Changes in Dairy Food and Nutrient Intakes in Australian Adolescents
Abstract
:1. Introduction
2. Subjects and Methods
2.1. Subjects
2.2. Dietary Data Collection
2.3. Weight Status and Socio-Economic Status
2.4. Data Analysis
3. Results
3.1. Subjects
3.2. Intake of Dairy Nutrients
3.3. Intake of Dairy Products by Grams
| 14 year follow-up (aged 13–15 y) | 17 year follow-up (aged 16–18 y) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nutrients | One dairy serve a | Total (n = 860) | Girls (n = 461) | Boys (n = 399) | Total (n = 860) | Girls (n = 461) | Boys (n = 399) | ||||||||||
| Mean ± SD | % meet RDI | RDI b | Mean ± SD | % meet RDI | RDI | Mean ± SD | % meet RDI | Mean ± SD | % meet RDI | RDI | Mean ± SD | % meet RDI | RDI | Mean ± SD | % meet RDI | ||
| Calcium (mg) | 300 | 1154 ± 525 | 33.0 | 1300 | 1030 ± 480 | 23.4 | 1300 | 1298 ± 539 | 44.1 | 1088 ± 592 ** | 29.2 * | 1300 | 913 ± 465 ** | 17.6 * | 1300 | 1291 ± 655 | 42.6 |
| Potassium (mg) | 318 | 3674 ± 1217 | 70.2 | AI c13 y: 2500 14–15 y: 2600 | 3476 ± 1217 | 76.4 | AI c13 y: 3000 14–15 y: 3600 | 3903 ± 1177 | 63.2 | 3408 ± 1276 ** | 56.9 ** | 2600 | 3095 ± 1113 ** | 63.3 ** | 3600 | 3771 ± 1355 | 49.4 ** |
| Phosphorus (mg) | 251 | 1599 ± 561 | 70.6 | 1250 | 1456 ± 525 | 59.2 | 1250 | 1765 ± 558 | 83.7 | 1564 ± 657 | 63.8 ** | 1250 | 1343 ± 526 ** | 51.2 ** | 1250 | 1819 ± 701 | 78.4 * |
| Magnesium (mg) | 23.6 | 309 ± 102 | 33.6 | 13 y: 240 14–15 y: 360 | 288 ± 98.9 | 31.7 | 13 y: 240 14–15 y: 410 | 335 ± 100 | 35.8 | 303 ± 115 | 20.5 ** | 360 | 269 ± 96.8 ** | 14.8** | 410 | 342 ± 122 | 27.1 ** |
| Riboflavin (mg) | 0.47 | 2.37 ± 0.95 | 93.3 | 13 y: 0.9 14–15 y: 1.1 | 2.13 ± 0.85 | 91.8 | 13 y: 0.9 14–15 y: 1.3 | 2.65 ± 0.98 | 95.0 | 2.24 ± 1.03 ** | 88.0 ** | 1.1 | 1.91 ± 0.84 ** | 84.9 ** | 1.3 | 2.63 ± 1.10 | 91.6 |
| Vitamin A d (μg) | 86.7 | 1219 ± 582 | 83.7 | 13 y: 600 14–15 y: 700 | 1176 ± 610 | 87.0 | 13 y: 600 14–15 y: 900 | 1269 ± 543 | 79.9 | 1091 ± 802 ** | 67.5 ** | 700 | 1030 ± 716 ** | 70.6 ** | 900 | 1161 ± 887 * | 63.7 ** |
| Vitamin B12 (mg) | n/a | 4.34 ± 2.12 | 88.7 | 13 y: 1.8 14–15 y: 2.4 | 3.93 ± 2.10 | 84.2 | 13 y: 1.8 14–15 y: 2.4 | 4.81 ± 2.03 | 94.0 | 4.41 ± 2.76 | 83.2 ** | 2.4 | 3.70 ± 2.34 ** | 75.1 ** | 2.4 | 5.23 ± 2.98 * | 92.7 |
