Building a Sustainable Healthcare Model: A Cross-Country Analysis
Abstract
:1. Introduction
2. Methods
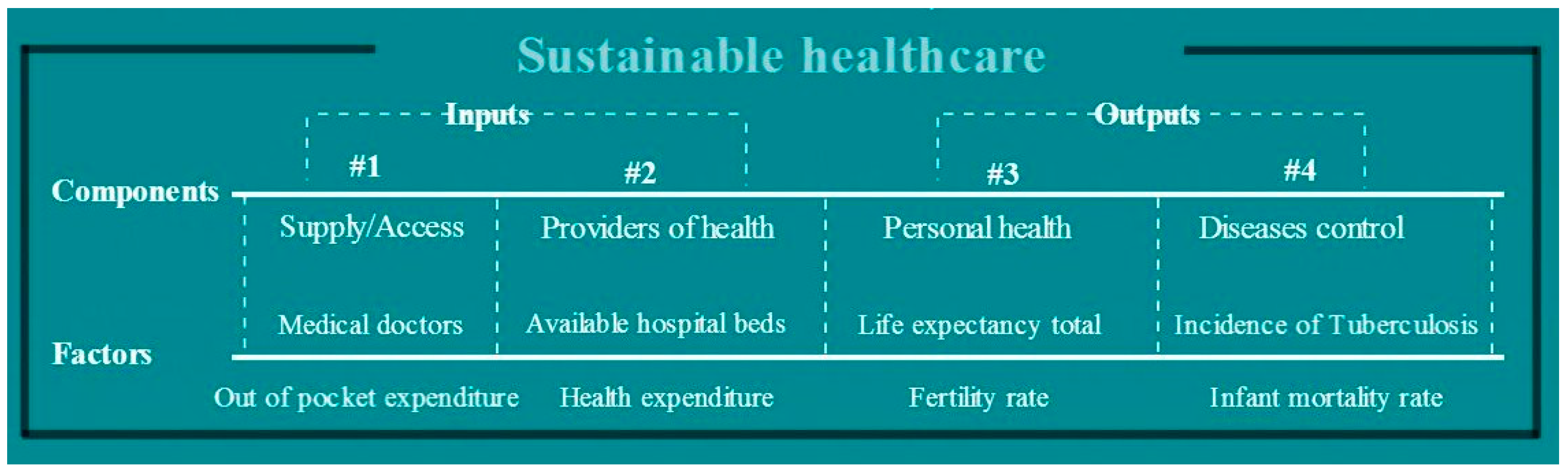
2.1. Conceptual Framework of Sustainable Healthcare
- Inputs of the healthcare system:
2.2. Selection of the Factors of the Sustainable Healthcare Model
2.3. Methodology Used for ISH Determination
3. Results
3.1. Factors of Sustainable Healthcare
3.2. Index of Sustainable Healthcare
- Group I: sustainable countries—characterized by values of ISH > 0.70, meaning that the countries applied meaningful measures dedicated to increase wellbeing of their inhabitants, in terms of healthcare system development. These are the best countries for a patient to be treated in.
- Group II: on-track countries—characterized by 0.50 < ISH < 0.70, indicating that the countries applied necessary, but insufficient, measures.
- Group III: unsustainable countries—characterized by ISH < 0.50, meaning that the countries employed measures which adversely affected the population, being both unnecessary and insufficient. These are the worst countries for a patient to be treated in.
4. Discussion
- Address the weak points by:
- Improving the funding of the healthcare system, as the country still has the lowest total health expenditure as a % of GDP from EU28; the health expenditure may be correlated to the health outcomes, if this is below a certain limit. Evidence proved that an increase in the health expenditure generates improvements, to a large extent for infant mortality or marginally for life expectancy [41].
- design an action plan for fighting tuberculosis;
- combat infant mortality rate by urgent measures.
- Encourage the development of strong points by:
- offering incentives for motivating the medical graduates to practice medicine domestically;
- updating the available hospital care to increase the quality of medical treatment and improving overall performance.
5. Conclusions
Conflicts of Interest
References
- Mayberry, R.; Nicewander, D.; Qin, H.; Ballard, D. Improving quality and reducing inequities: A challenge in achieving best care. Proc. (Bayl. Univ. Med. Cent.) 2006, 19, 103–118. [Google Scholar] [PubMed]
- Gilson, L. (Ed.) Health Policy and Systems Research: A Methodology Reader; World Health Organization: Geneva, Switzerland, 2012.
