Using a Clustering Approach to Investigate Socio-Environmental Inequality in Preterm Birth—A Study Conducted at Fine Spatial Scale in Paris (France)
Abstract
:1. Introduction
2. Materials
2.1. Study Area
2.2. Health Data: Preterm Birth
2.3. Air pollution: Nitrogen Dioxide (NO2)
2.4. Socioeconomic Deprivation Index
3. Methods
3.1. Spatial Methodology
3.2. Analytical Strategy and Results Interpretation
- When a significant most-likely cluster (with p < 0.05) was detected, the next step consist in taking into account the neighborhood characteristics to see whether or not the significant cluster can be explained by them. Spatial analyses were structured in four successive steps: A crude (unadjusted) analysis, to identify and localize the most-likely cluster of high risk of PTB.
- An adjusted analysis for NO2 concentrations
- An adjusted analysis for socioeconomic deprivation index
- One final adjusted analysis for air pollution and socioeconomic deprivation index including interaction between the two variables.
4. Results
4.1. Description of the Population
4.2. Neighborhood Socio-Economic Deprivation, NO2 Ambient Air Concentrations and Spatial Distribution of PTB in Paris
5. Discussion
- (i)
- (ii)
- (iii)
- (i)
- The first mechanisms—vulnerability differential—could explain the greater susceptibility to NO2 exposure of women living in the most deprived neighborhoods. Several studies demonstrated that people with a lower socio-economic status may be more vulnerable to the health effects of proximity to road, air pollution and noise exposure because they experience poorer health due to their economic and psychosocial conditions [15]. Living in communities with lower household income and education levels would also tend to increase vulnerability level to air pollution [102].
- (ii)
- The second mechanism—combined vulnerability differential with exposure differential—may explain the greater susceptibility to NO2 exposure of women living in the deprived neighborhood. Although a majority of studies have found that people living in the most deprived neighborhoods may be more vulnerable to environmental nuisances, some authors have hypothesized that those living in middle deprived neighborhoods may have also a particular vulnerability. In this context, high NO2 exposure may act on this particular sensitive subpopulation, as an exacerbating factor, which, in combination with unfavorable living conditions, could generate greater health effects than in the rest of the population. The assumption of a synergy of differential exposure and vulnerability to explain our findings therefore seems highly probable.
Strengths and Limitations
- -
- Health data: the advantage of the data used in our study is the rate of completeness of the data which reach 93% on average and the large population size, resulting in a small variability of our estimates [107]. To our knowledge, this is the first French study investigate at fine spatial scale the birth certificates which list all birth in Paris during our study period.
- -
- Modeled air pollution data: the air pollutant modeling procedure used provides unbiased estimates of exposure to ambient air pollution at census block level. This type of model was validated by Jerrett et al. who demonstrated its effectiveness and reliability [108].
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Terzidou, V.; Bennett, P.R. Preterm labour. Curr. Opin. Obstet. Gynecol. 2002, 14, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Hack, M.; Klein, N.K.; Taylor, H.G. Long-term developmental outcomes of low birth weight infants. Future Child 1995, 5, 176–196. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.S.; Inskip, H.M.; Godfrey, K.M.; Foreman, C.T.; Warner, J.O.; Gregson, R.K.; Clough, J.B. Small size at birth and greater postnatal weight gain: relationships to diminished infant lung function. Am. J. Respir. Crit. Care Med. 2004, 170, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Barker, D.J.; Gluckman, P.D.; Godfrey, K.M.; Harding, J.E.; Owens, J.A.; Robinson, J.S. Fetal nutrition and cardiovascular disease in adult life. Lancet 1993, 341, 938–941. [Google Scholar] [CrossRef]
- Mathews, T.J.; MacDorman, M.F. Infant mortality statistics from the 2005 period linked birth/infant death data set. Natl. Vital Stat. Rep. 2008, 57, 1–32. [Google Scholar] [PubMed]
