Compliance, Palatability and Feasibility of PALEOLITHIC and Australian Guide to Healthy Eating Diets in Healthy Women: A 4-Week Dietary Intervention
Abstract
:1. Introduction
2. Materials and Methods
3. Results
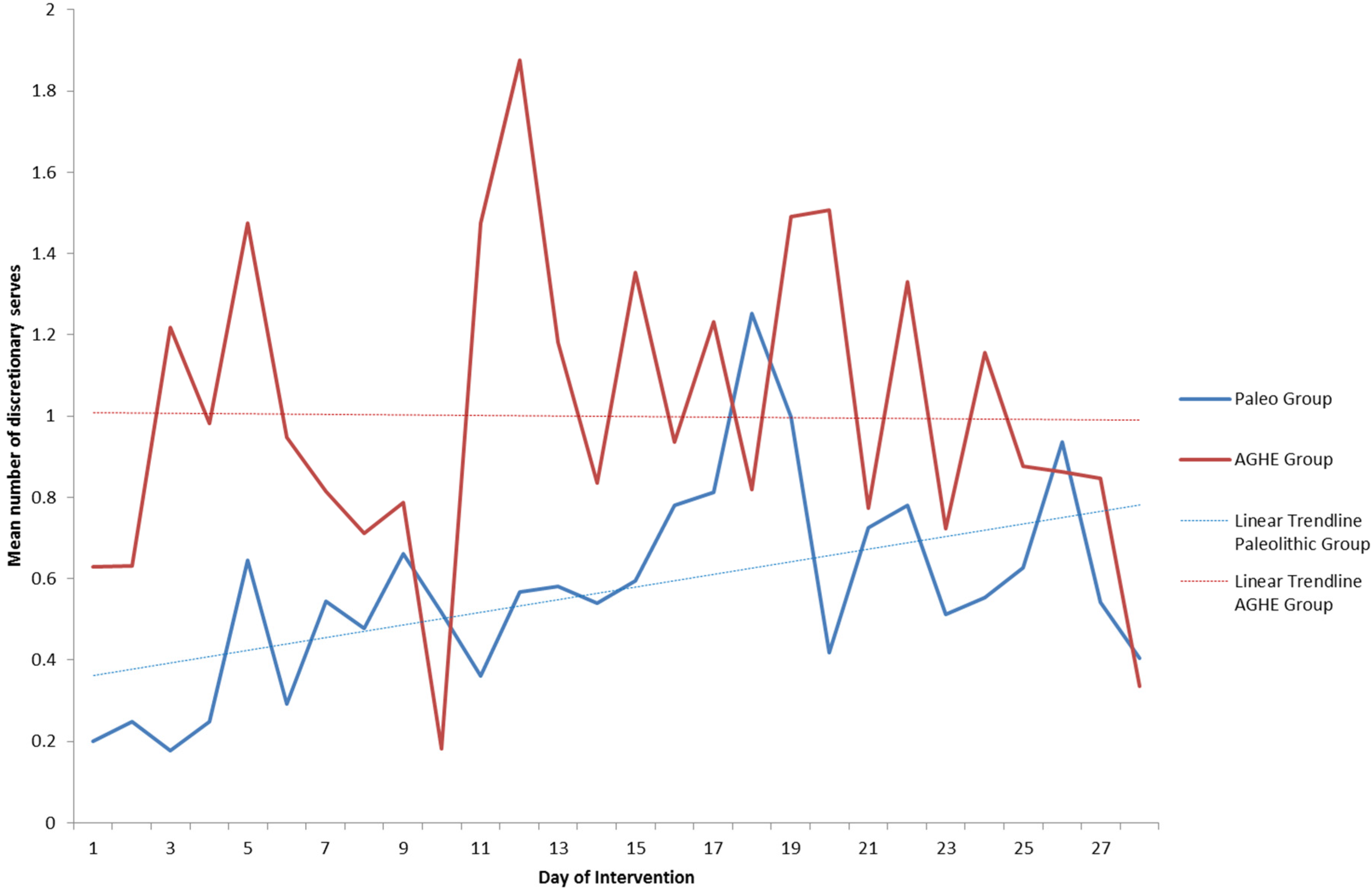
3.1. Compliance
3.2. Adverse Events
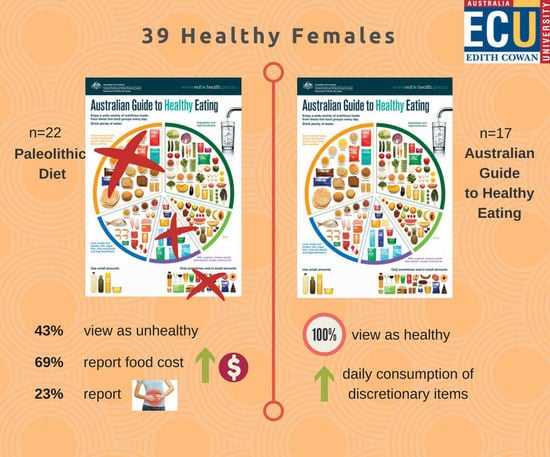
3.3. Palatability and Feasibility Questionnaire
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| AGHE | Australian Guide to Healthy Eating |
References
- Brown, R. Paleo Diet Touted as Better for Diabetics Could Cause Rapid Weight Gain, Research Finds, in ABC News, Australian Broadcasting Corporation. 2016. Available online: http://www.abc.net.au/news/2016-02-19/paleo-diet-can-cause-rapid-weight-gain-research-finds/7183790 (accessed on 21 July 2016).
- Garipoli, A.; Shivaraman, N. The First Five Weeks: Willesee Road-Tests the Paleo Diet, in Sunday Night, Channel 7. 2015. Available online: https://au.news.yahoo.com/sunday-night/features/a/29270243/the-first-five-weeks-willesee-road-tests-the-paleo-diet/#page1 (accessed on 21 July 2016).
- National Health and Medical Research Council. Australian Dietary Guidelines; National Health and Medical Research Council: Canberra, Australia, 2013.
- Boers, I.; Muskiet, F.A.J.; Berkelaar, E.; Schut, E.; Penders, R.; Hoenderdos, K.; Wichers, H.J.; Jong, M.C. Favourable effects of consuming a Palaeolithic-type diet on characteristics of the metabolic syndrome: A randomized controlled pilot-study. Lipids Health Dis. 2014, 13. [Google Scholar] [CrossRef] [PubMed]
- Jönsson, T.; Granfeldt, Y.; Ahrén, B.; Branell, U.-C.; Pålsson, G.; Hansson, A.; Söderström, M.; Lindeberg, S.; Sektion, I. Beneficial effects of a Paleolithic diet on cardiovascular risk factors in type 2 diabetes: A randomized cross-over pilot study. Cardiovasc. Diabetol. 2009, 8, 35. [Google Scholar] [CrossRef]
- Lindeberg, S.; Jönsson, T.; Granfeldt, Y.; Borgstrand, E.; Soffman, J.; Sjöström, K.; Ahrén, B. A Palaeolithic diet improves glucose tolerance more than a Mediterranean-like diet in individuals with ischaemic heart disease. Diabetologia 2007, 50, 1795–1807. [Google Scholar] [CrossRef] [PubMed]