- World Commission on Environment and Development (WCED). Our Common Future; Oxford University Press: New York, NY, USA, 1987; p. 44. [Google Scholar]
- Prada, G.; Grimes, K.; Sklokin, I. Defining Health and Health Care Sustainability. In Proceedings of the Conference Board of Canada, Ottawa, ON, Canada, 15 July 2014.
- Mackenbach, J.; McKee, M. (Eds.) Successes and Failures of Health Policy in Europe, McGraw Hill Education, European Observatory on Health Systems and Policies; Open University Press: New York, NY, USA, 2013.
- McKee, M.; MacLehose, L.; Nolte, E. (Eds.) Health Policy and European Union Enlargement, European Observatory on Health Systems and Policies; McGraw Hill: Berkshire, UK, 2004.
- World Health Organization. Global Health Observatory Data Repository, Out of Pocket Expenditure as % of Total Health Expenditure; World Health Organization Press: Geneva, Switzerland, 2015. [Google Scholar]
- World Health Organization. Global Health Observatory Data Repository, Health Expenditure Ratios; World Health Organization Press: Geneva, Switzerland, 2015. [Google Scholar]
- European Commission. The 2015 Aging Report; Directorate-General for Economic and Financial Affairs: Brussels, Belgium, 2015. [Google Scholar]
- Carnero, M.C. Assessment of Environmental Sustainability in Health Care Organizations. Sustainability 2015, 7, 8270–8291. [Google Scholar] [CrossRef]
- Organization for Economic Co-Operation and Development (OECD). Health Expenditure in Relation to GDP. In Health at a Glance 2011: OECD Indicators; OECD Publishing: Paris, France, 2011. [Google Scholar]
- Abbasi, K. (Ed.) Sustainable Health Systems; World Economic Forum: Geneva, Switzerland, 2013.
- Organization for Economic Co-Operation and Development (OECD). Monthly Economic Indicators (MEI)—Composite Leading Indicators. 2016. Available online: http://stats.oecd.org/Index.aspx?DataSetCode=MEI_CLI (accessed on 16 May 2016).
- Jahan, S. Human Development Report 2015: Work for Human Development; UNDP (United Nations Development Program): New York, NY, USA, 2015. [Google Scholar]
- World Economic Forum (WEF). Environmental Performance Index. 2002. Available online: http://sedac.ciesin.columbia.edu/es/esi/EPI2002_11FEB02.pdf (accessed on 16 May 2016).
- European Commission. European Innovation Scoreboards—2015, Innovation Union Scoreboard Interactive Tool; Publications Office of the European Union: Brussels, Belgium, 2015. [Google Scholar]
- World Health Organization. Global Reference List of 100 Core Health Indicators; World Health Organization Press: Luxembourg City, Luxembourg, 2015. [Google Scholar]
- Metge, C.; Chateau, D.; Prior, H.; Soodeen, R.; De Coster, C.; Barre, L. Composite Measures/Indices of Health and Health System Performance; Manitoba Centre for Health Policy: Winnipeg, MB, Cananda, 2009. [Google Scholar]
- Grzebyk, M.; Stec, M. Sustainable Development in EU Countries: Concept and Rating of Levels of Development. Sustain. Dev. 2015, 23, 110–123. [Google Scholar] [CrossRef]
- European Commission. Communication from the Commission on Effective, Assessable and Resilient Health Systems; 215/2014; Publications Office of the European Union: Brussels, Belgium, 2014. [Google Scholar]
- Eurostat Online Database. Medical Doctors: Health Graduates, Code [hlth_rs_grd]. 2015. Available online: http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_rs_grd&lang=en (accessed on 17 May 2016).
- World Bank Online Database. World Development Indicators, Available Beds in Hospitals, Code [SH.MED.BEDS.ZS]. 2015. Available online: http://data.worldbank.org/indicator/SH.MED.BEDS.ZS (accessed on 16 May 2016).
- Eurostat Online Database. Hospital Beds by Type of Care, Code [hlth_rs_bds]. 2015. Available online: http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_rs_bds&lang=en (accessed on 16 May 2016).
