1. Introduction
Many cancers metastasize via the lymphatic system, including melanoma, breast, colon, lung, and ovarian cancers [
1,
2]. Accurate determination of which nodes are involved in initial lymphatic spread plays a key role in prognosis and treatment. In melanoma for example, the five year survival rates are >90% for localized disease with no lymphatic involvement, 40–60% if 1 to 3 local nodes are involved, and 15–20% when distant lymph nodes and extra nodal sites are involved [
3]. The clinical method for determining the first draining lymph node or sentinel lymph node (SLN) has not changed significantly since its first use in the 1960s. Sentinel lymph node biopsies have been widely used for clinical staging of melanoma and breast cancer since the early 1990s [
4,
5,
6,
7,
8].
SLN mapping involves injection of dye proximal to the primary tumor before imaging or clinical examination. Dyes include (isosulfan blue, patent blue, or methylene blue) or
99mTc-sulfur colloid singly or in combination. Both dye and colloid drain to the regional lymphatic vessels and regional nodes that fuel the SLNs, which is observed visually for dyes, or with a gamma camera, for
99mTc colloids. Each method has its own disadvantages. Dyes suffer from rapid dispersion and lack of localization to only the SLN, risk of anaphylaxis, and propensity for long term staining of skin. Technetium-99m disadvantages include low resolution and radioactivity risks [
4,
9,
10]. Because accurate SLN and lymphatic mapping is crucial in clinical tumor staging, there is a need for new imaging agents for lymphatic mapping.
Several nanoparticles have been evaluated for lymphatic imaging, including liposomes, micelles, quantum dots (QDs), and iron nanoparticles [
11]. Particulate uptake into lymphatic capillaries after subcutaneous administration depends on size, charge, and hydrophobicity; macrophage uptake depends predominantly on size [
12,
13]. Due to the natural structure of the clefts and pores along the lymphatic capillaries and the presence of aqueous channels (100 nm in diameter) within the interstitium [
14], particles with sizes of 10 to 100 nm are preferentially taken up by the lymphatics [
13,
15]. In contrast, particles > 100 nm largely remain at the injection site as a depot, and particles < 10 nm are reabsorbed by the blood capillaries. Though it is generally accepted that the pores in blood capillaries in the skin are
ca. 5 nm in diameter and non-fenestrated, it has been shown that capillaries of rodent footpads are fenestrated with pores of 6 to 12 nm [
16,
17,
18], thus the use of the 10 nm cutoff rather than 5 nm for lymphatic targeting. It also has been shown that particulates carrying a net negative charge have enhanced lymphatic uptake and retention in lymph nodes [
13,
19,
20,
21].
Fluorescent probes are used extensively for preclinical imaging of research animals and increasingly for image-guided surgeries in human patients. To enhance signal to noise ratios for
in vivo imaging, the emission of the fluorophores must be in the near infrared (NIR) range (600–1000 nm) where there is minimal autofluorescence of hemoglobin, elastin, collagen, chlorophyll (from food), and various other biological chromophores [
22,
23]. The two chromophores commonly used for
in vivo imaging are QDs and NIR organic fluorophores. QDs have several qualities ideal for
in vivo imaging, including inherently bright fluorescence, narrow emission spectra, high quantum yields, excellent photostability, and small size (5 to 20 nm) [
24,
25]. However, the principal concern with the use of QDs is the toxicity associated with the use of the heavy metals Cd, Te, and Se in QDs cores’ construction. The size and charge of the QDs dictate their clearance mechanism and residence time
in vivo. Because of the considerable toxicity concerns, the size of the QDs is limited to less than 6 nm to ensure renal clearance and minimize tissue exposure [
22,
26]. Larger and negatively to neutrally charged (e.g., PEG coated) QDs have shown significant liver and spleen retention, from 1 to 6 months [
24,
25]. Thus, even though QDs can be conjugated to therapeutic drugs for theranostic applications, are the correct size, and are photostable in the NIR range, toxicity and bioretention may limit their utility.
