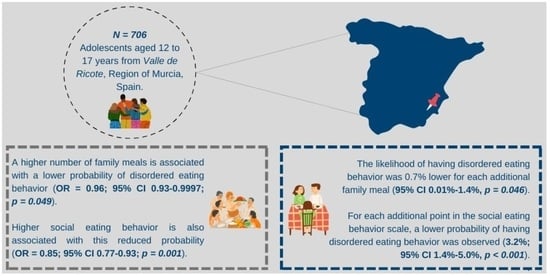
Family Meals and Social Eating Behavior and Their Association with Disordered Eating among Spanish Adolescents: The EHDLA Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Measurements
2.1.1. Family Meals (Independent Variable)
2.1.2. Social Eating Behavior (Independent Variable)
2.1.3. Disordered Eating (Dependent Variable)
2.2. Covariates
2.2.1. Sociodemographic Factors
2.2.2. Lifestyle Factors
2.2.3. Anthropometric Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association (Ed.) Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR, 5th ed.; Text Revision; American Psychiatric Association Publishing: Washington, DC, USA, 2022; ISBN 978-0-89042-575-6. [Google Scholar]
- Hornberger, L.L.; Lane, M.; Breuner, C.C.; Alderman, E.M.; Grubb, L.K.; Powers, M.; Upadhya, K.K.; Wallace, S.B.; Hornberger, L.L.; Lane, M.; et al. Identification and Management of Eating Disorders in Children and Adolescents. Pediatrics 2021, 147, e2020040279. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.K.N.; Correll, C.U.; Wong, C.S.M.; Chu, R.S.T.; Fung, V.S.C.; Wong, G.H.S.; Lei, J.H.C.; Chang, W.C. Life Expectancy and Years of Potential Life Lost in People with Mental Disorders: A Systematic Review and Meta-Analysis. eClinicalMedicine 2023, 65, 102294. [Google Scholar] [CrossRef]
- Seitz, J.; Herpertz-Dahlmann, B.; Konrad, K. Brain Morphological Changes in Adolescent and Adult Patients with Anorexia Nervosa. J. Neural Transm. 2016, 123, 949–959. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Mental Disorders Collaborators. Global, Regional, and National Burden of 12 Mental Disorders in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- US Preventive Services Task Force; Davidson, K.W.; Barry, M.J.; Mangione, C.M.; Cabana, M.; Chelmow, D.; Coker, T.R.; Davis, E.M.; Donahue, K.E.; Jaén, C.R.; et al. Screening for Eating Disorders in Adolescents and Adults: US Preventive Services Task Force Recommendation Statement. JAMA 2022, 327, 1061. [Google Scholar] [CrossRef] [PubMed]
- Attia, E.; Guarda, A.S. Prevention and Early Identification of Eating Disorders. JAMA 2022, 327, 1029. [Google Scholar] [CrossRef]
- Feltner, C.; Peat, C.; Reddy, S.; Riley, S.; Berkman, N.; Middleton, J.C.; Balio, C.; Coker-Schwimmer, M.; Jonas, D.E. Screening for Eating Disorders in Adolescents and Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2022, 327, 1068–1082. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Luyando, M.; Alvarez-Rayón, G.; Garner, D.M.; Amaya-Hernández, A.; Bautista-Díaz, M.L.; Mancilla-Díaz, J.M. Systematic Review of Disordered Eating Behaviors: Methodological Considerations for Epidemiological Research. Rev. Mex. Trastor. Aliment. 2015, 6, 51–63. [Google Scholar] [CrossRef]
- López-Gil, J.F.; García-Hermoso, A.; Smith, L.; Firth, J.; Trott, M.; Mesas, A.E.; Jiménez-López, E.; Gutiérrez-Espinoza, H.; Tárraga-López, P.J.; Victoria-Montesinos, D. Global Proportion of Disordered Eating in Children and Adolescents: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2023, 177, 363–372. [Google Scholar] [CrossRef]