- World Health Organization. Global Health Expenditure Database, Health Expenditure as a % of GDP; World Health Organization Press: Geneva, Switzerland, 2015. [Google Scholar]
- World Bank Online Database. World Development Indicators, Life Expectancy Total, Code [SP.DYN.LE00.IN]. 2016. Available online: http://data.worldbank.org/indicator/SP.DYN.LE00.IN (accessed on 17 May 2016).
- World Bank Online Database. World Development Indicators, Fertility Rate, Code [SP.DYN.TFRT.IN]. 2016. Available online: http://data.worldbank.org/indicator/SP.DYN.TFRT.IN (accessed on 15 May 2016).
- World Bank Online Database. World Development Indicators, Incidence of Tuberculosis, Code [SH.TBS.INCD]. 2016. Available online: http://data.worldbank.org/indicator/SH.TBS.INCD (accessed on 15 May 2016).
- World Bank Online Database. World Development Indicators, Infant mortality Rate, Code [SP.DYN.IMRT.IN]. 2015. Available online: http://data.worldbank.org/indicator/SP.DYN.IMRT.IN. (accessed on 15 May 2016).
- United Nations Children’s Fund (UNICEF). UN Inter-Agency Group for Child Mortality Estimation; UNICEF: New York, NY, USA, 2016. [Google Scholar]
- World Bank Online Database. World Development Indicators, Physicians (per 1000 People), Code [SH.MED.PHYS.ZS]. 2016. Available online: http://data.worldbank.org/indicator/SH.MED.PHYS.ZS (accessed on 16 May 2016).
- Eurostat Online Database. Nursing and caring professionals, Code [hlth_rs_prsns]. 2016. Available online: http://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do (accessed on 22 July 2016).
- Organization for Economic Co-Operation and Development (OECD). Burden of Out-of-Pocket Health Expenditure. In Health at a Glance 2011: OECD Indicators; OECD Publishing: Paris, France, 2011. [Google Scholar]
- Xu, K.; Evans, D.; Carrin, G.; Aguilar-Rivera, A.M. Designing Health Financing Systems to Reduce Catastrophic Health Expenditure; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- United Nations Center for Human Settlements (UNCHS). Urban Initiatives, United Nations Habitat. 2012. Available online: http://unhabitat.org/ (accessed on 26 July 2016).
- European Commission. Public Health Indicators, European Core Health Indicators (ECHI), ECHI Data Tool. Available online: http://ec.europa.eu/health/indicators/indicators/index_en.htm (accessed on 22 May 2016).
- Eurostat Online Database. Detailed Amenable and Preventable Deaths of EU Residents, Code [hlth_cd_apreu]. 2016. Available online: http://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=hlth_cd_apr&lang=en (accessed on 22 July 2016).
- Organization for Economic Co-Operation and Development (OECD). Health Care Systems: Getting More Value for Money, OECD Economics Department Policy Notes; No. 2; OECD: Paris, France, 2010. [Google Scholar]
- Velasquez, M.; Hester, P. An Analysis of Multi-Criteria Decision Making Methods. Int. J. Oper. Res. 2013, 10, 56–66. [Google Scholar]
- St. George’s University of London. News 2015, Medical School’s First Graduation Ceremony in Cyprus. Available online: http://www.sgul.ac.uk/news (accessed on 12 May 2016).
- The Economist. The Economist Intelligence Unit, Report: Romania and Tuberculosis; The Economist Intelligence Unit: London, UK, 2015. [Google Scholar]
- Nixon, J.; Ulmann, F. The relationship between health care expenditure and health outcomes. Eur. J. Health Econ. 2006, 7, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Organization for Economic Co-Operation and Development (OECD). Towards a Sustainable Health Care Model. In Proceedings of the OECD Health Ministerial Meeting, Paris, France, 7–8 October 2010.
- Ricciardi, W. (Ed.) White Paper: Acting Together: A Roadmap for Sustainable Health Care; European Steering Group on Sustainable Healthcare: Brussels, Belgium, 2014.
