Decreased Quality of Life in Individuals with Type 2 Diabetes Mellitus Is Associated with Emotional Distress
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Participants
2.3. Assessment Procedure
2.4. Statistical Analysis
3. Results
3.1. Demographic and Clinical Features
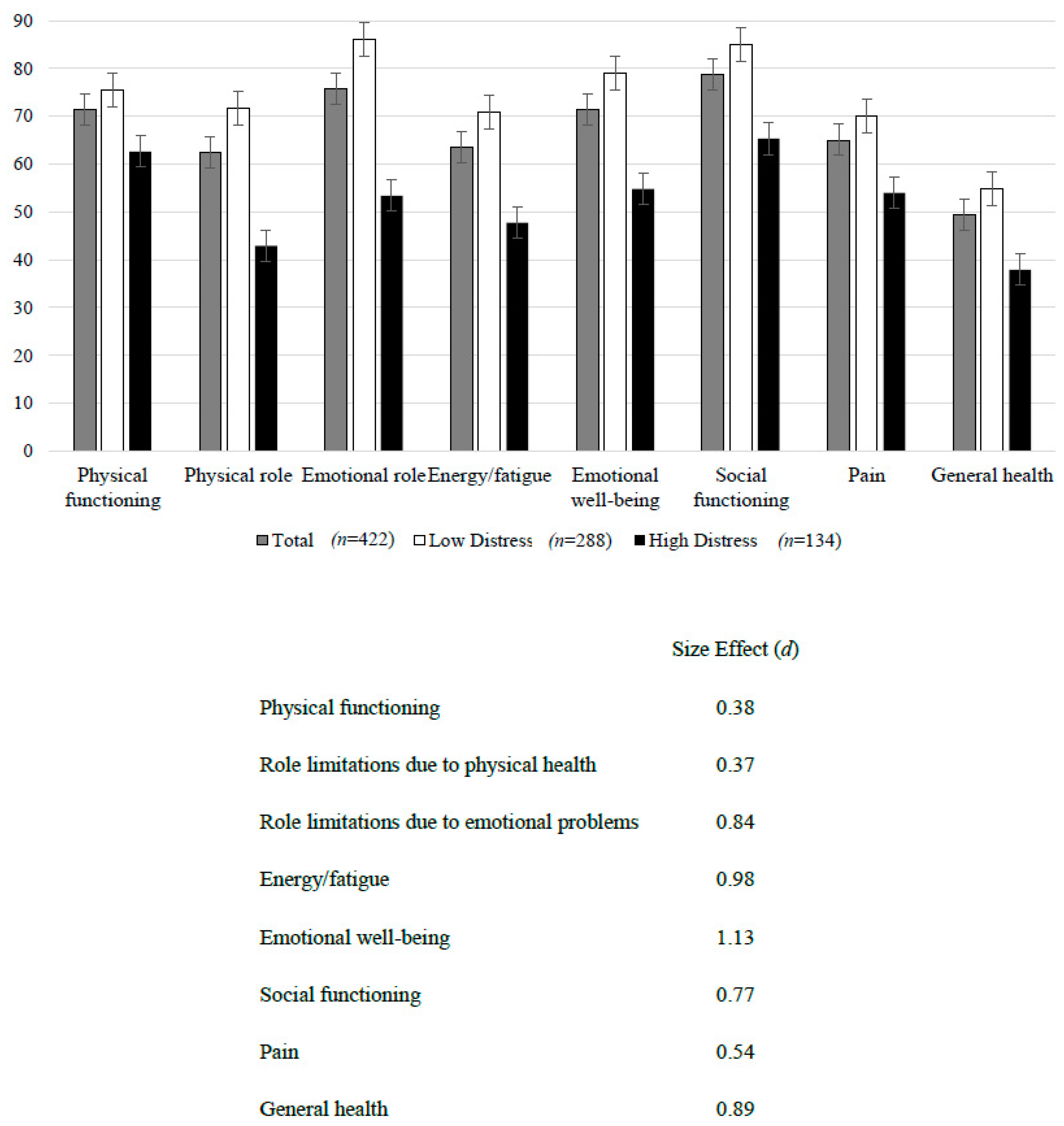
3.2. Health-Related Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cho, N.; Shaw, J.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.; Ohlrogge, A.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Prac. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Federation, I.D. IDF Diabetes Atlas; International Diabetes Federation: Brussels, Belgium, 2015. [Google Scholar]
- Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [CrossRef]
- DeFronzo, R.A.; Ferrannini, E.; Alberti, K.G.M.M.; Zimmet, P.; Alberti, G. International Textbook of Diabetes Mellitus, 2 Volume Set; John Wiley Sons: Hoboken, NJ, USA, 2015; Volume 1. [Google Scholar]
- Molina Iriarte, A.; Acevedo Giles, O.; Yáñez Sandoval, M.E.; Dávila Mendoza, R.; González Pedraza Avilés, A. Comparación de las prevalencias de duelo, depresión y calidad de vida asociados con la enfermedad entre pacientes con diabetes mellitus tipo 2 descontrolados y controlados. Rev. Espec. Médico-Quirúrgicas 2013, 18, 13–18. [Google Scholar]
- Juárez-Rojop, I.E.; Fortuny-Falconi, C.M.; González-Castro, T.B.; Tovilla-Zárate, C.A.; Villar-Soto, M.; Sanchez, E.R.; Hernández-Díaz, Y.; López-Narvaez, M.L.; Ble-Castillo, J.L.; Pérez-Hernández, N.; et al. Association between reduced quality of life and depression in patients with type 2 diabetes mellitus: A cohort study in a Mexican population. Neuropsychiatr. Dis. Treat. 2018, 14, 2511–2518. [Google Scholar] [CrossRef]
- Ogurtsova, K.; da Rocha Fernandes, J.; Huang, Y.; Linnenkamp, U.; Guariguata, L.; Cho, N.; Cavan, D.; Shaw, J.; Makaroff, L. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res. Clin. Prac. 2017, 128, 40–50. [Google Scholar] [CrossRef] [Green Version]
- Rivera-Ledesma, A.; Lena, M.M.-L.; Sandoval-Ávila, R. Desajuste psicológico, calidad de vida y afrontamiento en pacientes diabéticos con insuficiencia renal crónica en diálisis peritoneal. Salud Ment. 2012, 35, 329–337. [Google Scholar]
- Granados, E.E.; Escalante, E. Estilos de personalidad y adherencia al tratamiento en pacientes con diabetes mellitus. Liberabit 2010, 16, 203–216. [Google Scholar]
- Lazcano Ortiz, M.; Salazar González, B.C. Estrés percibido y adaptación en pacientes con diabetes mellitus tipo 2. Aquichan 2007, 7, 77–84. [Google Scholar]
