Abstract
Prion diseases or transmissible spongiform encephalopathies are a unique category of infectious protein-misfolding neurodegenerative disorders. Hypothesized to be caused by misfolding of the cellular prion protein these disorders possess an infectious quality that thrives in immune-competent hosts. While much has been discovered about the routing and critical components involved in the peripheral pathogenesis of these agents there are still many aspects to be discovered. Research into this area has been extensive as it represents a major target for therapeutic intervention within this group of diseases. The main focus of pathological damage in these diseases occurs within the central nervous system. Cells of the innate immune system have been proven to be critical players in the initial pathogenesis of prion disease, and may have a role in the pathological progression of disease. Understanding how prions interact with the host innate immune system may provide us with natural pathways and mechanisms to combat these diseases prior to their neuroinvasive stage. We present here a review of the current knowledge regarding the role of the innate immune system in prion pathogenesis.
1. Introduction
1.1. Prion Diseases
Prion diseases or transmissible spongiform encephalopathies (TSEs) are infectious neurodegenerative conditions characterized by vacuolar degeneration of the central nervous system (CNS) and deposition of an abnormal isoform of the host-encoded prion protein (PrP). These diseases affect a wide variety of animal species and display limited zoonotic potential. Usually displaying prolonged incubation periods, they are clinically recognized via progressive neurological deterioration resulting from synaptic and neuronal loss and associated activated glial responses to CNS damage. Identification of genetically inherited forms of these diseases implicate further the critical role of the prion protein in disease pathogenesis and their classification as protein-misfolding disorders, with similarities to other progressive dementias such as Alzheimer’s and Parkinson’s diseases and amyotrophic lateral sclerosis. Sporadic prion diseases, with no known genetic risk factor or exposure to infection, have also been identified. The disease-associated isoform of the prion protein gains several properties including ability to transmit infection, limited protease resistance, and increased ability to fibrillize and form amyloid, these observations on both etiology and biochemical nature of the agent resulted in the prion hypothesis [1].
The prion hypothesis proposed that the infectious agent may be solely composed of a proteinaceous particle, i.e., the disease-associated isoform of the prion protein (PrPSc), with the means to self-propagate via an auto-catalytic process of template-mediated refolding of the nascent cellular prion protein (PrPC). The pathway and mechanisms from refolding of the prion protein to neurodegeneration are still unknown. The peripheral pathogenesis of these diseases have been extensively studied using animal models, as mice are naturally susceptible to both sheep scrapie and bovine spongiform encephalopathy (BSE). Following natural peripheral exposure to prion agents, infection is usually sequestered to lymphoid organs prior to invasion of the nervous system (termed neuroinvasion) [2,3]. In the absence of local draining lymphoid tissue, subsequent circulation to other lymphoid organs and neuroinvasion are ultimately blocked [4,5]. Using transgenic mouse models or bone marrow chimeric mouse models various hypotheses regarding the genes and cells involved in the prion infectious pathway have been proven or refuted. Though often contradictory, results from these studies have revealed that disease-associated PrP is deposited in lymphoid follicles and replicates upon follicular dendritic cells (FDCs). This stage of pathogenesis has been shown to be dependent upon expression of cellular prion protein by FDCs [6,7]. The lymphoid stage of prion pathogenesis is not always obligatory and is dependent upon various factors including: the host, strain of infectious agent, route of infection and infectious dose [8,9,10,11]. Experimental delivery of prion agent directly to the nervous system may facilitate direct neuroinvasion [12,13]. Direct delivery of the prion agent to the central nervous system may bypass peripheral pathogenesis completely resulting in infection in naturally resistant hosts [14,15]. Concurrent lymphoid sequestration of infection likely still occurs after direct CNS infection and may play a role in subsequent pathogenesis [15,16].
Originating from the stromal cell compartment FDC are specialized cells that capture and retain antigen for presentation to cognate B-cells and subsequent generation of specific antibody responses and thus reside within primary B-cell follicles and germinal centers within lymphoid tissues [17,18]. Due to the reliance of FDCs on lymphotoxin signaling from B-cells to maintain FDC homeostasis [19], immune-compromised models lacking mature FDCs reveal deficits in peripheral prion pathogenesis. As such a positive relationship has been firmly established between the immune-competence of the host and ability to support prion pathogenesis. As with most infectious agents, typical pathogenesis occurs via the preferred route often as a compromise between the agent and the host. Prevention or blocking of this route may promote adaption or alternative pathways of pathogenic activity. For example blocking of intestinal Peyer’s patch formation prior to oral prion infection led to pathogenesis via FDC contained within isolated lymphoid follicles [4]. Similar altered pathogenic routes may be induced following splenectomy or sympathectomy [3,20]. Data obtained from prion pathogenesis studies reveal that rarely infection is blocked completely and more often disease is attenuated, revealing alterations to well-definable characteristics such as the disease incubation period or targeting of pathological changes both peripherally and within the host CNS. The difficulties in analyzing such data are compounded by the problems of global host models (i.e., gene-knockout) that effect both peripheral and CNS innate or adaptive immune responses. Despite these difficulties several clear messages have been received regarding the role of specific components of the innate immune system, some of which are less inter-dependent than the systems regulating the adaptive immune response, which we review and summarize below.
1.2. The Innate Immune System
The innate immune system is considered to be a protective system that is older in evolutionary terms than the adaptive immune system. This system was originally proposed to respond in a non-specific way to invading pathogens in an attempt to eliminate them or their activity, whilst alerting or informing the adaptive immune response. As such the innate immune system confers no immunological memory or lasting protective immunity. The identification and characterization of specific pattern recognition receptors, such as Toll-like (TLR), C-type lectin (CLR), NOD-like (NLR) and RIG-I-like (RLR) receptors, has revealed the diversity of the innate immune system to detect and tailor specific responses to pathogen-associated molecular patterns (PAMPs) [21,22,23,24]. In line with the innate immune system constituting the first line of active defense after physical barrier mechanisms, a significant portion of the cellular component is pre-localized to potential exposure sites. This tissue-resident, or homeostatically maintained, population primarily assesses and responds to insults accordingly, and likely deals effectively with acute insults. A large systemic pool of both cellular (inflammatory) and proteinaceous components of the innate immune system also exists, to be mobilized rapidly in response to signals from epithelia or resident innate immune cells. Below we consider various components of the innate immune system, both cellular and proteinaceous, and their possible roles in prion pathogenesis (summarized in Figure 1).
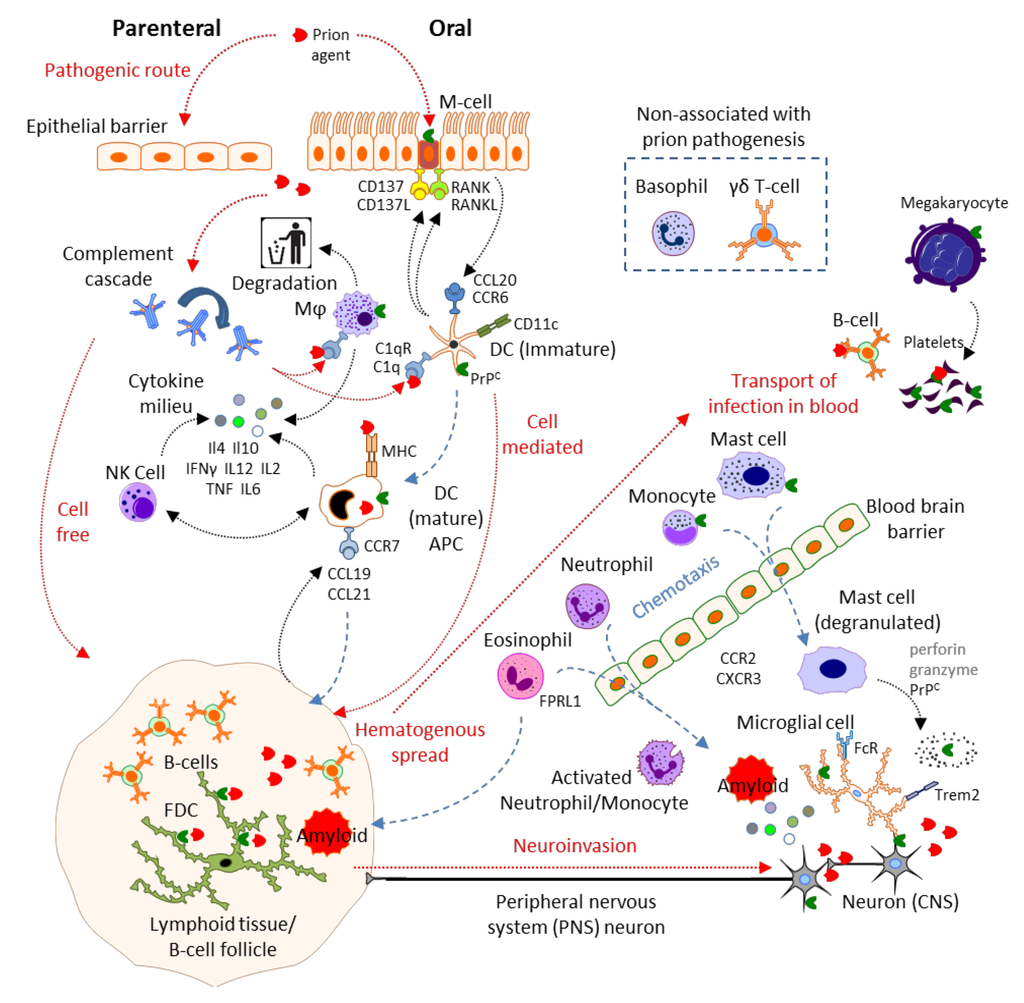
Figure 1.
Prion disease and the innate immune system. Adapted with permission from motifolio.com, Biomedical PowerPoint Toolkit Suite.
2. Results and Discussion
2.1. Physical Barrier to Infection: Epithelial Cells, Microfold Cells
The epithelial cell layers constitute the first physical barrier to infection. Prion infection via the skin is experimentally facilitated by scarification or breaking of the keratinized epidermal barrier layers to allow access to the epithelial layer beneath [25]. Prion infection via the oral or nasal route appears to be naturally more efficient. Prion pathogenesis can be greatly enhanced by disruption of the epithelial layers involved in these routes [26,27]. Under steady state conditions oral uptake of prion infection occurs via specialized microfold cells (M-cells) localized to the follicle-associated epithelium (FAE) of intestinal Peyer’s patches [28,29]. The developmental maturation of M-cells has been shown to require CD137 signaling, with CD137 ligand provided by hematopoietic cells (either B-cells or dendritic cells) [30]. To provide this signal hematopoietic cells are likely required to localize to the sub-epithelial vicinity via chemotaxis mediated by C-C chemokine receptor type 6 (CCR6) responding to C–C chemokine ligand 20 (CCL20), as M-cells do not form if CCR6-CCL20 signaling is prevented [31,32]. The PrPC expressed by M-cells has been hypothesized to function as an uptake receptor for pathogenic bacteria [33]. Translocated PrPSc has also been observed on enterocyte derived extracellular vesicles suggesting an M-cell independent pathway for prions to cross epithelial barriers [34]. Lumenal sampling by dendritic cells (DC) has been observed [35]. Although this activity by classical DC is rare under steady-state conditions it suggests an additional potential prion uptake mechanism. The de-differentiation of M-cells prior to oral scrapie infection was sufficient to block pathogenesis completely [29], indicating that prion uptake via epithelial and DC mechanisms are insufficient to establish infection in the steady state. The incidence of DC sampling increased following epithelial TLR signaling [36]. Thus the possibility of coincident bacterial infection or other inflammatory stimuli enhancing prion uptake to threshold levels via this mechanism are worthy of further investigation.
Following uptake and translocation across the epithelial barrier layer, prions are then free to encounter other elements of the innate immune system. Directly beneath the FAE and within basolateral pockets of the M-cells themselves are areas enriched in classical DC, macrophages (Mϕ) and lymphocytes termed the subepithelial dome (SED), precisely located so as to process incoming antigen. The final physical barrier to prion pathogenesis appears to be the distance between site of entry and FDC and subsequently between FDC and peripheral nerves. Innervation of the lymphoid organs has been shown to be critical for prion neuroinvasion [20]. Manipulation to shorten the distance between FDC and peripheral nerves has shown to increase the rate of neuroinvasion [37]. These data provide a strong argument against hematogenous spread of prion agent directly to the CNS. Following aerosol exposure, prion pathogenesis occurs independently of the immune system, FDC, B cells, T cells, NK cells, lymphotoxin β receptor or CD40 ligand signaling [11].
2.2. Complement
The complement system is composed of numerous blood borne proteins that are generally synthesized in the liver and circulate as inactive precursors or pro-proteins. Significant amounts of complement components are also synthesized locally by tissue-resident mononuclear phagocytes (MNPs) [38,39], epithelial and stromal cells such as FDC [40]. The complement system is activated by numerous triggers that establish a proteolytic cleavage cascade, amplifying the response and typically resulting in the formation of the membrane attack complex (MAC). The classical complement activation pathway is triggered mainly by antigen-antibody complexes. Alternative activation pathways exist wherein complement component C3b may bind directly to foreign material (alternative pathway) or where mannose-binding lectin recognizes and binds to sugar moieties (lectin pathway) both associated with pathogenic microorganisms. The MAC functions to form transmembrane pores, thereby punching holes in pathogenic cells with the aim of promoting cell lysis and death.
Complement has been shown to be activated early during prion pathogenesis by as yet undetermined mechanisms and may constitute the first active response to infection. Prion protein has been shown to be directly bound by C1q and Factor H [41] and this binding occurs specifically when prion protein is conformationally modified to represent the conversion to the disease-associated isoform [42]. The role of complement in prion pathogenesis has recently been subject to review [43]. In brief prion or TSE agents are opsonized by complement components including C1q and C3, most likely via the classical complement activation pathway, which may aid in their targeting of the agent to lymphoid follicles. Mice lacking in complement components C1qa, C2 or C3 revealed deficient peripheral prion pathogenesis under specific conditions [44,45].
