Evaluation of a Novel Enteral Phosphorus Therapy with Enteral Nutrition during a National Intravenous Sodium Phosphate Shortage
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brown, K.A.; Dickerson, R.N.; Morgan, L.M.; Alexander, K.H.; Minard, G.; Brown, R.O. A new graduated dosing regimen for phosphorus replacement in patients receiving nutrition support. JPEN J. Parenter. Enteral Nutr. 2006, 30, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Calvo, M.S.; Moshfegh, A.J.; Tucker, K.L. Assessing the health impact of phosphorus in the food supply: Issues and considerations. Adv. Nutr. 2014, 5, 104–113. [Google Scholar] [CrossRef]
- da Silva, J.S.V.; Seres, D.S.; Sabino, K.; Adams, S.C.; Berdahl, G.J.; Citty, S.W.; Cober, M.P.; Evans, D.C.; Greaves, J.R.; Gura, K.M.; et al. ASPEN consensus recommendations for refeeding syndrome. Nutr. Clin. Pract. 2020, 35, 178–195. [Google Scholar] [CrossRef]
- Heaney, R.P. Phosphorus nutrition and the treatment of osteoporosis. Mayo Clin. Proc. 2004, 79, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Gulbis, B.E.; Ruiz, M.C.; Denktas, A.E. The impact of drug shortages on the pharmacy, nursing, and medical staff’s ability to effectively care for critically ill patients. Crit. Care Nurs. Q. 2013, 36, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Erstad, B.L. Dosing of medications in morbidly obese patients in the intensive care unit setting. Intensive Care Med. 2004, 30, 18–32. [Google Scholar] [CrossRef] [PubMed]
- Dickerson, R.N.; Pitts, S.L.; Maish, G.O., 3rd; Schroeppel, T.J.; Magnotti, L.J.; Croce, M.A.; Minard, G.; Brown, R.O. A reappraisal of nitrogen requirements for patients with critical illness and trauma. J. Trauma. Acute Care Surg. 2012, 73, 549–557. [Google Scholar] [CrossRef]
- Bliss, D.Z.; Guenter, P.A.; Settle, R.G. Defining and reporting diarrhea in tube-fed patients—What a mess! Am. J. Clin. Nutr. 1992, 55, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Aubier, M.; Murciano, D.; Lecocguic, Y.; Viires, N.; Jacquens, Y.; Squara, P.; Pariente, R. Effect of hypophosphatemia on diaphragmatic contractility in patients with acute respiratory failure. N. Engl. J. Med. 1985, 313, 420–424. [Google Scholar] [CrossRef]