- Ortiz, M.; Ortiz, E.; Gatica, A.; Gómez, D. Factores psicosociales asociados a la adherencia al tratamiento de la diabetes mellitus tipo 2. Ter. Psicol. 2011, 29, 5–11. [Google Scholar] [CrossRef]
- Schmidt, C.B.; van Loon, B.J.P.; Vergouwen, A.C.M.; Snoek, F.J.; Honig, A. Systematic review and meta-analysis of psychological interventions in people with diabetes and elevated diabetes-distress. Diabet. Med. 2018. [Google Scholar] [CrossRef]
- Babenko, A.Y.; Mosikian, A.A.; Lebedev, D.L.; Khrabrova, E.A.; Shlyakhto, E.V. Mental state, psychoemotional status, quality of life and treatment compliance in patients with Type 2 diabetes mellitus. J. Comp. Eff. Res. 2019, 8, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, P.; Dos Santos, M.; Zanetti, M.; Ferronato, A. Dificultades de los pacientes diabéticos para el control de la enfermedad: Sentimientos y comportamientos. Rev. Latino-Am. Enferm. 2007, 15, 1105–1112. [Google Scholar]
- Iriarte, A.M.; Acevedo Giles, O.; Sandoval, M.E.Y.; Dávila Mendoza, R.; González Pedraza Avilés, A. Comparison of prevalence of mourning, depression and quality of life related to disease between patients with uncontrolled and controlled diabetes mellitus type 2. Rev. Espec. Médico-Quirúrgicas 2013, 18, 13–18. [Google Scholar]
- Organization, W.H. Use of Glycated Haemoglobin (HbA1c) in Diagnosis of Diabetes Mellitus: Abbreviated Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Durán-Arenas, L.; Gallegos-Carrillo, K.; Salinas-Escudero, G.; Martínez-Salgado, H. Towards a Mexican normative standard for measurement of the short format 36 health-related quality of life instrument. Salud Publica Mex. 2004, 46, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Zúniga, M.A.; Carrillo-Jiménez, G.T.; Fos, P.J.; Gandek, B.; Medina-Moreno, M.R. Evaluación del estado de salud con la Encuesta SF-36: Resultados preliminares en México. Salud Pública Méx. 1999, 41, 110–118. [Google Scholar] [CrossRef] [PubMed]
- McGuire, B.; Morrison, T.; Hermanns, N.; Skovlund, S.; Eldrup, E.; Gagliardino, J.; Kokoszka, A.; Matthews, D.; Pibernik-Okanović, M.; Rodríguez-Saldaña, J. Short-form measures of diabetes-related emotional distress: The Problem Areas in Diabetes Scale (PAID)-5 and PAID-1. Diabetologia 2010, 53, 66. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Thames, UK, 2013. [Google Scholar]
- Sánchez-Cruz, J.F.; Hipólito-Lóenzo, A.; Mugártegui-Sánchez, S.G.; Yáñez-González, R.M. Estrés y Depresión asociados a la no adherencia al tratamiento en pacientes con Diabetes Mellitus tipo 2. Atención Fam. 2016, 23, 43–47. [Google Scholar] [CrossRef]