The local production of complement components by MNP has been shown to alter their function [46]. C1q enhances the receptor-mediated uptake of disease-associated PrP by classical dendritic cells (see section 2.4.2 below) [47]. The association of C1q with PrPSc may alter the downstream processing by classical DC, indeed Flores-Langarica and colleagues imply the receptor calreticulin in this process suggesting targeting towards a protein degradative pathway. This is counter-intuitive to the concept that classical DC may retain intact antigen via a FcγRIIB and complement-mediated process for subsequent presentation [48] which seems more likely to be a requirement for prion pathogenesis under the current prion hypothesis. Uptake of prion agent by other Fc receptors may mediate intracellular processing, e.g., for presentation on MHC class II molecules. Extreme processing of the prion agent is likely to render it ineffective. Cleavage of the cellular prion protein has been shown to protect against infection [49], whilst cleavage of PrPSc has been shown to modulate prion propagation in a similar fashion [50].
Complement component C1q also regulates dendritic cell development from monocytes via DC-SIGN signaling [51,52]. This induces more tolerogenic DCs and alters their cytokine production, leading to increased Il-10 and reduced Il-12 production and increased phagocytosis of apoptotic cells [53,54]. These data would suggest that C1q deficient mice may also possess a bias in their DC component or functions, as well as a deficiency in immune-complex trapping to FDC, further complicating the interpretation of prion pathogenesis studies performed within them.
The role of complement during prion pathogenesis is further complicated by the observation that the individual complement components mediating interaction with PrPSc appear to differ dependent upon the strain of infectious agent [55]. Cell-autonomous and complement-assisted cell-mediated waves of prion trafficking occurs to lymphoid follicles, the relevance of each transport mechanism to disease pathogenesis remains undetermined [56].
The role of the complement system within the CNS has also been extensively reviewed recently [57,58]. As with most innate immune functions within the CNS a clear neuroprotective/neurodegenerative dichotomy exists within the literature, likely indicative that complement activation may lead to both protective and degenerative effects dependent upon the context, responsive and regulatory mechanisms involved. There is currently little evidence supporting a role for complement in prion pathogenesis within the CNS. Mice lacking C1qa, C2 or C3 revealed no deficit to prion pathogenesis following intracerebral inoculation [44] and mice lacking both complement components C3 and C4 revealed unaltered pathogenesis following aerosol exposure to prions [11].
2.3. Mast Cells
Mast cells have been implicated in prion pathogenesis due to their high expression levels of cellular prion protein (PrP or PrPC) and their ability to traffic to the brain [59]. In fact mast cells are resident, and are also capable of trafficking from the blood to specific regions within the CNS. These different populations of mast cells differentially express the c-kit receptor [60]. Mast cells function to release histamine (via binding of allergens to FcεR1α) and heparin in an early response to infection, and are critical to induce chemotaxis and infiltration of neutrophils and MNPs. Due to the non-inflammatory nature of prion infection there is little evidence to suggest that mast cells undertake this conventional role during peripheral prion pathogenesis. Studies of the activation pathways in mast cells reveal that other factors such as C3a and CCL3 may trigger mast cell degranulation without IgE binding to FcεR1α [61]. This activation pathway is most likely to occur during prion pathogenesis as there is little evidence of the induction of an adaptive immune response and specific anti-prion antibody generation during pathogenesis. The role of immediate local responses to prion infection is in clear need of further investigation to determine the activation effects on mast cells, MNPs and neutrophils amongst other innate immune cell types.
The role of mast cells within the brain is thought to be neuro-modulatory and mast cell trafficking to the brain is linked to steroidal hormones and sexual activity or anxiety behaviors [62]. The presence of mast cells within the brain and their ability to shed expressed PrP upon activation [59] may have implications for prion pathogenesis within the CNS. Shedding of PrPC by mast cells likely occurs via proteolytic or lipolytic cleavage mechanisms removing the glycosylphosphatidylinisotol (GPI) anchor from the protein [59,63]. Activation of mast cells within the CNS may provide copious extracellular PrPC substrate for conversion to the disease-associated isoform late in the disease process, when significant damage has occurred to the CNS already, adding to the exponential accumulation of misfolded protein within the clinical stage of disease. Investigation of GPI-anchorless PrP transgenic mice has revealed that they are capable of forming amyloid in the brain without clinical prion disease symptoms, whilst co-expression of anchorless and native PrPC increased prion pathogenesis [64]. Novel synthetic prion strains have subsequently been generated in the above mentioned co-expressing model [65], suggesting that mast cell involvement during infection may aid in or promote the natural prion strain mutation [66] or prion evolution phenomena [67].
2.4. Mononuclear Phagocytes: Microglia, Macrophages, Monocytes, Dendritic Cells and Langerhans Cells
MNP constitute a system of highly phagocytic cells that have a common origin in the bone marrow and circulate or reside in the body tissues in order to sample their environment via uptake of foreign (and self) material. The development of MNP relies upon expression of the colony stimulating factor 1 receptor (CSF-1R) during their differentiation in order to respond to CSF-1. MNP play a vital role in the bridge between the innate and adaptive immune systems by processing and presenting of antigenic compounds to stimulate specific antibody production. During the initial processing by MNP material may be directly disposed of by degradation via lysosomal or proteasomal pathways. These actions of MNP aid in the development of immunity or tolerance to the vast multitude of foreign material encountered. Numerous (particularly intracellular) pathogens have adapted to abuse the functions of MNP as a vehicle for pathogenesis, allowing for their uptake into MNP and trafficking to lymphoid organs for further spread. It is most likely that the uptake and spread of prions to lymphoid organs occurs using MNP as a ‘Trojan horse’ via a similar mechanism.
The role of MNP in prion pathogenesis have been subject to recent review and are considered diverse [68]. This reflects the wide diversity of MNP and their roles in innate immunity. To simplify this diversity MNP can be broadly categorized into the following: (1), resident cells with degradative functions; (2) resident cells with antigen presenting functions and (3) systemic circulating cells responsive to inflammatory stimuli. At present there is little evidence implicating circulating ‘inflammatory monocyte’ populations in prion pathogenesis due to the non-inflammatory nature of infection.
Regardless of their major functionality all MNP likely use similar surface receptor based pathways and mechanisms to sense their local micro-environment and tailor their responses to pathogens or tissue damage. The exact receptor-mediated mechanism determining the response to prion agents has not been identified or definitively characterized. MNP-mediated uptake of prion agent is enhanced by complement opsonization (see Section 2.1 above). The uptake of prions likely involves complement, lectin or scavenger receptors while there is evidence that Fc [44] (FcγR, RII and RIII deficient mice reveal no deficit following i.c. or i.p. inoculation), or toll-like receptors [69] (at least via the Myd88-dependent pathway) have little role in peripheral pathogenesis under steady state conditions. The downstream processing of the prion agent will likely depend upon the MNP type it has been encountered by.
2.4.1. Degradative MNP
The expression of cellular prion protein in MNP has been associated with phagocytic ability and modulation of inflammatory responses [70,71,72]. Evidence suggests that macrophages (generally identifiable by the markers integrin alpha M, Macrosialin or the F4/80 antigen) degrade the prion agent [73]. The degradative and prion clearance abilities of macrophages appear to be down-regulated when macrophage (Mϕ) activation is stimulated by other danger signal molecules [74]. Again the mechanism of degradation is unknown but represents a critical therapeutic target as it constitutes a natural regulatory mechanism to prion pathogenesis. Stimulating or enhancing this degradative ability may improve peripheral resistance to prion infection. The degradation of agent is countered by the relative replicative ability of the prion agent and its spread through the host. While much has been postulated regarding the prion protein sequence, protein folded conformation and glycosylation in constituting the relative ‘species-barrier’ effect observed relating to limited or lack of cross-species infection ability of specific strains of prion agent (for review see [75]). An alternate hypothesis is to suggest that in prion infection with low or poor replicative ability (i.e., due to the factors mentioned above) the balance is switched in favor of degradation of agent, thereby preventing or dramatically slowing pathogenesis. This may occur both within any given cell (and not exclusively to degradative or phagocytic cell types), in fact it is well known that there are limited in vitro cell infection models in the prion field due to the relevant inability to infect numerous cell types with a variety of prion strains even within the same species [76], and within the complexity of the host innate immune response.
Cellular degradation of PrPSc has been shown to be inhibited by cysteine protease inhibitors [77]. It has also been shown that prions may be taken up and trafficked to the endosomal compartment [78] one possible intracellular site of PrPC to PrPSc conversion [79]. The role of Rab GTPase proteins and their effectors shifting the balance of trafficking away from recycling endosomes and towards late endosomal/lysosomal pathways may play a pivotal role in the cellular decision between propagation and degradation of prions [79]. The cellular ability to uptake and degrade prions appears to be independent of cellular prion protein expression [80,81].
2.4.2. Antigen Presenting Cells (APC)
APC have long been identified as being critical to prion pathogenesis. While evidence exists for both cell-free and cell-mediated transport of prions to lymphoid tissues [56], removal of the cell-mediated trafficking severely hampers prion pathogenesis. The basis of cell-mediated trafficking lies in chemotactic efflux of APC to lymph nodes during their maturation [5,82]. The initial phase of transport results from the linked down-regulation of CCR6 and up-regulation of CCR7 allowing APCs to relocate to lymphoid follicles [83]. Prion infection of ‘plt’ mice (deficient in CCL19/CCL21) revealed delayed pathogenesis following transcutaneous infection attributable to impaired CCR7-mediated chemotaxis of DC [82]. Following oral prion infection altered homeostasis in DC levels has been reported in intestinal Peyer’s patches [84]. Transient depletion of CD11c-expressing cells (a commonly used marker indicative of classical DC) revealed the ability to completely block or severely impair pathogenesis via oral and intraperitoneal routes [85,86]. This depletion strategy was observed to eliminate all MNP types from the intestine, including classical DC and macrophages, suggesting that neither transport nor degradation are actively occurring during depletion [87]. Depletion models of CD11c+ CD8+ (in this case CD8αα) DC subsets restricts intraperitoneal but not oral pathogenesis suggesting that alternative DC subsets may be employed following different infection routes. CD8 knockout mice revealed no alteration of prion pathogenesis, suggesting no direct role for CD8 [88]. This paradigm seems more clearly established in the parenteral ‘skin scarification’ model route of infection. In this model numerous DC and Langerhans cell (LC, expressing the marker Langerin) MNP types are known to interact with the prion agent but the depletion of non-epidermal CD11c+ cells had the biggest impact upon pathogenesis [89]. Extracted cell populations representing classical DC and plasmacytoid DC (pDC) have been shown to be capable of transfer of infection in vivo [90] and in vitro [91] respectively. These findings strongly link these cell types to the retention of intact prion agent and, in the case of classical DC, traffic of the agent in the pre-neuroinvasive stage of prion infection. Resident macrophage cell types within lymphoid organs have so far been shown to have little impact upon disease pathogenesis, indicating that cell free material arriving at the lymphoid tissue is either sequestered to FDC (via complement opsonization) or degraded by resident tingible body macrophages.
2.4.3. MNP in the CNS
Within the CNS the innate immune response is mediated by specialized MNP known as microglia. Microglial development is also dependent upon signaling via the CSF1-R [92], however microglial population of the CNS appears to require both CSF-1R ligands; interleukin-34 (Il-34) [93] and CSF-1 [94]. Microglia activated by amyloidogenic peptides including PrP106-126, also reveal enhanced survival and proliferative responses to CSF-1 [95]. Following peripheral prion infection the microglia show signs of activation after neurons and astrocytes have responded. These findings suggest that microglia do not respond directly to presence of misfolded prion protein per se but may require priming by other CNS cell types. Following priming the microglial cells undergo chemotaxis to the site of insult [96], impairment of this chemotaxis by knockout of CXCR3 revealed altered central prion pathogenesis [97]. Once activated the microglial population expands and has been shown to upregulate various markers including Trem2, SiglecF, CD200R, and Fcγ receptors in a non-classical immune-response [98]. In fact many of the CNS gene expression profiling studies focused on prion infected CNS have repeatedly identified genes strongly associated with MNP activation (Table 1). Together these data suggest that MNPs constitute the most clinically relevant target innate immune cell population both within and without the CNS during prion pathogenesis.

Table 1.
