Sex-Specific Sociodemographic Correlates of Dietary Patterns in a Large Sample of French Elderly Individuals
Abstract
:1. Introduction
2. Methods
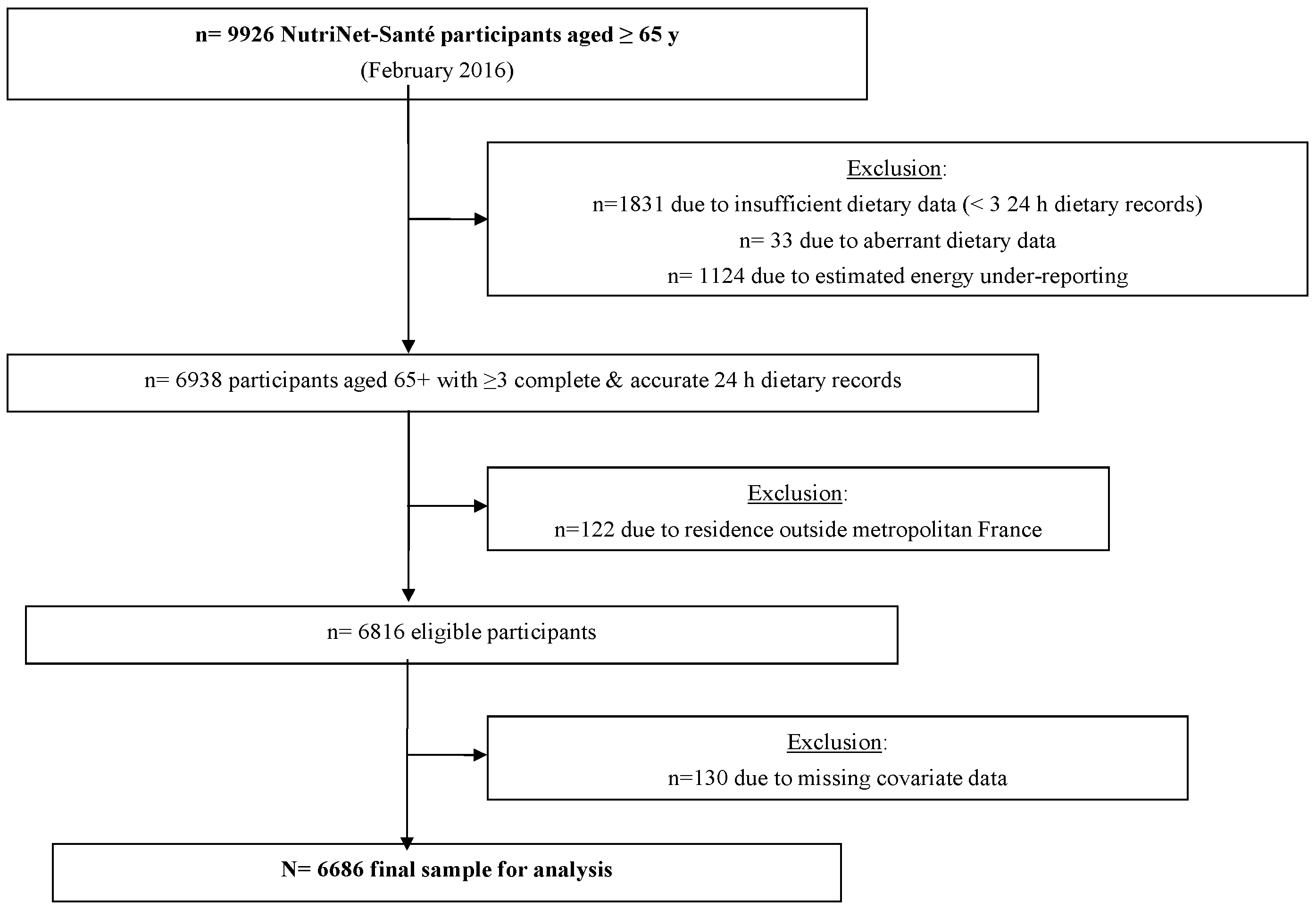
2.1. Context and Sample
2.2. Dietary Assessment
2.3. Dietary Patterns
2.4. Covariates
2.5. Statistical Analysis
2.6. Supplementary Analysis
3. Results
3.1. Sample Characteristics
3.2. Dietary Patterns in French Elderly
3.3. Sociodemographic and Health Status Correlates of the Three DP
3.4. Supplementary Analysis
4. Discussion
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hawkes, C. Uneven dietary development: Linking the policies and processes of globalization with the nutrition transition, obesity and diet-related chronic diseases. Glob. Health 2006, 2, 4. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). A snapshot from across Europe. Successful nutrition policies—country examples. In The WHO Europe Food and Nutrition Action Plan 2015–2020; WHO: Copenhagen, Denmark, 2014. [Google Scholar]
- Alt, K.W.; Rossbach, A. Nothing in nature is as consistent as change. Front. Oral Biol. 2009, 13, 190–196. [Google Scholar] [PubMed]
- Bernstein, M.; Munoz, N.; Academy of Nutrition and Dietetics. Position of the Academy of Nutrition and Dietetics. Food and nutrition for older adults: Promoting health and wellness. J. Acad. Nutr. Diet. 2012, 112, 1255–1277. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, M.F.; Weddle, D.O.; American Dietetic Association. Position paper of the American Dietetic Association: Nutrition across the spectrum of aging. J. Am. Diet. Assoc. 2005, 105, 616–633. [Google Scholar] [PubMed]
- Duffy, V.B.; Backstrand, J.R.; Ferris, A.M. Olfactory dysfunction and related nutritional risk in free-living, elderly women. J. Am. Diet. Assoc. 1995, 95, 879–884. [Google Scholar] [CrossRef]
- Bartali, B.; Salvini, S.; Turrini, A.; Lauretani, F.; Russo, C.R.; Corsi, A.M.; Bandinelli, S.; D’Amicis, A.; Palli, D.; Guralnik, J.M.; et al. Age and disability affect dietary intake. J. Nutr. 2003, 133, 2868–2873. [Google Scholar] [PubMed]