- Mellberg, C.; Sandberg, S.; Ryberg, M.; Eriksson, M.; Brage, S.; Larsson, C.; Olsson, T.; Lindahl, B. Long-term effects of a Palaeolithic-type diet in obese postmenopausal women: A 2-year randomized trial. Eur. J. Clin. Nutr. 2014, 68, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Hammarstrom, A.; Wiklund, A.F.; Lindahl, B.; Larsson, C.; Ahlgren, C. Experiences of barriers and facilitators to weight-loss in a diet intervention—A qualitative study of women in Northern Sweden. BMC Womens Health 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Manheimer, E.W.; van Zuuren, E.J.; Fedorowicz, Z.; Pijl, H. Paleolithic nutrition for metabolic syndrome: Systematic review and meta-analysis. Am. J. Clin. Nutr. 2015, 102, 922–932. [Google Scholar] [CrossRef] [PubMed]
- Metzgar, M.; Rideout, T.C.; Fontes-Villalba, M.; Kuipers, R.S. The feasibility of a Paleolithic diet for low-income consumers. Nutr. Res. 2011, 31, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Genoni, A.; Lyons-Wall, P.; Lo, J.; Devine, A. Cardiovascular, Metabolic Effects and Dietary Composition of Ad-Libitum Paleolithic vs. Australian Guide to Healthy Eating Diets: A 4-Week Randomised Trial. Nutrients 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Conlon, M.A.; Bird, A.R. The impact of diet and lifestyle on gut microbiota and human health. Nutrients 2015, 7, 17–44. [Google Scholar] [CrossRef] [PubMed]
- Westman, E.C.; Yancy, W.S.; Edman, J.S.; Tomlin, K.F.; Perkins, C.E. Effect of 6-month adherence to a very low carbohydrate diet program. Am. J. Med. 2002, 113, 30–36. [Google Scholar] [CrossRef]
- Yancy, J.W.S.; Olsen, M.K.; Guyton, J.R.; Bakst, R.P.; Westman, E.C. A low-carbohydrate, ketogenic diet versus a low-fat diet to Treat obesity and hyperlipidemia: A randomized, controlled trial. Ann. Intern. Med. 2004, 140, 769–777. [Google Scholar] [CrossRef] [PubMed]
| Paleolithic (n = 22) Mean ± SD | AGHE (n = 17) Mean ± SD | p-Value 1 | |
|---|---|---|---|
| Mean total extras over the 28-day intervention | 15.9 ± 16 | 28.0 ± 17 | 0.03 |
| Mean extras per day | 0.569 ± 0.6 | 0.998 ± 0.6 | 0.03 |
| Adverse Event | Paleolithic (n = 22) | AGHE (n = 17) | Fisher’s Exact p-Value |
|---|---|---|---|
| Tiredness | 15 (68.2%) | 7 (41.2%) | 0.09 |
| Low Mood | 2 (9.1%) | 3 (17.6%) | 0.38 |