Many of the following genes/proteins have been proven or implicated to have a role in the interaction between prion pathogenesis and the innate immune system and are mentioned in this review.
| Gene name | Gene | Uniprot | Phase a | Ref |
|---|---|---|---|---|
| Allograft inflammatory factor 1 | Aif1 / Iba1 | O70200 | M | [99] |
| B-cell differentiation antigen CD72 | Cd72 / Ly32, Lyb-2 | P21855 | M | [98] |
| Beta-2-microglobulin | B2m | P01887 | M | [99,100] |
| Calreticulin | Calr / CRP55 | P14211 | E | [47] |
| C3a anaphylatoxin chemotactic receptor | C3ar1 | O09047 | M | [101] |
| CAMPATH-1 antigen | Cd52 / Mb7 | Q64389 | E | [99,100,102] |
| C–C chemokine receptor type 5 | Ccr5 / MIP-1αR, CD195 | P51682 | E | [96,103] |
| C–C chemokine receptor type 6 | Ccr6 / CD196 | O54689 | E | [104] |
| C–C chemokine receptor type 7 | Ccr7 / MIP-3βR, CD197 | P47774 | E | [82] |
| C–C motif chemokine 2 | Ccl2 / MCP-1 | P10148 | E | [105,106,107] |
| C–C motif chemokine 3 | Ccl3 / MIP-1α | P10855 | E | [100,105,106] |
| C–C motif chemokine 4 | Ccl4 / MIP-1β | P14097 | E | [106] |
| C–C motif chemokine 5 | Ccl5 / RANTES | P30882 | M | [105] |
| C–C motif chemokine 7 | Ccl7 / MCP-3 | Q03366 | M | [103] |
| C–C motif chemokine 9 | Ccl9 / MRP-2 | P51670 | M | [99,102] |
| C–C motif chemokine 12 | Ccl12 / MCP-5 | Q62401 | M | [99,102] |
| C–C motif chemokine 19 | Ccl19 / ELC | O70460 | E | [82] |
| C–C motif chemokine 20 | Ccl20 / MIP-3α, Exodus-1 | O89093 | E | [104] |
| C–C motif chemokine 21a | Ccl21 / Exodus-2 | P84444 | E | [82] |
| C–C motif chemokine 21b | P86792 | |||
| C–C motif chemokine 21c | P86793 | |||
| CD9 antigen | Cd9 | P40240 | M | [99,108] |
| CD40 ligand | Cd40lg / Gp39, CD154 | P27548 | E | [109,110,111] |
| CD48 antigen | Cd48 / BLAST-1 | P18181 | E | [106] |
| CD209 antigen-like protein A b | Cd209a / DC-SIGN | Q91ZX1 | ||
| Cell surface glycoprotein CD200 receptor 4 | Cd200r4 | Q6XJV4 | M | [98] |
| CMRF35-like molecule 8 | Cd300a / MAIR1 | Q6SJQ0 | M | [98] |
| Complement C1q subcomponent subunit A | C1qa | P98086 | E | [41,44,45,47,100,101,106] |
| Complement C1q subcomponent subunit B | C1qb | P14106 | E | |
| Complement C1q subcomponent subunit C | C1qc | Q02105 | E | |
| Complement C2 | C2 | P21180 | E | [44] |
| Complement C3 | C3 / HSE-MSF | P01027 | M | [44,45,100,101] |
| Complement C4-B | C4B | P01029 | E | [41,99,101,102] |
| Complement C5 | C5 | P06684 | [112] | |
| Complement C7 c | C7 | D3YXF5 | E | [113] |
| Complement component C1q receptor | Cd93 / C1qRp, Ly68 | O89103 | ||
| Complement receptor type 1 | CR1 / CD35 | P17927 | E | [44,114] |
| Complement receptor type 2 | CR2 / CD21 | P19070 | E | [44,114,115,116] |
| C-type lectin domain family 4 member K | Cd207 / Langerin | Q8VBX4 | ||
| C-type lectin domain family 7 member A | Clec7a / Dectin1 | Q6QLQ4 | E | [99,101,102] |
| C-type lectin domain family 11 member A | Clec11a / Scgf | O88200 | L | [108] |
| CX3C chemokine receptor 1 | Cx3cr1 | Q9Z0D9 | E | [106,117] |
| C-X-C motif chemokine 9 | Cxcl9 / MIG, Scyb9 | P18340 | M | [118] |
| C-X-C motif chemokine 10 | Cxcl10 / Crg2, Ifi10, Inp10, Scyb10 | P17515 | E | [100,105,109,113] |
| C-X-C motif chemokine 11 | Cxcl11 / I-TAC, Scyb11 | Q9JHH5 | ||
| C-X-C motif chemokine 13 | Cxcl13 / BLC, Scyb13 | O55038 | E | [109] |
| C-X-C chemokine receptor type 3 | Cxcr3 / Cmkar3, CD183 | O88410 | M | [97] |
| C-X-C chemokine receptor type 4 | Cxcr4 / Cmkar4, Lestr, Sdf1r, CD184 | P70658 | M | [103] |
| C-X-C chemokine receptor type 5 | Cxcr5 / Blr1, Gpcr6, CD185 | Q04683 | L | [109] |
| EGF-like module-containing mucin-like hormone receptor-like 1 | Emr1 / GpF4/80 | Q61549 | E | [119] |
| Eotaxin | Ccl11 / Syca11 | P48298 | ||
| Forkhead box protein P3 | Foxp3 | Q99JB6 | [120] | |
| Formyl peptide receptor-related sequence 1 | Fpr-s1 / Fpr2, Fpr3, Fprl1, Lxa4r | O08790 | [121] | |
| Galectin-3 | Lgals3 / MAC-2 | P16110 | E | [106] |
| Galectin-3-binding protein | Lgals3bp / Cycap, Mama | Q07797 | E | [99,101] |
| Granulins | Grn / PCDGF | P28798 | E | [99,117,122] |
| Granulocyte-macrophage colony-stimulating factor | Csf2 / GM-CSF | P01587 | M | [105] |
| Granzyme B | Gzmb / Ctla1 | P04187 | ||
| Growth-regulated alpha protein | Cxcl1 / Gro, Gro1, Mgsa, Scyb1 | P12850 | E | [105] |
| Guanylate-binding protein 4 | Gbp4 / Gbp3 | Q61107 | M | [99] |
| H-2 class I histocompatibility antigen, D-37 alpha chain | H2-T23 | P06339 | M | [99] |
| H-2 class I histocompatibility antigen, D-D alpha chain | H2-D1 | P01900 | M | [99] |
| H-2 class I histocompatibility antigen, K-B alpha chain, | H2-K1 | Q7TN03 | E | [99] |
| Hematopoietic progenitor cell antigen CD34 | Cd34 | Q64314 | [123] | |
| High affinity immunoglobulin epsilon receptor subunit alpha | Fcer1a / FcεR1α | P20489 | ||
| High affinity immunoglobulin epsilon receptor subunit gamma | Fcer1g / FcεR1γ | P20491 | M | [99,101,102,117,122] |
| High affinity immunoglobulin gamma Fc receptor I | Fcgr1 / FcγRI, CD64 | P26151 | E | [44,98] |
| IgG receptor FcRn large subunit p51 | Fcgrt / FcRn | Q61559 | E | [124] |
| Integrin alpha-4 | Itga4 / CD49d | Q00651 | E | [125] |
| Integrin alpha-X | Itgax / CD11c | Q9QXH4 | E | [9,85,90,100,115,126] |
| Integrin alpha-M | Itgam / CD11b | P05555 | E | [96,100,127] |
| Integrin beta-1 | Itgb1 / VLA-4β, CD29 | P09055 | [128] | |
| Integrin beta-2 | Itgb2 / CD18 | P11835 | E | [101,117] |
| Integrin beta-7 | Itgb7 | P26011 | [125] | |
| Interferon alpha-inducible protein 27-like protein 2A | Ifi27 | Q8R412 | E | [99] |
| Interferon-induced protein with tetratricopeptide repeats 1 | Ifit1 | Q64282 | M | [99] |
| Interferon-induced protein with tetratricopeptide repeats 3 | Ifit3 | Q64345 | L | [99,108,122] |
| Interferon-induced transmembrane protein 3 | Ifitm3 | Q9CQW9 | E | [99,108] |
| Interferon gamma | Ifng / IFNγ | P01580 | M | [105,129] |
| Interferon gamma receptor 1 | Ifngr1 / IFNγR1, CD119 | P15261 | ||
| Interleukin-1 alpha | Il1a / Il1α | P01582 | E | [105,106,108,117] |
| Interleukin-1 beta | Il1b / Il1β | P10749 | E | [105,117,118,129] |
| Interleukin-1 receptor type 1 | Il1ra / IL1Rα, CD121a | P13504 | M | [118,130] |
| Interleukin-2 | Il2 | P04351 | E | |
| Interleukin-2 receptor subunit alpha | Il2ra / Il2Rα, CD25 | P01590 | E | [120] |
| Interleukin-4 | Il4 | P07750 | E | [131] |
| Interleukin-6 | Il6 | P08505 | M | [105,129,132] |
| Interleukin-10 | Il10 | P18893 | E | [130,131] |
| Interleukin-12 subunit alpha | Il12p35 | P43431 | [105,133] | |
| Interleukin-12 subunit beta | IL12p40 | P43432 | E | |
| Interleukin 13 | Il13 | P20109 | M | [105,131] |
| Interleukin 15 | Il15 | P48346 | ||
| Interleukin 18 | Il18 | P70380 | ||
| Interleukin 34 | Il34 | Q8R1R4 | ||
| Killer cell lectin-like receptor subfamily B member 1 | Klrb1 / NK1.1, CD161 | Q0ZUP1 | ||
| Leukocyte-associated immunoglobulin-like receptor 1 | Lair1 / CD305 | Q8BG84 | L | [98] |
| Leukocyte surface antigen CD47 | Cd47 / IAP | Q61735 | L | [108] |
| Leukocyte surface antigen CD53 | Cd53 | Q61451 | M | [99,100] |
| Low affinity immunoglobulin gamma Fc region receptor II | Fcgr2b / FcγRIIB, CD32 | P08101 | M | [44,98,99,101,102,117] |
| Low affinity immunoglobulin gamma Fc region receptor III | Fcgr3 / FcγRIII, CD16 | P08508 | M | [44,98,99,101,102,117] |
| L-selectin | Sell / Ly22, LAM1, LECAM1, CD62L | P18337 | E | [106] |
| Lymphocyte antigen 6C1 | Ly6c1 / Ly-6C | P0CW02 | M | [108,122] |
| Lymphocyte antigen 75 | Ly75 / DEC-205, CD205 | Q60767 | E | [127,134] |
| Lymphocyte antigen 86 | Ly86 / Md1 | O88188 | E | [99,102,106,108,122,135] |
| Lymphotoxin-alpha | Lta / LTα, TNFβ, Tnfsf1 | P09225 | E | [125,136] |
| Lymphotoxin-beta | Ltb / LTβ, Tnfc, Tnfsf3 | P41155 | E | [136] |
| Lysozyme C-2 | Lyz2 / Lyzs | P08905 | M | [99,102,137] |
| Macrophage colony-stimulating factor 1 | Csf1 / MCSF | P07141 | M | |
| Macrophage colony-stimulating factor 1 receptor | Csf1r / c-fms, CD115 | P09581 | M | [117] |
| Macrophage receptor MARCO | Marco | Q60754 | E | [138] |
| Macrophage scavenger receptor types I and II | Msr1 / Scvr, SRA, CD204 | P30204 | E | [138] |
| Macrosialin | Cd68 | P31996 | E | [99,100,101,106,115,127] |
| Mannose-binding protein A | Mbl1 / MBP-A | P39039 | ||
| Mannose-binding protein C | Mbl2 / MBP-C | P41317 | ||
| Mast cell surface glycoprotein Gp49A | Gp49a | Q61450 | M | [98] |
| Mast/stem cell growth factor receptor Kit | Kit / SCFR, c-Kit, CD117 | P05532 | ||
| MicroRNA 146a | miR-146a | E | [139] | |
| Monocyte differentiation antigen CD14 | Cd14 | P10810 | E | [101,106,115] |
| Myeloid cell surface antigen CD33 | Cd33 / Siglec3 | Q63994 | M | [98] |
| Myeloid differentiation primary response protein MyD88 | Myd88 | P22366 | [69] | |
| Perforin | Prf1 / Pfp | P10820 | ||
| Probable C-C chemokine receptor type 3 | Ccr3/ Cmkbr1l2, Cmkbr3, MIP-1αRl2, CD193 | P51678 | M | [103] |
| Prion protein | Prnp / PrP, CD230 | P04925 | E | [140,141] |
| Receptor-transporting protein 4 | Rtp4 / Ifrg28 | Q9ER80 | E | [99] |
| Scavenger receptor cysteine-rich type 1 protein M130 | Cd163 / M130 | Q2VLH6 | E | [113] |
| Sialic acid-binding Ig-like lectin 5 | Siglec5 / SiglecF, CD170 | Q920G3 | M | [98] |
| Sialoadhesin | Siglec1 / Sa, Sn, CD169 | Q62230 | E | [142] |
| SLAM family member 5 | Cd84 / Slamf5 | Q18PI6 | L | [101] |
| Sphingosine 1-phosphate receptor 1 | S1pr1 / Edg1, CD363 | O08530 | E | [143] |
| Stromal cell-derived factor 1 | Cxcl12 / SDF-1 | P40224 | E | [113] |
| T-cell surface glycoprotein CD3 gamma chain | Cd3g / TCRγ | P11942 | M | [116] |
| T-cell surface glycoprotein CD3 delta chain | Cd3d / TCRδ | P04235 | M | [116] |
| T-cell surface glycoprotein CD4 | Cd4 | P06332 | M | [116,120,144] |
| T-cell surface glycoprotein CD8 alpha chain | Cd8a / CD8α | P01731 | E | [9,116,144,145] |
| TGF-beta receptor type-2 | Tgfbr2 / TGFβR2 | Q62312 | M | [130] |
| TNF receptor-associated factor 5 | Traf5 | P70191 | L | [108] |
| Toll-like receptor 2 | Tlr2 / CD282 | Q9QUN7 | M | [101] |
| Transforming growth factor beta-1 | Tgfb1 / TGFβ1 | P04202 | M | [108,130,146,147] |
| Triggering receptor expressed on myeloid cells 2 | Trem2 | Q99NH8 | M | [98,99] |
| Tumor necrosis factor | Tnfa / TNFα | P06804 | E | [106,108,130,131,132] |
| Tumor necrosis factor ligand superfamily member 9 | Tnfsf9 / Cd137l, Cd157l, Ly63l | P41274 | E | |
| Tumor necrosis factor receptor superfamily member 1A | Tnfr1 / CD120a | P25118 | E | [130,148,149] |
| Tumor necrosis factor receptor superfamily member 1B | Tnfr2 / CD120b | P25119 | E | [130] |
| Tumor necrosis factor receptor superfamily member 9 | Tnfrsf9 / Ly63, CD137 | P20334 | E | |
| Tumor necrosis factor ligand superfamily member 11 | Tnfsf11 / RANKL, CD254 | O35235 | E | [29] |
| TYRO protein tyrosine kinase-binding protein | Tyrobp / DAP12, CD300d | O54885 | E | [98,99,101] |
| Tyrosine-protein phosphatase non-receptor type substrate 1 | Sirpa / Sirpα1, CD172a | P97797 | E | [115] |
a Reported involvement phase of genes during prion pathogenesis, occurring (E)arly <50%; (M)id 50%–90% or (L)ate >90% during disease incubation period. Data also extrapolated from [150]; b There are 5 murine homologues (A–E) of human DC-SIGN; c From MGI:88235 unreviewed Uniprot entry.