| Zinc (mg) | 1.12 | 12.5 ± 4.1 | 78.5 | 13 y: 6 14–15 y: 7 | 11.5 ± 3.8 | 90.9 | 13 y: 6 14–15 y: 13 | 13.5 ± 4.1 | 64.2 | 12.2 ± 4.8 | 68.7 ** | 7 | 10.5 ± 4.0 ** | 81.6 ** | 13 | 14.1 ± 4.9 * | 53.4 ** |
| Energy (MJ) | 842 | 9.42 ± 2.89 | n/a | n/a | 8.74 ± 2.78 | n/a | n/a | 10.20 ± 2.82 | n/a | 9.35 ± 3.37 | n/a | n/a | 8.00 ± 2.64 ** | n/a | n/a | 10.90 ± 3.47 ** | n/a |
| Protein (g) | 9.67 | 92.7 ± 28.9 | 95.1 | 13 y: 35 14–15 y: 45 | 85.3 ± 27.3 | 96.7 | 13 y: 40 14–15 y: 65 | 101 ± 28.4 | 93.2 | 92.2 ± 36.1 | 89.5 ** | 45 | 79.1 ± 28.8 ** | 90.9 ** | 65 | 107.3 ± 37.9 ** | 88.0 ** |
| Saturated fat (g) | 5.77 | 39.0 ± 15.8 | n/a | n/a | 35.7 ± 14.5 | n/a | n/a | 42.8 ± 16.5 | n/a | 37.1 ± 18.3 ** | n/a | n/a | 30.7 ± 14.4 ** | n/a | n/a | 44.6 ± 19.6 | n/a |
| Mono-unsaturated fat (g) | 2.13 | 30.8 ± 11.2 | n/a | n/a | 28.5 ± 10.3 | n/a | n/a | 33.4 ± 11.7 | n/a | 28.7 ± 12.4 ** | n/a | n/a | 24.1 ± 9.73 ** | n/a | n/a | 34.0 ± 13.2 | n/a |
| Poly-unsaturated fat (g) | 0.27 | 13.5 ± 6.5 | n/a | n/a | 12.8 ± 6.1 | n/a | n/a | 14.2 ± 6.9 | n/a | 11.7 ± 6.5 ** | n/a | n/a | 10.4 ± 5.7 ** | n/a | n/a | 13.3 ± 7.1 * | n/a |
| Dairy product | 14 year follow-up | 17 year follow-up | ||||
|---|---|---|---|---|---|---|
| Total (n = 860) Mean ± SD | Boys (n = 399) Mean ± SD | Girls (n = 461) Mean ± SD | Total Mean ± SD | Boys (n = 399) Mean ± SD | Girls (n = 461) Mean ± SD | |
| Total dairy (g) | 523 ± 326 | 622 ± 349 | 437 ± 279 | 452 ± 330 ** | 570 ± 372 ** | 350 ± 246 ** |
| Consumers (%) | 99.9 | 100 | 99.8 | 99.8 | 99.7 | 99.8 |
| Consumer intake (g) # | 523 ± 326 | 622 ± 349 | 438 ± 278 | 453 ± 329 | 571 ± 371 | 350 ± 246 |
| Total milk (g) | 424 ± 307 | 517 ± 335 | 343 ± 254 | 368 ± 309 ** | 479 ± 353 * | 272 ± 225 ** |
| Consumers (%) | 98.7 | 99.2 | 98.3 | 97.3 * | 98.2 | 96.5 |
| Consumer intake (g) # | 429 ± 305 | 521 ± 333 | 349 ± 252 | 378 ± 307 | 488 ± 350 | 281 ± 223 |
| Regular milk (g) | 205 ± 297 | 269 ± 362 | 149 ± 212 | 153 ± 260 ** | 223 ± 18 ** | 92 ± 176 ** |
| Consumers (%) | 55.0 | 55.1 | 54.9 | 48.7 ** | 53.4 | 44.7 ** |
| Consumer intake (g) # | 373 ± 313 | 488 ± 361 | 273 ± 221 | 314 ± 298 | 419 ± 329 | 206 ± 214 |