- Kärkkäinen, U.; Mustelin, L.; Raevuori, A.; Kaprio, J.; Keski-Rahkonen, A. Do Disordered Eating Behaviours Have Long-term Health-related Consequences? Eur. Eat. Disord. Rev. 2018, 26, 22–28. [Google Scholar] [CrossRef]
- Nagata, J.M.; Garber, A.K.; Tabler, J.L.; Murray, S.B.; Bibbins-Domingo, K. Prevalence and Correlates of Disordered Eating Behaviors among Young Adults with Overweight or Obesity. J. Gen. Intern. Med. 2018, 33, 1337–1343. [Google Scholar] [CrossRef] [PubMed]
- Chaves, E.; Jeffrey, D.T.; Williams, D.R. Disordered Eating and Eating Disorders in Pediatric Obesity: Assessment and Next Steps. Int. J. Environ. Res. Public Health 2023, 20, 6638. [Google Scholar] [CrossRef] [PubMed]
- Pauli-Pott, U.; Becker, K.; Albayrak, Ö.; Hebebrand, J.; Pott, W. Links between Psychopathological Symptoms and Disordered Eating Behaviors in Overweight/Obese Youths. Int. J. Eat. Disord. 2013, 46, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Piran, N.; Robinson, S.R. Associations between Disordered Eating Behaviors and Licit and Illicit Substance Use and Abuse in a University Sample. Addict. Behav. 2006, 31, 1761–1775. [Google Scholar] [CrossRef] [PubMed]
- Tabler, J.; Utz, R.L. The Influence of Adolescent Eating Disorders or Disordered Eating Behaviors on Socioeconomic Achievement in Early Adulthood. Int. J. Eat. Disord. 2015, 48, 622–632. [Google Scholar] [CrossRef]
- Quick, V.M.; Byrd-Bredbenner, C.; Neumark-Sztainer, D. Chronic Illness and Disordered Eating: A Discussion of the Literature. Adv. Nutr. 2013, 4, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Zeeck, A.; Herpertz-Dahlmann, B.; Friederich, H.-C.; Brockmeyer, T.; Resmark, G.; Hagenah, U.; Ehrlich, S.; Cuntz, U.; Zipfel, S.; Hartmann, A. Psychotherapeutic Treatment for Anorexia Nervosa: A Systematic Review and Network Meta-Analysis. Front. Psychiatry 2018, 9, 158. [Google Scholar] [CrossRef]
- Murray, S.B.; Quintana, D.S.; Loeb, K.L.; Griffiths, S.; Le Grange, D. Treatment Outcomes for Anorexia Nervosa: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Psychol. Med. 2019, 49, 535–544. [Google Scholar] [CrossRef]
- Ragelienė, T.; Grønhøj, A. The Influence of Peers’ and Siblings’ on Children’s and Adolescents′ Healthy Eating Behavior. A Systematic Literature Review. Appetite 2020, 148, 104592. [Google Scholar] [CrossRef]
- Chung, A.; Vieira, D.; Donley, T.; Tan, N.; Jean-Louis, G.; Kiely Gouley, K.; Seixas, A. Adolescent Peer Influence on Eating Behaviors via Social Media: Scoping Review. J. Med. Internet Res. 2021, 23, e19697. [Google Scholar] [CrossRef]
- Higgs, S.; Thomas, J. Social Influences on Eating. Curr. Opin. Behav. Sci. 2016, 9, 1–6. [Google Scholar] [CrossRef]
- Fisberg, M.; Gioia, N.; Maximino, P. Transgenerational Transmission of Eating Habits. J. Pediatr. 2023, 100 (Suppl. S1), S82–S87. [Google Scholar] [CrossRef] [PubMed]
- Herman, C.P. The Social Facilitation of Eating. A Review. Appetite 2015, 86, 61–73. [Google Scholar] [CrossRef]