2.5. Granulocytes: Neutrophils, Basophils and Eosinophils
Gene expression data reveal that PrP expression is generally down-regulated during granulocyte differentiation [151] though some expression is still detectable [152] (see also Figure 2). Neutrophil functions have been shown to be inhibited by both native and scrapie associated prion protein, resulting in failure of neutrophil aggregation and deficits in superoxide radical and beta-glucuronidase export [153]. A 20 amino acid fragment of the prion protein sequence (termed PrP106-126) has been shown to be directly neurotoxic, activate MNPs and act as a chemotactic agonist for the FPRL1 receptor [121]; the relevance of the PrP106-126 fragment to prion pathogenesis is elusive at best. FPRL1 is strongly expressed on granulocytes and MNP cell types and promotes chemotaxis to sites in response to allergic inflammation [154]. Eosinophilic inclusions have been observed in both central and peripheral amyloid deposits, although amyloid deposits themselves are eosinophilic, there is some evidence to suggest eosiniophils are present within or around peripheral amyloid deposits. The basis for this localization appears to lie in FPRL1 chemotaxis.
2.6. Natural Killer Cells and γδ T Cells
Natural killer (NK) and γδ T cells are thought to play little role in the pathogenesis of prion diseases. Both cell types require triggering or activation by danger signals, for NK cell this is usually via cytokines and for γδ T cells little is known about their activating signals. NK cells primarily respond to virally-infected cells and function to destroy these cells via expression of perforin and granzyme. Perforin-knockout mice revealed unaltered prion pathogenesis [88]. NK cells are typically stimulated via interleukins, 2, 12, 15 and 18 and chemokine CCL5 as well as down-regulation of MHC class I molecules following viral infection. The lack of reported NK cell response to prion pathogenesis suggests that prion agent uptake by monocytes may fail to activate NK cells. There are numerous viral mechanisms used to evade NK cell activation including regulating apoptosis, modulating cytokines and chemokines, and compromising DC functions for review see [155,156,157]. Little evidence has been discovered for any of these functions following prion infection apart from the possible induction of apoptotic cell death mechanisms (in neurons). Recently NK/T cells (a subset of T-cells that express both the NK1.1 marker and αβ T cell receptor) in the spleen have been associated with prion infectivity [91]. Investigating the role of NK/T cells in prion pathogenesis is hampered by the fact that though Rag2−/− mice are deficient in NK/T cells they are unsusceptible to prion infection due to their B-cell deficiency and failure to generate mature FDC. Selective reconstitution of the Rag2−/− model for prion pathogenesis studies has not been reported. An increase in γδ T cells in the peripheral blood mononuclear cells (PBMCs) has been reported following scrapie infection in sheep [116].
2.7. Megakaryocytes and Platelets
The megakaryocyte lineage and platelets have been associated with the expression of prion protein [123,158] and MicroRNA miR146a [159]. Following activation of platelets PrPC is released in exosomes [160], similar to the release of exosomal PrPC from macrophages [161]. While not classically considered part of the innate immune system, evidence regarding the expression of TLR2 having a regulatory function has suggested a new role for megakaryocytes in immunity [162]. The over-expression of miR146a, TLR2 and TLR4 has also been reported in microglial cells during scrapie (prion) infection [139]. These data may indicate some common co-expression mechanism of these genes or their possible functional interaction. Regardless of their role in immunity megakaryocytes and platelets constitute a significant portion of the PrP expressing bodies within the blood compartment and as such represent a major vector for prion transmission during blood transfusion [163,164,165,166]. Spread of prion infection between lymphoid organs (i.e., from draining to contralateral non-draining lymph nodes) has been prevented by blocking the egress and thus recirculation of B-cells [143]. The routing of prion pathogenesis has been characterized in precise immunohistological detail and describes neuroinvasion from lymphoid organs via the peripheral nervous system [167,168]. Hematogenous spread from lymphoid organs to the CNS has been proposed as an alternative or complementary pathway to neuroinvasion in natural ruminant prion disease with involvement of the circumventricular organs (CVO) in the CNS [169].
2.8. Prion Protein Expression
Expression of the cellular prion protein (PrPC) by the hematopoietic compartment is not required for prion pathogenesis [170], confirming that the innate immune system function in disease pathogenesis operates via non-PrPC dependent mechanisms. Little is known about the uptake mechanisms of prions and the factors that lead to cell clearance, infection or passivity that may facilitate transport. PrPC is not required for uptake of prions in vitro, even by non-phagocytic cell types such as neurons [171]. There has been much debate regarding which cells of the immune system do or do not express appreciable levels of PrP. It has long been known that PrP is strongly expressed on hematopoietic stem cells within the bone-marrow compartment; specific lineages appear to lose or down-regulate this expression during differentiation [172,173]. Maturation of cells in response to all-trans retinoic acid is one mechanism known to down-regulate PrP expression [151]. In light of the current debate regarding hematopoietic differentiation and retention or loss of PrPC expression we present here data on the expression of the prion protein gene (Prnp) transcripts in various innate immunity relevant cellular compartments (Figure 2). The ability to detect Prnp gene expression and cellular prion protein differ, indeed it appears that the mature protein is often more labile or difficult to detect than its corresponding mRNA message, possibly accounting for some of the reported discrepancies [174,175]. The data we present here clearly depicts altered Prnp expression levels between subcomponents of the hematopoietic system with Mϕ, DC, Microglia, LC and IFN-producing killer DC displaying the highest observable levels of expressed Prnp transcript.
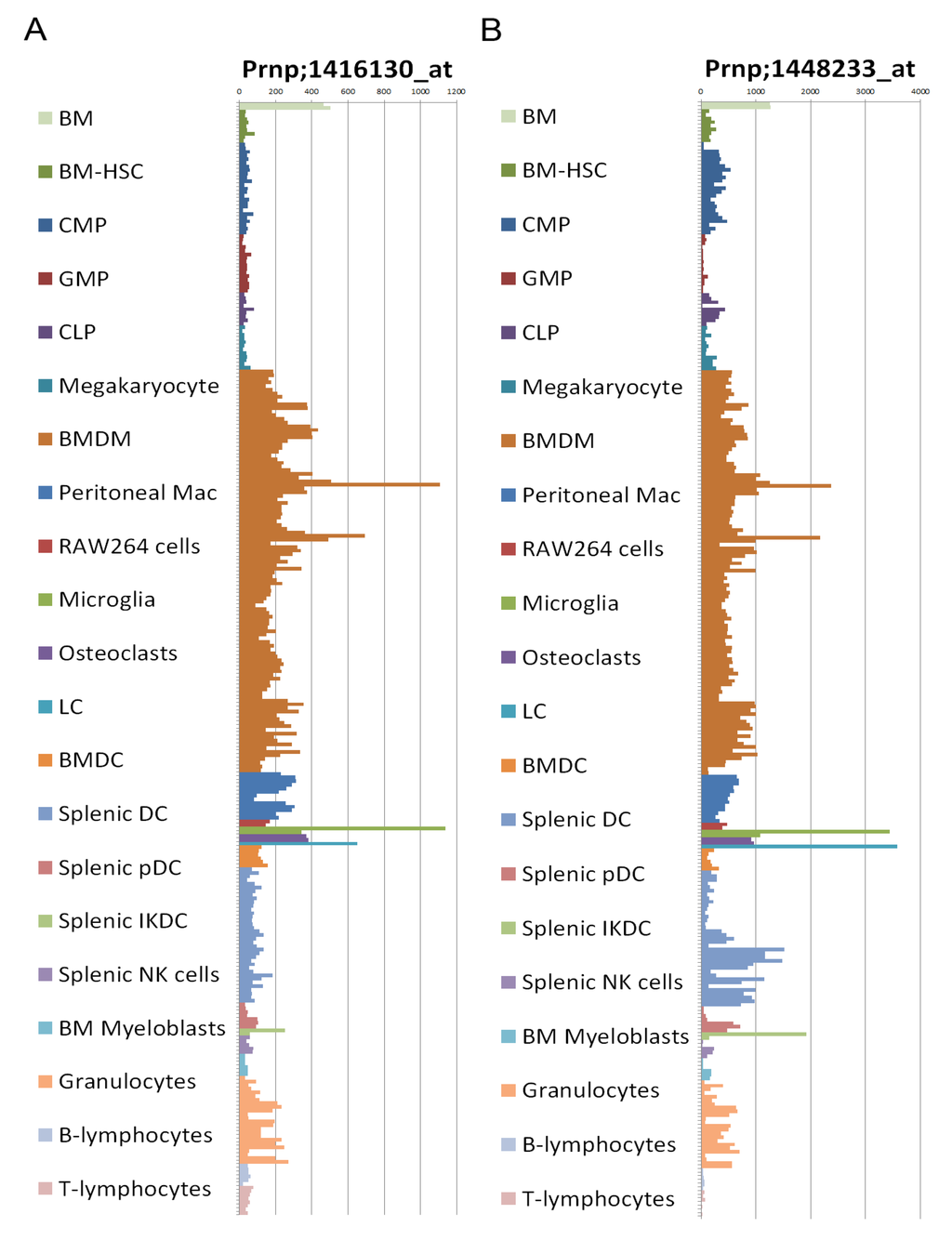
Figure 2.
(a) Prnp expression profiling using Affymetrix GeneChip Mouse Genome 430 2.0 Array probesets 1416130_at and (b) 1448233_at; data from [176]. BM, bone marrow; HSC, hematopoietic stem cells; CMP, common myeloid progenitor; GMP, granulocyte-macrophage progenitor; CLP, common lymphoid progenitor; BMDM, bone marrow-derived macrophage; LC, Langerhans cell; BMDC, bone marrow-derived dendritic cell; DC, dendritic cell; pDC, plasmacytoid dendritic cell; IKDC, interferon-producing killer dendritic cell; NK, natural killer.
2.9. Transgenic Mice Models
The most common mechanism for determining or proving a correlation between components of the innate immune system (be they cells or proteins) and prion pathogenesis is via transgenic mouse models. These models have been used to determine the effect of knockout or overexpression of a particular protein or cell type on prion pathogenesis. The classic experiment revealed that knockout of Prnp resulted in complete resistance to prion infection [140,141]. A plethora of immunity-associated candidate genes have been identified by observational techniques e.g., following gene expression profiling and numerous genes have been screened for a role in prion pathogenesis via knockout transgenic mouse models, e.g., [130] (see also Table 1). The majority of such studies have determined that knockout of an individual component does not prevent prion pathogenesis, for some a slight alteration in pathogenesis was observed and for relatively few a block of pathogenesis was observed and then often only under certain specific conditions. We have performed a pathway analysis of the innate immunity associated genes implicated in prion pathogenesis and determined the major host upstream regulators of prion pathogenesis-associated gene expression (Table 2).

Table 2.
Major upstream regulators of genes implicated in prion pathogenesis (Table 1), as determined by Ingenuity pathway analysis IPA (Ingenuity® Systems, www.ingenuity.com).
| Upstream regulator | Acronym | P-value of overlap | # of genes |
|---|---|---|---|
| Interleukin-4 | Il-4 | 5.85E-68 | 73 |
| Interleukin-12 | IL-12 | 4.89E-64 | 49 |
| Interferon gamma | IFNγ | 1.32E-63 | 80 |
| Interleukin-10 | IL-10 | 3.85E-63 | 56 |
| Interleukin-2 | IL-2 | 1.05E-56 | 58 |
| Tumor necrosis factor | TNF | 2.70E-53 | 80 |
| Interleukin-6 | IL-6 | 9.31E-49 | 57 |
| Colony stimulating factor 2 | CSF2 | 2.85E-46 | 43 |
From these candidates all have previously been implicated with prion pathogenesis, Il-4, Il-6 and Il-12 have been shown not to be required. Il-10 knockout mice revealed major alterations to, but not prevention of, prion pathogenesis. These data reveal the cytokine milieu occurring during prion pathogenesis and may underlie the basis of alternative activation of MNP and lack of inflammatory, or tolerization of, responses during prion infection. These upstream regulators accounted for 118 out of the 144 genes analyzed presented as a wheel network diagram to reveal the overlap between the regulators and target genes (Figure 3), perhaps revealing why knockout of any individual component may have little overall effect upon prion pathogenesis. Many of these genes and their regulators effect MNP differentiation, maturation and homeostasis as well as modulating MNP responses during infection. These findings indicate that prion pathogenesis is influenced by the steady-state, activation and response of the innate immune system.