| Reduced fat milk (g) | 150 ± 253 | 167 ± 267 | 136 ± 238 | 138 ± 240 | 160 ± 285 | 118 ± 191 |
| Consumers (%) | 42.2 | 40.9 | 43.4 | 42.8 | 39.8 | 45.3 |
| Consumer intake (g) # | 357 ± 279 | 410 ± 276 | 314 ± 274 | 323 ± 274 | 403 ± 326 | 262 ± 207 |
| Skim milk (g) | 17.6 ± 85.9 | 20.8 ± 98.8 | 14.8 ± 72.9 | 23.8 ± 101 | 19.9 ± 97.8 | 27.2 ± 104 * |
| Consumers (%) | 6.3 | 6.0 | 6.5 | 9.5 ** | 7.3 | 11.5 ** |
| Consumer intake (g) # | 280 ± 211 | 346 ± 226 | 227±185 | 250 ± 228 | 275 ± 252 | 237 ± 215 |
| Milkshakes (g) | 22.1 ± 39.2 | 24.7 ± 41.7 | 19.8 ± 36.8 | 17.1 ± 37.1 ** | 23.3 ± 47.1 | 11.7 ± 24.3 ** |
| Consumers (%) | 56.3 | 57.8 | 54.8 | 48.2 ** | 51.7 | 45.0 ** |
| Consumer intake (g) # | 39.3 ± 45.4 | 42.3 ± 47.3 | 36.6 ± 43.5 | 36.2 ± 47.1 | 45.7 ± 57.6 | 26.5 ± 30.7 |
| Flavored milk (g) | 25.3 ± 56.0 | 31.6 ± 69.5 | 19.8 ± 40.1 | 33.7 ± 78.0 ** | 49.0 ± 103 ** | 20.5 ± 42.3 |
| Consumers (%) | 59.1 | 66.6 | 52.2 | 54.2 | 59.3 | 49.6 |
| Consumer intake (g) # | 42.9 ± 67.6 | 47.7 ± 80.8 | 37.7 ± 48.9 | 62.6 ± 97.4 | 82.4 ± 123 | 41.9 ± 52.5 |
| Total cheese (g) | 20.7 ± 17.6 | 20.5 ± 18.8 | 20.8 ± 16.5 | 24.2 ± 28.3 ** | 26.0 ± 29.4 ** | 22.5 ± 27.1 |
| Consumers (%) | 98.4 | 98.5 | 98.3 | 96.0 ** | 96.7 | 95.4 * |
| Consumer intake (g) # | 21.0 ± 17.6 | 20.8 ± 18.8 | 21.2 ± 16.4 | 25.1 ± 28.4 | 26.9 ± 29.5 | 23.6 ± 27.2 |
| Regular cheese (g) | 11.2 ± 15.0 | 11.3 ± 17.7 | 11.1 ± 12.2 | 13.1 ± 21.1 ** | 14.6 ± 21.6 ** | 11.9 ± 20.5 |
| Consumers (%) | 75.7 | 74.4 | 76.8 | 72.3 ** | 73.2 ** | 71.6 ** |
| Consumer intake (g) # | 13.5 ± 14.5 | 14.6 ± 17.2 | 12.5 ± 11.8 | 18.2 ± 22.9 | 20.0 ± 23.1 | 16.6 ± 22.6 |
| Reduced fat cheese (g) (including cottage cheese) | 6.52 ± 10.9 | 5.85 ± 9.40 | 7.09 ± 11.9 | 7.72 ± 17.1 * | 7.19 ± 16.4 | 8.19 ± 17.7 |
| Consumers (%) | 47.6 | 45.6 | 49.2 | 43.4 * | 38.1 * | 47.9 |
| Consumer intake (g) # | 9.4 ± 12.7 | 8.5 ± 10.6 | 10.0 ± 14.2 | 17.8 ± 22.3 ** | 18.9 ± 22.2 ** | 17.1 ± 22.5 ** |
| Cheese from pizza (g) | 2.7 ± 2.6 | 3.0 ± 3.0 | 2.4 ± 2.2 | 3.0 ± 4.2 ** | 3.9 ± 5.3 ** | 2.3 ± 2.8 |
| Consumers (%) | 86.5 | 87.0 | 86.1 | 81.7 ** | 86.7 | 77.4 ** |