- Zazzo, J.F.; Troche, G.; Ruel, P.; Maintenant, J. High incidence of hypophosphatemia in surgical intensive care patients: Efficacy of phosphorus therapy on myocardial function. Intensive Care Med. 1995, 21, 826–831. [Google Scholar] [CrossRef]
- Sheldon, G.F.; Grzyb, S. Phosphate depletion and repletion: Relation to parenteral nutrition and oxygen transport. Ann. Surg. 1975, 182, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Silvis, S.E.; Paragas, P.D., Jr. Paresthesias, weakness, seizures, and hypophosphatemia in patients receiving hyperalimentation. Gastroenterology 1972, 62, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Weinsier, R.L.; Krumdieck, C.L. Death resulting from overzealous total parenteral nutrition: The refeeding syndrome revisited. Am. J. Clin. Nutr. 1981, 34, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Liamis, G.; Milionis, H.J.; Elisaf, M. Medication-induced hypophosphatemia: A review. QJM 2010, 103, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Barak, V.; Schwartz, A.; Kalickman, I.; Nisman, B.; Gurman, G.; Shoenfeld, Y. Prevalence of hypophosphatemia in sepsis and infection: The role of cytokines. Am. J. Med. 1998, 104, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, R.; Khardori, R. Severe hypophosphatemia. Pathophysiologic implications, clinical presentations, and treatment. Medicine 2000, 79, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, K.A.; Brown, R.O.; Maish, G.O., 3rd; Croce, M.A.; Minard, G.; Dickerson, R.N. Influence of traumatic brain injury on potassium and phosphorus homeostasis in critically ill multiple trauma patients. Nutrition 2010, 26, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Frankenfield, D.C.; Coleman, A.; Alam, S.; Cooney, R.N. Analysis of estimation methods for resting metabolic rate in critically ill adults. JPEN J. Parenter. Enteral Nutr. 2009, 33, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Dickerson, R.N.; Melnik, G. Osmolality of oral drug solutions and suspensions. Am. J. Hosp. Pharm. 1988, 45, 832–834. [Google Scholar] [CrossRef]