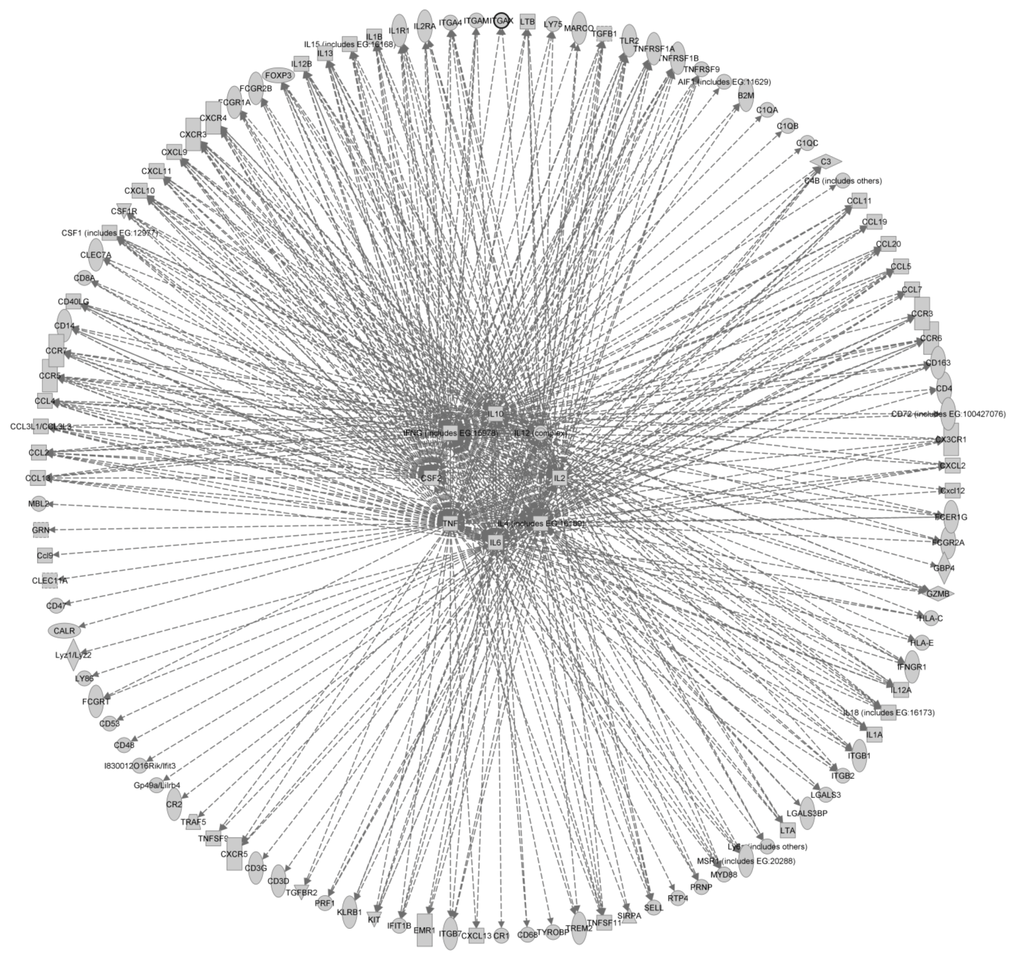
Figure 3.
Wheel network diagram showing the overlap of the major upstream regulators of genes implicated in prion pathogenesis. The network was generated through the use of IPA (Ingenuity® Systems, www.ingenuity.com).
3. Summary and Conclusions
In summary the innate immune system has many and varied roles in the response to prion pathogenesis, providing both the means to facilitate spread of infection and natural mechanisms to combat infection. The activation (or alternative activation) of mononuclear phagocyte cells appears critical to both peripheral and central prion pathogenesis through as yet unidentified receptors and signaling pathways. Investigation of the expression and function or cellular prion protein has clearly identified widespread expression throughout cell types of the innate immune system and has also suggested possible immune-system specific functions of PrP separate from its possible roles within the CNS.
Acknowledgments
This work was supported by Project (BB/F019726-1) and Institute Strategic Grant funding from the BBSRC. The authors would like to thank Paula L. Stewart, A. Richard Alejo-Blanco and Thomas Wishart for helpful advice and discussion.
Conflict of Interest
The authors declare no conflict of interest.
References and Notes
- Prusiner, S.B. Novel proteinaceous infectious particles cause scrapie. Science 1982, 216, 136–144. [Google Scholar]
- Fraser, H.; Dickinson, A.G. Pathogenesis of Scrapie in the Mouse: The Role of the Spleen. Nature 1970, 226, 462–463. [Google Scholar]
- Kimberlin, R.H.; Walker, C.A. The role of the spleen in the neuroinvasion of scrapie in mice. Virus Res. 1989, 12, 201–211. [Google Scholar] [CrossRef]
- Glaysher, B.R.; Mabbott, N.A. Role of the GALT in Scrapie Agent Neuroinvasion from the Intestine. J. Immunol. 2007, 178, 3757–3766. [Google Scholar]
- Glaysher, B.R.; Mabbott, N.A. Role of the draining lymph node in scrapie agent transmission from the skin. Immunol. Lett. 2007, 109, 64–71. [Google Scholar] [CrossRef]
- McCulloch, L.; Brown, K.L.; Bradford, B.M.; Hopkins, J.; Bailey, M.; Rajewsky, K.; Manson, J.C.; Mabbott, N.A. Follicular Dendritic Cell-Specific Prion Protein (PrPc) Expression Alone Is Sufficient to Sustain Prion Infection in the Spleen. PLoS Pathog. 2011, 7, e1002402. [Google Scholar]
- Brown, K.L.; Stewart, K.; Ritchie, D.L.; Mabbott, N.A.; Williams, A.; Fraser, H.; Morrison, W.I.; Bruce, M.E. Scrapie replication in lymphoid tissues depends on prion protein-expressing follicular dendritic cells. Nat. Med. 1999, 5, 1308–1312. [Google Scholar] [CrossRef]
- Kimberlin, R.H.; Walker, C.A. Pathogenesis of scrapie in mice after intragastric infection. Virus Res. 1989, 12, 213–220. [Google Scholar]
- Sethi, S.; Kerksiek, K.M.; Brocker, T.; Kretzschmar, H. Role of the CD8+ Dendritic Cell Subset in Transmission of Prions. J. Virol. 2007, 81, 4877–4880. [Google Scholar]
- Bartz, J.C.; Kincaid, A.E.; Bessen, R.A. Rapid prion neuroinvasion following tongue infection. J. Virol. 2003, 77, 583–591. [Google Scholar]
- Haybaeck, J.; Heikenwalder, M.; Klevenz, B.; Schwarz, P.; Margalith, I.; Bridel, C.; Mertz, K.; Zirdum, E.; Petsch, B.; Fuchs, T.J.; et al. Aerosols Transmit Prions to Immunocompetent and Immunodeficient Mice. PLoS Pathog. 2011, 7, e1001257. [Google Scholar] [CrossRef]
- Kimberlin, R.H.; Hall, S.M.; Walker, C.A. Pathogenesis of mouse scrapie: Evidence for direct neural spread of infection to the CNS after injection of sciatic nerve. J. Neurol. Sci. 1983, 61, 315–325. [Google Scholar] [CrossRef]
- Kimberlin, R.H.; Cole, S.; Walker, C.A. Pathogenesis of scrapie is faster when infection is intraspinal instead of intracerebral. Microb. Pathog. 1987, 2, 405–415. [Google Scholar]
- González, L.; Chianini, F.; Martin, S.; Sisó, S.; Gibbard, L.; Reid, H.W.; Jeffrey, M. Comparative titration of experimental ovine BSE infectivity in sheep and mice. J. Gen. Virol. 2007, 88, 714–717. [Google Scholar] [CrossRef]
- Fraser, H.; Brown, K.L.; Stewart, K.; McConnell, I.; McBride, P.; Williams, A. Replication of scrapie in spleens of SCID mice follows reconstitution with wild-type mouse bone marrow. J. Gen. Virol. 1996, 77, 1935–1940. [Google Scholar]
- Friedman-Levi, Y.; Hoftberger, R.; Budka, H.; Mayer-Sonnenfeld, T.; Abramsky, O.; Ovadia, H.; Gabizon, R. Targeting of prion-infected lymphoid cells to the central nervous system accelerates prion infection. J. Neuroinflammation 2012, 9. [Google Scholar] [CrossRef]
- Mabbott, N.A.; Kenneth Baillie, J.; Kobayashi, A.; Donaldson, D.S.; Ohmori, H.; Yoon, S.-O.; Freedman, A.S.; Freeman, T.C.; Summers, K.M. Expression of mesenchyme-specific gene signatures by follicular dendritic cells: Insights from the meta-analysis of microarray data from multiple mouse cell populations. Immunology 2011, 133, 482–498. [Google Scholar] [CrossRef]
- Fu, Y.-X.; Molina, H.; Matsumoto, M.; Huang, G.; Min, J.; Chaplin, D.D. Lymphotoxin-α (LTα) Supports Development of Splenic Follicular Structure That Is Required for IgG Responses. J. Exp. Med. 1997, 185, 2111–2120. [Google Scholar]
- Ansel, K.M.; Ngo, V.N.; Hyman, P.L.; Luther, S.A.; Forster, R.; Sedgwick, J.D.; Browning, J.L.; Lipp, M.; Cyster, J.G. A chemokine-driven positive feedback loop organizes lymphoid follicles. Nature 2000, 406, 309–314. [Google Scholar]
- Glatzel, M.; Heppner, F.L.; Albers, K.M.; Aguzzi, A. Sympathetic innervation of lymphoreticular organs is rate limiting for prion neuroinvasion. Neuron 2001, 31, 25–34. [Google Scholar] [CrossRef]
- Akira, S.; Takeda, K. Toll-like receptor signalling. Nat. Rev. Immunol. 2004, 4, 499–511. [Google Scholar]
- Geijtenbeek, T.B.H.; Gringhuis, S.I. Signalling through C-type lectin receptors: Shaping immune responses. Nat. Rev. Immunol. 2009, 9, 465–479. [Google Scholar] [CrossRef]
- Fritz, J.H.; Ferrero, R.L.; Philpott, D.J.; Girardin, S.E. Nod-like proteins in immunity, inflammation and disease. Nat. Immunol. 2006, 7, 1250–1257. [Google Scholar]
- Takeuchi, O.; Akira, S. Innate immunity to virus infection. Immunol. Rev. 2009, 227, 75–86. [Google Scholar] [CrossRef]
- Taylor, D.M.; McConnell, I.; Fraser, H. Scrapie infection can be established readily through skin scarification in immunocompetent but not immunodeficient mice. J. Gen. Virol. 1996, 77, 1595–1599. [Google Scholar] [CrossRef]
- Sigurdson, C.J.; Heikenwalder, M.; Manco, G.; Barthel, M.; Schwarz, P.; Stecher, B.; Krautler, N.J.; Hardt, W.-D.; Seifert, B.; MacPherson, A.J.S.; et al. Bacterial Colitis Increases Susceptibility to Oral Prion Disease. J. Infect. Dis. 2009, 199, 243–252. [Google Scholar] [CrossRef]
- Bessen, R.A.; Wilham, J.M.; Lowe, D.; Watschke, C.P.; Shearin, H.; Martinka, S.; Caughey, B.; Wiley, J.A. Accelerated shedding of prions following damage to the olfactory epithelium. J. Virol 2012, 86, 1777–1788. [Google Scholar]
- Foster, N.; Macpherson, G.G. Murine Cecal Patch M Cells Transport Infectious Prions in Vivo. J. Infect. Dis. 2010, 202, 1916–1919. [Google Scholar] [CrossRef]
- Donaldson, D.S.; Kobayashi, A.; Ohno, H.; Yagita, H.; Williams, I.R.; Mabbott, N.A. M cell-depletion blocks oral prion disease pathogenesis. Mucosal Immunol. 2012, 5, 216–225. [Google Scholar] [CrossRef]
- Hsieh, E.H.; Fernandez, X.; Wang, J.; Hamer, M.; Calvillo, S.; Croft, M.; Kwon, B.S.; Lo, D.D. CD137 is Required for M Cell Functional Maturation but not Lineage Commitment. Am. J. Pathol. 2010, 177, 666–676. [Google Scholar] [CrossRef]
- Lugering, A.; Floer, M.; Westphal, S.; Maaser, C.; Spahn, T.W.; Schmidt, M.A.; Domschke, W.; Williams, I.R.; Kucharzik, T. Absence of CCR6 Inhibits CD4+ Regulatory T-Cell Development and M-Cell Formation inside Peyer’s Patches. Am. J. Pathol. 2005, 166, 1647–1654. [Google Scholar] [CrossRef]
- Westphal, S.; Lügering, A.; von Wedel, J.; von Eiff, C.; Maaser, C.; Spahn, T.; Heusipp, G.; Schmidt, M.A.; Herbst, H.; Williams, I.R.; et al. Resistance of Chemokine Receptor 6-Deficient Mice to Yersinia Enterocolitica Infection: Evidence of Defective M-Cell Formation in Vivo. Am. J. Pathol. 2008, 172, 671–680. [Google Scholar] [CrossRef]
- Nakato, G.; Hase, K.; Suzuki, M.; Kimura, M.; Ato, M.; Hanazato, M.; Tobiume, M.; Horiuchi, M.; Atarashi, R.; Nishida, N.; et al. Cutting Edge: Brucella abortus Exploits a Cellular Prion Protein on Intestinal M Cells as an Invasive Receptor. J. Immunol. 2012, 189, 1540–1544. [Google Scholar] [CrossRef]
- Kujala, P.; Raymond, C.R.; Romeijn, M.; Godsave, S.F.; van Kasteren, S.I.; Wille, H.; Prusiner, S.B.; Mabbott, N.A.; Peters, P.J. Prion Uptake in the Gut: Identification of the First Uptake and Replication Sites. PLoS Pathog. 2011, 7, e1002449. [Google Scholar]
- Rescigno, M.; Urbano, M.; Valzasina, B.; Francolini, M.; Rotta, G.; Bonasio, R.; Granucci, F.; Kraehenbuhl, J.-P.; Ricciardi-Castagnoli, P. Dendritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat. Immunol. 2001, 2, 361–367. [Google Scholar]
- Chieppa, M.; Rescigno, M.; Huang, A.Y.C.; Germain, R.N. Dynamic imaging of dendritic cell extension into the small bowel lumen in response to epithelial cell TLR engagement. J. Exp. Med. 2006, 203, 2841–2852. [Google Scholar] [CrossRef]
- Prinz, M.; Heikenwalder, M.; Junt, T.; Schwarz, P.; Glatzel, M.; Heppner, F.L.; Fu, Y.-X.; Lipp, M.; Aguzzi, A. Positioning of follicular dendritic cells within the spleen controls prion neuroinvasion. Nature 2003, 425, 957–962. [Google Scholar]
- Colten, H.R.; Ooi, Y.M.; Edelson, P.J. Synthesis and Secretion of Complement Proteins by Macrophages. Ann. NY Acad. Sci. 1979, 332, 482–490. [Google Scholar]
- Colten, H.R.; Perlmutter, R.C.; Schlessinger, D.H.; Cole, F.S. Regulation of Complement Protein Biosynthesis in Mononuclear Phagocytes; John Wiley & Sons, Ltd.: Chichester, UK, 1986; pp. 141–154. [Google Scholar]
- Schwaeble, W.; Schäfer, M.K.; Petry, F.; Fink, T.; Knebel, D.; Weihe, E.; Loos, M. Follicular dendritic cells, interdigitating cells, and cells of the monocyte-macrophage lineage are the C1q-producing sources in the spleen. Identification of specific cell types by in situ hybridization and immunohistochemical analysis. J. Immunol. 1995, 155, 4971–4978. [Google Scholar]
- Mitchell, D.A.; Kirby, L.; Paulin, S.M.; Villiers, C.L.; Sim, R.B. Prion protein activates and fixes complement directly via the classical pathway: Implications for the mechanism of scrapie agent propagation in lymphoid tissue. Mol. Immunol. 2007, 44, 2997–3004. [Google Scholar]