- Koehler, J.; Leonhaeuser, I.U. Changes in food preferences during aging. Ann. Nutr. Metab. 2008, 52, S15–S19. [Google Scholar] [CrossRef] [PubMed]
- Volkert, D. Nutrition and lifestyle of the elderly in Europe. J. Public Health 2005, 13, 56–61. [Google Scholar] [CrossRef]
- Samieri, C.; Jutand, M.A.; Feart, C.; Capuron, L.; Letenneur, L.; Barberger-Gateau, P. Dietary patterns derived by hybrid clustering method in older people: Association with cognition, mood, and self-rated health. J. Am. Diet. Assoc. 2008, 108, 1461–1471. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.L.; Harris, T.B.; Tylavsky, F.A.; Perry, S.E.; Houston, D.K.; Hue, T.F.; Strotmeyer, E.S.; Sahyoun, N.R.; Health ABC Study. Dietary patterns and survival of older adults. J. Am. Diet. Assoc. 2011, 111, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Ashby-Mitchell, K.; Peeters, A.; Anstey, K.J. Role of dietary pattern analysis in determining cognitive status in elderly Australian adults. Nutrients 2015, 7, 1052–1067. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, D.R., Jr.; Gross, M.D.; Tapsell, L.C. Food synergy: An operational concept for understanding nutrition. Am. J Clin. Nutr. 2009, 89, 1543S–1548S. [Google Scholar] [CrossRef] [PubMed]
- Alles, B.; Samieri, C.; Feart, C.; Jutand, M.A.; Laurin, D.; Barberger-Gateau, P. Dietary patterns: A novel approach to examine the link between nutrition and cognitive function in older individuals. Nutr. Res. Rev. 2012, 25, 207–222. [Google Scholar] [CrossRef] [PubMed]
- Bamia, C.; Orfanos, P.; Ferrari, P.; Overvad, K.; Hundborg, H.H.; Tjonneland, A.; Olsen, A.; Kesse, E.; Boutron-Ruault, M.C.; Clavel-Chapelon, F.; et al. Dietary patterns among older Europeans: The EPIC-Elderly study. Br. J. Nutr. 2005, 94, 100–113. [Google Scholar] [CrossRef] [PubMed]
- Charles, M.A.; Eschwege, E.; Basdevant, A. Monitoring the obesity epidemic in France: The Obepi surveys 1997–2006. Obesity 2008, 16, 2182–2186. [Google Scholar] [CrossRef] [PubMed]