- Victoria-Montesinos, D.; Jiménez-López, E.; Mesas, A.E.; López-Bueno, R.; Garrido-Miguel, M.; Gutiérrez-Espinoza, H.; Smith, L.; López-Gil, J.F. Are Family Meals and Social Eating Behaviour Associated with Depression, Anxiety, and Stress in Adolescents? The EHDLA Study. Clin. Nutr. 2023, 42, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Berge, J.M.; Wall, M.; Hsueh, T.-F.; Fulkerson, J.A.; Larson, N.; Neumark-Sztainer, D. The Protective Role of Family Meals for Youth Obesity: 10-Year Longitudinal Associations. J. Pediatr. 2015, 166, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.S.N.; Chen, J.Y.; Ng, M.Y.C.; Yeung, M.H.Y.; Bedford, L.E.; Lam, C.L.K. How Does the Family Influence Adolescent Eating Habits in Terms of Knowledge, Attitudes and Practices? A Global Systematic Review of Qualitative Studies. Nutrients 2021, 13, 3717. [Google Scholar] [CrossRef] [PubMed]
- Fulkerson, J.A.; Story, M.; Mellin, A.; Leffert, N.; Neumark-Sztainer, D.; French, S.A. Family Dinner Meal Frequency and Adolescent Development: Relationships with Developmental Assets and High-Risk Behaviors. J. Adolesc. Health 2006, 39, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Utter, J.; Larson, N.; Berge, J.M.; Eisenberg, M.E.; Fulkerson, J.A.; Neumark-Sztainer, D. Family Meals among Parents: Associations with Nutritional, Social and Emotional Wellbeing. Prev. Med. 2018, 113, 7–12. [Google Scholar] [CrossRef]
- Neumark-Sztainer, D.; Larson, N.I.; Fulkerson, J.A.; Eisenberg, M.E.; Story, M. Family Meals and Adolescents: What Have We Learned from Project EAT (Eating Among Teens)? Public Health Nutr. 2010, 13, 1113–1121. [Google Scholar] [CrossRef]
- Videon, T.M.; Manning, C.K. Influences on Adolescent Eating Patterns: The Importance of Family Meals. J. Adolesc. Health 2003, 32, 365–373. [Google Scholar] [CrossRef]
- Gratão, L.H.A.; Pessoa, M.C.; Rodrigues da Silva, T.P.; Rocha, L.L.; Louise Cassimiro Inácio, M.; Resende Prado Rangel de Oliveira, T.; de Freitas Cunha, C.; Mendes, L.L. Dietary Patterns, Breakfast Consumption, Meals with Family and Associations with Common Mental Disorders in Adolescents: A School-Based Cross-Sectional Study. BMC Public Health 2022, 22, 980. [Google Scholar] [CrossRef]
- Valero-Solis, S.; Granero-Perez, R.; Sanchez-Carracedo, D.; Valero-Solis, S.; Granero-Perez, R.; Sanchez-Carracedo, D. Frequency of Family Meals and Risk of Eating Disorders in Adolescents in Spain and Peru. Rev. Latinoam. Psicol. 2019, 51, 48–57. [Google Scholar] [CrossRef]
- López-Gil, J.F.; Chen, S.; Jiménez-López, E.; Abellán-Huerta, J.; Herrera-Gutiérrez, E.; Royo, J.M.P.; Mesas, A.E.; Tárraga-López, P.J. Are the Use and Addiction to Social Networks Associated with Disordered Eating among Adolescents? Findings from the EHDLA Study. Int. J. Ment. Health Addict. 2023. [Google Scholar] [CrossRef]
- Bevilacqua, L.; Shackleton, N.; Hale, D.; Allen, E.; Bond, L.; Christie, D.; Elbourne, D.; Fitzgerald-Yau, N.; Fletcher, A.; Jones, R.; et al. The Role of Family and School-Level Factors in Bullying and Cyberbullying: A Cross-Sectional Study. BMC Pediatr. 2017, 17, 160. [Google Scholar] [CrossRef] [PubMed]
- Utter, J.; Denny, S.; Lucassen, M.; Dyson, B. Adolescent Cooking Abilities and Behaviors: Associations with Nutrition and Emotional Well-Being. J. Nutr. Educ. Behav. 2016, 48, 35–41.e1. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.I.; Neumark-Sztainer, D.; Hannan, P.J.; Story, M. Family Meals during Adolescence Are Associated with Higher Diet Quality and Healthful Meal Patterns during Young Adulthood. J. Am. Diet. Assoc. 2007, 107, 1502–1510. [Google Scholar] [CrossRef] [PubMed]