- Viveros, G.R.O.; Herrera, É.O. Capacidad predictiva de la adherencia al tratamiento en los modelos socio-cognitivos de creencias en salud. Psicol. Y Salud 2011, 21, 79–90. [Google Scholar]
- Pedraza Banderas, G.L.; Vega Valero, C.Z. Caracterización psicosocial de pacientes diabéticos mexicanos. Rev. Electrón. Psicol. Iztacala 2019, 21, 1371–1393. [Google Scholar]
- Le, T.K.; Curtis, B.; Kahle-Wrobleski, K.; Johnston, J.; Haldane, D.; Melfi, C. Treatment patterns and resource use among patients with comorbid diabetes mellitus and major depressive disorder. J. Med. Econ. 2011, 14, 440–447. [Google Scholar] [CrossRef]
- Bruno, B.A.; Choi, D.; Thorpe, K.E.; Yu, C.H. Relationship Among Diabetes Distress, Decisional Conflict, Quality of Life, and Patient Perception of Chronic Illness Care in a Cohort of Patients with Type 2 Diabetes and Other Comorbidities. Diabetes Care 2019, 42, 1170–1177. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.J.; McKay, S.V. Barriers to glycemic control in youth with type 1 diabetes and type 2 diabetes. Pediatr. Diabetes 2011, 12, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Chan, O.; Inouye, K.; Akirav, E.; Park, E.; Riddell, M.C.; Vranic, M.; Matthews, S.G. Insulin alone increases hypothalamo-pituitary-adrenal activity, and diabetes lowers peak stress responses. Endocrinology 2005, 146, 1382–1390. [Google Scholar] [CrossRef] [PubMed]
- Chong, A.C.; Vogt, M.C.; Hill, A.S.; Bruning, J.C.; Zeltser, L.M. Central insulin signaling modulates hypothalamus-pituitary-adrenal axis responsiveness. Mol. Metab. 2015, 4, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Lopez, J.F.; Chalmers, D.T.; Little, K.Y.; Watson, S.J.A.E. Bennett Research Award. Regulation of serotonin1A, glucocorticoid, and mineralocorticoid receptor in rat and human hippocampus: Implications for the neurobiology of depression. Biol. Psychiatry 1998, 43, 547–573. [Google Scholar] [CrossRef]
- Lyra, E.S.N.M.; Lam, M.P.; Soares, C.N.; Munoz, D.P.; Milev, R.; De Felice, F.G. Insulin Resistance as a Shared Pathogenic Mechanism Between Depression and Type 2 Diabetes. Front. Psychiatry 2019, 10, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Starr, J.M.; Wardlaw, J.; Ferguson, K.; MacLullich, A.; Deary, I.J.; Marshall, I. Increased blood-brain barrier permeability in type II diabetes demonstrated by gadolinium magnetic resonance imaging. J. Neurol. Neurosurg. Psychiatry 2003, 74, 70–76. [Google Scholar] [CrossRef]