- Bohringer, C.; Jochem, P. Measuring the Immeasurable: A Survey of Sustainability Indices. Ecol. Econ. 2007, 63, 1–8. [Google Scholar] [CrossRef]
- Momete, D.C. Rational Development as a Sustainable Progress Welfare Vector: A Cross-Country Analysis. Sust. Dev. 2016. [Google Scholar] [CrossRef]

| Component | Factor | Actual Data | Reason of Selection | Unit | Desirable |
|---|---|---|---|---|---|
| Inputs | |||||
| Supply/Access (SA) | Medical doctors (1) | Number of health graduates/100,000 inhabitants | Reflects the availability of specialized medical supply and available national supply | Number | max |
| Out of pocket expenditure (2) | Out of pocket expenditure as % of total health expenditure | Reflects the easiness of access to medical care | % | min | |
| Providers of health (PR) | Available hospital beds (3) | Hospital beds/1000 inhabitants | Reflects the ability to provide health care | Number | max |
| Health expenditure (4) | Total health expenditure as a % of GDP | Reflects the will of the Government to support health system | % | max | |
| Outputs | |||||
| Personal health (PH) | Life expectancy at birth total (5) | Healthy life years (the number of years a newborn infant would live if the mortality conditions will be the same) | Reflects expectation of healthy years | Number | max |
| Fertility rate (6) | Number of births/woman | Reflects ability to procreate | Number | max | |
| Diseases control (ID) | Incidence of tuberculosis (7) | Tuberculosis cases/100,000 inhabitants | Reflects the eradication of severe diseases, mainly connected with hygiene, amendable to health prevention and care | Number | min |
| Infant mortality rate (8) | Number of infants dying before reaching one year of age/1000 live births | Reflects the possibly to support new life | Number | min | |
| Geo/Factors | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 | Factor 7 | Factor 8 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Geo/time | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 |
| Austria | 13.07 | 12.13 | 15.10 | 15.81 | 8.54 | 7.65 | 9.58 | 11.03 | 76.67 | 81.14 | 1.42 | 1.44 | 19.00 | 8.40 | 5.70 | 3.20 |
| Belgium | 10.58 | 10.52 | 19.59 | 19.91 | 7.41 | 6.25 | 7.61 | 11.19 | 76.84 | 80.59 | 1.56 | 1.79 | 15.00 | 9.10 | 6.30 | 3.50 |
| Bulgaria | 12.39 | 9.51 | 26.04 | 39.63 | 10.37 | 6.82 | 5.25 | 7.63 | 71.05 | 74.86 | 1.23 | 1.50 | 62.00 | 29.00 | 19.40 | 10.10 |
| Croatia | 9.50 | 12.01 | 13.54 | 12.46 | 5.94 | 5.86 | 7.00 | 7.00 | 72.08 | 77.13 | 1.58 | 1.51 | 54.00 | 13.00 | 8.70 | 3.80 |