| Consumer intake (g) # | 3.1 ± 2.6 | 3.4 ± 2.9 | 2.7 ± 2.2 | 3.7 ± 4.4 | 4.5 ± 5.5 | 3.0 ± 2.8 |
| Total yoghurt (g) | 50.5 ± 62.9 | 52.9 ± 66.2 | 48.4 ± 59.9 | 35.5 ± 59.2 ** | 36.0 ± 60.3 ** | 35.0 ± 58.4 ** |
| Consumers (%) | 73.6 | 71.9 | 75.1 | 60.5 ** | 58.6 ** | 62.0 ** |
| Consumer intake (g) # | 68.7 ± 64.3 | 73.6 ± 67.6 | 64.5 ± 61.2 | 58.7 ± 66.6 | 61.5 ± 68.1 | 56.5 ± 65.4 |
| Regular yoghurt (g) | 16.9 ± 43.5 | 18.3 ± 49.1 | 15.7 ± 38.1 | 12.7 ± 42.7 * | 16.5 ± 48.6 | 9.36 ± 36.5 ** |
| Consumers (%) | 26.6 | 25.8 | 27.3 | 21.2 ** | 26.1 | 16.9 ** |
| Consumer intake (g) # | 63.6 ± 64.6 | 70.9 ± 75.2 | 57.6 ± 53.9 | 60.1 ± 76.1 | 63.6 ± 78.2 | 55.3 ± 73.4 |
| Reduced fat yoghurt (g) | 33.4 ± 56.5 | 34.3 ± 56.8 | 32.6 ± 56.3 | 22.7 ± 47.6 ** | 19.2 ± 43.6 ** | 25.7 ± 50.6 * |
| Consumers (%) | 46.5 | 45.4 | 47.5 | 39.1 ** | 32.3 ** | 44.9 |
| Consumer intake (g) # | 71.8 ± 64.2 | 75.6 ± 63.3 | 68.7 ± 64.8 | 58.1 ± 61.1 | 59.5 ± 59.2 | 57.2 ± 62.4 |
| Dairy from milk dishes a (g) | 3.2 ± 8.1 | 3.7 ± 9.7 | 2.7 ± 6.384 | 2.6 ± 7.8 | 3.3 ± 9.5 | 1.9 ± 6.00 |
| Consumers (%) | 31.2 | 34.1 | 28.6 | 22.9 ** | 25.3 ** | 20.8 ** |
| Consumer intake (g) # | 10.2 ± 11.8 | 10.9 ± 4.0 | 9.46 ± 8.87 | 11.2 ± 13.1 | 12.9 ± 15.2 | 9.35 ± 10.2 |
| Total ice cream (g) | 17.6 ± 15.1 | 18.8 ± 14.8 | 16.4 ± 15.3 | 12.4 ± 13.9 ** | 14.1 ± 16.1 ** | 11.0 ± 11.5 ** |
| Consumers (%) | 96.1 | 96.9 | 95.4 | 88.1 ** | 87.4 ** | 88.8 ** |
| Consumer intake (g) # | 18.2 ± 14.9 | 19.4 ± 14.5 | 17.1 ± 15.2 | 14.1 ± 13.9 | 15.9 ± 16.2 | 12.5 ± 11.5 |
| Regular ice cream (g) | 15.3 ± 14.6 | 16.3 ± 14.4 | 14.5 ± 14.9 | 10.9 ± 13.6 ** | 12.8 ± 15.8 ** | 9.34 ± 11.1 ** |
| Consumers (%) | 94.5 | 95.7 | 93.5 | 85.6 ** | 85.5 ** | 85.7 ** |
| Consumer intake (g) # | 16.2 ± 14.6 | 17.0 ± 14.3 | 15.5 ± 14.8 | 12.8 ± 13.9 | 14.9 ± 16.1 | 10.9 ± 11.2 |
| Reduced fat ice cream (g) | 2.3 ± 6.9 | 2.6 ± 7.2 | 2.0 ± 6.6 | 1.5 ± 4.1 ** | 1.3 ± 4.3 ** | 1.7 ± 3.8 |
| Consumers (%) | 27.6 | 27.3 | 27.8 | 28.6 | 23.3 | 33.2 |
| Consumer intake (g) # | 8.3 ± 11.1 | 9.4 ± 11.3 | 7.3 ± 10.9 | 5.3 ± 6.1 | 5.6 ± 7.5 | 5.1 ± 5.1 |
| Butter (g) | 4.8 ± 10.5 | 5.5 ± 11.6 | 4.2 ± 9.5 | 7.2 ± 12.1 ** | 8.8 ± 14.6 ** | 5.7 ± 9.3 ** |