- Felger, J.C.; Haroon, E.; Woolwine, B.J.; Raison, C.L.; Miller, A.H. Interferon-alpha-induced inflammation is associated with reduced glucocorticoid negative feedback sensitivity and depression in patients with hepatitis C virus. Physiol. Behav. 2016, 166, 14–21. [Google Scholar] [CrossRef]
- Clarke, J.R.; Lyra, E.S.N.M.; Figueiredo, C.P.; Frozza, R.L.; Ledo, J.H.; Beckman, D.; Katashima, C.K.; Razolli, D.; Carvalho, B.M.; Frazao, R.; et al. Alzheimer-associated Abeta oligomers impact the central nervous system to induce peripheral metabolic deregulation. EMBO Mol. Med. 2015, 7, 190–210. [Google Scholar] [CrossRef]
- Lourenco, M.V.; Clarke, J.R.; Frozza, R.L.; Bomfim, T.R.; Forny-Germano, L.; Batista, A.F.; Sathler, L.B.; Brito-Moreira, J.; Amaral, O.B.; Silva, C.A.; et al. TNF-alpha mediates PKR-dependent memory impairment and brain IRS-1 inhibition induced by Alzheimer’s beta-amyloid oligomers in mice and monkeys. Cell Metab. 2013, 18, 831–843. [Google Scholar] [CrossRef]
- Gupta, S.; Bi, R.; Kim, C.; Chiplunkar, S.; Yel, L.; Gollapudi, S. Role of NF-kappaB signaling pathway in increased tumor necrosis factor-alpha-induced apoptosis of lymphocytes in aged humans. Cell Death Differ. 2005, 12, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Dantzer, R.; O’Connor, J.C.; Freund, G.G.; Johnson, R.W.; Kelley, K.W. From inflammation to sickness and depression: When the immune system subjugates the brain. Nat. Rev. Neurosci. 2008, 9, 46. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Sun, X.; Yu, Y. The prevalence of impaired glucose regulation in psychiatric patients with sleep disorders and its relationship with altered hypothalamopituitary–adrenal and hypothalamopituitary–thyroid axis activity. Sleep Med. 2013, 14, 662–667. [Google Scholar] [CrossRef] [PubMed]
| Total Sample n = 422 | Low Distress n = 288 | High Distress n = 134 | Statistics | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Gender-Women | 294 | 69.7 | 195 | 67.7 | 99 | 73.9 | Fisher = 0.19 |
| Marital status-Married | 258 | 61.1 | 184 | 63.9 | 74 | 66.2 | Fisher = 0.10 |
| Socioeconomic status | Fisher = 0.20 | ||||||
| Medium | 187 | 44.3 | 134 | 46.5 | 53 | 39.6 | |
| Low | 231 | 54.7 | 151 | 52.4 | 80 | 59.7 | |
| Non-remunerated activity | 280 | 66.4 | 184 | 63.9 | 96 | 71.6 | Fisher = 0.12 |
| BMI—Overweight/obesity | 333 | 78.9 | 235 | 81.6 | 98 | 73.1 | Fisher = 0.06 |
| HbA1C ≥ 6.5 | 340 | 80.6 | 227 | 78.8 | 113 | 84.3 | Fisher = 0.18 |
| Medical comorbidity | |||||||
| -Hepatic | 54 | 12.8 | 28 | 9.7 | 26 | 19.4 | Fisher = 0.008 |
| -Renal | 103 | 24.4 | 65 | 22.6 | 38 | 28.4 | Fisher = 0.22 |
| -Neuropathy | 191 | 45.3 | 125 | 43.4 | 66 | 49.3 | Fisher = 0.29 |