- Kramer, M.S.; Demissie, K.; Yang, H.; Platt, R.W.; Sauvé, R.; Liston, R. The contribution of mild and moderate preterm birth to infant mortality. Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. JAMA 2000, 284, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Leem, J.-H.; Kaplan, B.M.; Shim, Y.K.; Pohl, H.R.; Gotway, C.A.; Bullard, S.M.; Rogers, J.F.; Smith, M.M.; Tylenda, C.A. Exposures to Air Pollutants during Pregnancy and Preterm Delivery. Environ. Health Perspect. 2006, 114, 905–910. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathews, T.J.; MacDorman, M.F. Infant mortality statistics from the 2004 period linked birth/infant death data set. Natl. Vital Stat. Rep. 2007, 55, 1–32. [Google Scholar] [PubMed]
- Hutchinson, E.A.; De Luca, C.R.; Doyle, L.W.; Roberts, G.; Anderson, P.J. Victorian Infant Collaborative Study Group School-age outcomes of extremely preterm or extremely low birth weight children. Pediatrics 2013, 131, e1053–e1061. [Google Scholar] [CrossRef] [PubMed]
- Proietti, E.; Röösli, M.; Frey, U.; Latzin, P. Air pollution during pregnancy and neonatal outcome: a review. J. Aerosol. Med. Pulm. Drug Deliv. 2013, 26, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.S.; Balkhair, T.; Knowledge Synthesis Group on Determinants of Preterm/LBW births. Air pollution and birth outcomes: A systematic review. Environ. Int. 2011, 37, 498–516. [Google Scholar] [CrossRef] [PubMed]
- Stieb, D.M.; Chen, L.; Eshoul, M.; Judek, S. Ambient air pollution, birth weight and preterm birth: A systematic review and meta-analysis. Environ. Res. 2012, 117, 100–111. [Google Scholar] [CrossRef] [PubMed]
- Bonzini, M.; Carugno, M.; Grillo, P.; Mensi, C.; Bertazzi, P.A.; Pesatori, A.C. Impact of ambient air pollution on birth outcomes: systematic review of the current evidences. Med. Lav. 2010, 101, 341–363. [Google Scholar] [PubMed]
- Wu, J.; Wilhelm, M.; Chung, J.; Ritz, B. Comparing exposure assessment methods for traffic-related air pollution in an adverse pregnancy outcome study. Environ. Res. 2011, 111, 685–692. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miranda, M.L.; Edwards, S.E.; Chang, H.H.; Auten, R.L. Proximity to roadways and pregnancy outcomes. J. Expo. Sci. Environ. Epidemiol. 2013, 23, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; Bobb, J.F.; Ito, K.; Savitz, D.A.; Elston, B.; Shmool, J.L.C.; Dominici, F.; Ross, Z.; Clougherty, J.E.; Matte, T. Ambient Fine Particulate Matter, Nitrogen Dioxide, and Preterm Birth in New York City. Environ. Health Perspect. 2016, 124, 1283–1290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nieuwenhuijsen, M.J.; Dadvand, P.; Grellier, J.; Martinez, D.; Vrijheid, M. Environmental risk factors of pregnancy outcomes: A summary of recent meta-analyses of epidemiological studies. Environ. Health 2013, 12, 6. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, C.; Nieuwenhuijsen, M.J.; Gallus, S.; Cipriani, S.; La Vecchia, C.; Parazzini, F. Ambient particulate matter and preterm birth or birth weight: A review of the literature. Arch. Toxicol. 2010, 84, 447–460. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.H.; Reich, B.J.; Miranda, M.L. Time-to-event analysis of fine particle air pollution and preterm birth: Results from North Carolina, 2001-2005. Am. J. Epidemiol. 2012, 175, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Gehring, U.; Wijga, A.H.; Fischer, P.; de Jongste, J.C.; Kerkhof, M.; Koppelman, G.H.; Smit, H.A.; Brunekreef, B. Traffic-related air pollution, preterm birth and term birth weight in the PIAMA birth cohort study. Environ. Res. 2011, 111, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.; Neller, A.; Williams, G.; Simpson, R. Maternal exposure to low levels of ambient air pollution and preterm birth in Brisbane, Australia. BJOG 2006, 113, 935–941. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghio, A.J.; Carraway, M.S.; Madden, M.C. Composition of air pollution particles and oxidative stress in cells, tissues, and living systems. J. Toxicol. Environ. Health B Crit. Rev. 2012, 15, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; Sheppard, L.; Clyde, M. Health Effects of Air Pollution: A Statistical Review. Int. Stat. Rev. 2003, 71, 243–276. [Google Scholar] [CrossRef]