- Loth, K.; Wall, M.; Choi, C.; Bucchianeri, M.; Quick, V.; Larson, N.; Neumark-Sztainer, D. Family Meals and Disordered Eating in Adolescents: Are the Benefits the Same for Everyone? Int. J. Eat. Disord. 2015, 48, 100–110. [Google Scholar] [CrossRef] [PubMed]
- López-Gil, J.F. The Eating Healthy and Daily Life Activities (EHDLA) Study. Children 2022, 9, 370. [Google Scholar] [CrossRef]
- Garcia-Campayo, J.; Sanz-Carrillo, C.; Ibañez, J.A.; Lou, S.; Solano, V.; Alda, M. Validation of the Spanish Version of the SCOFF Questionnaire for the Screening of Eating Disorders in Primary Care. J. Psychosom. Res. 2005, 59, 51–55. [Google Scholar] [CrossRef]
- Muro-Sans, P.; Amador-Campos, J.A.; Morgan, J.F. The SCOFF-c: Psychometric Properties of the Catalan Version in a Spanish Adolescent Sample. J. Psychosom. Res. 2008, 64, 81–86. [Google Scholar] [CrossRef]
- Currie, C.; Molcho, M.; Boyce, W.; Holstein, B.; Torsheim, T.; Richter, M. Researching Health Inequalities in Adolescents: The Development of the Health Behaviour in School-Aged Children (HBSC) Family Affluence Scale. Soc. Sci. Med. 2008, 66, 1429–1436. [Google Scholar] [CrossRef] [PubMed]
- Saint-Maurice, P.F.; Welk, G.J. Validity and Calibration of the Youth Activity Profile. PLoS ONE 2015, 10, e0143949. [Google Scholar] [CrossRef]
- Segura-Díaz, J.M.; Barranco-Ruiz, Y.; Saucedo-Araujo, R.G.; Aranda-Balboa, M.J.; Cadenas-Sanchez, C.; Migueles, J.H.; Saint-Maurice, P.F.; Ortega, F.B.; Welk, G.J.; Herrador-Colmenero, M.; et al. Feasibility and Reliability of the Spanish Version of the Youth Activity Profile Questionnaire (YAP-Spain) in Children and Adolescents. J. Sports Sci. 2021, 39, 801–807. [Google Scholar] [CrossRef]
- Haines, J.; Gillman, M.W.; Rifas-Shiman, S.; Field, A.E.; Austin, S.B. Family Dinner and Disordered Eating Behaviors in a Large Cohort of Adolescents. Eat. Disord. 2010, 18, 10–24. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, M.E.; Olson, R.E.; Neumark-Sztainer, D.; Story, M.; Bearinger, L.H. Correlations between Family Meals and Psychosocial Well-Being among Adolescents. Arch. Pediatr. Adolesc. Med. 2004, 158, 792–796. [Google Scholar] [CrossRef]
- Van Dyke, N.; Drinkwater, E.J. Relationships between Intuitive Eating and Health Indicators: Literature Review. Public Health Nutr. 2014, 17, 1757–1766. [Google Scholar] [CrossRef]
- Ramseyer Winter, V.; Jones, A.; O’Neill, E. Eating Breakfast and Family Meals in Adolescence: The Role of Body Image. Soc. Work. Public Health 2019, 34, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Frieiro, P.; González-Rodríguez, R.; Domínguez-Alonso, J. Self-Esteem and Socialisation in Social Networks as Determinants in Adolescents’ Eating Disorders. Health Soc. Care Community 2022, 30, e4416–e4424. [Google Scholar] [CrossRef]
- Langdon-Daly, J.; Serpell, L. Protective Factors against Disordered Eating in Family Systems: A Systematic Review of Research. J. Eat. Disord. 2017, 5, 12. [Google Scholar] [CrossRef]