- Dickerson, R.N.; Crawford, C.N.; Tsiu, M.K.; Bujanowski, C.E.; Van Matre, E.T.; Swanson, J.M.; Filiberto, D.M.; Minard, G. Augmented renal clearance following traumatic injury in critically ill patients requiring nutrition therapy. Nutrients 2021, 13, 1681. [Google Scholar] [CrossRef]
- Dickerson, R.N.; Gervasio, J.M.; Sherman, J.J.; Kudsk, K.A.; Hickerson, W.L.; Brown, R.O. A comparison of renal phosphorus regulation in thermally injured and multiple trauma patients receiving specialized nutrition support. JPEN J. Parenter. Enteral Nutr. 2001, 25, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Markowitz, G.S.; Perazella, M.A. Acute phosphate nephropathy. Kidney Int. 2009, 76, 1027–1034. [Google Scholar] [CrossRef] [PubMed]
- Johnston, K.R.; Govel, L.A.; Andritz, M.H. Gastrointestinal effects of sorbitol as an additive in liquid medications. Am. J. Med. 1994, 97, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Velentzas, C.; Meindok, H.; Oreopoulos, D.G.; Meema, H.E.; Rabinovich, S.; Jones, M.; Sutton, D.; Rapoport, A.; deVeber, G. Visceral calcification and the CaXP product. Adv. Exp. Med. Biol. 1978, 103, 195–201. [Google Scholar] [CrossRef]
- Dickerson, R.N.; Alexander, K.H.; Minard, G.; Croce, M.A.; Brown, R.O. Accuracy of methods to estimate ionized and “corrected” serum calcium concentrations in critically ill multiple trauma patients receiving specialized nutrition support. JPEN J. Parenter. Enteral Nutr. 2004, 28, 133–141. [Google Scholar] [CrossRef]
| Variable * | Lower Dose | Higher Dose | p |
|---|---|---|---|
| N | 22 | 11 | - |
| Age, y | 49 [29, 64] | 34 [27, 48] | 0.331 |
| Actual weight, kg | 83 [68, 102] | 82 [72, 90] | 0.789 |
| Ideal body weight, kg | 65 (59, 75) | 71 (66, 78) | 0.292 |