| Consumers (%) | 21.2 | 22.6 | 20.0 | 36.7 ** | 38.1 ** | 35.6 ** |
| Consumer intake (g) # | 22.5 ± 11.1 | 24.3 ± 11.5 | 20.8 ± 10.4 | 19.5 ± 12.6 | 23.2 ± 15.0 | 16.1 ± 8.7 |
| Cream (g) | 0.9 ± 2.3 | 0.9 ± 2.1 | 0.9 ± 2.5 | 0.8 ± 4.0 | 0.8 ± 5.4 | 0.7 ± 2.1 |
| Consumers (%) | 34.9 | 35.6 | 34.3 | 24.5 ** | 23.6 ** | 25.4 ** |
| Consumer intake (g) # | 2.7 ± 3.3 | 2.6 ± 2.9 | 2.7 ± 3.7 | 3.2 ± 7.6 | 3.6 ± 10.7 | 2.8 ± 3.3 |
| Custard (g) | 4.9 ± 12.1 | 6.5 ± 15.2 | 3.4 ± 8.3 | 3.8 ± 11.4 * | 4.8 ± 13.5 | 2.9 ± 9.07 |
| Consumers (%) | 37.6 | 42.4 | 33.4 | 27.7 ** | 31.3 ** | 24.5 ** |
| Consumer intake (g) # | 13.0 ± 16.9 | 15.2 ± 20.3 | 10.6 ± 11.6 | 13.6 ± 18.4 | 15.2 ± 20.8 | 11.8 ± 15.2 |
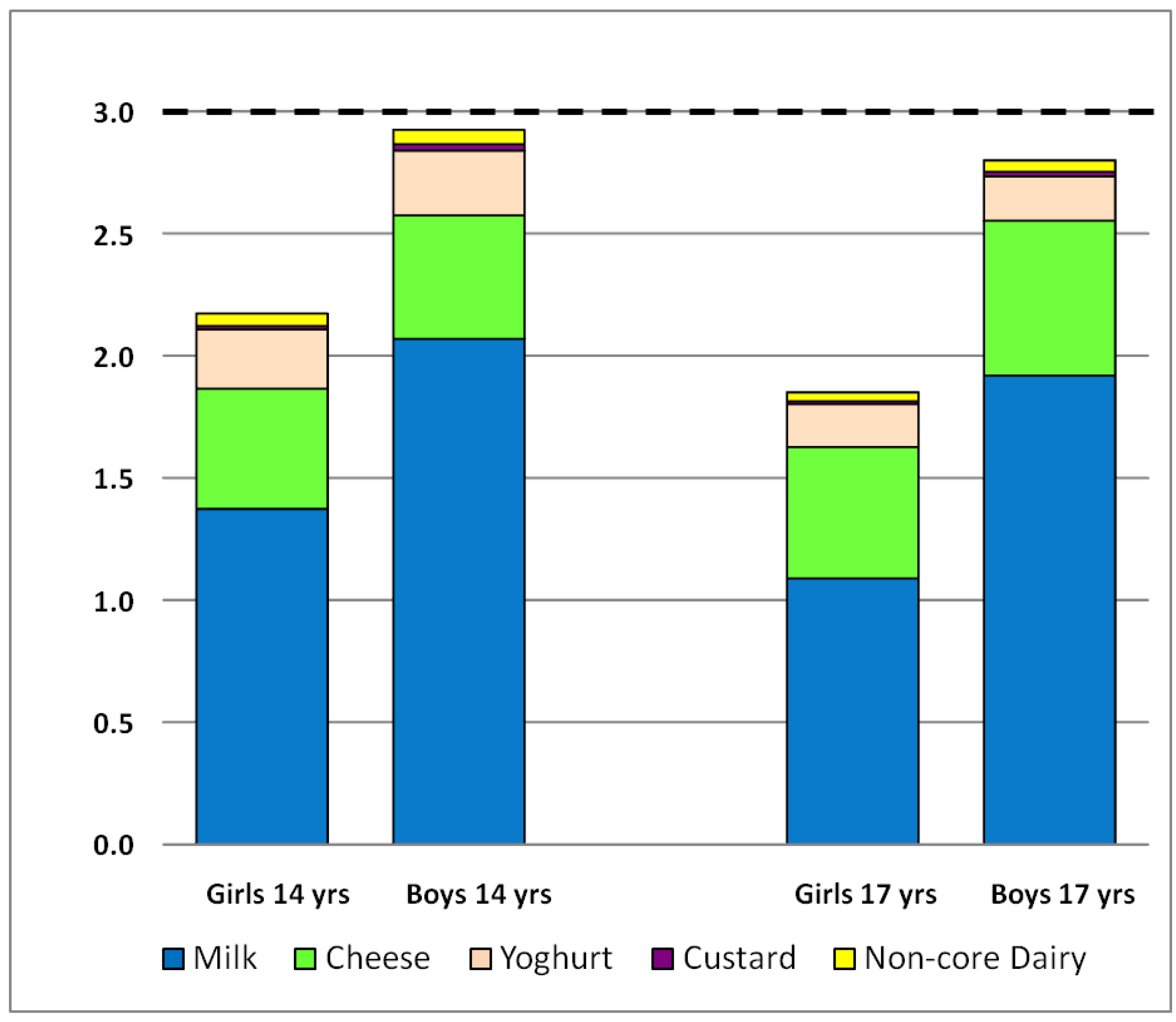
3.4. Intake of Dairy Products by Serves
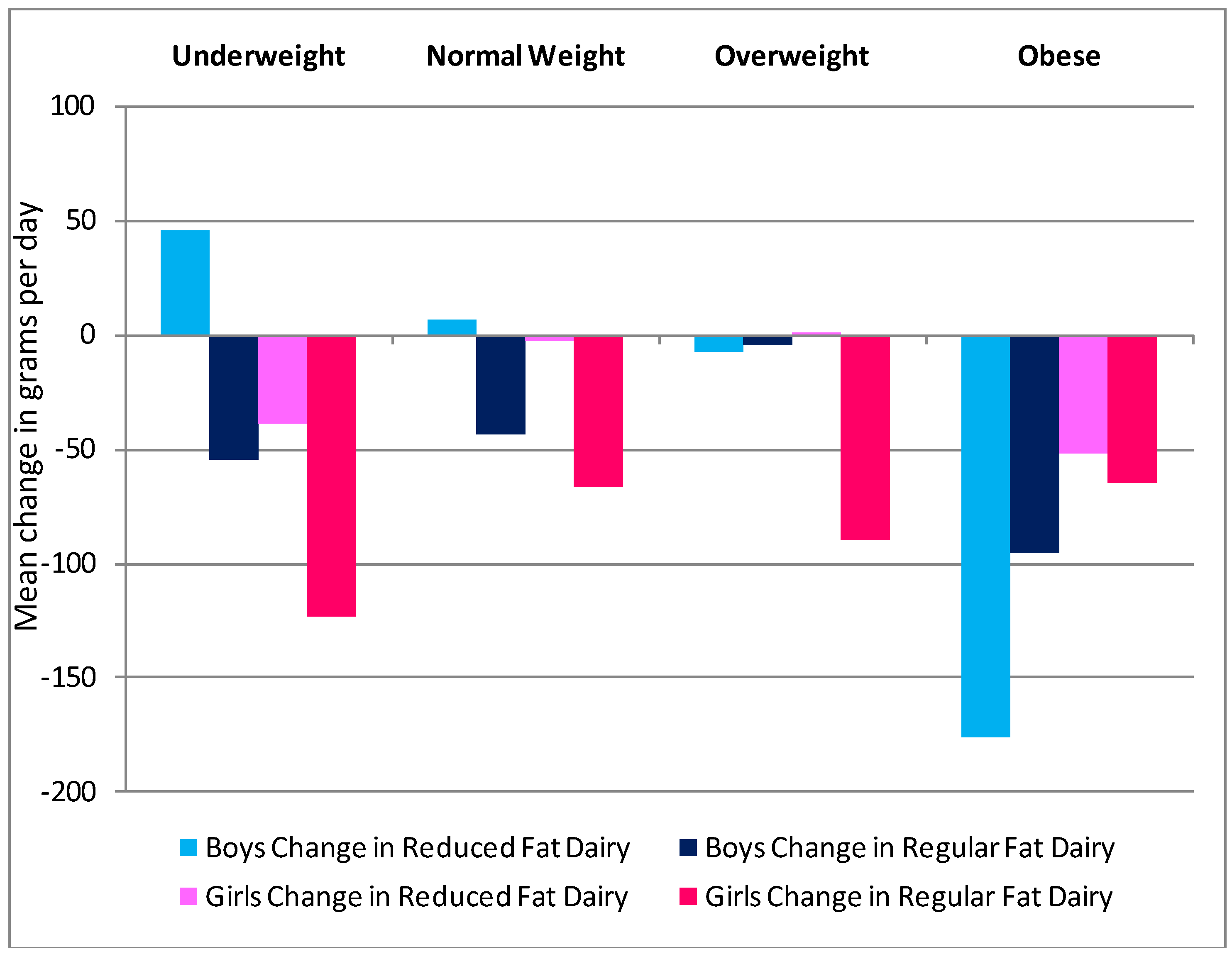
3.5. Gender, BMI and SES as Predictors of Change in Dairy Intake

4. Discussion
5. Conclusions
Acknowledgments
Conflict of Interest
References
- Shils, M.S. Modern Nutrition in Health and Disease, 10th ed; Lipponcott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar]
- Heaney, R.P. Dairy and bone health. J. Am. Coll. Nutr. 2009, 28, 81–90. [Google Scholar]
- Huncharek, M.; Muscat, J.; Kupelnick, B. Impact of dairy products and dietary calcium on bone-mineral content in children: Results of a meta analysis. Bone 2008, 2, 312–321. [Google Scholar]
- Lanou, A.J.; Berkow, S.E.; Barnard, N.D. Calcium, dairy products and bone health in children and young adults: A reevaluation of the evidence. Pediatrics 2005, 115, 736–743. [Google Scholar] [CrossRef]
- Bischoff-Ferrari, H.A.; Dawson-Hughes, B.; Baron, J.A.; Kanis, J.A.; Orav, E.J.; Staehelin, H.B.; Kiel, D.P.; Burckhardt, P.; Henschkowski, J.; Spiegelman, D.; et al. Milk intake and risk of hip fracture in men and women: A meta-analysis of prospective cohort studies. J. Bone Miner. Res. 2011, 26, 833–839. [Google Scholar]
- Stipanuk, M.H. Biochemical, Physiological, andMolecular Aspects of Human Nutrition, 2nd ed; Saunders Elsevier: St. Louis, MO, USA, 2006. [Google Scholar]
- Elwood, P.; Pickering, J.; Givens, D.; Gallacher, J. The consumption of milk and dairy foods and the incidence of vascular disease and diabetes: An overview of the evidence. Lipids 2010, 45, 925–939. [Google Scholar] [CrossRef]