We developed an organic NIR fluorophore-polymer conjugate for
in vivo imaging based off hyaluronan, which meets many of the ideal qualities for an
in vivo imaging agent. Hyaluronan (HA) is a natural polysaccharide distributed widely in the extracellular space and approved in the US for intraarticular injections, and to use as dermal fillers, and to replace the vitreous during occular surgery. Anionic polymer HA is non-immunogenic and hydrophilic, and its size can be varied by changing the molecular weight. In addition to meeting the requirements for lymphatic uptake and dissemination, HA’s primary receptors, CD44 and RHAMM, are overexpressed on most malignant cancer cells [
27,
28,
29], including invasive breast cancer and melanomas [
30]. Our previous studies of targeted lymphatic delivery using 35-kDa HA-chemotherapeutic conjugates (e.g., cisplatin and doxorubicin) demonstrated improved efficacy, decreased toxicity, and superior pharmacokinetics compared to their standard intravenous counterparts [
31,
32,
33,
34,
35,
36]. Herein, we describe the kinetics and optimization of the lymphatic uptake of a series of different molecular weight (6.4 kDa to 697 kDa) hyaluronan-NIR dye conjugates after subcutaneous injection in healthy and tumor-bearing mice.
2. Experimental Section
2.1. Materials
Sodium hyaluronate from microbial fermentation was purchased from Lifecore Biomedical (Chaska, MN, USA) and was used without further purification. All other reagents were purchased from Sigma Aldrich Chemical Co. (St. Louis, MO, USA) or Thermo Fisher Scientific (Waltham, MA, USA) and were ACS grade or better. D2O and CDCl3 were purchased from Cambridge Isotope Laboratories (Andover, MA, USA). PEG standards were obtained from Scientific Polymer Products (Ontario, NY, USA). B16F10 cells were purchased from the American Type Culture Collection (ATCC, Manassas, VA, USA) and were maintained in DMEM supplemented with 10% fetal bovine serum and under a 5% CO2 atmosphere. All animal procedures were approved by the University of Kansas Animal Care and Use Committee.
2.2. Synthesis of 5-Carboxypentyl-amino-IR-820
The 6-aminohexanoic acid (2 eq.) was dissolved in 20 mL of dry DMF with 2 eq. of triethylamine, and the solution was stirred under argon for ca. 5 min. After the addition of 500 mg (0.47 mmol) of IR-820, the reaction mixture was refluxed at 85 °C for 3 h in the dark. The solvent was removed under reduced pressure, and the 5-carboxypentyl-amino-IR-820 was purified by silica column chromatography using a gradient of 2:1 to 1:1 ethyl acetate: methanol. Identity of the blue 5-carboxypentyl-amino-IR-820 solid was confirmed by 1H NMR (400 MHz, Bruker) in CDCl3; 1H NMR (CDCl3, 400 MHz): δ = 8.13 (d, J = 8.4 Hz, 2H), 7.98–7.91 (m, 4H), 7.63 (d, J = 13.2 Hz, 2H), 7.56–7.52 (m, 4H), 7.35 (t, J = 8.0 Hz, 2H), 5.77 (d, J = 15.2 Hz, 2H), 4.06–4.00 (m, 4H), 3.05 (q, J = 12.4 Hz, 6.4 Hz, 1H), 2.57-2.51 (m 4H), 2.16 (t, J = 6.4 Hz, 2H), 2.07 (t, J = 7.2 Hz, 1H), 1.88 (bs, 11H), 1.82–1.68 (m, 14 H), 1.62–1.53 (m, 3H), 1.48–1.35 (m, 4 H), 1.28–1.22 (m, 1H).
2.3. Synthesis of HA-IR820 Conjugates
The 5-carboxypentyl-amino-IR-820 was dissolved in ddH
2O (<20 mL) with
N-(3-dimethylaminopropyl)-
N′-ethylcarbodiimide hydrochloride (EDAC, 1.2 eq, dye basis) and 4-(dimethylamino)pyridine (DMAP, 0.5 eq., dye basis), the pH was adjusted to 4.0 to 4.5, and the solution was stirred for approximately five minutes. Sodium hyaluronate (100 mg) was dissolved in 10 mL of ddH
2O and added to the solution (see
Table 1 for molar equivalents of reagents used). The mixture was stirred at ambient temperature (
ca. 20 °C) in the dark. The reaction was monitored by thin layer chromatography, using 6:4:1 methanol: ethyl acetate: dichloromethane as the mobile phase; the total reaction time was typically 1 to 5 days and increased with HA molecular weight. The HA-IR820 conjugate was dialyzed once against 95% ethanol and twice against ddH
2O. The purple HA-IR820 conjugate was lyophilized and stored at −20 °C until further use. The ratio of the
1H NMR peaks in D
2O of the acetamide methyl of HA and the third methylene groups on the 5-carboxypentyl-amino linker moiety were used to determine the dye content per HA polymer.