| Adjusted dosing weight, kg | 76 [68, 85] | 75 [72, 84] | 0.619 |
| Body mass index, kg/m2 | 26.3 [23.0, 33.1] | 27.0 [24.5, 28.8] | 0.717 |
| Sex, male/female, n/n | 14/8 | 9/2 | 0.430 |
| Race | |||
| Black, n | 13 | 7 | 0.586 |
| White, n | 7 | 4 | |
| Hispanic, n | 2 | 0 | |
| Admission diagnosis | |||
| Motor vehicle collision, n | 16 | 7 | 0.329 |
| GSW/KSW, n | 2 | 3 | |
| Fall/assault, n | 1 | 1 | |
| Other, n | 3 | 0 | |
| Severe TBI with ICP monitoring, n (%) | 7 (32%) | 2 (18%) | 0.681 |
| Ventilator dependent, n | 21 (95%) | 11 (100%) | 1.000 |
| TICU length of stay, d | 14 [9, 19] | 14 [12, 18] | 0.515 |
| Hospital length of stay, d | 28 [18, 45] | 21 [19, 41] | 0.390 |
| Ventilator dependent, n (%) | 21 (95%) | 11 (100%) | 1.000 |
| Survived, n (%) | 17 (77%) | 10 (91%) | 0.637 |
| Serum potassium, mEq/L | 4.2 [4.0, 4.3] | 4.2 [4.0, 4.4] | 0.546 |
| mmol/L | 4.2 [4.0, 4.3] | 4.2 [4.0, 4.4] | |
| White blood cell count, cells/µm3 | 10.7 [9.3, 13.5] | 10.5 [7.8. 14.3] | 0.717 |
| Serum magnesium, mg/dL | 2.0 [2.0, 2.1] | 1.8 [1.7, 2.1] | 0.055 |
| mmol/L | 0.82 [0.82, 0.86] | 0.74 [0.70, 0.86] | |
| C-reactive protein, mg/dL | 25.0 [17.9, 34.3] | 18.1 [10.9, 31.8] | 0.172 |
| mg/L | 250 [179, 343] | 181 [109, 318] | |
| Prealbumin, mg/dL | 9.0 [4.5, 13.5] | 10.0 [7.0, 14.3] | 0.364 |
| mg/L | 90 [45, 135] | 100 [70, 143] | |
| Serum creatinine, mg/dL | 0.8 [0.6, 1.0] | 0.8 [0.7, 0.9] | 0.907 |
| µmol/L | 71 [53, 88] | 77 [62, 80] | |
| Serum urea nitrogen, mg/dL | 18 [13, 27] | 18 [10, 27] | 0.804 |
| mmol/L | 6.4 [4.6, 9.6] | 6.4 [3.6, 9.6] | |
| Serum glucose, mg/dL | 135 [113, 164] | 113 [104, 122] | 0.070 |
| mmol/L | 7.5 [6.3, 9.1] | 6.3 [5.8, 6.8] | |
| Total fluid intake, L/d | 2.9 [2.2, 3.5] | 3.1 [1.8, 3.4] | 0.954 |
| Total fluid output, L/d | 1.9 [1.4, 3.0] | 2.2 [1.1, 3.7] | 0.554 |
| Received vasopressors during EN, n (%) | 2 (9%) | 1 (9%) | 1.000 |
| Variable * | Lower Dose | Higher Dose | p |
|---|---|---|---|
| Number of patients, n | 22 | 11 | - |