- Larrieu, S.; Letenneur, L.; Berr, C.; Dartigues, J.F.; Ritchie, K.; Alperovitch, A.; Tavernier, B.; Barberger-Gateau, P. Sociodemographic differences in dietary habits in a population-based sample of elderly subjects: The 3C study. J. Nutr. Health Aging 2004, 8, 497–502. [Google Scholar] [PubMed]
- Touvier, M.; Niravong, M.; Volatier, J.L.; Lafay, L.; Lioret, S.; Clavel-Chapelon, F.; Boutron-Ruault, M.C. Dietary patterns associated with vitamin/mineral supplement use and smoking among women of the E3N-EPIC cohort. Eur. J. Clin. Nutr. 2009, 63, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Feart, C.; Samieri, C.; Rondeau, V.; Amieva, H.; Portet, F.; Dartigues, J.F.; Scarmeas, N.; Barberger-Gateau, P. Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. JAMA 2009, 302, 638–648. [Google Scholar] [CrossRef] [PubMed]
- Bedard, A.; Garcia-Aymerich, J.; Sanchez, M.; Le Moual, N.; Clavel-Chapelon, F.; Boutron-Ruault, M.C.; Maccario, J.; Varraso, R. Confirmatory factor analysis compared with principal component analysis to derive dietary patterns: A longitudinal study in adult women. J. Nutr. 2015, 145, 1559–1568. [Google Scholar] [CrossRef] [PubMed]
- Alles, B.; Samieri, C.; Lorrain, S.; Jutand, M.A.; Carmichael, P.H.; Shatenstein, B.; Gaudreau, P.; Payette, H.; Laurin, D.; Barberger-Gateau, P. Nutrient patterns and their food sources in older persons from France and Quebec: Dietary and lifestyle characteristics. Nutrients 2016, 8, 225. [Google Scholar] [CrossRef] [PubMed]
- Ferrand, C.; Feart, C.; Barberger-Gateau, P.; Albinet, C.; Andre, N.; Audiffren, M. Dietary patterns in French home-living older women: Links with sociodemographic factors, depressive symptoms, cognitive function, and self-rated health. J. Nutr. Health Aging 2015, 19, S11. [Google Scholar]
- Agence Nationale de la Recherche (ANR). Projet ALIMASSENS: Toward Offering Healthy Food Products Better Adapted to Elderly People. Available online: http://www.agence-nationale-recherche.fr/?Project=ANR-14-CE20-0003 (accessed on 27 July 2016).