| Irritability | 2 (9.1%) | 0 (0%) | 0.31 |
| Irregular Bowel/Constipation | 4 (18.2%) | 2 (11.8%) | 0.46 |
| Diarrhoea | 5 (22.7%) | 0 (0%) | 0.046 * |
| Hungry | 8 (36.4%) | 4 (23.5%) | 0.39 |
| Muscle cramps | 3 (13.6%) | 1 (6.2%) | 0.41 |
| Headache | 8 (36.4%) | 4 (23.5%) | 0.39 |
| Bloating | 3 (13.6%) | 3 (17.6%) | 0.53 |
| Thirsty | 1 (4.5%) | 0 (0%) | 0.56 |
| Trouble sleeping | 4 (18.2%) | 0 (0%) | 0.09 |
| Dizziness | 4 (18.2%) | 1 (6.2%) | 0.26 |
| Nausea | 2 (9.1%) | 0 (0%) | 0.31 |
| Food Cravings | 4 (18.2%) | 0 (0%) | 0.09 |
| Question | Responses n (%) | p-Value † | ||
|---|---|---|---|---|
| How did you view the dietary pattern you were placed on? | Healthy | Neutral or Unhealthy | 0.21 | |
| Paleo | 16 (76.2%) | 5 (23.8%) | ||
| AGHE | 15 (93.8%) | 1 (6.2%) | ||
| Did you find your dietary pattern fit with your belief of a healthy diet? | Yes | Unsure or No | 0.005 * | |
| Paleo | 12 (57.1%) | 9 (42.9%) | ||
| AGHE | 16 (100%) | 0 (0%) | ||
| Did you find this way of eating difficult to adapt to? | Very easy or easy | Difficult or very difficult | 0.46 | |
| Paleo | 14 (66.7%) | 7 (33.3%) | ||
| AGHE | 13 (81.2%) | 3 (18.8%) | ||
| Did you feel like this way of eating was difficult once you had developed some routines with meals by the end of the study? | Very easy, easy or okay | Difficult or very difficult | 0.21 | |
| Paleo | 16 (76.2%) | 5 (23.8%) | ||
| AGHE | 15 (93.8%) | 1 (6.2%) | ||
| How would you rate your level of satisfaction or fullness after most meals? | Very full or full | Partly satisfied, still hungry, very hungry | 1.00 | |
| Paleo | 17 (80.9%) | 4 (19.1%) | ||
| AGHE | 13 (81.2%) | 3 (18.8%) | ||
| How would you rate the overall taste or palatability compared with your usual diet? | Very tasty, tasty or okay | A little unpleasant, very unpleasant | 0.12 | |
| Paleo | 17 (80.9%) | 4 (19.1%) | ||
| AGHE | 16 (100%) | 0 (0%) | ||
| Did you find it easy to cope with situations such as eating out or other social gatherings? | Very easy, easy or okay | Hard or very hard | 0.52 | |
| Paleo | 13 (61.9%) | 8 (38.1%) | ||
| AGHE | 8 (50.0%) | 8 (50.0%) | ||