| Phosphorus dose, mmol | 34 | 68 | - |
| Phosphorus dose, mmol/kg dosing weight | 0.45 [0.40, 0.50] | 0.91 [0.81, 0.94] | 0.001 |
| EN phosphorus intake, mmol ¶ | 19.5 [8.8, 34] | 24 [12, 33] | 0.789 |
| Day of EN, d ¶ | 2 [1, 7] | 2 [1, 4] | 0.556 |
| TICU day, d ¶, | 5 [3, 10] | 4 [2, 6] | 0.317 |
| Caloric intake, kcals/d ¶ | 899 [423, 1405] | 1035 [443, 1513] | 0.717 |
| Carbohydrate intake, g/d ¶ | 64 [39, 136] | 107 [55, 161] | 0.480 |
| Insulin intake, units/d ¶ | 0 [0, 3] | 0 [0, 0] | 0.477 |
| Arterial pH pre-dose | 7.42 [7.36, 7.47] | 7.42 [7.37, 7.45] | 0.560 |
| Arterial pH post-dose | 7.45 [7.39, 7.49] | 7.44 [7.29, 7.50] | 0.830 |
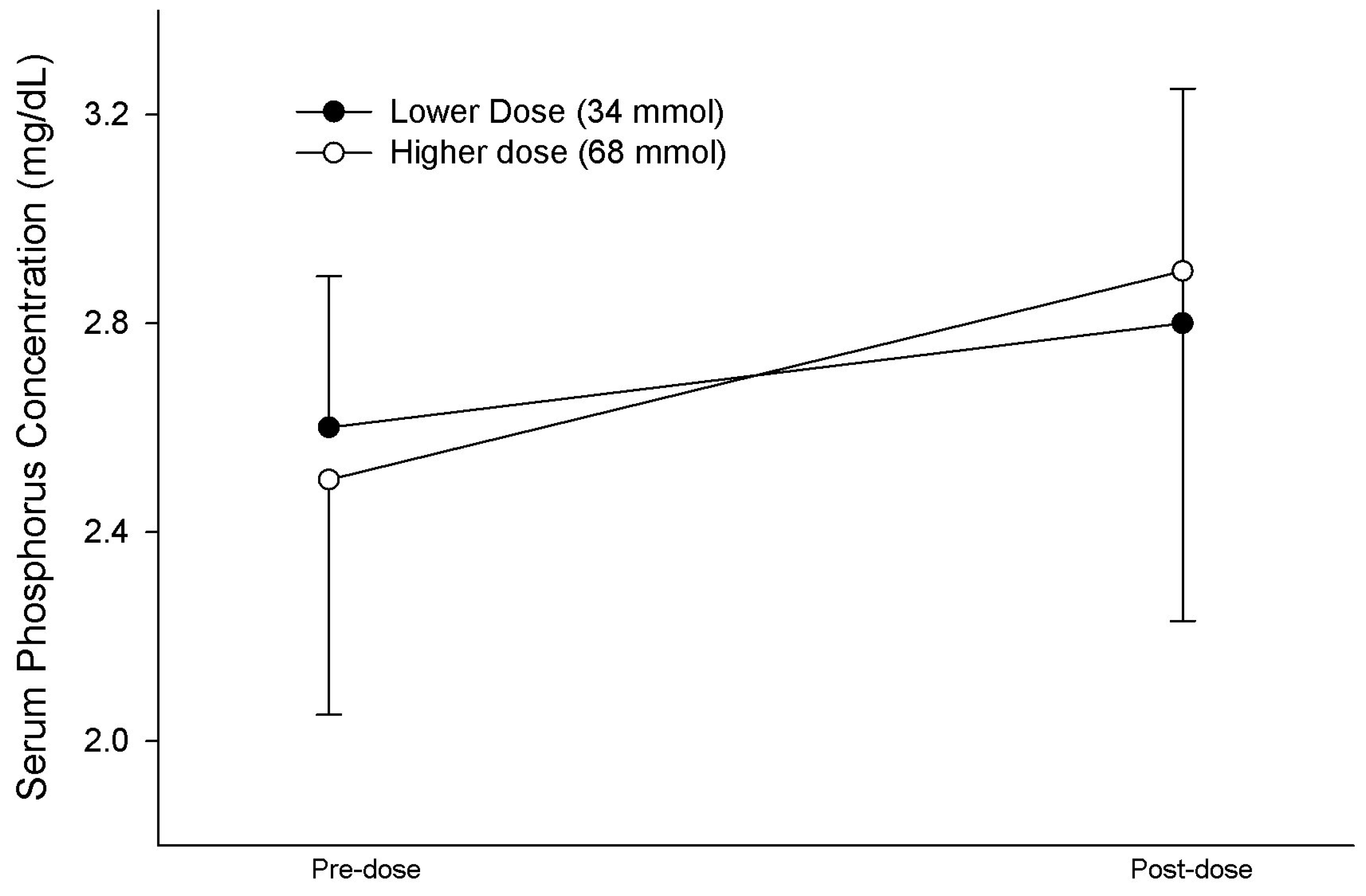
| Initial serum phosphorus, mg/dL | 2.6 [2.4, 2.8] | 2.5 [2.1, 2.8] | 0.465 |
| mmol/L | 0.84 [0.77, 0.90] | 0.81 [0.68, 0.90] | |
| Final serum phosphorus, mg/dL | 2.8 [1.9, 3.3] | 2.9 [2.2, 3.0] | 0.878 |
| mmol/L | 0.90 [0.61, 1.07] | 0.94 [0.71, 0.97] | |
| ∆ in serum phosphorus, mg/dL | 0.2 [−0.5, 0.7] | 0.6 [−0.3, 0.8] | 0.646 |
| mmol/L | 0.06 [−0.16, 0.23] | 0.19 [−0.10, 0.26] | |
| Improvement in serum phosphorus, n (%) | 12 (55%) | 8 (73%) | 0.436 |
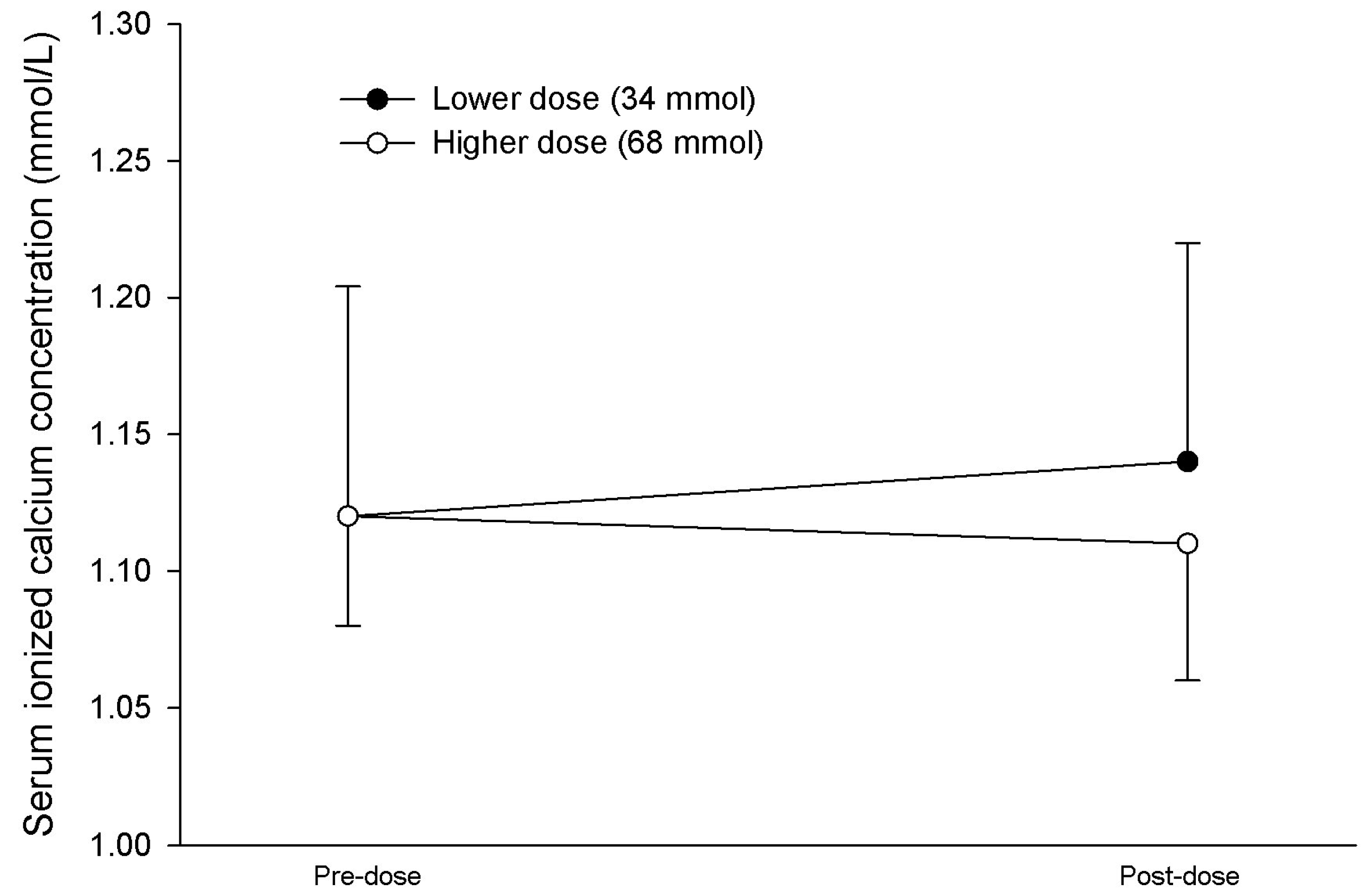
| Initial serum iCa, mmol/L | 1.11 [1.07, 1.17] | 1.14 [1.11, 1.15] | 0.984 |
| Final serum iCa, mmol/L | 1.15 [1.09, 1.20] | 1.12 [1.08, 1.16] | 0.251 |
| Diarrhea, n (%) | 3 (14%) | 0 (0%) | 0.534 |
| Variable * | Responded | Not Responded | p |
|---|---|---|---|
| Number of patients, n | 20 | 13 | - |
| Initial serum phosphorus, mg/dL | 2.6 [2.3, 2.8] | 2.6 [2.3, 2.8] | 0.811 |
| mmol/L | 0.84 [0.74, 0.90] | 0.84 [0.74, 0.90] | |
| Final serum phosphorus, mg/dL | 3.1 [2.9, 3.6] | 1.9 [1.6, 2.3] | 0.001 |
| mmol/L | 1.0 [0.94, 1.16] | 0.61 [0.52, 0.74] | |
| Phosphorus dose, mmol | 35 [35, 70] | 35 [35, 53] | 0.332 |
| Phosphorus dose, mmol/kg dosing weight | 0.53 [0.44, 0.85] | 0.51 [0.42, 0.80] | 0.495 |
| EN phosphorus intake, mmol/d | 16 [7, 31] | 24 [16, 35] | 0.172 |
| Age, y | 36 [26, 60] | 48 [40, 66] | 0.167 |