- Šrám, R.J.; Binková, B.; Dejmek, J.; Bobak, M. Ambient Air Pollution and Pregnancy Outcomes: A Review of the Literature. Environ. Health Perspect. 2005, 113, 375–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strickland, M.J.; Klein, M.; Darrow, L.A.; Flanders, W.D.; Correa, A.; Marcus, M.; Tolbert, P.E. The Issue of Confounding in Epidemiological Studies of Ambient Air Pollution and Pregnancy Outcomes. J. Epidemiol. Community Health 2009, 63, 500–504. [Google Scholar] [CrossRef] [PubMed]
- Sexton, K.; Gong, H.; Bailar, J.C.; Ford, J.G.; Gold, D.R.; Lambert, W.E.; Utell, M.J. Air pollution health risks: Do class and race matter? Toxicol. Ind. Health 1993, 9, 843–878. [Google Scholar] [CrossRef] [PubMed]
- Yi, O.; Kim, H.; Ha, E. Does area level socioeconomic status modify the effects of PM10 on preterm delivery? Environ. Res. 2010, 110, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Salihu, H.M.; Ghaji, N.; Mbah, A.K.; Alio, A.P.; August, E.M.; Boubakari, I. Particulate pollutants and racial/ethnic disparity in feto-infant morbidity outcomes. Matern. Child Health J. 2012, 16, 1679–1687. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, T.J.; Parker, J.D.; Kyle, A.D.; Schoendorf, K.C. Disparities in exposure to air pollution during pregnancy. Environ. Health Perspect. 2003, 111, 942–946. [Google Scholar] [CrossRef] [PubMed]
- Ponce, N.A.; Hoggatt, K.J.; Wilhelm, M.; Ritz, B. Preterm Birth: The Interaction of Traffic-related Air Pollution with Economic Hardship in Los Angeles Neighborhoods. Am. J. Epidemiol. 2005, 162, 140–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carbajal-Arroyo, L.; Miranda-Soberanis, V.; Medina-Ramón, M.; Rojas-Bracho, L.; Tzintzun, G.; Solís-Gutiérrez, P.; Méndez-Ramírez, I.; Hurtado-Díaz, M.; Schwartz, J.; Romieu, I. Effect of PM(10) and O(3) on infant mortality among residents in the Mexico City Metropolitan Area: A case-crossover analysis, 1997–2005. J. Epidemiol. Community Health 2011, 65, 715–721. [Google Scholar] [CrossRef] [PubMed]
- OECD ENV/EPOC/WPNEP. Rapport Environment and Distributional Issues: Analysis, Evidence and Policy Implications; OECD Publishing: Paris, France, 2004. [Google Scholar]
- Bloch, J.R. Using Geographical Information Systems to Explore Disparities in Preterm Birth Rates among Foreign-born and U.S.-born Black Mothers. J. Obstet. Gynecol. Neonatal. Nurs. 2011, 40, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Ogneva-Himmelberger, Y.; Dahlberg, T.; Kelly, K.; Simas, T.A.M. Using Geographic Information Science to Explore Associations between Air Pollution, Environmental Amenities, and Preterm Births. AIMS Public Health 2015, 2, 469–486. [Google Scholar] [CrossRef] [PubMed]
- Cockings, S.; Martin, D. Zone design for environment and health studies using pre-aggregated data. Soc. Sci. Med. 2005, 60, 2729–2742. [Google Scholar] [CrossRef] [PubMed]
- Haynes, R.; Daras, K.; Reading, R.; Jones, A. Modifiable neighbourhood units, zone design and residents’ perceptions. Health Place 2007, 13, 812–825. [Google Scholar] [CrossRef] [PubMed]
- Insaf, T.Z.; Talbot, T. Identifying areas at risk of low birth weight using spatial epidemiology: A small area surveillance study. Prev. Med. 2016, 88, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Sabel, C.E.; Wilson, J.G.; Kingham, S.; Tisch, C.; Epton, M. Spatial implications of covariate adjustment on patterns of risk: Respiratory hospital admissions in Christchurch, New Zealand. Soc. Sci. Med. 2007, 65, 43–59. [Google Scholar] [CrossRef] [PubMed]
- Kihal-Talantikite, W.; Deguen, S.; Padilla, C.; Siebert, M.; Couchoud, C.; Vigneau, C.; Bayat, S. Spatial distribution of end-stage renal disease (ESRD) and social inequalities in mixed urban and rural areas: A study in the Bretagne administrative region of France. Clin. Kidney J. 2015, 8, 7–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ncube, C.N.; Enquobahrie, D.A.; Albert, S.M.; Herrick, A.L.; Burke, J.G. Association of neighborhood context with offspring risk of preterm birth and low birthweight: A systematic review and meta-analysis of population-based studies. Soc. Sci. Med. 2016, 153, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Vos, A.A.; Posthumus, A.G.; Bonsel, G.J.; Steegers, E.A.P.; Denktaş, S. Deprived neighborhoods and adverse perinatal outcome: A systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 2014, 93, 727–740. [Google Scholar] [CrossRef] [PubMed]
- WHO. Preterm Birth. Available online: http://www.who.int/news-room/fact-sheets/detail/preterm-birth (accessed on 7 August 2018).