| Cyprus | 0.00 | 0.00 | 63.27 | 46.42 | 5.07 | 3.42 | 4.74 | 7.44 | 77.27 | 79.95 | 2.12 | 1.46 | 4.80 | 5.80 | 7.90 | 2.80 |
| Czech Republic | 13.47 | 12.73 | 9.11 | 15.71 | 8.50 | 6.46 | 6.69 | 7.24 | 73.07 | 78.18 | 1.28 | 1.45 | 22.00 | 5.50 | 8.80 | 2.90 |
| Denmark | 6.32 | 18.38 | 16.30 | 12.79 | 4.90 | 3.07 | 8.13 | 10.62 | 75.21 | 80.30 | 1.80 | 1.73 | 11.00 | 7.00 | 5.40 | 2.90 |
| Estonia | 11.21 | 10.93 | 10.23 | 18.89 | 8.35 | 5.01 | 6.32 | 5.72 | 67.54 | 77.14 | 1.38 | 1.56 | 52.00 | 22.00 | 12.80 | 2.70 |
| Finland | 13.94 | 11.47 | 22.65 | 18.54 | 8.12 | 4.86 | 7.85 | 9.40 | 76.41 | 80.98 | 1.81 | 1.80 | 14.00 | 5.70 | 4.30 | 2.10 |
| France | 8.05 | 10.51 | 7.60 | 7.40 | 8.90 | 6.29 | 10.36 | 11.66 | 77.75 | 82.22 | 1.74 | 2.01 | 18.00 | 8.80 | 5.30 | 3.50 |
| Germany | 12.57 | 12.04 | 9.99 | 12.89 | 9.68 | 8.20 | 10.11 | 11.30 | 76.42 | 80.84 | 1.25 | 1.38 | 17.00 | 5.80 | 5.30 | 3.20 |
| Greece | 13.26 | 9.20 | 43.45 | 26.39 | 4.91 | 7.04 | 9.62 | 9.82 | 77.59 | 81.29 | 1.31 | 1.29 | 11.00 | 5.00 | 9.10 | 3.70 |
| Hungary | 9.70 | 15.12 | 16.04 | 27.49 | 8.80 | 7.04 | 7.33 | 8.05 | 69.79 | 75.57 | 1.57 | 1.34 | 48.00 | 18.00 | 12.10 | 5.20 |
| Ireland | 12.86 | 20.25 | 15.34 | 16.84 | 6.97 | 2.76 | 6.56 | 8.92 | 75.57 | 81.00 | 1.84 | 2.01 | 16.00 | 8.50 | 6.10 | 3.20 |
| Italy | 11.99 | 11.18 | 24.71 | 18.01 | 6.27 | 3.38 | 7.06 | 9.09 | 78.17 | 82.69 | 1.19 | 1.43 | 10.00 | 5.70 | 6.40 | 3.00 |
| Latvia | 10.66 | 13.46 | 33.73 | 36.45 | 11.19 | 5.80 | 5.76 | 5.72 | 66.39 | 73.98 | 1.25 | 1.44 | 127.00 | 50.00 | 19.70 | 7.40 |
| Lithuania | 12.01 | 14.81 | 22.39 | 32.63 | 10.94 | 7.28 | 5.37 | 6.24 | 69.01 | 73.91 | 1.55 | 1.60 | 90.00 | 65.00 | 13.50 | 4.00 |
| Luxembourg | 0.00 | 0.00 | 6.19 | 10.80 | 7.10 | 5.05 | 5.57 | 7.10 | 76.51 | 81.80 | 1.70 | 1.57 | 9.80 | 8.70 | 5.20 | 1.60 |
| Malta | 13.15 | 20.31 | 31.14 | 31.53 | 5.43 | 4.80 | 5.63 | 8.73 | 77.14 | 81.75 | 1.53 | 1.72 | 6.30 | 11.00 | 8.30 | 5.40 |
| Netherlands | 7.87 | 14.41 | 9.64 | 5.39 | 5.27 | 4.48 | 8.33 | 12.89 | 77.40 | 81.30 | 1.87 | 1.85 | 12.00 | 6.10 | 5.70 | 3.30 |
| Poland | 10.70 | 9.88 | 27.11 | 22.81 | 5.50 | 6.58 | 5.48 | 6.66 | 71.89 | 77.00 | 1.62 | 1.30 | 48.00 | 22.00 | 12.60 | 4.50 |
| Portugal | 4.08 | 13.64 | 23.92 | 26.63 | 3.92 | 3.40 | 7.52 | 9.71 | 75.31 | 80.72 | 1.41 | 1.28 | 62.00 | 26.00 | 7.50 | 3.10 |
| Romania | 13.29 | 14.83 | 25.46 | 19.69 | 7.64 | 6.67 | 3.22 | 5.34 | 69.46 | 75.06 | 1.33 | 1.53 | 189.00 | 87.00 | 27.30 | 10.50 |