- Schriber, R.A.; Guyer, A.E. Adolescent Neurobiological Susceptibility to Social Context. Dev. Cogn. Neurosci. 2016, 19, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.S.; Tung, K.T.S.; Wong, W.H.S.; Ho, F.K.W.; Tso, W.W.Y.; Yip, P.S.F.; Wong, C.K.H.; Fan, S.Y.S.; Ip, P. Associations of Family Meals with Adolescent Perception of Family Relationship and Compliance with Parental Guidance in Hong Kong: Results of a Representative Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 5402. [Google Scholar] [CrossRef] [PubMed]
- Fjellström, C. Mealtime and Meal Patterns from a Cultural Perspective. Scand. J. Nutr. 2004, 48, 161–164. [Google Scholar] [CrossRef]
- Dunbar, R.I.M. Breaking Bread: The Functions of Social Eating. Adapt. Hum. Behav. Physiol. 2017, 3, 198–211. [Google Scholar] [CrossRef] [PubMed]
- Grech, P.; Azzopardi, A.; Borg, S. An Account of Loneliness while Living with an Eating Disorder. Psychiatr. Ment. Health Nurs. 2023, 31, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Fiese, B.H.; Winter, M.A.; Botti, J.C. The ABCs of Family Mealtimes: Observational Lessons for Promoting Healthy Outcomes for Children with Persistent Asthma. Child Dev. 2011, 82, 133–145. [Google Scholar] [CrossRef] [PubMed]
- Elgar, F.J.; Craig, W.; Trites, S.J. Family Dinners, Communication, and Mental Health in Canadian Adolescents. J. Adolesc. Health 2013, 52, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Hammons, A.J.; Fiese, B.H. Is Frequency of Shared Family Meals Related to the Nutritional Health of Children and Adolescents? Pediatrics 2011, 127, e1565–e1574. [Google Scholar] [CrossRef]
- Herman, C.P. The Social Facilitation of Eating or the Facilitation of Social Eating? J. Eat. Disord. 2017, 5, 16. [Google Scholar] [CrossRef]
- Suwalska, J.; Bogdański, P. Social Modeling and Eating Behavior—A Narrative Review. Nutrients 2021, 13, 1209. [Google Scholar] [CrossRef]
- White, H.J.; Haycraft, E.; Meyer, C. Family Mealtimes and Eating Psychopathology: The Role of Anxiety and Depression among Adolescent Girls and Boys. Appetite 2014, 75, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Snuggs, S.; Harvey, K. Family Mealtimes: A Systematic Umbrella Review of Characteristics, Correlates, Outcomes and Interventions. Nutrients 2023, 15, 2841. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total | |
|---|---|---|
| School | IES Vicente Medina (%) | 376 (53.5) |
| IES Pedro Guillén (%) | 187 (26.5) | |
| CE El Ope (%) | 143 (20.3) | |
| Age (years) | Median (IQR) | 14.0 (2.0) |
| Sex | Boys (%) | 310 (43.9) |
| Girls (%) | 396 (56.1) | |
| FAS-III (score) | Median (IQR) | 8.0 (3.0) |
| YAP-S physical activity (score) | Median (IQR) | 2.6 (0.9) |
| YAP-S sedentary behavior (score) | Median (IQR) | 2.6 (0.8) |
| Overall sleep duration (minutes) | Median (IQR) | 501.4 (71.8) |
| Body mass index | Median (IQR) | 21.7 (6.0) |
| Energy intake (kcal) | Median (IQR) | 2554.3 (1465.9) |
| Weekly family meals (number) | Median (IQR) | 14.0 (6.0) |
| Social eating behavior (score) a | Median (IQR) | 9.8 (1.8) |
| SCOFF (score) | Median (IQR) | 1.0 (2.0) |
| Disordered eating behavior b | No (%) | 493 (69.2) |