- Hercberg, S.; Castetbon, K.; Czernichow, S.; Malon, A.; Mejean, C.; Kesse, E.; Touvier, M.; Galan, P. The Nutrinet-Santé Study: A web-based prospective study on the relationship between nutrition and health and determinants of dietary patterns and nutritional status. BMC Public Health 2010, 10, 242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le Moullec, N.; Deheeger, M.; Preziosi, P.; Monteiro, P.; Valeix, P.; Rolland-Cachera, M.F.; Potier de Courcy, G.; Christides, J.P.; Cherouvrier, F.; Galan, P.; et al. Validation du manuel photos utilisé pour l'enquête alimentaire de l'étude SU.VI.MAX. Cah. Nutr. Diét. 1996, 31, 158–164. [Google Scholar]
- Etude NutriNet-Santé. Table de Composition des Aliments; Économica: Paris, France, 2013. [Google Scholar]
- Hatcher, L. A Step-by-Step Approach to Using SAS for Factor Analysis and Structural Equation Modeling; SAS Institute Inc.: Cary, NC, USA, 1994. [Google Scholar]
- Black, A.E. Critical evaluation of energy intake using the Goldberg cut-off for energy intake: Basal metabolic rate. A practical guide to its calculation, use and limitations. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 1119–1130. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.; Stampfer, M.J. Total energy intake: Implications for epidemiologic analyses. Am. J. Epidemiol. 1986, 124, 17–27. [Google Scholar] [PubMed]
- Feart, C.; Jutand, M.A.; Larrieu, S.; Letenneur, L.; Delcourt, C.; Combe, N.; Barberger-Gateau, P. Energy, macronutrient and fatty acid intake of French elderly community dwellers and association with socio-demographic characteristics: Data from the Bordeaux sample of the Three-City Study. Br. J. Nutr. 2007, 98, 1046–1057. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, P.Y.; Mitchell, D.C.; Coffman, D.L.; Allman, R.M.; Locher, J.L.; Sawyer, P.; Jensen, G.L.; Hartman, T.J. Dietary patterns and diet quality among diverse older adults: The University of Alabama at Birmingham Study of Aging. J. Nutr. Health Aging 2013, 17, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Bertin, M.; Touvier, M.; Dubuisson, C.; Dufour, A.; Havard, S.; Lafay, L.; Volatier, J.L.; Lioret, S. Dietary patterns of French adults: Associations with demographic, socio-economic and behavioural factors. J. Hum. Nutr. Diet. 2016, 29, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Hercberg, S.; Chat-Yung, S.; Chaulia, M. The French National Nutrition and Health Program: 2001-2006-2010. Int. J. Public Health 2008, 53, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Assmann, K.E.; Lassale, C.; Galan, P.; Hercberg, S.; Kesse-Guyot, E. Dietary quality and 6-year anthropometric changes in a sample of French middle-aged overweight and obese adults. PLoS ONE 2014, 9, e87083. [Google Scholar] [CrossRef]
- Estaquio, C.; Kesse-Guyot, E.; Deschamps, V.; Bertrais, S.; Dauchet, L.; Galan, P.; Hercberg, S.; Castetbon, K. Adherence to the French Programme National Nutrition Santé Guideline Score is associated with better nutrient intake and nutritional status. J. Am. Diet. Assoc. 2009, 109, 1031–1041. [Google Scholar] [CrossRef] [PubMed]
- Lelong, H.; Blacher, J.; Menai, M.; Galan, P.; Fezeu, L.; Hercberg, S.; Kesse-Guyot, E. Association between blood pressure and adherence to French dietary guidelines. Am. J. Hypertens. 2016, 29, 948–958. [Google Scholar] [CrossRef] [PubMed]