- Blanquet-Grossard, F.; Thielens, N.M.; Vendrely, C.; Jamin, M.; Arlaud, G.J. Complement Protein C1q Recognizes a Conformationally Modified Form of the Prion Protein. Biochemistry 2005, 44, 4349–4356. [Google Scholar]
- Mabbott, N.A. The complement system in prion diseases. Curr. Opin. Immunol. 2004, 16, 587–593. [Google Scholar]
- Klein, M.A.; Kaeser, P.S.; Schwarz, P.; Weyd, H.; Xenarios, I.; Zinkernagel, R.M.; Carroll, M.C.; Verbeek, J.S.; Botto, M.; Walport, M.J.; et al. Complement facilitates early prion pathogenesis. Nat. Med. 2001, 7, 488–492. [Google Scholar]
- Mabbott, N.A.; Bruce, M.E.; Botto, M.; Walport, M.J.; Pepys, M.B. Temporary depletion of complement component C3 or genetic deficiency of C1q significantly delays onset of scrapie. Nat. Med. 2001, 7, 485–487. [Google Scholar]
- Hartung, H.P.; Hadding, U. Synthesis of complement by macrophages and modulation of their functions through complement activation. Springer Semin. Immunopathol. 1983, 6, 283–326. [Google Scholar] [CrossRef]
- Flores-Langarica, A.; Sebti, Y.; Mitchell, D.A.; Sim, R.B.; MacPherson, G.G. Scrapie Pathogenesis: The Role of Complement C1q in Scrapie Agent Uptake by Conventional Dendritic Cells. J. Immunol. 2009, 182, 1305–1313. [Google Scholar]
- Bergtold, A.; Desai, D.D.; Gavhane, A.; Clynes, R. Cell Surface Recycling of Internalized Antigen Permits Dendritic Cell Priming of B Cells. Immunity 2005, 23, 503–514. [Google Scholar]
- Lewis, V.; Hill, A.F.; Haigh, C.L.; Klug, G.M.; Masters, C.L.; Lawson, V.A.; Collins, S.J. Increased proportions of C1 truncated prion protein protect against cellular M1000 prion infection. J. Neuropathol. Exp. Neurol. 2009, 68, 1125–1135. [Google Scholar] [CrossRef]
- Yadavalli, R.; Guttmann, R.P.; Seward, T.; Centers, A.P.; Williamson, R.A.; Telling, G.C. Calpain-dependent Endoproteolytic Cleavage of PrPSc Modulates Scrapie Prion Propagation. J. Biol. Chem. 2004, 279, 21948–21956. [Google Scholar]
- Hosszu, K.K.; Santiago-Schwarz, F.; Peerschke, E.I.B.; Ghebrehiwet, B. Evidence that a C1q/C1qR system regulates monocyte-derived dendritic cell differentiation at the interface of innate and acquired immunity. Innate Immun. 2010, 16, 115–127. [Google Scholar]
- Hosszu, K.K.; Valentino, A.; Vinayagasundaram, U.; Vinayagasundaram, R.; Joyce, M.G.; Ji, Y.; Peerschke, E.I.B.; Ghebrehiwet, B. DC-SIGN, C1q, and gC1qR form a trimolecular receptor complex on the surface of monocyte-derived immature dendritic cells. Blood 2012, 120, 1228–1236. [Google Scholar] [CrossRef]
- Teh, B.K.; Yeo, J.G.; Chern, L.M.; Lu, J. C1q regulation of dendritic cell development from monocytes with distinct cytokine production and T cell stimulation. Mol. Immunol. 2011, 48, 1128–1138. [Google Scholar]
- vajger, U.; Obermajer, N.; Anderluh, M.; Kos, J.; Jeras, M. DC-SIGN ligation greatly affects dendritic cell differentiation from monocytes compromising their normal function. J. Leukoc. Biol. 2011, 89, 893–905. [Google Scholar] [CrossRef]
- Hasebe, R.; Raymond, G.J.; Horiuchi, M.; Caughey, B. Reaction of complement factors varies with prion strains in vitro and in vivo. Virology 2012, 423, 205–213. [Google Scholar] [CrossRef]
- Michel, B.; Meyerett-Reid, C.; Johnson, T.; Ferguson, A.; Wyckoff, C.; Pulford, B.; Bender, H.; Avery, A.; Telling, G.; Dow, S.; et al. Incunabular Immunological Events in Prion Trafficking. Sci. Rep. 2012, 2. [Google Scholar] [CrossRef]
- Yanamadala, V.; Friedlander, R.M. Complement in neuroprotection and neurodegeneration. Trends Mol. Med. 2010, 16, 69–76. [Google Scholar]
- Veerhuis, R.; Nielsen, H.M.; Tenner, A.J. Complement in the brain. Mol. Immunol. 2011, 48, 1592–1603. [Google Scholar]
- Haddon, D.J.; Hughes, M.R.; Antignano, F.; Westaway, D.; Cashman, N.R.; McNagny, K.M. Prion Protein Expression and Release by Mast Cells After Activation. J. Infect. Dis. 2009, 200, 827–831. [Google Scholar] [CrossRef]
- Shanas, U.; Bhasin, R.; Sutherland, A.K.; Silverman, A.-J.; Silver, R. Brain mast cells lack the c-kit receptor: Immunocytochemical evidence. J. Neuroimmunol. 1998, 90, 207–211. [Google Scholar]
- Gilfillan, A.M.; Tkaczyk, C. Integrated signalling pathways for mast-cell activation. Nat. Rev. Immunol. 2006, 6, 218–230. [Google Scholar] [CrossRef]
- Silver, R.; Silverman, A.-J.; Vitković, L.; Lederhendler, I.I. Mast cells in the brain: Evidence and functional significance. Trends Neurosci. 1996, 19, 25–31. [Google Scholar]
- Parkin, E.T.; Watt, N.T.; Turner, A.J.; Hooper, N.M. Dual Mechanisms for Shedding of the Cellular Prion Protein. J. Biol. Chem. 2004, 279, 11170–11178. [Google Scholar]
- Chesebro, B.; Trifilo, M.; Race, R.; Meade-White, K.; Teng, C.; LaCasse, R.; Raymond, L.; Favara, C.; Baron, G.; Priola, S.; et al. Anchorless Prion Protein Results in Infectious Amyloid Disease without Clinical Scrapie. Science 2005, 308, 1435–1439. [Google Scholar]
- Raymond, G.J.; Race, B.; Hollister, J.R.; Offerdahl, D.K.; Moore, R.A.; Kodali, R.; Raymond, L.D.; Hughson, A.G.; Rosenke, R.; Long, D.; et al. Isolation of Novel Synthetic Prion Strains by Amplification in Transgenic Mice Coexpressing Wild-Type and Anchorless Prion Proteins. J. Virol. 2012, 86, 11763–11778. [Google Scholar]
- Bruce, M.E. Scrapie strain variation and mutation. Br. Med. Bull. 1993, 49, 822–838. [Google Scholar]
- Weissmann, C. Mutation and Selection of Prions. PLoS Pathog. 2012, 8, e1002582. [Google Scholar] [CrossRef]
- Wathne, G.J.; Mabbott, N.A. The diverse roles of mononuclear phagocytes in prion disease pathogenesis. Prion 2012, 6, 124–133. [Google Scholar] [CrossRef]
- Prinz, M.; Heikenwalder, M.; Schwarz, P.; Takeda, K.; Akira, S.; Aguzzi, A. Prion pathogenesis in the absence of Toll-like receptor signalling. EMBO Rep. 2003, 4, 195–199. [Google Scholar]
- de Almeida, C.J.G.; Chiarini, L.B.; da Silva, J.P.; e Silva, P.M.R.; Martins, M.A.; Linden, R. The cellular prion protein modulates phagocytosis and inflammatory response. J. Leukoc. Biol. 2005, 77, 238–246. [Google Scholar]
- Uraki, R.; Sakudo, A.; Ando, S.; Kitani, H.; Onodera, T. Enhancement of phagocytotic activity by prion protein in PrP-deficient macrophage cells. Int. J. Mol. Med. 2010, 26, 527–532. [Google Scholar] [Green Version]
- Nitta, K.; Sakudo, A.; Masuyama, J.; Xue, G.; Sugiura, K.; Onodera, T. Role of Cellular Prion Proteins in the Function of Macrophages and Dendritic Cells. Protein Pept. Lett. 2009, 16, 239–246. [Google Scholar] [CrossRef]
- Sassa, Y.; Inoshima, Y.; Ishiguro, N. Bovine macrophage degradation of scrapie and BSE PrPSc. Vet. Immunol. Immunopathol. 2010, 133, 33–39. [Google Scholar]
- Gilch, S.; Schmitz, F.; Aguib, Y.; Kehler, C.; Bülow, S.; Bauer, S.; Kremmer, E.; Schätzl, H.M. CpG and LPS can interfere negatively with prion clearance in macrophage and microglial cells. FEBS J. 2007, 274, 5834–5844. [Google Scholar]
- Moore, R.A.; Vorberg, I.; Priola, S.A. Species barriers in prion diseases—Brief review. In Infectious Diseases from Nature: Mechanisms of Viral Emergence and Persistence; Peters, C.J., Calisher, C.H., Eds.; Springer: Vienna, Austria, 2005; pp. 187–202. [Google Scholar]
- Neale, M.H.; Mountjoy, S.J.; Edwards, J.C.; Vilette, D.; Laude, H.; Windl, O.; Saunders, G.C. Infection of Cell Lines with Experimental and Natural Ovine Scrapie Agents. J. Virol. 2010, 84, 2444–2452. [Google Scholar] [CrossRef]
- Luhr, K.M.; Nordstrom, E.K.; Low, P.; Ljunggren, H.-G.; Taraboulos, A.; Kristensson, K. Scrapie Protein Degradation by Cysteine Proteases in CD11c+ Dendritic Cells and GT1-1 Neuronal Cells. J. Virol. 2004, 78, 4776–4782. [Google Scholar]
- Peters, P.J.; Mironov, A.; Peretz, D.; van Donselaar, E.; Leclerc, E.; Erpel, S.; DeArmond, S.J.; Burton, D.R.; Williamson, R.A.; Vey, M.; et al. Trafficking of prion proteins through a caveolae-mediated endosomal pathway. J. Cell Biol. 2003, 162, 703–717. [Google Scholar] [CrossRef]
- Marijanovic, Z.; Caputo, A.; Campana, V.; Zurzolo, C. Identification of an Intracellular Site of Prion Conversion. PLoS Pathog. 2009, 5, e1000426. [Google Scholar]
- Rybner-Barnier, C.; Jacquemot, C.; Cuche, C.; Doré, G.; Majlessi, L.; Gabellec, M.-M.; Moris, A.; Schwartz, O.; Di Santo, J.; Cumano, A.; et al. Processing of the Bovine Spongiform Encephalopathy-Specific Prion Protein by Dendritic Cells. J. Virol. 2006, 80, 4656–4663. [Google Scholar]
- Paquet, S.; Daude, N.; Courageot, M.-P.; Chapuis, J.; Laude, H.; Vilette, D. PrPc Does Not Mediate Internalization of PrPSc but is Required at an Early Stage for De Novo Prion Infection of Rov Cells. J. Virol. 2007, 81, 10786–10791. [Google Scholar]
- Levavasseur, E.; Metharom, P.; Dorban, G.; Nakano, H.; Kakiuchi, T.; Carnaud, C.; Sarradin, P.; Aucouturier, P. Experimental scrapie in ‘plt’ mice: An assessment of the role of dendritic-cell migration in the pathogenesis of prion diseases. J. Gen. Virol. 2007, 88, 2353–2360. [Google Scholar]
- Dieu, M.-C.; Vanbervliet, B.; Vicari, A.; Bridon, J.-M.; Oldham, E.; Ait-Yahia, S.; Briere, F.; Zlotnik, A.; Lebecque, S.; Caux, C. Selective Recruitment of Immature and Mature Dendritic Cells by Distinct Chemokines Expressed in Different Anatomic Sites. J. Exp. Med. 1998, 188, 373–386. [Google Scholar]
- Dorban, G.; Defaweux, V.; Levavasseur, E.; Demonceau, C.; Thellin, O.; Flandroy, S.; Piret, J.; Falisse, N.; Heinen, E.; Antoine, N. Oral scrapie infection modifies the homeostasis of Peyer’s patches’ dendritic cells. Histochem. Cell Biol. 2007, 128, 243–251. [Google Scholar] [CrossRef]
- Raymond, C.R.; Aucouturier, P.; Mabbott, N.A. In vivo Depletion of CD11c+ Cells Impairs Scrapie Agent Neuroinvasion from the Intestine. J. Immunol. 2007, 179, 7758–7766. [Google Scholar]
- Cordier-Dirikoc, S.; Chabry, J. Temporary Depletion of CD11c+ Dendritic Cells Delays Lymphoinvasion after Intraperitonal Scrapie Infection. J. Virol. 2008, 82, 8933–8936. [Google Scholar]
- Bradford, B.M.; Sester, D.P.; Hume, D.A.; Mabbott, N.A. Defining the anatomical localisation of subsets of the murine mononuclear phagocyte system using integrin alpha X (Itgax, CD11c) and colony stimulating factor 1 receptor (Csf1r, CD115) expression fails to discriminate dendritic cells from macrophages. Immunobiology 2011, 216, 1228–1237. [Google Scholar] [CrossRef]
- Klein, M.A.; Frigg, R.; Flechsig, E.; Raeber, A.J.; Kalinke, U.; Bluethmann, H.; Bootz, F.; Suter, M.; Zinkernagel, R.M.; Aguzzi, A. A crucial role for B cells in neuroinvasive scrapie. Nature 1997, 390, 687–690. [Google Scholar]
