. 2004, 92, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R.S.; Ferguson, E.L. An Interactive 24-h Recall for Assessing the Adequacy of Iron and Zinc Intakes in Developing Countries; International Food Policy Research Institute (IFPRI) and International Center for Tropical Agriculture (CIAT): Washington, DC, USA; Cali, Colombia, 2008. [Google Scholar]
- Cheng, Y.; Yan, H.; Dibley, M.J.; Shen, Y.; Li, Q.; Zeng, L. Validity and reproducibility of a semi-quantitative food frequency questionnaire for use among pregnant women in rural China. Asia Pac. J. Clin. Nutr. 2008, 17, 166–177. [Google Scholar] [PubMed]


| Fortificant | Standard |
|---|---|
| Rice | 70 mg/kg of iron as micronized ferric pyrophosphate, 50 mg/kg of zinc, 1 mg/kg of folic acid, and 0.008 mg/kg of vitamin B12 |
| Wheat flour | 40 mg/kg of iron as NaFeEDTA, 50 mg/kg of zinc, 5 mg/kg of folic acid, and 0.04 mg/kg of vitamin B12 |
| Sugar | 10 parts per million (ppm) of retinyl palmitate |
| Vegetable oil | 10–15 ppm of retinyl palmitate |
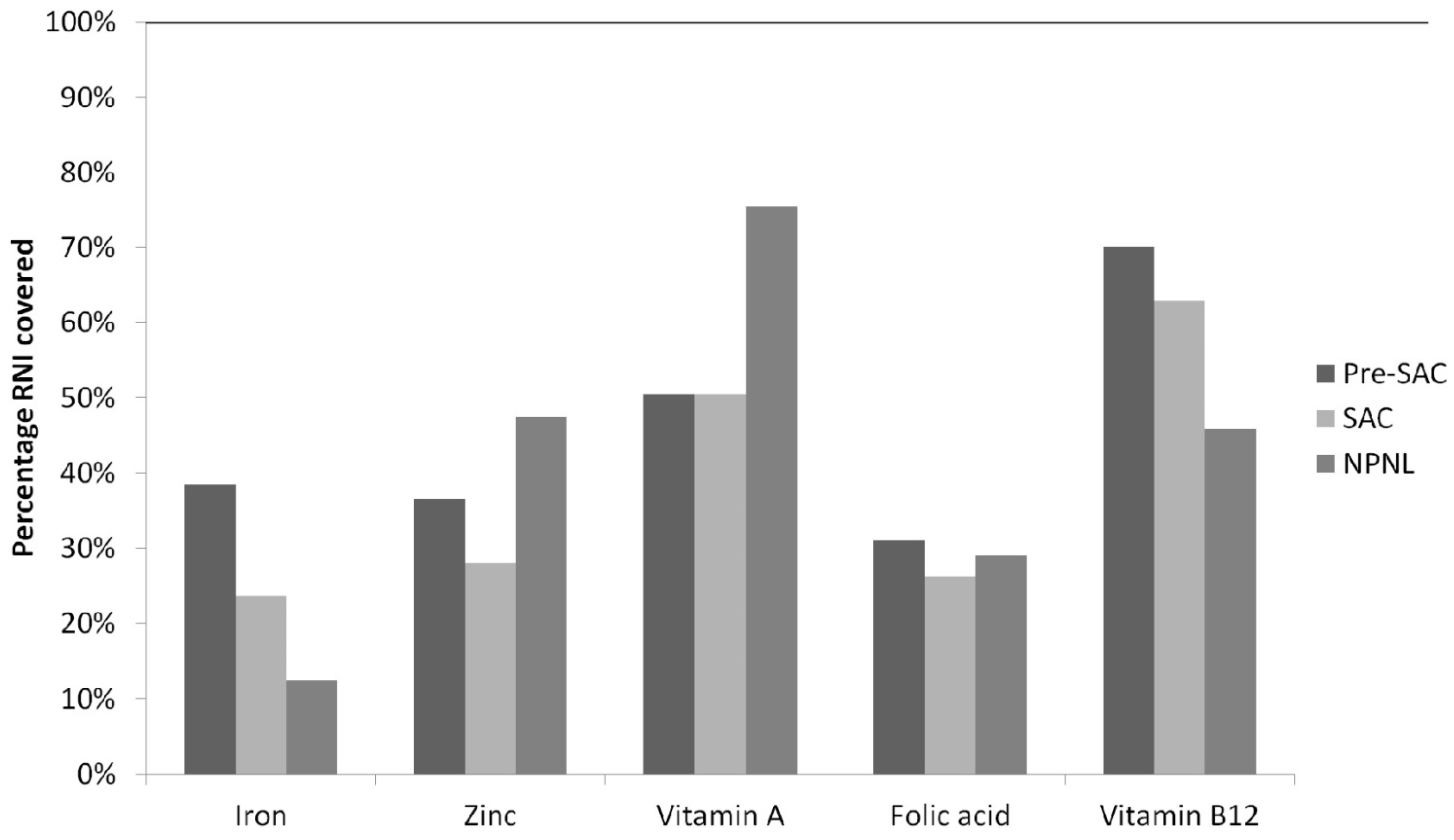
| Micronutrients | Preschool-Aged Children (Pre-SAC) | School-Aged Children (SAC) | Nonpregnant Nonlactating Women (NPNL) |
|---|---|---|---|
| Iron (mg/day) | 4.6 (3.2–5.0) | 6.2 (5.6–7.0) | 7.4 (7.0–8.0) |
| Zinc (mg/day) | 3.2 (2.8–4.0) | 3.8 (3.4–4.0) | 4.9 (4.3–5.0) |
| Vitamin A (RE/day) | 210.6 (75.0–468.4) | 277.9 (91.7–620.1) | 385.8 (127.5–780.1) |
| Folic acid (µg/day) | 51.7 (47.7–55.7) | 90.3 (85.6–95.7) | 116.0 (110.4–121.9) |
| Vitamin B12 (µg/day) | 0.7 (0.6–0.8) | 1.3 (1.2–1.4) | 1.1 (1.1–1.2) |
| Fortifiable Foods | Pre-SAC | SAC | NPNL |
|---|---|---|---|
| Rice | 99.3% | 100.0% | 100.0% |
| Bread | 33.5% | 28.0% | 10.5% |
| Wheat flour | 76.2% | 66.5% | 41.9% |
| Sugar | 41.1% | 36.7% | 30.3% |
| Fortifiable Foods | Pre-SAC | n | SAC | n | NPNL | n |
|---|---|---|---|---|---|---|
| Rice | 157.1 (147.6–166.4) | 841 | 260.6 (233.1–288.1) | 1428 | 359.5 (318.6–400.4) | 1412 |
| Bread | 20.5 (16.3–24.7) | 284 | 18.0 (14.4–21.6) | 400 | 16.2 (12.7–19.6) | 207 |
| Wheat flour | 41.8 (35.0–48.6) | 646 | 58.2 (47.6–68.8) | 1050 | 77.9 (63.8–92.0) | 907 |
| Sugar | 7.8 (5.8–9.8) | 348 | 7.9 (6.3–9.5) | 530 | 7.8 (5.3–10.2) | 485 |