- Quinn, J.-A.; Munoz, F.M.; Gonik, B.; Frau, L.; Cutland, C.; Mallett-Moore, T.; Kissou, A.; Wittke, F.; Das, M.; Nunes, T.; et al. Preterm birth: Case definition & guidelines for data collection, analysis, and presentation of immunisation safety data. Vaccine 2016, 34, 6047–6056. [Google Scholar] [CrossRef] [PubMed]
- Vardoulakis, S.; Fisher, B.E.A.; Pericleous, K.; Gonzalez-Flesca, N. Modelling air quality in street canyons: A review. Atmos. Environ. 2003, 37, 155–182. [Google Scholar] [CrossRef]
- Wahida, K.-T.; Padilla, C.M.; Denis, Z.-N.; Olivier, B.; Géraldine, L.N.; Philippe, Q.; Séverine, D. A Conceptual Framework for the Assessment of Cumulative Exposure to Air Pollution at a Fine Spatial Scale. Int. J. Environ. Res. Public Health 2016, 13, 319. [Google Scholar] [CrossRef] [PubMed]
- Deguen, S.; Petit, C.; Delbarre, A.; Kihal, W.; Padilla, C.; Benmarhnia, T.; Lapostolle, A.; Chauvin, P.; Zmirou-Navier, D. Neighbourhood Characteristics and Long-Term Air Pollution Levels Modify the Association between the Short-Term Nitrogen Dioxide Concentrations and All-Cause Mortality in Paris. PLoS ONE 2015, 10, e0131463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padilla, C.M.; Kihal-Talantikit, W.; Vieira, V.M.; Deguen, S. City-Specific Spatiotemporal Infant and Neonatal Mortality Clusters: Links with Socioeconomic and Air Pollution Spatial Patterns in France. Int. J. Environ. Res. Public Health 2016, 13, 624. [Google Scholar] [CrossRef] [PubMed]
- Levy, I.; Mihele, C.; Lu, G.; Narayan, J.; Brook, J.R. Evaluating Multipollutant Exposure and Urban Air Quality: Pollutant Interrelationships, Neighborhood Variability, and Nitrogen Dioxide as a Proxy Pollutant. Environ. Health Perspect. 2014, 122, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Ritz, B.; Wilhelm, M. Ambient Air Pollution and Adverse Birth Outcomes: Methodologic Issues in an Emerging Field. Basic Clin. Pharmacol. Toxicol. 2008, 102, 182–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brauer, M.; Lencar, C.; Tamburic, L.; Koehoorn, M.; Demers, P.; Karr, C. A Cohort Study of Traffic-Related Air Pollution Impacts on Birth Outcomes. Environ. Health Perspect. 2008, 116, 680–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Darrow, L.A.; Klein, M.; Flanders, W.D.; Waller, L.A.; Correa, A.; Marcus, M.; Mulholland, J.A.; Russell, A.G.; Tolbert, P.E. Ambient air pollution and preterm birth: A time-series analysis. Epidemiology 2009, 20, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Lalloué, B.; Monnez, J.-M.; Padilla, C.; Kihal, W.; Le Meur, N.; Zmirou-Navier, D.; Deguen, S. A statistical procedure to create a neighborhood socioeconomic index for health inequalities analysis. Int. J. Equity Health 2013, 12, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kihal-Talantikite, W.; Padilla, C.M.; Lalloué, B.; Gelormini, M.; Zmirou-Navier, D.; Deguen, S. Green space, social inequalities and neonatal mortality in France. BMC Pregnancy Childbirth 2013, 13, 191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kihal-Talantikite, W.; Padilla, C.M.; Lalloue, B.; Rougier, C.; Defrance, J.; Zmirou-Navier, D.; Deguen, S. An exploratory spatial analysis to assess the relationship between deprivation, noise and infant mortality: An ecological study. Environ. Health 2013, 12, 109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padilla, C.M.; Deguen, S.; Lalloue, B.; Blanchard, O.; Beaugard, C.; Troude, F.; Navier, D.Z.; Vieira, V.M. Cluster analysis of social and environment inequalities of infant mortality. A spatial study in small areas revealed by local disease mapping in France. Sci. Total Environ. 2013, 454–455, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Kulldorff, M. SaTScan: Software for the Spatial, Temporal, and Space-Time Scan Statistics, version 6.0; Information Management Services, Inc.: Rockville, MD, USA, 2005. [Google Scholar]
- Kulldorff, M.; Feuer, E.J.; Miller, B.A.; Freedman, L.S. Breast cancer clusters in the northeast United States: A geographic analysis. Am. J. Epidemiol. 1997, 146, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Kulldorff, M. A spatial scan statistic. Commun. Stat. Theory Methods 1997, 26, 1481–1496. [Google Scholar] [CrossRef]
- Dwass, M. Modified Randomization Tests for Nonparametric Hypotheses. Ann. Math. Stat. 1957, 28, 181–187. [Google Scholar] [CrossRef]