Table 1.
Molar equivalents of each reagent used in the conjugation of 5-carboxypentyl-amino-IR-820 (dye) to each MW of HA to form the HA-IR820 conjugates.
Table 1.
Molar equivalents of each reagent used in the conjugation of 5-carboxypentyl-amino-IR-820 (dye) to each MW of HA to form the HA-IR820 conjugates.
| HA MW (kDa) | Dye Equivalents | EDAC Equivalents | DMAP Equivalents |
|---|
| 6.4 | 1.5 | 1.8 | 0.75 |
| 35 | 3 | 3.6 | 1.5 |
| 74 | 10 | 12 | 5 |
| 132 | 25 | 30 | 12.5 |
| 357 | 50 | 60 | 25 |
| 697 | 100 | 120 | 50 |
2.4. Size Exclusion Chromatography
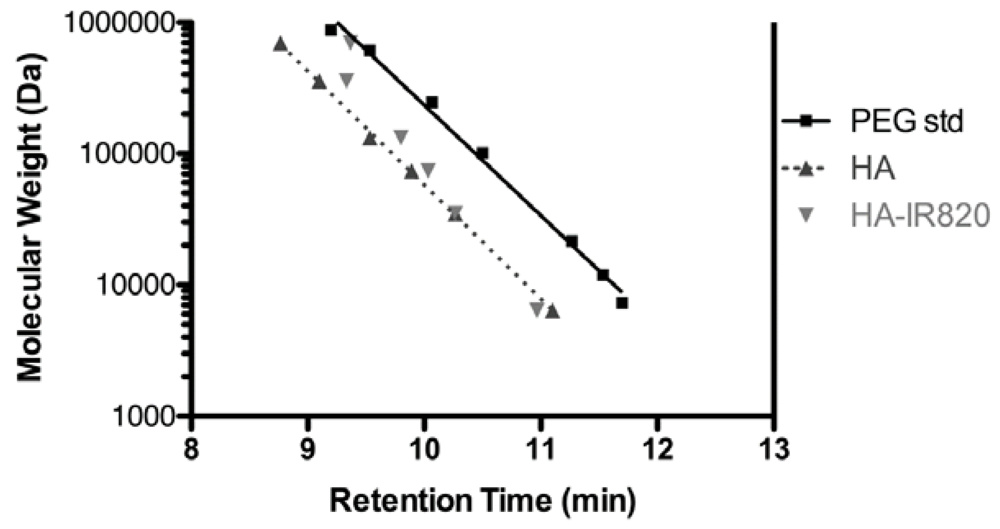
Conjugation of IR-820 dye to HA was verified by equivalent size exclusion chromatography (SEC) column retention times using evaporative light scattering (ELSD) and UV detection. HA of the same molecular weights (MW) used in conjugation reactions and PEG standard samples were used to generate a calibration curve, and the retention times of HA-IR820 were compared to that of HA and PEG to determine MW changes post conjugation reactions. All SEC traces were collected using a Shodex OHpak SB-806M HQ column thermostated at 35 °C, with 0.8 mL/min mobile phase of 5-mM acetate buffer adjusted to pH 5. Detection was with a UV detector (Shimadzu LC2010CHT) (λ = 520 nm) and an evaporative light scattering detector (Shimadzu ELSD-LT II, 70 °C and 3.6 bar purified air).