| -Cardiovascular | 184 | 43.6 | 124 | 43.1 | 60 | 44.8 | Fisher = 0.74 |
| Current treatment | |||||||
| -Insulin | 296 | 70.1 | 194 | 67.4 | 102 | 76.1 | Fisher = 0.07 |
| -Hypoglycemic agent | 387 | 91.7 | 269 | 93.4 | 118 | 88.1 | Fisher = 0.08 |
| -Antihypertensive agent | 203 | 48.1 | 142 | 49.3 | 61 | 45.5 | Fisher = 0.53 |
| Substance use | |||||||
| -Alcohol—Yes | 67 | 15.9 | 43 | 14.9 | 24 | 17.9 | Fisher = 0.43 |
| -Marihuana—Yes | 2 | 0.5 | 1 | 0.3 | 1 | 0.7 | Fisher = 0.53 |
| -Nicotine—Yes | 23 | 5.5 | 17 | 5.9 | 6 | 4.5 | Fisher = 0.65 |
| Psychiatric comorbidity | |||||||
| -Major depression—Yes | 46 | 10.9 | 25 | 8.7 | 21 | 15.7 | Fisher = 0.04 |
| -Manic episodes—Yes | 1 | 0.2 | 1 | 0.3 | - | Fisher = 1.00 | |
| -Alcohol use disorder—Yes | 2 | 0.5 | 1 | 0.3 | 1 | 0.7 | Fisher = 0.53 |
| -Psychosis—Yes | 1 | 0.2 | 1 | 0.3 | - | Fisher = 1.00 | |
| Mean | S.D. | Mean | S.D. | Mean | S.D. | ||
| Current age | 54.8 | 12.8 | 56.8 | 12.1 | 50.6 | 13.1 | t =1.2, p = 0.23 |
| Years of education | 6.9 | 4.4 | 7.1 | 4.5 | 6.6 | 4.4 | t = 0.2, p = 0.83 |
| Illness evolution (years) | 15.1 | 8.7 | 15.8 | 8.8 | 13.6 | 8.1 | t = 0.2, p = 0.82 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Pimienta, E.; González-Castro, T.B.; Fresan, A.; Juárez-Rojop, I.E.; Martínez-López, M.C.; Barjau-Madrigal, H.A.; Ramírez-González, I.R.; Martínez-Villaseñor, E.; Rodríguez-Sánchez, E.; Villar-Soto, M.; et al. Decreased Quality of Life in Individuals with Type 2 Diabetes Mellitus Is Associated with Emotional Distress. Int. J. Environ. Res. Public Health 2019, 16, 2652. https://doi.org/10.3390/ijerph16152652
Gómez-Pimienta E, González-Castro TB, Fresan A, Juárez-Rojop IE, Martínez-López MC, Barjau-Madrigal HA, Ramírez-González IR, Martínez-Villaseñor E, Rodríguez-Sánchez E, Villar-Soto M, et al. Decreased Quality of Life in Individuals with Type 2 Diabetes Mellitus Is Associated with Emotional Distress. International Journal of Environmental Research and Public Health. 2019; 16(15):2652. https://doi.org/10.3390/ijerph16152652
Chicago/Turabian StyleGómez-Pimienta, Elena, Thelma Beatriz González-Castro, Ana Fresan, Isela Esther Juárez-Rojop, Miriam Carolina Martínez-López, Hugo Adrián Barjau-Madrigal, Iris Rubí Ramírez-González, Esteban Martínez-Villaseñor, Esther Rodríguez-Sánchez, Mario Villar-Soto, and et al. 2019. "Decreased Quality of Life in Individuals with Type 2 Diabetes Mellitus Is Associated with Emotional Distress" International Journal of Environmental Research and Public Health 16, no. 15: 2652. https://doi.org/10.3390/ijerph16152652