- Padula, A.M.; Mortimer, K.M.; Tager, I.B.; Hammond, S.K.; Lurmann, F.W.; Yang, W.; Stevenson, D.K.; Shaw, G.M. Traffic-related air pollution and risk of preterm birth in the San Joaquin Valley of California. Ann. Epidemiol. 2014, 24, 888–895.e4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dadvand, P.; Basagaña, X.; Figueras, F.; Martinez, D.; Beelen, R.; Cirach, M.; de Nazelle, A.; Hoek, G.; Ostro, B.; Nieuwenhuijsen, M.J. Air pollution and preterm premature rupture of membranes: A spatiotemporal analysis. Am. J. Epidemiol. 2014, 179, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, M.; Ghosh, J.K.; Su, J.; Cockburn, M.; Jerrett, M.; Ritz, B. Traffic-related air toxics and preterm birth: A population-based case-control study in Los Angeles County, California. Environ. Health 2011, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Liang, Z.; Tao, S.; Zhu, J.; Du, Y. Effects of air pollution on neonatal prematurity in Guangzhou of China: A time-series study. Environ. Health 2011, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Hannam, K.; McNamee, R.; Baker, P.; Sibley, C.; Agius, R. Air pollution exposure and adverse pregnancy outcomes in a large UK birth cohort: Use of a novel spatio-temporal modelling technique. Scand. J. Work Environ. Health 2014, 40, 518–530. [Google Scholar] [CrossRef] [PubMed]
- Gehring, U.; Tamburic, L.; Sbihi, H.; Davies, H.W.; Brauer, M. Impact of noise and air pollution on pregnancy outcomes. Epidemiology 2014, 25, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Schifano, P.; Lallo, A.; Asta, F.; De Sario, M.; Davoli, M.; Michelozzi, P. Effect of ambient temperature and air pollutants on the risk of preterm birth, Rome 2001–2010. Environ. Int. 2013, 61, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Le, H.Q.; Batterman, S.A.; Wirth, J.J.; Wahl, R.L.; Hoggatt, K.J.; Sadeghnejad, A.; Hultin, M.L.; Depa, M. Air pollutant exposure and preterm and term small-for-gestational-age births in Detroit, Michigan: Long-term trends and associations. Environ. Int. 2012, 44, 7–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van den Hooven, E.H.; Pierik, F.H.; de Kluizenaar, Y.; Willemsen, S.P.; Hofman, A.; van Ratingen, S.W.; Zandveld, P.Y.J.; Mackenbach, J.P.; Steegers, E.A.P.; Miedema, H.M.E.; et al. Air pollution exposure during pregnancy, ultrasound measures of fetal growth, and adverse birth outcomes: A prospective cohort study. Environ. Health Perspect. 2012, 120, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Estarlich, M.; Ballester, F.; Davdand, P.; Llop, S.; Esplugues, A.; Fernández-Somoano, A.; Lertxundi, A.; Guxens, M.; Basterrechea, M.; Tardón, A.; et al. Exposure to ambient air pollution during pregnancy and preterm birth: A Spanish multicenter birth cohort study. Environ. Res. 2016, 147, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Généreux, M.; Auger, N.; Goneau, M.; Daniel, M. Neighbourhood socioeconomic status, maternal education and adverse birth outcomes among mothers living near highways. J. Epidemiol. Community Health 2008, 62, 695–700. [Google Scholar] [CrossRef] [PubMed]
- Yorifuji, T.; Naruse, H.; Kashima, S.; Ohki, S.; Murakoshi, T.; Takao, S.; Tsuda, T.; Doi, H. Residential proximity to major roads and preterm births. Epidemiology 2011, 22, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Yorifuji, T.; Naruse, H.; Kashima, S.; Takao, S.; Murakoshi, T.; Doi, H.; Kawachi, I. Residential proximity to major roads and adverse birth outcomes: A hospital-based study. Environ. Health 2013, 12, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yorifuji, T.; Naruse, H.; Kashima, S.; Murakoshi, T.; Doi, H. Residential proximity to major roads and obstetrical complications. Sci. Total Environ. 2015, 508, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-Y.; Chang, C.-C.; Chuang, H.-Y.; Ho, C.-K.; Wu, T.-N.; Tsai, S.-S. Evidence for increased risks of preterm delivery in a population residing near a freeway in Taiwan. Arch. Environ. Health 2003, 58, 649–654. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, M.; Ritz, B. Residential proximity to traffic and adverse birth outcomes in Los Angeles county, California, 1994–1996. Environ. Health Perspect. 2003, 111, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Vadillo-Ortega, F.; Osornio-Vargas, A.; Buxton, M.A.; Sánchez, B.N.; Rojas-Bracho, L.; Viveros-Alcaráz, M.; Castillo-Castrejón, M.; Beltrán-Montoya, J.; Brown, D.G.; O’Neill, M.S. Air pollution, inflammation and preterm birth: A potential mechanistic link. Med. Hypotheses 2014, 82, 219–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sapkota, A.; Chelikowsky, A.P.; Nachman, K.E.; Cohen, A.J.; Ritz, B. Exposure to particulate matter and adverse birth outcomes: A comprehensive review and meta-analysis. Air Qual. Atmos. Health 2012, 5, 369–381. [Google Scholar] [CrossRef]