2.5. Fluorescence
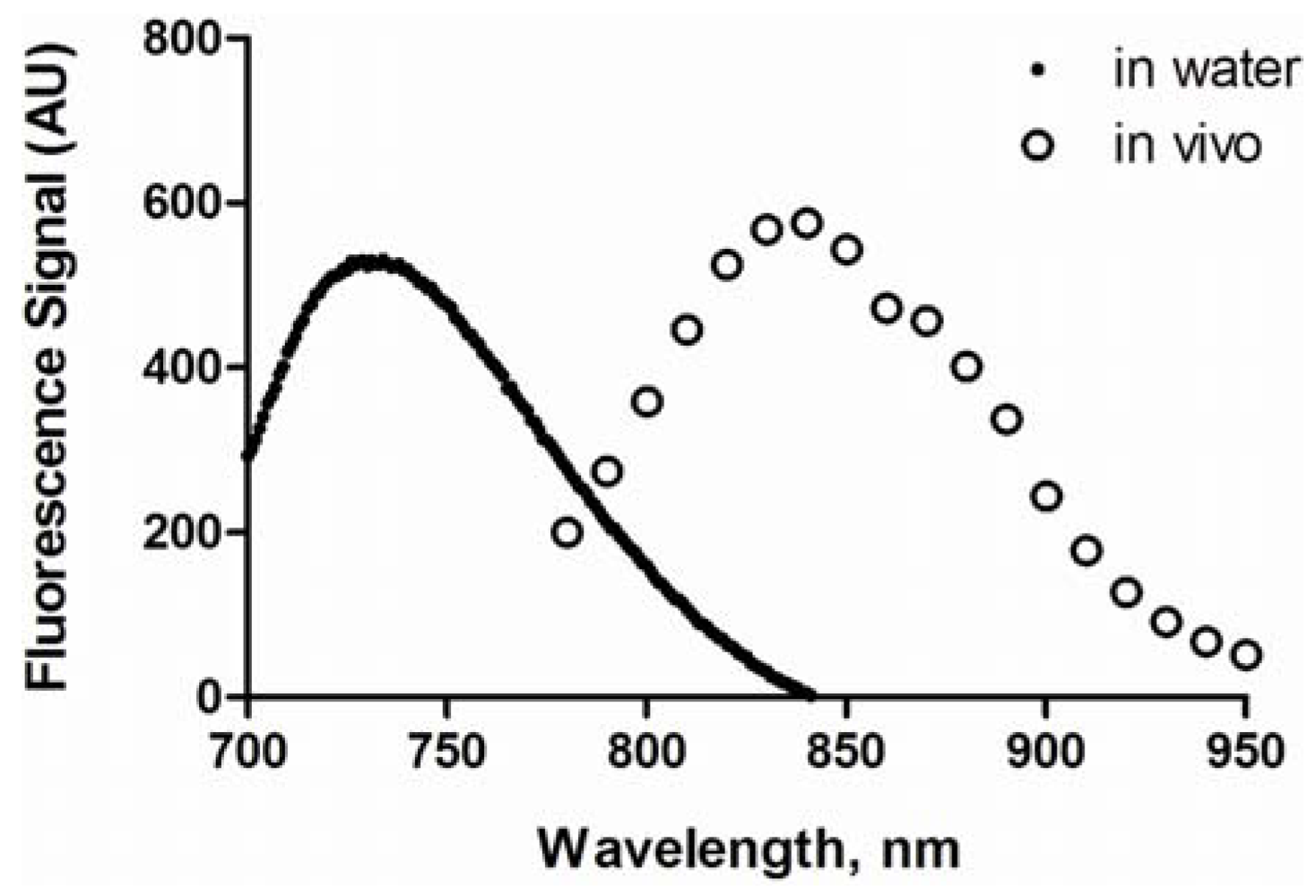
The HA-IR820 samples were dissolved in ddH2O at a concentration of 0.1 mg/mL of IR-820. The maximum excitation and emission wavelengths were determined using a fluorescent spectrophotometer (Shimadzu RF-5301 PC, Columbia MD; Panorama Fluorescence Software). The total fluorescence emission spectrum (λex = 700 nm, λem = 800–900 nm) was determined for the HA-IR820 samples, which was used for the normalization of the in vivo imaging data.