- National Health and Medical Research Council, Dietary Guidelines for Children and Adolescents in Australia; Commonwealth of Australia: Canberra, Australia, 2003.
- National Health and Medical Research Council, Dietary Guidelines for Australian Adults; Commonwealth of Australia: Canberra, Australia, 2003.
- Martin, A.D.; Bailey, D.A.; McKay, H.A.; Whiting, S. Bone mineral and calcium accretion during puberty. Am. J. Clin. Nutr. 1997, 66, 611–615. [Google Scholar]
- Kalkwarf, H.J.; Khoury, J.C.; Lanphear, B.P. Milk intake during childhood and adolescence, adult bone density and osteoporotic fractures in US women. Am. J. Clin. Nutr. 2003, 77, 257–265. [Google Scholar]
- Baroncelli, G.I.; Bertelloni, S.; Sordini, F.; Saggese, G. Osteoporosis in children and adolescents: Etiology and management. Paediatr. Drugs 2005, 7, 295–323. [Google Scholar] [CrossRef]
- US Department of Human Services, Bone Halth and Osteoporosis: A Surgeons Report; US Department of Health and Human Services: Rockville, MD, USA, 2004.
- Sanders, K.M.; Nowson, C.A.; Kotowicz, M.A.; Briffa, K.; Devine, A.; Reid, I.R. Calcium and bone health: Position statement for the Australian and New Zealand Bone and Mineral Society, Osteoporosis Australia and the Endocrine Society of Australia. Med. J. Aust. 2007, 190, 316–320. [Google Scholar]
- Birch, L.L.; Fisher, J.O. Development of eating behaviors among children and adolescents. Pediatrics 1998, 101, 539–549. [Google Scholar]
- Kelder, S.H.; Perry, C.L.; Klepp, K.I.; Lytle, L.L. Longitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. Am. J. Public Health 1994, 84, 1121–1126. [Google Scholar] [CrossRef]
- Spear, B.A. Adolescent growth and development. J. Am. Diet. Assoc. 2002, 102, S23–S29. [Google Scholar] [CrossRef]
- Siega-Riz, A.M.; Carson, T.; Popkin, B. Three squares or mostly snacks—what do teens really eat? A sociodemographic study of meal patterns. J. Adolesc. Health 1998, 22, 29–36. [Google Scholar] [CrossRef]
- 2007 Australian National Childrens Nutrition and Physical Activity Survey—Main Findings. Commonwealth of Australia: Canberra, Austrilia, 2008.