| Slovakia | 12.78 | 12.75 | 11.48 | 22.14 | 8.17 | 5.80 | 6.06 | 8.21 | 72.25 | 76.41 | 1.52 | 1.34 | 34.00 | 7.70 | 12.60 | 6.00 |
| Slovenia | 7.74 | 11.89 | 11.22 | 12.11 | 5.73 | 4.55 | 7.46 | 9.16 | 73.96 | 80.32 | 1.29 | 1.58 | 31.00 | 7.50 | 6.20 | 2.30 |
| Spain | 11.60 | 10.23 | 23.54 | 22.80 | 3.93 | 2.96 | 7.44 | 8.88 | 77.98 | 83.08 | 1.17 | 1.32 | 27.00 | 13.00 | 6.90 | 3.60 |
| Sweden | 8.73 | 10.27 | 13.34 | 16.32 | 4.80 | 2.59 | 7.96 | 9.71 | 78.74 | 81.96 | 1.73 | 1.91 | 7.10 | 7.20 | 4.00 | 2.40 |
| United Kingdom | 6.55 | 13.18 | 10.91 | 9.29 | 4.80 | 2.76 | 6.69 | 9.12 | 76.84 | 81.00 | 1.71 | 1.92 | 12.00 | 13.00 | 6.10 | 3.90 |
| Geo/Utility | U1 | U2 | U3 | U4 | U5 | U6 | U7 | U8 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Geo/time | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 | 1995 | 2013 |
| Austria | 0.94 | 0.60 | 0.84 | 0.75 | 0.83 | 0.79 | 0.26 | 0.22 | 0.64 | 0.90 | 0.89 | 0.75 | 0.92 | 0.96 | 0.93 | 0.82 |
| Belgium | 0.76 | 0.52 | 0.77 | 0.65 | 0.85 | 0.73 | 0.41 | 0.70 | 0.48 | 0.65 | 0.62 | 0.77 | 0.94 | 0.95 | 0.90 | 0.79 |
| Bulgaria | 0.89 | 0.47 | 0.65 | 0.17 | 0.38 | 0.10 | 0.06 | 0.30 | 0.89 | 0.75 | 0.28 | 0.30 | 0.69 | 0.71 | 0.34 | 0.04 |
| Croatia | 0.68 | 0.59 | 0.87 | 0.83 | 0.46 | 0.35 | 0.43 | 0.32 | 0.28 | 0.58 | 0.53 | 0.22 | 0.73 | 0.90 | 0.80 | 0.75 |
| Cyprus | 0.00 | 0.00 | 0.00 | 0.00 | 0.88 | 0.66 | 1.00 | 0.25 | 0.16 | 0.15 | 0.21 | 0.28 | 1.00 | 0.99 | 0.83 | 0.87 |
| Czech Republic | 0.97 | 0.63 | 0.95 | 0.75 | 0.54 | 0.46 | 0.12 | 0.23 | 0.63 | 0.69 | 0.49 | 0.25 | 0.91 | 0.99 | 0.79 | 0.85 |
| Denmark | 0.45 | 0.90 | 0.82 | 0.82 | 0.71 | 0.70 | 0.66 | 0.62 | 0.14 | 0.08 | 0.69 | 0.70 | 0.97 | 0.98 | 0.94 | 0.85 |
| Estonia | 0.80 | 0.54 | 0.93 | 0.67 | 0.09 | 0.35 | 0.22 | 0.38 | 0.61 | 0.43 | 0.43 | 0.05 | 0.74 | 0.79 | 0.62 | 0.88 |
| Finland | 1.00 | 0.56 | 0.71 | 0.68 | 0.81 | 0.77 | 0.67 | 0.71 | 0.58 | 0.40 | 0.65 | 0.54 | 0.95 | 0.99 | 0.99 | 0.94 |
| France | 0.58 | 0.52 | 0.98 | 0.95 | 0.92 | 0.91 | 0.60 | 1.00 | 0.69 | 0.66 | 1.00 | 0.84 | 0.93 | 0.95 | 0.94 | 0.79 |
| Germany | 0.90 | 0.59 | 0.93 | 0.82 | 0.81 | 0.76 | 0.08 | 0.14 | 0.79 | 1.00 | 0.97 | 0.79 | 0.93 | 0.99 | 0.94 | 0.82 |
| Greece | 0.95 | 0.45 | 0.35 | 0.49 | 0.91 | 0.80 | 0.15 | 0.01 | 0.14 | 0.79 | 0.90 | 0.59 | 0.97 | 1.00 | 0.78 | 0.76 |
| Hungary | 0.70 | 0.74 | 0.83 | 0.46 | 0.28 | 0.18 | 0.42 | 0.08 | 0.67 | 0.79 | 0.58 | 0.36 | 0.77 | 0.84 | 0.65 | 0.60 |