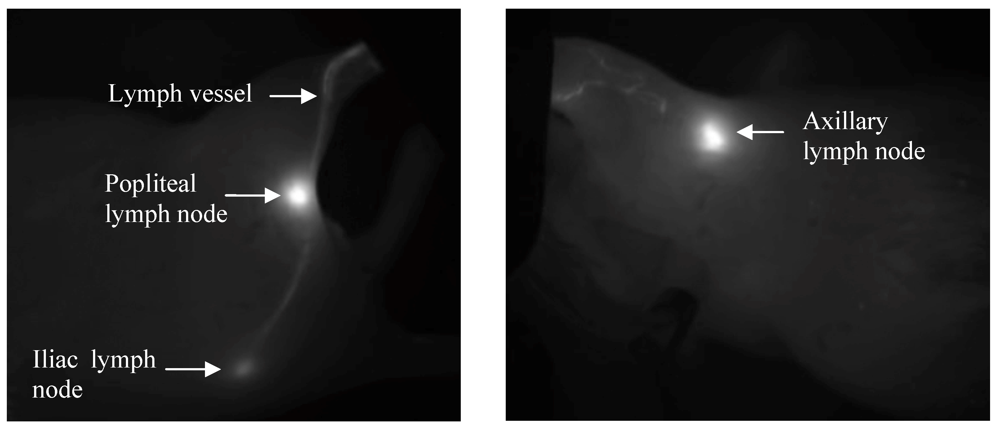
2.6. In Vivo Imaging
All mice were fed a low chlorophyll diet at least one week prior to imaging to decrease food induced organ and skin autofluorescence (Harlan 2918 irradiated diet). The mouse’s hair in the area of interest for imaging was removed 24 h prior to imaging with clippers followed by depilatory cream. Female BALB/c mice (20–25 g, Charles River) (3 per group) were anesthetized under isoflurane, placed on a heating pad to help regulate body temperature, and were injected subcutaneously (s.c.) with 10 μL of a 1-mg/mL 5-carboxypentyl-amino-IR-820 or HA-IR820 (dye basis) in the center of the right hind footpad or on the inner-side of the right front forearm. The mice were imaged on both the dorsal and right sides (for footpad injections) or ventral and right sides (for front forearm injections), both with and without the injection site being covered, using whole body fluorescent imaging (Cambridge Research and Instrumentation Maestro multi-spectrum imager, Woburn, MA, USA) with an excitation filter of 710–760 nm and long pass emission filter of 800–950 nm. The animals were imaged for 7 days in the footpad studies and 14 days in the forearm studies. Images were acquired using the autoexposure function in the imaging software to prevent pixel saturation.
For the imaging studies in tumor-bearing mice, tumors were developed by injecting a 50-μL suspension of B16F10 cells (1.1 × 108 cells/mL) s.c. into the right hind thigh of female BALB/c mice (20–25 g, Charles River, n = 5) under isoflurane anesthesia (Day 1). The mouse’s hair in the area of interest for imaging was removed 24 h prior to imaging (Day 3) with clippers followed by depilatory cream. On day 4, mice with similar tumor volume, shape, and location were chosen for the imaging study. Three mice were anesthetized under isoflurane anesthesia, placed on a heating pad to regulate body temperature, and were injected subcutaneously with 10 μL of a 1.0-mg/mL solution (IR-820 dye basis) of 74-kDa HA-IR820 in the center of the right hind footpad. The mice were imaged on both the dorsal and right sides, both with and without covering the injection site, at predetermined time intervals using a whole body fluorescence imager. The animals were imaged for a maximum of seven days. Images were acquired using the autoexposure function in the imaging software.