| Yes (%) | 213 (30.2) |
| Disordered Eating Behavior a (Outcome) | ||
|---|---|---|
| Predictor | OR (95% CI, p-Value) Univariable | OR (95% CI, p-Value) Multivariable |
| Family meals global (per one meal) | 0.95 (0.92 to 0.99, p = 0.005) | 0.96 (0.93 to 0.9997, p = 0.049) |
| Sex | ||
| Boys | Reference | Reference |
| Girls | 2.32 (1.65 to 3.28, p < 0.001) | 2.93 (2.00 to 4.34, p < 0.001) |
| Age (per one year) | 1.03 (0.92 to 1.14, p = 0.620) | 0.93 (0.82 to 1.05, p = 0.260) |
| FAS-III score (per one point) | 0.92 (0.85 to 1.00, p = 0.040) | 0.92 (0.85 to 1.00, p = 0.052) |
| YAP-S physical activity (per one point) | 1.11 (0.87 to 1.41, p = 0.386) | 1.27 (0.97 to 1.67, p = 0.085) |
| YAP-S sedentary behavior (per one point) | 1.04 (0.80 to 1.35, p = 0.782) | 1.03 (0.75 to 1.40, p = 0.859) |
| Overall sleep duration global (per one hour) | 0.79 (0.66 to 0.95, p = 0.011) | 0.86 (0.70 to 1.05, p = 0.144) |
| Body mass index (per one kg/m2) | 1.12 (1.09 to 1.17, p < 0.001) | 1.14 (1.10 to 1.19, p < 0.001) |
| Energy intake (per 1000 kcal) | 1.04 (0.96 to 1.12, p = 0.280) | 1.02 (0.94 to 1.12, p = 0.578) |
| Disordered Eating Behavior a (Outcome) | ||
|---|---|---|
| Predictor | OR (95% CI, p-Value) Univariable | OR (95% CI, p-Value) Multivariable |
| Social eating behavior (per one point) | 0.83 (0.76 to 0.90, p < 0.001) | 0.85 (0.77 to 0.93, p = 0.001) |
| Sex | ||
| Boys | Reference | Reference |
| Girls | 2.32 (1.65 to 3.28, p < 0.001) | 3.10 (2.11 to 4.61, p < 0.001) |
| Age (per one year) | 1.03 (0.92 to 1.14, p = 0.620) | 0.95 (0.84 to 1.07, p = 0.398) |
| FAS-III score (per one point) | 0.92 (0.85 to 1.00, p = 0.040) | 0.93 (0.86 to 1.02, p = 0.111) |
| YAP-S physical activity (per one point) | 1.11 (0.87 to 1.41, p = 0.386) | 1.28 (0.98 to 1.69, p = 0.076) |
| YAP-S sedentary behavior (per one point) | 1.04 (0.80 to 1.35, p = 0.782) | 1.00 (0.73 to 1.36, p = 0.995) |
| Overall sleep duration global (per one hour) | 0.79 (0.66 to 0.95, p = 0.011) | 0.86 (0.70 to 1.06, p = 0.148) |
| Body mass index (per one kg/m2) | 1.12 (1.09 to 1.17, p < 0.001) | 1.14 (1.10 to 1.19, p < 0.001) |
| Energy intake (per 1000 kcal) | 1.04 (0.96 to 1.12, p = 0.280) | 1.02 (0.94 to 1.11, p = 0.705) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Gil, J.F.; Victoria-Montesinos, D.; Gutiérrez-Espinoza, H.; Jiménez-López, E. Family Meals and Social Eating Behavior and Their Association with Disordered Eating among Spanish Adolescents: The EHDLA Study. Nutrients 2024, 16, 951. https://doi.org/10.3390/nu16070951
López-Gil JF, Victoria-Montesinos D, Gutiérrez-Espinoza H, Jiménez-López E. Family Meals and Social Eating Behavior and Their Association with Disordered Eating among Spanish Adolescents: The EHDLA Study. Nutrients. 2024; 16(7):951. https://doi.org/10.3390/nu16070951
Chicago/Turabian StyleLópez-Gil, José Francisco, Desirée Victoria-Montesinos, Héctor Gutiérrez-Espinoza, and Estela Jiménez-López. 2024. "Family Meals and Social Eating Behavior and Their Association with Disordered Eating among Spanish Adolescents: The EHDLA Study" Nutrients 16, no. 7: 951. https://doi.org/10.3390/nu16070951