- Neumark-Sztainer, D.; Story, M.; Dixon, L.; Resnick, M.D.; Blum, R.V. Correlates of inadequate consumption of dairy products among adolescents. J. Nutr. Educ. 1997, 29, 12–19. [Google Scholar] [CrossRef]
- Martin, K.; Rosenberry, M.; Miller, M.; French, S.; McCormack, G.; Bull, F.; Giles-Corti, B.; Pratt, S. Child and Adolescent Physical Activity and Nutrition Survey WA Final Report 2008: Key Findings; Western Australian Government: Perth, Australia, 2009. [Google Scholar]
- Abbott, R.; Macdonald, D.; Stubbs, C.; Lee, A.; Harper, C.; Gedge, V.; Davies, P. The Healthy Kids Queensland Survey: Key findings. J. Sci. Med. Sport 2007, 10, 26. [Google Scholar]
- NSW Centre for Overweight and Obesity, NSW School Physical Activity and Nutrition Survey (SPANS) 2004: Short Report; NSW Department of Health: Sydney, Austrilia, 2006.
- Baird, D.L.; Syrette, J.; Hendrie, G.A.; Riley, M.D.; Bowen, J.; Noakes, M. Dairy food intake of Australian children and adolescents 2–16 years of age: 2007 Australian National Children’s Nutrition and Physical Activity Survey. Public Health Nutr. 2012, 15, 2060–2073. [Google Scholar] [CrossRef]
- Newnham, J.P.; Evans, S.F.; Michael, C.A.; Stanley, F.J.; Landau, L.I. Effects of frequent ultrasound during pregnancy: A randomised controlled trial. Lancet 1993, 342, 887–891. [Google Scholar]
- Baghurst, K.I.; Recird, S.J. A computerized dietary analysis system for use with diet diaries or food frequency questionnaires. Community Health Stud. 1984, 8, 11–18. [Google Scholar] [CrossRef]
- Ambrosini, G.L.; de Klerk, N.H.; O’Sullivan, T.A.; Beilin, L.J.; Oddy, W.H. The reliability of a food frequency questionnaire for use among adolescents. Eur.J. Clin. Nutr. 2009, 63, 1251–1259. [Google Scholar] [CrossRef]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity world-wide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar]
- Cole, T.J.; Flegal, K.M.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 2007, 335, 194–201. [Google Scholar]
- Australian Bureau of Statistics SEIFA Socio-Economic Indexes for Areas. Available online: http://www.abs.gov.au (accessed on 20 February 2012).
- The Trustees of the Home Economics Teachers Group, Baldwin, E.M.; Barrowman, E.M.; Cameron, S.; McDonnell, E.D.; Russell, S.M.; Williams, W.I. Cookery—The Australian Way; McMillan of Australia: Melbourne, Australia, 1967. [Google Scholar]
- Taste Australia. Available online: http://www.taste.com.au/ (accessed on 20 April 2012).
- National Health and Medical Research Council, The Australian Guide to Healthy Eating; Commonwealth of Australia: Canberra, Australia, 2003.
- Australian Government; Department of Aging; National Health and Medical Research Council, Nutrient Reference Values for Australia and New Zealand: Including Recommended Dietary Intakes; NHMRC: Canberra, Australia, 2005.
- Rockett, H.R.; Breitenbach, M.; Frazier, A.L.; Witschi, J.; Wolf, A.M.; Field, A.E.; Colditz, G.A. Validation of a youth/adolescent food frequency questionnaire. Prev. Med. 1997, 26, 808–816. [Google Scholar] [CrossRef]
- Lumley, T.; Diehr, P.; Emerson, S.; Chen, L. The importance of the normality assumption in large public health data sets. Ann. Rev. Public Health 2002, 23, 151–169. [Google Scholar]
- Portsmouth, K.; Henderson, K.; Graham, N.; Price, R.; Cole, J.; Allen, J. Dietary calcium intake in 18 year old women: Comparison with recommended daily intake and dietary energy intake. J. Adv. Nurs. 1994, 20, 1073–1078. [Google Scholar]
- Larson, N.I.; Neumark-Sztainer, D.; Harnack, L.; Wall, M.; Story, M.; Eisenberg, M.E. Calcium and dairy intake: Longitudinal trends during transition to young adulthood and correlates of calcium intake. J. Nutr. Educ. Behav. 2009, 41, 254–264. [Google Scholar] [CrossRef]
- Ali, N.; Siktberg, L. Osteoporosis prevention in female adolescents: Calcium intake and exercise participation. Pediatr. Nurs. 2001, 27, 135–139. [Google Scholar]
- Chan, G.M. Dietary calcium and bone mineral status of children and adolescents. Am. J. Dis. Child. 1991, 145, 631–634. [Google Scholar]
- Cashman, K.D. Calcium intake, calcium bioavailability and bone health. Br. J. Nutr. 2002, 87, S169–S177. [Google Scholar] [CrossRef]
- Mahan, L.K.; Escot-Stump, S. Krause’s Food and Nutrition Therapy, 12th ed; Saunders Elsevier Evolve: St. Louis, MO, USA, 2008. [Google Scholar]
- Huerta, M.G.; Roemmich, J.N.; Kington, M.L.; Bovbjerg, V.E.; Weltman, A.L.; Holmes, V.F.; Patrie, J.T.; Rogol, A.D.; Nadler, J.L. Magnesium deficiency is associated with insulin resistance in obese children. Diabetes Care 2005, 28, 1175–1181. [Google Scholar] [CrossRef]
- Lunt, M.; Masaryk, P.; Scheidt-Nave, C.; Nijis, J.; Poor, G.; Pols, H.; Falch, J.A.; Hammermeister, G.; Reid, D.M.; Benevolenskaya, L.; et al. The effects of lifestyle, dietary dairy intake and diabetes on bone mineral density and vertebral deformity prevalence: The EVOS study. Osteoporosis Int. 2001, 12, 688–698. [Google Scholar] [CrossRef]
- Malik, V.S.; Sun, Q.; van Dam, R.M.; Rimm, E.B.; Willett, W.C.; Rosner, B.; Hu, F.B. Adolescent dairy product consumption and risk of type 2 diabetes in middle-aged women. Am. J. Clin. Nutr. 2011, 94, 854–861. [Google Scholar] [CrossRef]
- Doidge, J.C.; Segal, L. Most Australians do not meet recommendations for dairy consumption: Findings of a new technique to analyse nutrition surveys. Aust. N. Z.J. Public Health 2012, 36, 236–240. [Google Scholar] [CrossRef]
- McLennan, W.; Podger, A. National Nutrition Survey: Foods Eaten, Australia 1995; Commonwealth of Australia: Canberra, Australia, 1999. [Google Scholar]
- Coffee kick: The undisputed champion of the flavoured milk world just keeps getting stronger. Convenience & Impulse Retailing, Sep/Oct 2009; Available online: http://www.c-store.com.au/article-archive/2009-sept-oct-coffee-kick (accessed on 12 October 2012).