- Longini, M.; Perrone, S.; Vezzosi, P.; Marzocchi, B.; Kenanidis, A.; Centini, G.; Rosignoli, L.; Buonocore, G. Association between oxidative stress in pregnancy and preterm premature rupture of membranes. Clin. Biochem. 2007, 40, 793–797. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.-C.; Wilkins, R.; Kramer, M.S.; Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. Effect of neighbourhood income and maternal education on birth outcomes: A population-based study. CMAJ 2006, 174, 1415–1420. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.-C.; Kierans, W.J.; Wilkins, R.; Liston, R.M.; Mohamed, J.; Kramer, M.S.; British Columbia Vital Statistics Agency. Disparities in birth outcomes by neighborhood income: Temporal trends in rural and urban areas, British Columbia. Epidemiology 2004, 15, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Agyemang, C.; Vrijkotte, T.G.M.; Droomers, M.; van der Wal, M.F.; Bonsel, G.J.; Stronks, K. The effect of neighbourhood income and deprivation on pregnancy outcomes in Amsterdam, The Netherlands. J. Epidemiol. Community Health 2009, 63, 755–760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, N.; Wen, S.W.; Katherine, W.; Bottomley, J.; Yang, Q.; Walker, M.C. Neighbourhood family income and adverse birth outcomes among singleton deliveries. J. Obstet. Gynaecol. Can. 2010, 32, 1042–1048. [Google Scholar] [CrossRef]
- Urquia, M.L.; Frank, J.W.; Glazier, R.H.; Moineddin, R. Birth outcomes by neighbourhood income and recent immigration in Toronto. Health Rep. 2007, 18, 21–30. [Google Scholar] [PubMed]
- Garcia-Subirats, I.; Pérez, G.; Rodríguez-Sanz, M.; Ruiz-Muñoz, D.; Muñoz, D.R.; Salvador, J. Neighborhood inequalities in adverse pregnancy outcomes in an urban setting in Spain: A multilevel approach. J. Urban Health 2012, 89, 447–463. [Google Scholar] [CrossRef] [PubMed]
- Janghorbani, M.; Stenhouse, E.; Millward, A.; Jones, R.B. Neighborhood deprivation and preterm birth in Plymouth, UK. J. Matern. Fetal. Neonatal. Med. 2006, 19, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.; Bonellie, S.R.; Chalmers, J.; Greer, I.; Jarvis, S.; Williams, C. Social inequalities in preterm birth in Scotland 1980–2003: Findings from an area-based measure of deprivation. BJOG 2008, 115, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.K.; Draper, E.S.; Manktelow, B.N.; Field, D.J. Socioeconomic inequalities in survival and provision of neonatal care: Population based study of very preterm infants. BMJ 2009, 339, b4702. [Google Scholar] [CrossRef] [PubMed]
- Janevic, T.; Stein, C.R.; Savitz, D.A.; Kaufman, J.S.; Mason, S.M.; Herring, A.H. Neighborhood deprivation and adverse birth outcomes among diverse ethnic groups. Ann. Epidemiol. 2010, 20, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Robinson, D.; Agarwal, U.; Diggle, P.J.; Platt, M.J.; Yoxall, B.; Alfirevic, Z. Quantifying the impact of deprivation on preterm births: A retrospective cohort study. PLoS ONE 2011, 6, e23163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buka, S.L.; Brennan, R.T.; Rich-Edwards, J.W.; Raudenbush, S.W.; Earls, F. Neighborhood support and the birth weight of urban infants. Am. J. Epidemiol. 2003, 157, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Schempf, A.; Strobino, D.; O’Campo, P. Neighborhood Effects on Birthweight: An Exploration of Psychosocial and Behavioral Pathways in Baltimore, 1995–1996. Soc. Sci. Med. 2009, 68, 100–110. [Google Scholar] [CrossRef] [PubMed]
- Nkansah-Amankra, S.; Luchok, K.J.; Hussey, J.R.; Watkins, K.; Liu, X. Effects of maternal stress on low birth weight and preterm birth outcomes across neighborhoods of South Carolina, 2000–2003. Matern. Child Health J. 2010, 14, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, E.A.; Robinson, E.; Clark, P.M.; Becroft, D.M.O.; Glavish, N.; Pattison, N.S.; Pryor, J.E.; Thompson, J.M.D.; Wild, C.J. Maternal nutritional risk factors for small for gestational age babies in a developed country: A case-control study. Arch. Dis. Child. Fetal Neonatal Ed. 2004, 89, F431–F435. [Google Scholar] [CrossRef] [PubMed]
- Kozuki, N.; Lee, A.C.C.; Black, R.E.; Katz, J. Nutritional and Reproductive Risk Factors for Small for Gestational Age and Preterm Births. Nestle Nutr. Inst. Works. Ser. 2015, 81, 17–28. [Google Scholar] [CrossRef]
- Patra, J.; Bakker, R.; Irving, H.; Jaddoe, V.W.V.; Malini, S.; Rehm, J. Dose-response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA)—A systematic review and meta-analyses. BJOG 2011, 118, 1411–1421. [Google Scholar] [CrossRef] [PubMed]