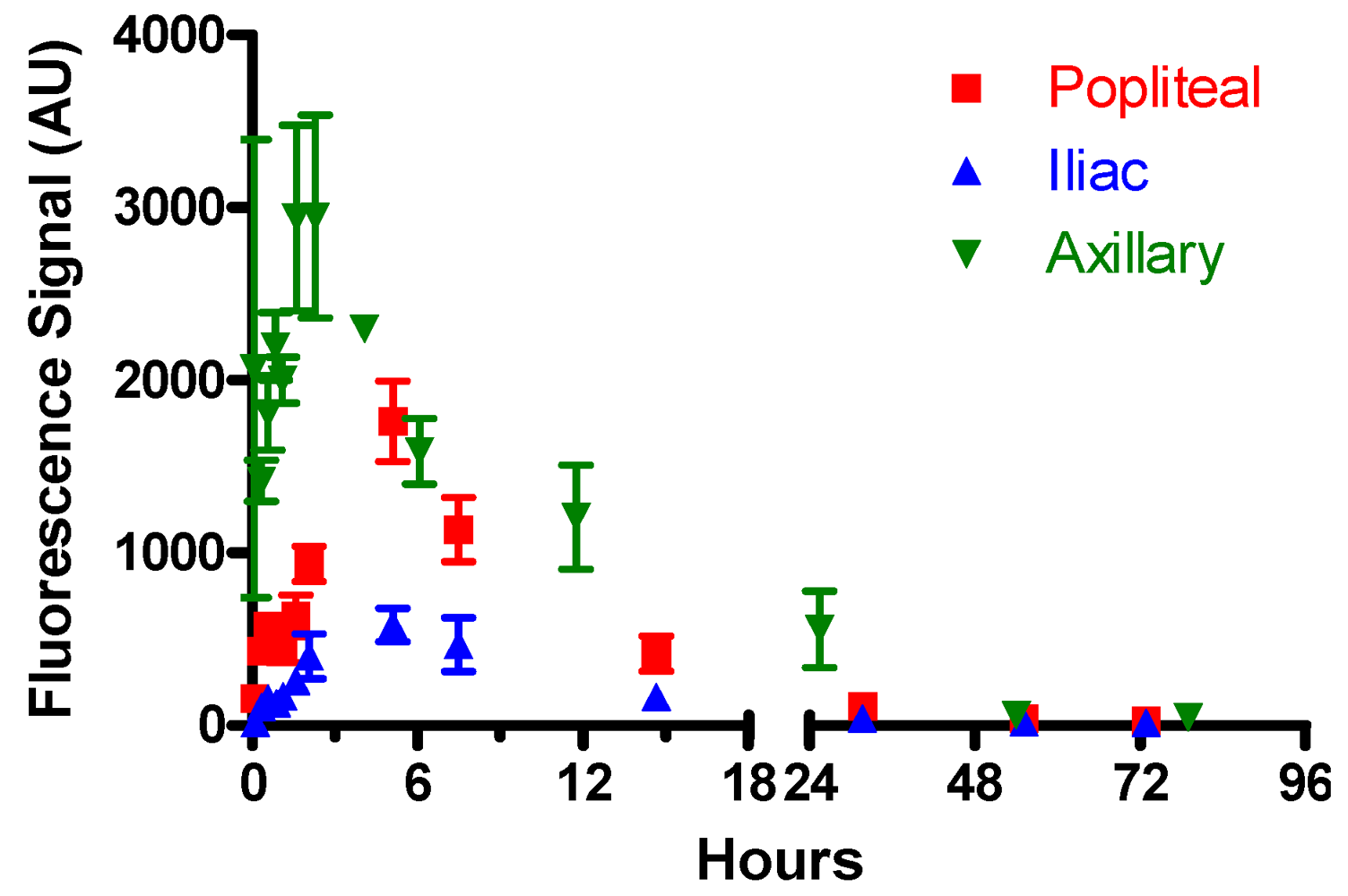
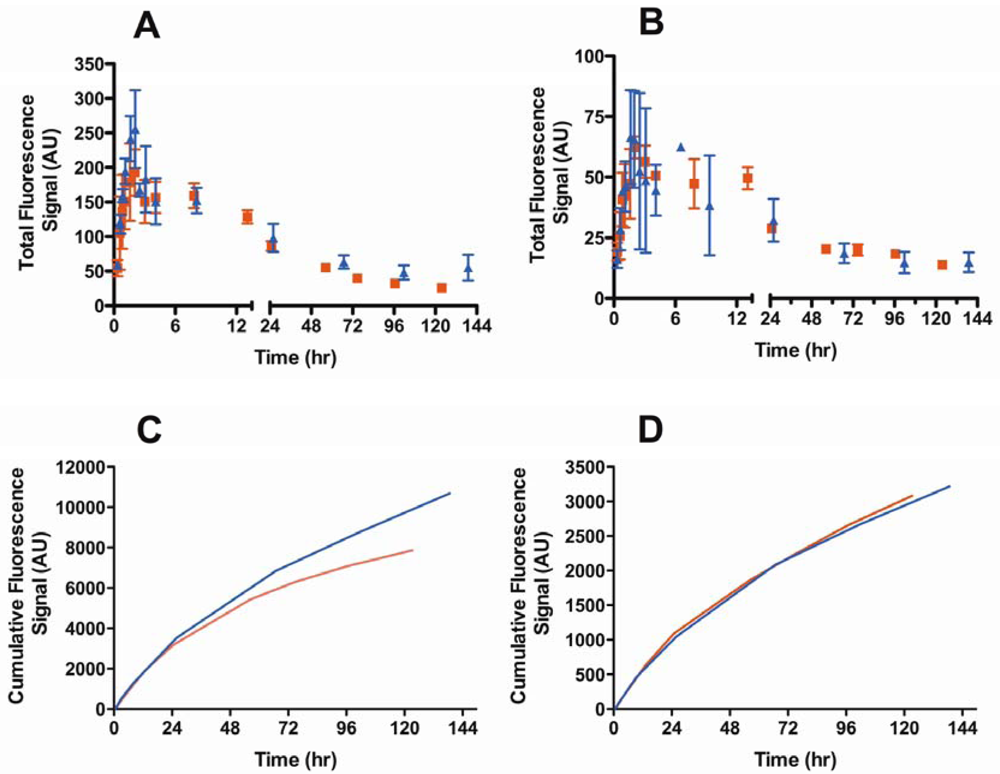
2.7. Data Analysis
Image analysis was performed using Maestro software (version 2.10; CRi Maestro Caliper Life Sciences: Hopkinton, MA, USA, 2010). Regions of interest were placed over the popliteal and iliac lymph nodes or axillary lymph node package. The total signal (scaled counts/s) intensity values (arbitrary units, AU) were recorded for each region of interest (ROI), for all positions (dorsal, ventral, and right sides), and were plotted versus time in GraphPad Prism (version 4, GraphPad Software Inc., La Jolla, CA, USA, 2007). The total integrated fluorescence was determined for each HA-IR820 sample (0.1 mg/mL IR-820) emission spectrum (λex = 700 nm, λem = 800–900 nm), which was used to normalize the ROIs for each HA-IR820 sample. The normalized ROI vs. time graphs were integrated to calculate the cumulative fluorescence over time. In addition, the area under the curve (AUC) was determined from the normalized ROI vs. time graphs.
4. Conclusions
We optimized the molecular weight of HA for use as a combined carrier for lymphatic imaging and drug delivery. Hyaluronan with a molecular weight of 74 kDa was determined to be optimal for lymphatic imaging due to its maximal lymphatic uptake and enhanced lymph node retention. This corresponds to a size of
ca. 30 to 50 nm, which is consistent with the reported optimal size for lymphatic uptake of liposomes as well [
53]. Previous studies that optimized particulate size for enhanced lymphatic uptake have used either dendrimers between 5 and 20 nm in size, which are so small they are near the size for capillary uptake [
64,
65], or liposomes and other nanoparticles with non-uniform compositions that vary over an extremely wide size range (100–150 nm spread) [
13,
53,