| Body mass index (kg/m2) | 27.5 [24.5, 31.5] | 25.8 [22.6, 30.0] | 0.585 |
| Serum creatinine, mg/dL | 0.8 [0.6, 0.9] | 0.8 [0.8, 1.0] | 0.202 |
| µmol/L | 71 [53, 80] | 71 [71, 88] | |
| C-reactive protein, mg/dL ¶ | 25.0 [16.5, 34.3] | 19.6 [10.0, 29.5] | 0.144 |
| mg/L ¶ | 250 [165, 343] | 196 [100, 295] | |
| Prealbumin, mg/dL ¶ | 8.5 [5.8, 13.0] | 10.0 [6.0, 16.0] | 0.518 |
| mg/L ¶ | 85 [58, 130] | 100 [60, 160] | |
| WBC, cells/µm3 | 10.6 [9.0, 12.0] | 11.9 [9.5, 15.8] | 0.308 |
| Arterial pH pre-dose | 7.42 [7.36, 7.48] | 7.40 [7.36, 7.44] | 0.639 |
| Arterial pH post-dose | 7.44 [7.34, 7.47] | 7.45 [7.41, 7.51] | 0.208 |
| Admit diagnosis of MVC, n (%) | 15 (75%) | 8 (62%) | 0.745 |
| Traumatic brain injury, n (%) | 5 (25%) | 4 (31%) | 1.000 |
| Survived, n (%) | 16 (80%) | 11 (85%) | 1.000 |
| Day of EN, d ¶ | 2 [1, 4] | 2 [1, 8] | 0.955 |
| TICU day, d ¶, | 4 [3, 6] | 4 [2, 11] | 0.741 |
| Caloric intake, kcals/d ¶ | 703 [340, 1469] | 985 [777, 1467] | 0.261 |
| Carbohydrate intake, g/d ¶ | 60 [28, 123] | 108 [63, 162] | 0.203 |
| Serum glucose, mg/dL ¶ | 118 [109, 139] | 136 [115, 161] | 0.196 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harris, T.D.; Farrar, J.E.; Byerly, S.; Filiberto, D.M.; Dickerson, R.N. Evaluation of a Novel Enteral Phosphorus Therapy with Enteral Nutrition during a National Intravenous Sodium Phosphate Shortage. Nutrients 2024, 16, 1394. https://doi.org/10.3390/nu16091394
Harris TD, Farrar JE, Byerly S, Filiberto DM, Dickerson RN. Evaluation of a Novel Enteral Phosphorus Therapy with Enteral Nutrition during a National Intravenous Sodium Phosphate Shortage. Nutrients. 2024; 16(9):1394. https://doi.org/10.3390/nu16091394
Chicago/Turabian StyleHarris, Tinia D., Julie E. Farrar, Saskya Byerly, Dina M. Filiberto, and Roland N. Dickerson. 2024. "Evaluation of a Novel Enteral Phosphorus Therapy with Enteral Nutrition during a National Intravenous Sodium Phosphate Shortage" Nutrients 16, no. 9: 1394. https://doi.org/10.3390/nu16091394