- Northstone, K.; Emmett, P.; Rogers, I. Dietary patterns in pregnancy and associations with socio-demographic and lifestyle factors. Eur. J. Clin. Nutr. 2008, 62, 471–479. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, C.M.; Nassar, N.; Kurinczuk, J.J.; Bower, C. The effect of maternal alcohol consumption on fetal growth and preterm birth. BJOG 2009, 116, 390–400. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, V.C.-R.; Shieh, S.-H.; Chen, C.-Y.; Liou, S.-H.; Hsiao, Y.-C.; Wu, T.-N. Does Social Health Insurance Close the Gap: The Case of Socioeconomic Status and Preterm Low-Birth-Weight Survival. Asia Pac. J. Public Health 2015, 27, 497–508. [Google Scholar] [CrossRef] [PubMed]
- Timmermans, S.; Bonsel, G.J.; Steegers-Theunissen, R.P.M.; Mackenbach, J.P.; Steyerberg, E.W.; Raat, H.; Verbrugh, H.A.; Tiemeier, H.W.; Hofman, A.; Birnie, E.; et al. Individual accumulation of heterogeneous risks explains perinatal inequalities within deprived neighbourhoods. Eur. J. Epidemiol. 2011, 26, 165–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hodgson, E.J.; Lockwood, C.J. Preterm Birth: A Complex Disease. In Preterm Birth; Wiley-Blackwell: Oxford, UK, 2010; pp. 8–16. [Google Scholar]
- Hao, H.; Chang, H.H.; Holmes, H.A.; Mulholland, J.A.; Klein, M.; Darrow, L.A.; Strickland, M.J. Air Pollution and Preterm Birth in the U.S. State of Georgia (2002–2006): Associations with Concentrations of 11 Ambient Air Pollutants Estimated by Combining Community Multiscale Air Quality Model (CMAQ) Simulations with Stationary Monitor Measurements. Environ. Health Perspect. 2016, 124, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Cakmak, S.; Hebbern, C.; Cakmak, J.D.; Vanos, J. The modifying effect of socioeconomic status on the relationship between traffic, air pollution and respiratory health in elementary schoolchildren. J. Environ. Manag. 2016, 177, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Clark, L.P.; Millet, D.B.; Marshall, J.D. National Patterns in Environmental Injustice and Inequality: Outdoor NO2 Air Pollution in the United States. PLoS ONE 2014, 9, e94431. [Google Scholar] [CrossRef] [PubMed]
- Tian, N.; Xue, J.; Barzyk, T.M. Evaluating socioeconomic and racial differences in traffic-related metrics in the United States using a GIS approach. J. Expo. Sci. Environ. Epidemiol. 2013, 23, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Clougherty, J.E.; Kubzansky, L.D. A Framework for Examining Social Stress and Susceptibility to Air Pollution in Respiratory Health. Environ. Health Perspect. 2009, 117, 1351–1358. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandoli, G.; von Ehrenstein, O.; Ghosh, J.K.; Ritz, B. Synergistic effects of air pollution and psychosocial stressors on adolescent lung function. J. Allergy Clin. Immunol. 2016, 138, 918–920.e4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Premiers Certificats de Santé des Enfants nés en 2010 et Domiciliés en Île-de-France—Observatoire Régional de Santé Île-de-France—15 rue Falguière 75015 Paris—Tel.: 01 77 49 78 60—ors-idf@ors-idf.org. Available online: http://www.erpurs.org/index.php/fr/publications/56-groupes-de-population/meres-et-enfants/87-premiers-certificats-de-sante-des-enfants-nes-en-2010-et-domicilies-en-ile-de-france (accessed on 17 July 2018).
- Jerrett, M.; Gale, S.; Kontgis, C. Spatial modeling in environmental and public health research. Int. J. Environ. Res. Public Health 2010, 7, 1302–1329. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S. Ecologic versus individual-level sources of bias in ecologic estimates of contextual health effects. Int. J. Epidemiol. 2001, 30, 1343–1350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krieger, N.; Williams, D.R.; Moss, N.E. Measuring social class in US public health research: Concepts, methodologies, and guidelines. Annu. Rev. Public Health 1997, 18, 341–378. [Google Scholar] [CrossRef] [PubMed]
- Miranda, M.L.; Maxson, P.; Edwards, S. Environmental contributions to disparities in pregnancy outcomes. Epidemiol. Rev. 2009, 31, 67–83. [Google Scholar] [CrossRef] [PubMed]
- De Graaf, J.P.; Steegers, E.A.P.; Bonsel, G.J. Inequalities in perinatal and maternal health. Curr. Opin. Obstet. Gynecol. 2013, 25, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Beltran, A.J.; Wu, J.; Laurent, O. Associations of meteorology with adverse pregnancy outcomes: A systematic review of preeclampsia, preterm birth and birth weight. Int. J. Environ. Res. Public Health 2013, 11, 91–172. [Google Scholar] [CrossRef] [PubMed]
- Airparif. Inventaire Régional des Emissions en Ile-de-France—Année de Référence 2012. Available online: https://www.airparif.asso.fr/_pdf/publications/inventaire-emissions-idf-2012-150121.pdf,%22 (accessed on 9 August 2018).