55]. In addition to variable sizing, the non-uniform particles in prior studies often have very different overall charges or hydrophobicities, and even go so far as to use non-uniform protein compositions [
66]. These variables further complicated prior attempts to define the effect of size on lymphatic uptake. We addressed this by using a single polymer, HA, so that resulting differences in uptake kinetics were independent of charge or hydrophobicity. Since HA is a linear polymer, the molecular weight is directly proportional to the number of surface carboxylic acid groups. In contrast, the number of surface groups on dendrimers increases exponentially with molecular weight, and charge can vary with size changes due to increased exposure of the more hydrophobic core.
Hyaluronan is more favorable for clinical imaging than non-biodegradable imaging agents, such as PAMAM dendrimers and QDs. Hyaluronan is used in several clinical products, and we observed no toxicities over several weeks in these studies. Agents such as QDs must be limited to 5 nm or less in size for renal clearance, but even so they are susceptible to prolonged bioretention and heavy metal leakage. In addition, most dendrimers currently under investigation contain multiple amino groups that must be further functionalized with neutral PEG or anionic ligands to reduce their cationic nature and mitigate their toxicity [
67].
Hyaluronan holds great promise as a natural biopolymer for drug delivery and lymphatic imaging in the clinic. It is non-immunogenic, non-toxic, and it naturally degrades within the lymphatics and liver unlike most other drug delivery platforms. We have shown that the retention of HA within the nodal tissues can be tailored from a period of hours to days; this makes HA conjugates suitable for both sustained drug delivery and long-term imaging of the lymphoid tissues.