- Lassale, C.; Fezeu, L.; Andreeva, V.A.; Hercberg, S.; Kengne, A.P.; Czernichow, S.; Kesse-Guyot, E. Association between dietary scores and 13-year weight change and obesity risk in a French prospective cohort. Int. J. Obes. 2012, 36, 1455–1462. [Google Scholar] [CrossRef] [PubMed]
- Kesse-Guyot, E.; Bertrais, S.; Peneau, S.; Estaquio, C.; Dauchet, L.; Vergnaud, A.C.; Czernichow, S.; Galan, P.; Hercberg, S.; Bellisle, F. Dietary patterns and their sociodemographic and behavioural correlates in French middle-aged adults from the SU.VI.MAX cohort. Eur. J. Clin. Nutr. 2009, 63, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Pala, V.; Sieri, S.; Masala, G.; Palli, D.; Panico, S.; Vineis, P.; Sacerdote, C.; Mattiello, A.; Galasso, R.; Salvini, S.; et al. Associations between dietary pattern and lifestyle, anthropometry and other health indicators in the elderly participants of the EPIC-Italy cohort. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 186–201. [Google Scholar] [CrossRef] [PubMed]
- Mullie, P.; Clarys, P.; Hulens, M.; Vansant, G. Dietary patterns and socioeconomic position. Eur. J. Clin. Nutr. 2010, 64, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; An, R. Impact of home-delivered meal programs on diet and nutrition among older adults: A review. Nutr. Health 2013, 22, 89–103. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.; Syddall, H.; Jameson, K.; Batelaan, S.; Martin, H.; Dennison, E.M.; Cooper, C.; Sayer, A.A.; Hertfordshire Study Group. Current patterns of diet in community-dwelling older men and women: Results from the Hertfordshire Cohort Study. Age Ageing 2009, 38, 594–599. [Google Scholar] [CrossRef] [PubMed]
- Spring, B.; Moller, A.C.; Coons, M.J. Multiple health behaviours: Overview and implications. J. Public Health 2012, 34, i3–i10. [Google Scholar] [CrossRef] [PubMed]
- Dernini, S.; Berry, E.M. Mediterranean diet: From a healthy diet to a sustainable dietary pattern. Front. Nutr. 2015, 2, 15. [Google Scholar] [CrossRef] [PubMed]
- Price, G.M.; Uauy, R.; Breeze, E.; Bulpitt, C.J.; Fletcher, A.E. Weight, shape, and mortality risk in older persons: Elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death. Am. J. Clin. Nutr. 2006, 84, 449–460. [Google Scholar] [PubMed]
- Andreeva, V.A.; Salanave, B.; Castetbon, K.; Deschamps, V.; Vernay, M.; Kesse-Guyot, E.; Hercberg, S. Comparison of the sociodemographic characteristics of the large NutriNet-Sante e-cohort with French Census data: The issue of volunteer bias revisited. J. Epidemiol. Community Health 2015, 69, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Bigot, R.; Croutte, P. La Diffusion des Technologies de L'information et de la Communication Dans la Société Française; Centre de Recherche pour l'Étude et l'Observation des Conditions de Vie (CRÉDOC): Paris, France, 2014. [Google Scholar]
- Thompson, F.E.; Subar, A.F. Chapter 1: Dietary Assessment Methodology; Elsevier, Inc.: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Tada, A.; Miura, H. Systematic review of the association of mastication with food and nutrient intake in the independent elderly. Arch. Gerontol. Geriatr. 2014, 59, 497–505. [Google Scholar] [CrossRef] [PubMed]