- Wathne, G.J.; Kissenpfennig, A.; Malissen, B.; Zurzolo, C.; Mabbott, N.A. Determining the role of mononuclear phagocytes in prion neuroinvasion from the skin. J. Leukoc. Biol. 2012, 91, 817–828. [Google Scholar]
- Aucouturier, P.; Geissmann, F.; Damotte, D.; Saborio, G.P.; Meeker, H.C.; Kascsak, R.; Kascsak, R.; Carp, R.I.; Wisniewski, T. Infected splenic dendritic cells are sufficient for prion transmission to the CNS in mouse scrapie. J. Clin. Invest. 2001, 108, 703–708. [Google Scholar] [Green Version]
- Castro-Seoane, R.; Hummerich, H.; Sweeting, T.; Tattum, M.H.; Linehan, J.M.; Fernandez de Marco, M.; Brandner, S.; Collinge, J.; Klöhn, P.-C. Plasmacytoid Dendritic Cells Sequester High Prion Titres at Early Stages of Prion Infection. PLoS Pathog. 2012, 8, e1002538. [Google Scholar] [CrossRef]
- Erblich, B.; Zhu, L.; Etgen, A.M.; Dobrenis, K.; Pollard, J.W. Absence of Colony Stimulation Factor-1 Receptor Results in Loss of Microglia, Disrupted Brain Development and Olfactory Deficits. PLoS One 2011, 6, e26317. [Google Scholar]
- Wang, Y.; Szretter, K.J.; Vermi, W.; Gilfillan, S.; Rossini, C.; Cella, M.; Barrow, A.D.; Diamond, M.S.; Colonna, M. IL-34 is a tissue-restricted ligand of CSF1R required for the development of Langerhans cells and microglia. Nat. Immunol. 2012, 13, 753–760. [Google Scholar]
- Kondo, Y.; Duncan, I.D. Selective reduction in microglia density and function in the white matter of colony-stimulating factor-1–deficient mice. J. Neurosci. Res. 2009, 87, 2686–2695. [Google Scholar] [CrossRef]
- Hamilton, J.A.; Whitty, G.; White, A.R.; Jobling, M.F.; Thompson, A.; Barrow, C.J.; Cappai, R.; Beyreuther, K.; Masters, C.L. Alzheimer’s disease amyloid beta and prion protein amyloidogenic peptides promote macrophage survival, DNA synthesis and enhanced proliferative response to CSF-1 (M-CSF). Brain Res. 2002, 940, 49–54. [Google Scholar]
- Marella, M.; Chabry, J. Neurons and Astrocytes Respond to Prion Infection by Inducing Microglia Recruitment. J. Neurosci. 2004, 24, 620–627. [Google Scholar]
- Riemer, C.; Schultz, J.; Burwinkel, M.; Schwarz, A.; Mok, S.W.F.; Gultner, S.; Bamme, T.; Norley, S.; van Landeghem, F.; Lu, B.; et al. Accelerated Prion Replication in, but Prolonged Survival Times of, Prion-Infected CXCR3−/− Mice. J. Virol. 2008, 82, 12464–12471. [Google Scholar]
- Lunnon, K.; Teeling, J.L.; Tutt, A.L.; Cragg, M.S.; Glennie, M.J.; Perry, V.H. Systemic Inflammation Modulates Fc Receptor Expression on Microglia during Chronic Neurodegeneration. J. Immunol. 2011, 186, 7215–7224. [Google Scholar]
- Kim, H.O.; Snyder, G.P.; Blazey, T.M.; Race, R.E.; Chesebro, B.; Skinner, P.J. Prion disease induced alterations in gene expression in spleen and brain prior to clinical symptoms. Adv. Appl. Bioinform. Chem. 2008, 1, 29–50. [Google Scholar]
- Riemer, C.; Neidhold, S.; Burwinkel, M.; Schwarz, A.; Schultz, J.; Krätzschmar, J.; Mönning, U.; Baier, M. Gene expression profiling of scrapie-infected brain tissue. Biochem. Biophys. Res. Commun. 2004, 323, 556–564. [Google Scholar]
- Hwang, D.; Lee, I.Y.; Yoo, H.; Gehlenborg, N.; Cho, J.-H.; Petritis, B.; Baxter, D.; Pitstick, R.; Young, R.; Spicer, D.; et al. A systems approach to prion disease. Mol. Syst. Biol. 2009, 5. [Google Scholar] [CrossRef]
- Xiang, W.; Windl, O.; Wunsch, G.; Dugas, M.; Kohlmann, A.; Dierkes, N.; Westner, I.M.; Kretzschmar, H.A. Identification of Differentially Expressed Genes in Scrapie-Infected Mouse Brains by Using Global Gene Expression Technology. J. Virol. 2004, 78, 11051–11060. [Google Scholar]
- Song, C.-H.; Honmou, O.; Furuoka, H.; Horiuchi, M. Identification of chemoattractive factors involved in the migration of bone marrow-derived mesenchymal stem cells to brain lesions caused by prion. J. Virol. 2011, 85, 11069–11078. [Google Scholar] [CrossRef]
- Heppner, F.L.; Christ, A.D.; Klein, M.A.; Prinz, M.; Fried, M.; Kraehenbuhl, J.-P.; Aguzzi, A. Transepithelial prion transport by M cells. Nat. Med. 2001, 7, 976–977. [Google Scholar]
- Tribouillard-Tanvier, D.; Striebel, J.F.; Peterson, K.E.; Chesebro, B. Analysis of Protein Levels of 24 Cytokines in Scrapie Agent-Infected Brain and Glial Cell Cultures from Mice Differing in Prion Protein Expression Levels. J. Virol. 2009, 83, 11244–11253. [Google Scholar] [CrossRef]
- Lu, Z.Y.; Baker, C.A.; Manuelidis, L. New molecular markers of early and progressive CJD brain infection. J. Cell. Biochem. 2004, 93, 644–652. [Google Scholar]
- Felton, L.M.; Cunningham, C.; Rankine, E.L.; Waters, S.; Boche, D.; Perry, V.H. MCP-1 and murine prion disease: Separation of early behavioural dysfunction from overt clinical disease. Neurobiol. Dis. 2005, 20, 283–295. [Google Scholar] [CrossRef]
- Sorensen, G.; Medina, S.; Parchaliuk, D.; Phillipson, C.; Robertson, C.; Booth, S. Comprehensive transcriptional profiling of prion infection in mouse models reveals networks of responsive genes. BMC Genomics 2008, 9. [Google Scholar] [CrossRef]
- Riemer, C.; Queck, I.; Simon, D.; Kurth, R.; Baier, M. Identification of Upregulated Genes in Scrapie-Infected Brain Tissue. J. Virol. 2000, 74, 10245–10248. [Google Scholar]
- Burwinkel, M.; Schwarz, A.; Riemer, C.; Schultz, J.; van Landeghem, F.; Baier, M. Rapid disease development in scrapie-infected mice deficient for CD40 ligand. EMBO Rep. 2004, 5, 527–531. [Google Scholar]
- Mohan, J.; Bruce, M.E.; Mabbott, N.A. Neuroinvasion by Scrapie following Inoculation via the Skin Is Independent of Migratory Langerhans Cells. J. Virol. 2005, 79, 1888–1897. [Google Scholar]
- Mabbott, N.A.; Bruce, M.E. Complement component C5 is not involved in scrapie pathogenesis. Immunobiology 2004, 209, 545–549. [Google Scholar] [CrossRef]
- Gossner, A.; Roupaka, S.; Foster, J.; Hunter, N.; Hopkins, J. Transcriptional profiling of peripheral lymphoid tissue reveals genes and networks linked to SSBP/1 scrapie pathology in sheep. Vet. Microbiol. 2011, 153, 218–228. [Google Scholar] [CrossRef]
- Zabel, M.D.; Heikenwalder, M.; Prinz, M.; Arrighi, I.; Schwarz, P.; Kranich, J.; von Teichman, A.; Haas, K.M.; Zeller, N.; Tedder, T.F.; et al. Stromal complement receptor CD21/35 facilitates lymphoid prion colonization and pathogenesis. J. Immunol. 2007, 179, 6144–6152. [Google Scholar]
- Sein, L.; Yasuo, I.; Yasuro, A.; Hiroshi, U.; Naotaka, I. Immune cell types involved in early uptake and transport of recombinant mouse prion protein in Peyer’s patches of calves. Cell Tissue Res. 2009, 338, 343–354. [Google Scholar]
- Eaton, S.L.; Rocchi, M.; Gonzalez, L.; Hamilton, S.; Finlayson, J.; Sales, J.; Jeffrey, M.; Steele, P.J.; Dagleish, M.P.; Rodger, S.M.; et al. Immunological differences between susceptible and resistant sheep during the preclinical phase of scrapie infection. J. Gen. Virol. 2007, 88, 1384–1391. [Google Scholar] [CrossRef]
- Baker, C.A.; Manuelidis, L. Unique inflammatory RNA profiles of microglia in Creutzfeldt-Jakob disease. Proc. Natl. Acad. Sci. USA 2003, 100, 675–679. [Google Scholar]
- Schultz, J.; Schwarz, A.; Neidhold, S.; Burwinkel, M.; Riemer, C.; Simon, D.; Kopf, M.; Otto, M.; Baier, M. Role of Interleukin-1 in Prion Disease-Associated Astrocyte Activation. Am. J. Pathol. 2004, 165, 671–678. [Google Scholar] [CrossRef]
- Williams, A.E.; Lawson, L.J.; Perry, V.H.; Fraser, H. Characterization of the microglial response in murine scrapie. Neuropathol. Appl. Neurobiol. 1994, 20, 47–55. [Google Scholar]
- Isaacs, J.D.; Garden, O.A.; Kaur, G.; Collinge, J.; Jackson, G.S.; Altmann, D.M. The cellular prion protein is preferentially expressed by CD4+ CD25+ Foxp3+ regulatory T cells. Immunology 2008, 125, 313–319. [Google Scholar] [CrossRef]
- Le, Y.; Yazawa, H.; Gong, W.; Yu, Z.; Ferrans, V.J.; Murphy, P.M.; Wang, J.M. Cutting Edge: The Neurotoxic Prion Peptide Fragment PrP106–126 is a Chemotactic Agonist for the G Protein-Coupled Receptor Formyl Peptide Receptor-Like 1. J. Immunol. 2001, 166, 1448–1451. [Google Scholar]
- Booth, S.; Bowman, C.; Baumgartner, R.; Sorensen, G.; Robertson, C.; Coulthart, M.; Phillipson, C.; Somorjai, R.L. Identification of central nervous system genes involved in the host response to the scrapie agent during preclinical and clinical infection. J. Gen. Virol. 2004, 85, 3459–3471. [Google Scholar] [CrossRef]
- Starke, R.; Harrison, P.; Mackie, I.; Wang, G.; Erusalimsky, J.D.; Gale, R.; MassÉ, J.M.; Cramer, E.; Pizzey, A.; Biggerstaff, J.; et al. The expression of prion protein (PrPC) in the megakaryocyte lineage. J. Thromb. Haemost. 2005, 3, 1266–1273. [Google Scholar] [CrossRef]
- Uraki, R.; Sakudo, A.; Michibata, K.; Ano, Y.; Kono, J.; Yukawa, M.; Onodera, T. Blocking of FcR Suppresses the Intestinal Invasion of Scrapie Agents. PLoS One 2011, 6, e17928. [Google Scholar]
- Prinz, M.; Huber, G.; Macpherson, A.J.S.; Heppner, F.L.; Glatzel, M.; Eugster, H.-P.; Wagner, N.; Aguzzi, A. Oral Prion Infection Requires Normal Numbers of Peyer’s Patches but Not of Enteric Lymphocytes. Am. J. Pathol. 2003, 162, 1103–1111. [Google Scholar]
- Luhr, K.M.; Wallin, R.P.A.; Ljunggren, H.-G.; Low, P.; Taraboulos, A.; Kristensson, K. Processing and Degradation of Exogenous Prion Protein by CD11c+ Myeloid Dendritic Cells in vitro. J. Virol. 2002, 76, 12259–12264. [Google Scholar]
- Piercey Åkesson, C.; Press, C.M.; Tranulis, M.A.; Jeffrey, M.; Aleksandersen, M.; Landsverk, T.; Espenes, A. Phenotypic characterization of cells participating in transport of prion protein aggregates across the intestinal mucosa of sheep. Prion 2012, 6, 261–275. [Google Scholar]
- Li, C.; Yu, S.; Nakamura, F.; Pentikäinen, O.T.; Singh, N.; Yin, S.; Xin, W.; Sy, M.-S. Pro-prion Binds Filamin A, Facilitating its Interaction with Integrin β1, and Contributes to Melanomagenesis. J. Biol. Chem. 2010, 285, 30328–30339. [Google Scholar]
- Walsh, D.T.; Betmouni, S.; Perry, V.H. Absence of detectable IL-1 beta production in murine prion disease: A model of chronic neurodegeneration. J. Neuropathol. Exp. Neurol. 2001, 60, 173–182. [Google Scholar]
- Tamguney, G.; Giles, K.; Glidden, D.V.; Lessard, P.; Wille, H.; Tremblay, P.; Groth, D.F.; Yehiely, F.; Korth, C.; Moore, R.C.; et al. Genes contributing to prion pathogenesis. J. Gen. Virol. 2008, 89, 1777–1788. [Google Scholar] [CrossRef]
- Thackray, A.M.; McKenzie, A.N.; Klein, M.A.; Lauder, A.; Bujdoso, R. Accelerated Prion Disease in the Absence of Interleukin-10. J. Virol. 2004, 78, 13697–13707. [Google Scholar]
- Mabbott, N.A.; Williams, A.; Farquhar, C.F.; Pasparakis, M.; Kollias, G.; Bruce, M.E. Tumor Necrosis Factor Alpha-Deficient, but Not Interleukin-6-Deficient, Mice Resist Peripheral Infection with Scrapie. J. Virol. 2000, 74, 3338–3344. [Google Scholar] [CrossRef]