| Ireland | 0.92 | 1.00 | 0.84 | 0.72 | 0.74 | 0.77 | 0.70 | 1.00 | 0.42 | 0.03 | 0.47 | 0.47 | 0.94 | 0.96 | 0.91 | 0.82 |
| Italy | 0.86 | 0.55 | 0.68 | 0.69 | 0.95 | 0.96 | 0.02 | 0.21 | 0.32 | 0.14 | 0.54 | 0.50 | 0.97 | 0.99 | 0.90 | 0.84 |
| Latvia | 0.76 | 0.66 | 0.52 | 0.24 | 0.00 | 0.01 | 0.08 | 0.22 | 1.00 | 0.57 | 0.36 | 0.05 | 0.34 | 0.45 | 0.33 | 0.35 |
| Lithuania | 0.86 | 0.73 | 0.72 | 0.34 | 0.21 | 0.00 | 0.40 | 0.44 | 0.97 | 0.84 | 0.30 | 0.12 | 0.54 | 0.27 | 0.59 | 0.73 |
| Luxembourg | 0.00 | 0.00 | 1.00 | 0.87 | 0.82 | 0.86 | 0.56 | 0.40 | 0.44 | 0.44 | 0.33 | 0.23 | 0.97 | 0.95 | 0.95 | 1.00 |
| Malta | 0.94 | 1.00 | 0.56 | 0.36 | 0.87 | 0.85 | 0.38 | 0.60 | 0.21 | 0.39 | 0.34 | 0.45 | 0.99 | 0.93 | 0.82 | 0.57 |
| Netherlands | 0.56 | 0.71 | 0.94 | 1.00 | 0.89 | 0.81 | 0.73 | 0.78 | 0.19 | 0.34 | 0.72 | 1.00 | 0.96 | 0.99 | 0.93 | 0.81 |
| Poland | 0.77 | 0.49 | 0.63 | 0.58 | 0.45 | 0.34 | 0.47 | 0.03 | 0.22 | 0.71 | 0.32 | 0.18 | 0.77 | 0.79 | 0.63 | 0.67 |
| Portugal | 0.29 | 0.67 | 0.69 | 0.48 | 0.72 | 0.74 | 0.25 | 0.00 | 0.00 | 0.14 | 0.60 | 0.58 | 0.69 | 0.74 | 0.85 | 0.83 |
| Romania | 0.95 | 0.73 | 0.66 | 0.65 | 0.25 | 0.13 | 0.17 | 0.34 | 0.51 | 0.73 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Slovakia | 0.92 | 0.63 | 0.91 | 0.59 | 0.47 | 0.27 | 0.37 | 0.08 | 0.58 | 0.57 | 0.40 | 0.38 | 0.84 | 0.97 | 0.63 | 0.51 |
| Slovenia | 0.56 | 0.59 | 0.91 | 0.84 | 0.61 | 0.70 | 0.13 | 0.41 | 0.25 | 0.35 | 0.59 | 0.51 | 0.86 | 0.97 | 0.91 | 0.92 |
| Spain | 0.83 | 0.50 | 0.70 | 0.58 | 0.94 | 1.00 | 0.00 | 0.05 | 0.00 | 0.07 | 0.59 | 0.47 | 0.88 | 0.90 | 0.88 | 0.78 |
| Sweden | 0.63 | 0.51 | 0.87 | 0.73 | 1.00 | 0.88 | 0.59 | 0.86 | 0.12 | 0.00 | 0.66 | 0.58 | 0.99 | 0.97 | 1.00 | 0.91 |
| United Kingdom | 0.47 | 0.65 | 0.92 | 0.91 | 0.85 | 0.77 | 0.57 | 0.88 | 0.12 | 0.03 | 0.49 | 0.50 | 0.96 | 0.90 | 0.91 | 0.74 |
| Geo/Time | 1995 | 2013 | Gain/Loss, % |
|---|---|---|---|
| Austria | 0.7816 | 0.7231 | −7.48 |
| Belgium | 0.7151 | 0.7193 | +0.59 |
| Bulgaria | 0.5227 | 0.3558 | −31.92 |
| Croatia | 0.5978 | 0.5678 | −5.03 |
| Cyprus | 0.5106 | 0.3983 | −21.98 |
| Czech Republic | 0.6737 | 0.6078 | −9.78 |
| Denmark | 0.6725 | 0.7066 | +5.06 |
| Estonia | 0.5570 | 0.5118 | −8.11 |
| Finland | 0.7947 | 0.7006 | −11.85 |
| France | 0.8284 | 0.8265 | −0.24 |
| Germany | 0.7960 | 0.7379 | −7.29 |
| Greece | 0.6416 | 0.6138 | −4.34 |
| Hungary | 0.6103 | 0.5070 | −16.92 |
| Ireland | 0.7432 | 0.7216 | −2.91 |
| Italy | 0.6551 | 0.6097 | −6.92 |
| Latvia | 0.4232 | 0.3192 | −24.57 |
| Lithuania | 0.5732 | 0.4321 | −24.61 |