- Kossioni, A.; Bellou, O. Eating habits in older people in Greece: The role of age, dental status and chewing difficulties. Arch. Gerontol. Geriatr. 2011, 52, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Andreeva, V.A.; Deschamps, V.; Salanave, B.; Castetbon, K.; Verdot, C.; Kesse-Guyot, E.; Hercberg, S. Dietary intake comparison between a large online cohort (Etude NutriNet-Santé) and a nationally-representative cross-sectional study in France (ENNS): Addressing the issue of generalizability in e-epidemiology. Am. J. Epidemiol. 2016. [Google Scholar] [CrossRef]
- Moeller, S.M.; Reedy, J.; Millen, A.E.; Dixon, L.B.; Newby, P.K.; Tucker, K.L.; Krebs-Smith, S.M.; Guenther, P.M. Dietary patterns: Challenges and opportunities in dietary patterns research an experimental biology workshop, April 1, 2006. J. Am. Diet. Assoc. 2007, 107, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.D. Principal components analysis and exploratory factor analysis: Definitions, differences, and choices. JALT Test. Eval. SIG Newsl. 2009, 13, 26–30. [Google Scholar]
- Andreeva, V.A.; Kesse-Guyot, E. Nutrition and cognition in the context of ageing: Role of dietary patterns. In Nutrition for Brain Health and Cognitive Performance; Best, T., Dye, L., Eds.; CRC Press, Taylor & Francis Group: Boca Raton, FL, USA, 2015; pp. 11–40. [Google Scholar]
- Johnston, R.; Poti, J.M.; Popkin, B.M. Eating and aging: Trends in dietary intake among older Americans from 1977–2010. J. Nutr. Health Aging 2014, 18, 234–242. [Google Scholar] [CrossRef] [PubMed]
| Pattern 1: Healthy | Pattern 2: Western | Pattern 3: Traditional | |
|---|---|---|---|
| Food | |||
| Vegetables | 0.48 | −0.28 | 0.44 |
| Fresh fruit | 0.47 | −0.02 | 0.12 |
| Dried fruits, nuts | 0.46 | −0.01 | −0.02 |
| Fish | 0.28 | −0.08 | −0.05 |
| Whole-grain products | 0.51 | −0.12 | −0.13 |
| Vegetable oils | 0.45 | 0.06 | 0.08 |
| Milk-based desserts | −0.29 | −0.05 | 0.09 |
| Bread, toast | −0.27 | 0.37 | 0.51 |
| Broth, stock | 0.07 | −0.33 | 0.61 |
| Butter, margarine | −0.02 | 0.13 | 0.60 |
| Potatoes, tubers | 0.01 | 0.08 | 0.50 |
| Sweet products (honey, candy) | 0.05 | 0.22 | 0.37 |
| Appetizers | 0.05 | 0.39 | −0.08 |
| Cheese | 0.16 | 0.52 | 0.22 |
| Cold cuts | −0.03 | 0.48 | 0.03 |
| Red meat, organ meats | −0.23 | 0.27 | 0.16 |
| Pastries, high-fat and high-sugar products | −0.04 | 0.29 | 0.05 |
| Yogurt | 0.12 | −0.38 | −0.06 |
| Legumes/pulses | 0.22 | −0.04 | 0.11 |
| Beverages | |||
| Milk | −0.28 | −0.12 | 0.27 |
| Non-alcoholic non-sweetend beverages | 0.48 | −0.01 | −0.00 |
| Alcoholic beverages | −0.04 | 0.64 | −0.07 |
| Men (n = 2991) | Women (n = 3695) | p b | |
|---|---|---|---|
| Age, years, mean (SD) | 69.2 (4.0) | 68.6 (3.8) | <0.0001 |
| 65–69 years | 1856 (62.1) | 2551 (69.0) | |
| 70–74 years | 822 (27.5) | 842 (22.8) | |
| ≥75 years | 313 (10.5) | 302 (8.2) | |
| Body mass index, kg/m2, mean (SD) | 25.6 (3.5) | 24.7 (4.5) | <0.0001 |
| Normal, 18.5–24.9 | 1423 (47.6) | 2247 (60.8) | |
| Overweight, 25.0–29.9 | 1285 (43.0) | 1026 (27.8) | |
| Obese, ≥30 | 283 (9.5) | 422 (11.4) | |
| Educational level | <0.001 | ||
| Up to high school | 1387 (46.4) | 2007 (54.3) | |
| Post-secondary education | 1604 (53.6) | 1688 (45.7) | |
| Living alone | 370 (12.4) | 1337 (36.2) | <0.0001 |