| Oil | 15.2 (13.8–16.6) | 2000 | 22.0 (19.9–24.0) | 2000 | 22.7 (20.6–24.8) | 2000 |
| Iron (mg/Day) | Zinc (mg/Day) | Folic Acid (µg/Day) | Vitamin B12 (µg/Day) | |
|---|---|---|---|---|
| Rice | ||||
| Pre-SAC | 10.4 | 7.46 | 78.6 | 0.9 |
| SAC | 17.3 | 12.4 | 130.3 | 1.5 |
| NPNL | 23.9 | 17.1 | 179.8 | 2.0 |
| Bread | ||||
| Pre-SAC | 0.8 | 1.0 | 51.3 | 0.6 |
| SAC | 0.7 | 0.9 | 45.0 | 0.5 |
| NPNL | 0.6 | 0.8 | 40.5 | 0.5 |
| Wheat flour | ||||
| Pre-SAC | 1.6 | 2.0 | 104.5 | 1.2 |
| SAC | 2.2 | 2.8 | 145.5 | 1.6 |
| NPNL | 3.0 | 3.7 | 194.8 | 2.2 |
| Population Groups | Vitamin A (µg Retinol Equivalent/Day) |
|---|---|
| Sugar | |
| Pre-SAC | 54.6 |
| SAC | 55.3 |
| NPNL | 54.6 |
| Oil | |
| Pre-SAC | 159.6 |
| SAC | 230.9 |
| NPNL | 238.0 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leyvraz, M.; Laillou, A.; Rahman, S.; Ahmed, T.; Rahman, A.S.; Alam, N.; Ireen, S.; Panagides, D. An Assessment of the Potential Impact of Fortification of Staples and Condiments on Micronutrient Intake of Young Children and Women of Reproductive Age in Bangladesh. Nutrients 2016, 8, 541. https://doi.org/10.3390/nu8090541
Leyvraz M, Laillou A, Rahman S, Ahmed T, Rahman AS, Alam N, Ireen S, Panagides D. An Assessment of the Potential Impact of Fortification of Staples and Condiments on Micronutrient Intake of Young Children and Women of Reproductive Age in Bangladesh. Nutrients. 2016; 8(9):541. https://doi.org/10.3390/nu8090541
Chicago/Turabian StyleLeyvraz, Magali, Arnaud Laillou, Sabuktagin Rahman, Tahmeed Ahmed, Ahmed Shafiqur Rahman, Nurul Alam, Santhia Ireen, and Dora Panagides. 2016. "An Assessment of the Potential Impact of Fortification of Staples and Condiments on Micronutrient Intake of Young Children and Women of Reproductive Age in Bangladesh" Nutrients 8, no. 9: 541. https://doi.org/10.3390/nu8090541
APA StyleLeyvraz, M., Laillou, A., Rahman, S., Ahmed, T., Rahman, A. S., Alam, N., Ireen, S., & Panagides, D. (2016). An Assessment of the Potential Impact of Fortification of Staples and Condiments on Micronutrient Intake of Young Children and Women of Reproductive Age in Bangladesh. Nutrients, 8(9), 541. https://doi.org/10.3390/nu8090541