| Do you feel like your desire to eat sugary foods has decreased after following this dietary pattern for a month? | Completely, somewhat | About the same or not really | 0.09 | |
| Paleo | 16 (76.2%) | 5 (23.8%) | ||
| AGHE | 7 (43.8%) | 9 (56.2%) | ||
| How would you rate your general level of health and wellbeing after your change of diet? | Feel much better, better | About the same, worse | 0.73 | |
| Paleo | 14 (66.7%) | 7 (33.3%) | ||
| AGHE | 9 (56.2%) | 7 (43.8%) | ||
| How easy did you find shopping for appropriate foods to eat from your daily checklist? | Very easy, easy, okay | Difficult, very difficult | 1.0 | |
| Paleo | 19 (90.5%) | 2 (9.5%) | ||
| AGHE | 15 (93.8%) | 1 (6.2%) | ||
| Did you notice any changes to the cost of your grocery shopping over the past month? | Much cheaper, cheaper, same | More expensive, much more expensive | 0.004 * | |
| Paleo | 10 (47.6%) | 11 (52.4%) | ||
| AGHE | 15 (93.8%) | 1 (6.2%) | ||
| Do you feel like you would recommend this style of eating to your family or friends? | Highly recommend, recommend | Maybe not, definitely not | 0.46 | |
| Paleo | 14 (66.7%) | 7 (33.3%) | ||
| AGHE | 13 (81.2%) | 3 (18.8%) | ||
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Genoni, A.; Lo, J.; Lyons-Wall, P.; Devine, A. Compliance, Palatability and Feasibility of PALEOLITHIC and Australian Guide to Healthy Eating Diets in Healthy Women: A 4-Week Dietary Intervention. Nutrients 2016, 8, 481. https://doi.org/10.3390/nu8080481
Genoni A, Lo J, Lyons-Wall P, Devine A. Compliance, Palatability and Feasibility of PALEOLITHIC and Australian Guide to Healthy Eating Diets in Healthy Women: A 4-Week Dietary Intervention. Nutrients. 2016; 8(8):481. https://doi.org/10.3390/nu8080481
Chicago/Turabian StyleGenoni, Angela, Johnny Lo, Philippa Lyons-Wall, and Amanda Devine. 2016. "Compliance, Palatability and Feasibility of PALEOLITHIC and Australian Guide to Healthy Eating Diets in Healthy Women: A 4-Week Dietary Intervention" Nutrients 8, no. 8: 481. https://doi.org/10.3390/nu8080481
APA StyleGenoni, A., Lo, J., Lyons-Wall, P., & Devine, A. (2016). Compliance, Palatability and Feasibility of PALEOLITHIC and Australian Guide to Healthy Eating Diets in Healthy Women: A 4-Week Dietary Intervention. Nutrients, 8(8), 481. https://doi.org/10.3390/nu8080481