| Luxembourg | 0.6329 | 0.5941 | −6.13 |
| Malta | 0.6385 | 0.6455 | +1.08 |
| Netherlands | 0.7399 | 0.8036 | +8.61 |
| Poland | 0.5311 | 0.4723 | −11.06 |
| Portugal | 0.5122 | 0.5242 | +2.34 |
| Romania | 0.3179 | 0.3221 | +1.31 |
| Slovakia | 0.6401 | 0.5000 | −21.89 |
| Slovenia | 0.6016 | 0.6598 | +9.68 |
| Spain | 0.6019 | 0.5434 | −9.72 |
| Sweden | 0.7328 | 0.6803 | −7.16 |
| United Kingdom | 0.6598 | 0.6723 | +1.89 |
| EU 28 average | 0.6323 | 0.5884 | −6.94 |
| Country | 1995 | Country | 2013 | Country Type |
|---|---|---|---|---|
| France | 0.8284 | France | 0.8265 | Group I: Sustainable countries in terms of health system ISH > 0.70 |
| Germany | 0.7960 | Netherlands | 0.8036 | |
| Finland | 0.7947 | Germany | 0.7379 | |
| Austria | 0.7816 | Austria | 0.7231 | |
| Ireland | 0.7432 | Ireland | 0.7216 | |
| Netherlands | 0.7399 | Belgium | 0.7193 | |
| Sweden | 0.7328 | Denmark | 0.7066 | |
| Belgium | 0.7151 | Finland | 0.7006 | |
| Czech Republic | 0.6737 | Sweden | 0.6803 | Group II: Countries on track towards sustainable health 0.70 < ISH < 0.50 |
| Denmark | 0.6725 | United Kingdom | 0.6723 | |
| United Kingdom | 0.6598 | Slovenia | 0.6598 | |
| Italy | 0.6551 | Malta | 0.6455 | |
| Greece | 0.6416 | Greece | 0.6138 | |
| Slovakia | 0.6401 | Italy | 0.6097 | |
| Malta | 0.6385 | Czech Republic | 0.6078 | |
| Luxembourg | 0.6329 | Luxembourg | 0.5941 | |
| Hungary | 0.6103 | Croatia | 0.5678 | |
| Spain | 0.6019 | Spain | 0.5434 | |
| Slovenia | 0.6016 | Portugal | 0.5242 | |
| Croatia | 0.5978 | Estonia | 0.5118 | |
| Lithuania | 0.5732 | Hungary | 0.5070 | |
| Estonia | 0.5570 | Slovakia | 0.5000 | |
| Poland | 0.5311 | Poland | 0.4723 | Group III: Unsustainable countries in terms of health system ISH < 0.50 |
| Bulgaria | 0.5227 | Lithuania | 0.4321 | |
| Portugal | 0.5122 | Cyprus | 0.3983 | |
| Cyprus | 0.5106 | Bulgaria | 0.3558 | |
| Latvia | 0.4232 | Romania | 0.3221 | |
| Romania | 0.3179 | Latvia | 0.3192 |
© 2016 by the author; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Momete, D.C. Building a Sustainable Healthcare Model: A Cross-Country Analysis. Sustainability 2016, 8, 836. https://doi.org/10.3390/su8090836
Momete DC. Building a Sustainable Healthcare Model: A Cross-Country Analysis. Sustainability. 2016; 8(9):836. https://doi.org/10.3390/su8090836
Chicago/Turabian StyleMomete, Daniela C. 2016. "Building a Sustainable Healthcare Model: A Cross-Country Analysis" Sustainability 8, no. 9: 836. https://doi.org/10.3390/su8090836