- Tribouillard-Tanvier, D.; Race, B.; Striebel, J.F.; Carroll, J.A.; Phillips, K.; Chesebro, B. Early cytokine elevation, PrPres deposition and gliosis in mouse scrapie: No effect on disease by deletion of cytokine genes, IL-12p40 and IL-12p35. J. Virol. 2012, 86, 10377–10383. [Google Scholar] [CrossRef]
- Rosicarelli, B.; Serafini, B.; Sbriccoli, M.; Lu, M.; Cardone, F.; Pocchiari, M.; Aloisi, F. Migration of dendritic cells into the brain in a mouse model of prion disease. J. Neuroimmunol. 2005, 165, 114–120. [Google Scholar]
- Baker, C.A.; Lu, Z.Y.; Manuelidis, L. Early induction of interferon-responsive mRNAs in Creutzfeldt-Jakob disease. J. Neurovirol. 2004, 10, 29–40. [Google Scholar]
- Oldstone, M.B.A.; Race, R.; Thomas, D.; Lewicki, H.; Homann, D.; Smelt, S.; Holz, A.; Koni, P.; Lo, D.; Chesebro, B.; et al. Lymphotoxin-α- and Lymphotoxin-β- Deficient Mice Differ in Susceptibility to Scrapie: Evidence against Dendritic Cell Involvement in Neuroinvasion. J. Virol. 2002, 76, 4357–4363. [Google Scholar]
- Kopacek, J.; Sakaguchi, S.; Shigematsu, K.; Nishida, N.; Atarashi, R.; Nakaoke, R.; Moriuchi, R.; Niwa, M.; Katamine, S. Upregulation of the Genes Encoding Lysosomal Hydrolases, a Perforin-Like Protein, and Peroxidases in the Brains of Mice Affected with an Experimental Prion Disease. J. Virol. 2000, 74, 411–417. [Google Scholar]
- Cunningham, C.; Wilcockson, D.C.; Boche, D.; Perry, V.H. Comparison of Inflammatory and Acute-Phase Responses in the Brain and Peripheral Organs of the ME7 Model of Prion Disease. J. Virol. 2005, 79, 5174–5184. [Google Scholar]
- Saba, R.; Gushue, S.; Huzarewich, R.L.C.H.; Manguiat, K.; Medina, S.; Robertson, C.; Booth, S.A. MicroRNA 146a (miR-146a) is Over-Expressed during Prion Disease and Modulates the Innate Immune Response and the Microglial Activation State. PLoS One 2012, 7, e30832. [Google Scholar]
- Bueler, H.; Aguzzi, A.; Sailer, A.; Greiner, R.A.; Autenried, P.; Aguet, M.; Weissmann, C. Mice devoid of PrP are resistant to scrapie. Cell 1993, 73, 1339–1347. [Google Scholar]
- Manson, J.C.; Clarke, A.R.; McBride, P.A.; McConnell, I.; Hope, J. PrP gene dosage determines the timing but not the final intensity or distribution of lesions in scrapie pathology. Neurodegeneration 1994, 3, 331–340. [Google Scholar]
- Betmouni, S.; Perry, V.H. The acute inflammatory response in CNS following injection of prion brain homogenate or normal brain homogenate. Neuropathol. Appl. Neurobiol. 1999, 25, 19–27. [Google Scholar] [CrossRef]
- Mok, S.W.F.; Proia, R.L.; Brinkmann, V.; Mabbott, N.A. B Cell-Specific S1PR1 Deficiency Blocks Prion Dissemination between Secondary Lymphoid Organs. J. Immunol. 2012, 188, 5032–5040. [Google Scholar]
- Segundo, F.D.S.; Sevilla, N.; Gutierrez, J.P.; Brun, A. Altered lymphocyte homeostasis after oral prion infection in mouse. Vet. Immunol. Immunopathol. 2008, 122, 204–215. [Google Scholar] [CrossRef]
- Martinez del Hoyo, G.; Lopez-Bravo, M.; Metharom, P.; Ardavin, C.; Aucouturier, P. Prion Protein Expression by Mouse Dendritic Cells is Restricted to the Nonplasmacytoid Subsets and Correlates with the Maturation State. J. Immunol. 2006, 177, 6137–6142. [Google Scholar]
- Cunningham, C.; Boche, D.; Perry, V.H. Transforming growth factor β1, the dominant cytokine in murine prion disease: influence on inflammatory cytokine synthesis and alteration of vascular extracellular matrix. Neuropathol. Appl. Neurobiol. 2002, 28, 107–119. [Google Scholar] [CrossRef]
- Baker, C.A.; Lu, Z.Y.; Zaitsev, I.; Manuelidis, L. Microglial Activation Varies in Different Models of Creutzfeldt-Jakob Disease. J. Virol. 1999, 73, 5089–5097. [Google Scholar]
- Raymond, C.R.; Mabbott, N.A. Assessing the involvement of migratory dendritic cells in the transfer of the scrapie agent from the immune to peripheral nervous systems. J. Neuroimmunol. 2007, 187, 114–125. [Google Scholar]
- Mabbott, N.A.; McGovern, G.; Jeffrey, M.; Bruce, M.E. Temporary Blockade of the Tumor Necrosis Factor Receptor Signaling Pathway Impedes the Spread of Scrapie to the Brain. J. Virol. 2002, 76, 5131–5139. [Google Scholar] [CrossRef]
- Gehlenborg, N.; Hwang, D.; Lee, I.Y.; Yoo, H.; Baxter, D.; Petritis, B.; Pitstick, R.; Marzolf, B.; DeArmond, S.J.; Carlson, G.A.; et al. The Prion Disease Database: A comprehensive transcriptome resource for systems biology research in prion diseases. Database 2009, 2009. [Google Scholar] [CrossRef]
- Rybner, C.; Hillion, J.; Sahraoui, T.; Lanotte, M.; Botti, J. All-trans retinoic acid down-regulates prion protein expression independently of granulocyte maturation. Leukemia 2002, 16, 940–948. [Google Scholar]
- Cordier-Dirikoc, S.; Zsürger, N.; Cazareth, J.; Ménard, B.; Chabry, J. Expression profiles of prion and doppel proteins and of their receptors in mouse splenocytes. Eur. J. Immunol. 2008, 38, 2131–2141. [Google Scholar]
- Miragliotta, G.; Fumarulo, R.; Fumarola, D. Inhibition of Neutrophil Functions by Scrapie Prion Protein—Description of Some Inhibitory Properties. Acta Virol. 1990, 34, 517–522. [Google Scholar]
- Le, Y.; Zhou, Y.; Tao, H.; Wang, J.M. Formylpeptide receptors and their potential roles in inflammatory airway diseases. Clin. Exp. Allergy Rev. 2004, 4, 155–161. [Google Scholar]
- Orange, J.S.; Fassett, M.S.; Koopman, L.A.; Boyson, J.E.; Strominger, J.L. Viral evasion of natural killer cells. Nat. Immunol. 2002, 3, 1006–1012. [Google Scholar] [CrossRef]
- Jonjić, S.; Babić, M.; Polić, B.; Krmpotić, A. Immune evasion of natural killer cells by viruses. Curr. Opin. Immunol. 2008, 20, 30–38. [Google Scholar]
- Lanier, L.L. Evolutionary struggles between NK cells and viruses. Nat. Rev. Immunol. 2008, 8, 259–268. [Google Scholar] [CrossRef]
- Raslova, H.; Kauffmann, A.; Sekkaï, D.; Ripoche, H.; Larbret, F.; Robert, T.; Le Roux, D.T.; Kroemer, G.; Debili, N.; Dessen, P.; et al. Interrelation between polyploidization and megakaryocyte differentiation: A gene profiling approach. Blood 2007, 109, 3225–3234. [Google Scholar] [CrossRef]
- Opalinska, J.B.; Bersenev, A.; Zhang, Z.; Schmaier, A.A.; Choi, J.; Yao, Y.; D'Souza, J.; Tong, W.; Weiss, M.J. MicroRNA expression in maturing murine megakaryocytes. Blood 2010, 116, e128–e138. [Google Scholar]
- Robertson, C.; Booth, S.A.; Beniac, D.R.; Coulthart, M.B.; Booth, T.F.; McNicol, A. Cellular prion protein is released on exosomes from activated platelets. Blood 2006, 107, 3907–3911. [Google Scholar]
- Wang, G.; Zhou, X.; Bai, Y.; Zhang, Z.; Zhao, D. Cellular prion protein released on exosomes from macrophages binds to Hsp70. Acta Biochim. Biophys. Sin. 2010, 42, 345–350. [Google Scholar] [CrossRef]
- Beaulieu, L.M.; Lin, E.; Morin, K.M.; Tanriverdi, K.; Freedman, J.E. Regulatory effects of TLR2 on megakaryocytic cell function. Blood 2011, 117, 5963–5974. [Google Scholar]
- McCutcheon, S.; Alejo Blanco, A.R.; Houston, E.F.; de Wolf, C.; Tan, B.C.; Smith, A.; Groschup, M.H.; Hunter, N.; Hornsey, V.S.; MacGregor, I.R.; et al. All Clinically-Relevant Blood Components Transmit Prion Disease following a Single Blood Transfusion: A Sheep Model of vCJD. PLoS One 2011, 6, e23169. [Google Scholar]
- Houston, F.; McCutcheon, S.; Goldmann, W.; Chong, A.; Foster, J.; Siso, S.; Gonzalez, L.; Jeffrey, M.; Hunter, N. Prion diseases are efficiently transmitted by blood transfusion in sheep. Blood 2008, 112, 4739–4745. [Google Scholar]
- Hunter, N.; Foster, J.; Chong, A.; McCutcheon, S.; Parnham, D.; Eaton, S.; MacKenzie, C.; Houston, F. Transmission of prion diseases by blood transfusion. J. Gen. Virol. 2002, 83, 2897–2905. [Google Scholar]
- Mathiason, C.K.; Hayes-Klug, J.; Hays, S.A.; Powers, J.; Osborn, D.A.; Dahmes, S.J.; Miller, K.V.; Warren, R.J.; Mason, G.L.; Telling, G.C.; et al. B Cells and Platelets Harbor Prion Infectivity in the Blood of Deer Infected with Chronic Wasting Disease. J. Virol. 2010, 84, 5097–5107. [Google Scholar]
- McBride, P.A.; Schulz-Schaeffer, W.J.; Donaldson, M.; Bruce, M.; Diringer, H.; Kretzschmar, H.A.; Beekes, M. Early Spread of Scrapie from the Gastrointestinal Tract to the Central Nervous System Involves Autonomic Fibers of the Splanchnic and Vagus Nerves. J. Virol. 2001, 75, 9320–9327. [Google Scholar] [CrossRef]
- Beekes, M.; McBride, P.A. The spread of prions through the body in naturally acquired transmissible spongiform encephalopathies. FEBS J. 2007, 274, 588–605. [Google Scholar]
- Sisó, S.; Jeffrey, M.; González, L. Neuroinvasion in sheep transmissible spongiform encephalopathies: The role of the haematogenous route. Neuropathol. Appl. Neurobiol. 2009, 35, 232–246. [Google Scholar] [CrossRef]
- Loeuillet, C.; Lemaire-Vieille, C.; Naquet, P.; Cesbron-Delauw, M.-F.; Gagnon, J.; Cesbron, J.-Y. Prion Replication in the Hematopoietic Compartment Is Not Required for Neuroinvasion in Scrapie Mouse Model. PLoS One 2010, 5, e13166. [Google Scholar]
- Magalhães, A.C.; Baron, G.S.; Lee, K.S.; Steele-Mortimer, O.; Dorward, D.; Prado, M.A.M.; Caughey, B. Uptake and Neuritic Transport of Scrapie Prion Protein Coincident with Infection of Neuronal Cells. J. Neurosci. 2005, 25, 5207–5216. [Google Scholar] [CrossRef]
- Liu, T.; Li, R.; Wong, B.-S.; Liu, D.; Pan, T.; Petersen, R.B.; Gambetti, P.; Sy, M.-S. Normal Cellular Prior Protein is Preferentially Expressed on Subpopulations of Murine Hemopoietic Cells. J. Immunol. 2001, 166, 3733–3742. [Google Scholar]
- Kubosaki, A.; Yusa, S.; Nasu, Y.; Nishimura, T.; Nakamura, Y.; Saeki, K.; Matsumoto, Y.; Itohara, S.; Onodera, T. Distribution of Cellular Isoform of Prion Protein in T Lymphocytes and Bone Marrow, Analyzed by Wild-Type and Prion Protein Gene-Deficient Mice. Biochem. Biophys. Res. Commun. 2001, 282, 103–107. [Google Scholar] [CrossRef]
- Ford, M.J.; Burton, L.J.; Li, H.; Graham, C.H.; Frobert, Y.; Grassi, J.; Hall, S.M.; Morris, R.J. A marked disparity between the expression of prion protein and its message by neurones of the CNS. Neuroscience 2002, 111, 533–551. [Google Scholar] [CrossRef]
- Ford, M.J.; Burton, L.J.; Morris, R.J.; Hall, S.M. Selective expression of prion protein in peripheral tissues of the adult mouse. Neuroscience 2002, 113, 177–192. [Google Scholar]
- Mabbott, N.A.; Kenneth Baillie, J.; Hume, D.A.; Freeman, T.C. Meta-analysis of lineage-specific gene expression signatures in mouse leukocyte populations. Immunobiology 2010, 215, 724–736. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).