- NCLS Research Profiling Australians: Blue-collar worker. Available online: http://www.ncls.org.au (accessed on 3 October 2012).
- Outerspace Case Study: Farmers Union Iced Coffee Stubby. Available online: http://www.outerspacedesign.com/index.php?id=117 (accessed on 12 October 2012).
- Packard, P.; Krugstrand, K.S. Half of rural girls aged 8–17 report concerns and dietary changes, with both more prevalent with age. J. Am. Diet. Assoc. 2002, 102, 672–677. [Google Scholar] [CrossRef]
- Louie, J.C.Y.; Flood, V.M.; Hector, D.J.; Rangan, A.M.; Gill, T.P. Dairy consumption and overweight and obesity: A systematic review of prospective cohort studies. Obes. Rev. 2011, 12, e582–e592. [Google Scholar] [CrossRef]
- Abargouei, A.S.; Janghorbani, M.; Salehi-Marzijarani, M.; Esmaillzadeh, A. Effect of dairy consumption on weight and body composition in adults: A systematic review and meta-analysis of randomized controlled clinical trials. Int. J. Obes. [CrossRef]
- Cade, J.; Thompson, R.; Burley, V.; Warm, D. Development, validation and utilisation of food-frequency questionnaires—a review. Public Health Nutr. 2002, 5, 567–587. [Google Scholar] [CrossRef]
- Ambrosini, G.L.; O’Sullivan, T.A.; de Klerk, N.H.; Movi, T.A.; Beilin, L.J.; Oddy, W.H. Relative validity of adolescent dietary patterns: A comparison of a food frequency questionnaire and a 3 day food record. Br. J. Nutr. 2011, 105, 625–633. [Google Scholar] [CrossRef]
- O’Sullivan, T.A.; Ambrosini, G.L.; Beilin, L.J.; Mori, T.A.; Oddy, W.H. Dietary intake and food sources of fatty acids in Australian adolescents. Nutrition 2011, 27, 153–159. [Google Scholar] [CrossRef]
- Li, J.; Kendall, G.E.; Henderson, S.; Downie, J.; Landsborough, L.; Oddy, W.H. Maternal psychosocial well-being in pregnancy and breastfeeding duration. Acta Paediatr. 2008, 97, 221–225. [Google Scholar] [CrossRef]
- Hendrie, G.A.; Brindal, E.; Baird, D.; Gardner, C. Improving children’s dairy food and calcium intake: Can intervention work? A systematic review of the literature. Public Health Nutr. 2012. [Google Scholar] [CrossRef]
- Bolland, M.J.; Grey, A.; Avenell, A.; Gamble, G.D.; Reid, I.R. Calcium supplements with or without vitamin D and risk of cardiovascular events: Reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ 2011, 342, d2040. [Google Scholar]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Parker, C.E.; Vivian, W.J.; Oddy, W.H.; Beilin, L.J.; Mori, T.A.; O'Sullivan, T.A. Changes in Dairy Food and Nutrient Intakes in Australian Adolescents. Nutrients 2012, 4, 1794-1811. https://doi.org/10.3390/nu4121794
Parker CE, Vivian WJ, Oddy WH, Beilin LJ, Mori TA, O'Sullivan TA. Changes in Dairy Food and Nutrient Intakes in Australian Adolescents. Nutrients. 2012; 4(12):1794-1811. https://doi.org/10.3390/nu4121794
Chicago/Turabian StyleParker, Carole E., Wendy J. Vivian, Wendy H. Oddy, Lawrence J. Beilin, Trevor A. Mori, and Therese A. O'Sullivan. 2012. "Changes in Dairy Food and Nutrient Intakes in Australian Adolescents" Nutrients 4, no. 12: 1794-1811. https://doi.org/10.3390/nu4121794