| Retired | 2925 (97.8) | 3564 (96.5) | 0.001 |
| Most recent occupation | <0.0001 | ||
| Farmer, manual labor, blue-collar | 259 (8.7) | 1053 (28.5) | |
| Office staff, self-employed | 1887 (63.1) | 1228 (33.2) | |
| Professional/executive staff | 845 (28.3) | 1414 (38.3) | |
| Smoking status | <0.0001 | ||
| Never | 848 (28.4) | 2055 (55.6) | |
| Former | 1949 (65.2) | 1448 (39.2) | |
| Current | 194 (6.5) | 192 (5.2) | |
| Residence in urban area (≥20,000 inhabitants) | 1841 (61.6) | 2403 (65.0) | 0.003 |
| Hypertension c | 1254 (42.0) | 1119 (30.7) | <0.0001 |
| Diabetes d | 273 (9.2) | 136 (3.7) | <0.0001 |
| Cardiovascular disease history e | 224 (7.5) | 92 (2.5) | <0.0001 |
| Total dietary energy, kcal/day, mean (SD) f | 2122.6 (473.1) | 1678.4 (362.5) | <0.0001 |
| Dietary Pattern 1 | Dietary Pattern 2 | Dietary Pattern 3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Healthy | Western | Traditional | ||||||||||
| Men | Women | Men | Women | Men | Women | |||||||
| beta | p | beta | p | beta | p | beta | p | beta | p | beta | p | |
| Age, years a | ||||||||||||
| 70–74 years | 0.05 | 0.28 | −0.03 | 0.44 | −0.06 | 0.09 | −0.05 | 0.08 | 0.12 | 0.003 | 0.13 | <0.0001 |
| 75+ years | −0.03 | 0.64 | −0.15 | 0.004 | −0.09 | 0.12 | −0.10 | 0.03 | 0.25 | <0.0001 | 0.30 | <0.0001 |
| Body mass index, kg/m2 b | ||||||||||||
| Overweight, BMI: 25.0–29.9 | −0.19 | <0.0001 | −0.10 | 0.003 | 0.18 | <0.0001 | 0.03 | 0.32 | −0.03 | 0.46 | 0.03 | 0.34 |
| Obesity, BMI ≥ 30 | −0.11 | 0.13 | −0.21 | <0.0001 | 0.13 | 0.03 | 0.04 | 0.28 | 0.03 | 0.62 | 0.08 | 0.06 |
| Post-secondary education | 0.16 | <0.0001 | 0.08 | 0.005 | −0.01 | 0.69 | −0.01 | 0.79 | −0.10 | 0.004 | 0.00 | 0.97 |
| Living alone | 0.18 | 0.002 | 0.11 | 0.0002 | −0.11 | 0.02 | −0.14 | <0.0001 | −0.08 | 0.14 | −0.01 | 0.82 |
| Smoking c | ||||||||||||
| Former smoker | 0.03 | 0.52 | 0.10 | 0.0009 | 0.29 | <0.0001 | 0.15 | <0.0001 | −0.22 | <0.0001 | −0.21 | <0.0001 |
| Current smoker | −0.36 | <0.0001 | −0.07 | 0.30 | 0.67 | <0.0001 | 0.27 | <0.0001 | −0.43 | <0.0001 | −0.27 | <0.0001 |
| Hypertension | 0.02 | 0.70 | −0.09 | 0.007 | 0.01 | 0.69 | −0.00 | 0.94 | −0.05 | 0.15 | 0.05 | 0.07 |
| Urban area (≥20,000 inhabitants) | −0.02 | 0.58 | 0.01 | 0.73 | 0.02 | 0.51 | 0.01 | 0.62 | −0.16 | <0.0001 | −0.09 | 0.0009 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andreeva, V.A.; Allès, B.; Feron, G.; Gonzalez, R.; Sulmont-Rossé, C.; Galan, P.; Hercberg, S.; Méjean, C. Sex-Specific Sociodemographic Correlates of Dietary Patterns in a Large Sample of French Elderly Individuals. Nutrients 2016, 8, 484. https://doi.org/10.3390/nu8080484
Andreeva VA, Allès B, Feron G, Gonzalez R, Sulmont-Rossé C, Galan P, Hercberg S, Méjean C. Sex-Specific Sociodemographic Correlates of Dietary Patterns in a Large Sample of French Elderly Individuals. Nutrients. 2016; 8(8):484. https://doi.org/10.3390/nu8080484
Chicago/Turabian StyleAndreeva, Valentina A., Benjamin Allès, Gilles Feron, Rebeca Gonzalez, Claire Sulmont-Rossé, Pilar Galan, Serge Hercberg, and Caroline Méjean. 2016. "Sex-Specific Sociodemographic Correlates of Dietary Patterns in a Large Sample of French Elderly Individuals" Nutrients 8, no. 8: 484. https://doi.org/10.3390/nu8080484