- Benmarhnia, T.; Kihal-Talantikite, W.; Ragettli, M.S.; Deguen, S. Small-area spatiotemporal analysis of heatwave impacts on elderly mortality in Paris: A cluster analysis approach. Sci. Total Environ. 2017, 592, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Lalloué, B.; Monnez, J.-M.; Padilla, C.; Kihal, W.; Zmirou-Navier, D.; Deguen, S. Data analysis techniques: A tool for cumulative exposure assessment. J. Expo. Sci. Environ. Epidemiol. 2015, 25, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Burton-Jeangros, C.; Cullati, S.; Sacker, A.; Blane, D. (Eds.) A Life Course Perspective on Health Trajectories and Transitions; Life Course Research and Social Policies; Springer International Publishing: Cham, Switzherland, 2015; ISBN 978-3-319-20483-3. [Google Scholar]


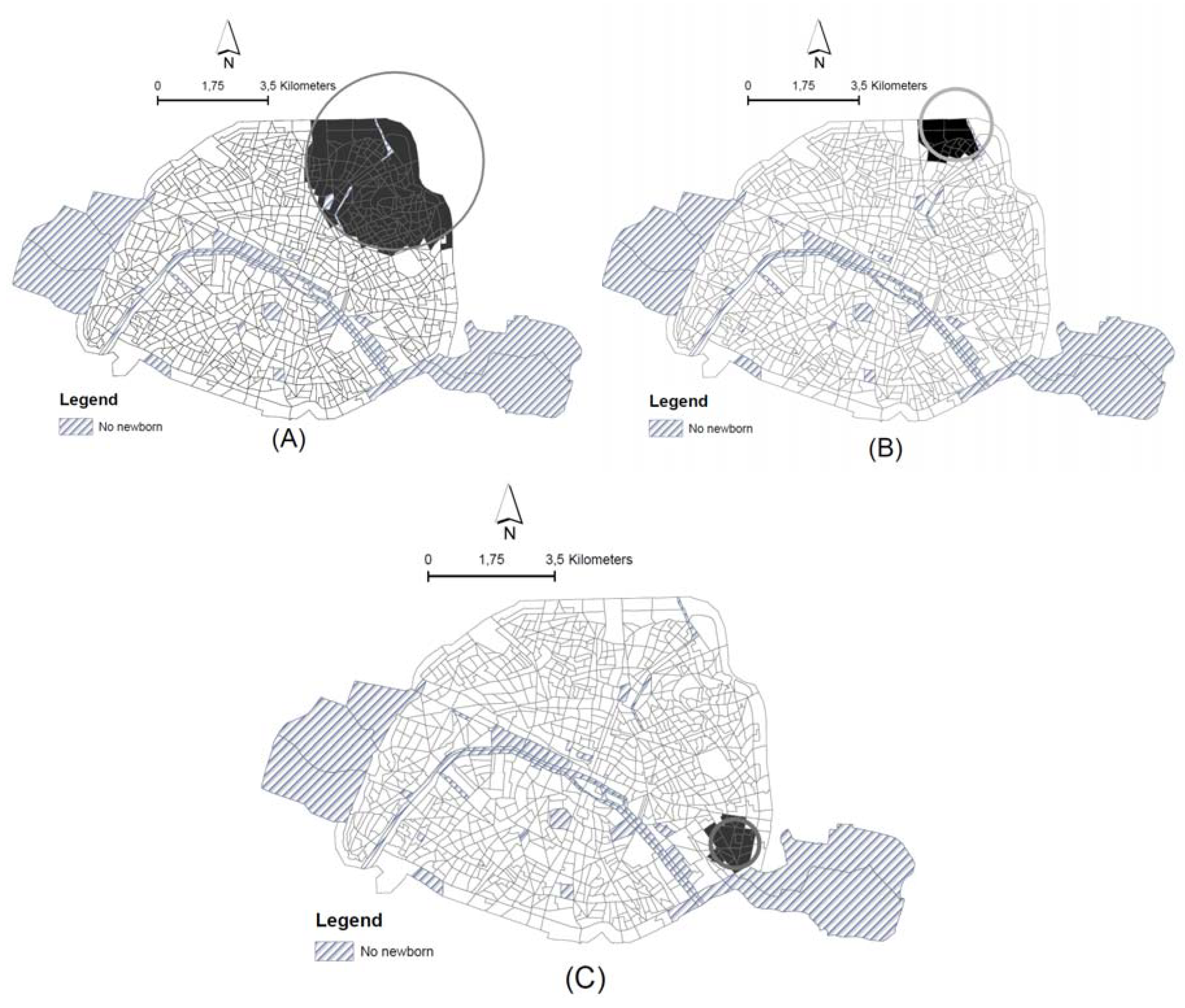
| Analysis | Control Variables | Cluster Radius | No of Census Blocks/No. of Birth in the Cluster | No of Expected Cases | No. of Observed Cases | RR | LLr | Shift | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted a | |||||||||
| No adjustment | 2816.01 | 169/25,503 | 1179.94 | 1310 | 1.15 | 9.23 | - | 0.06 | |
| Adjusted b | |||||||||
| 1 Annual concentration of NO2 | 1125.2 | 17/2814 | 130.84 | 181 | 1.40 | 8.84 | Same zone | 0.08 | |
| SES c index | 673.67 | 19/2396 | 104.95 | 140 | 1.34 | 5.42 | Yes | 0.81 | |
| NO2 and SES level | 673.67 | 19/2396 | 106.95 | 140 | 1.32 | 4.76 | Yes | 0.97 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deguen, S.; Ahlers, N.; Gilles, M.; Danzon, A.; Carayol, M.; Zmirou-Navier, D.; Kihal-Talantikite, W. Using a Clustering Approach to Investigate Socio-Environmental Inequality in Preterm Birth—A Study Conducted at Fine Spatial Scale in Paris (France). Int. J. Environ. Res. Public Health 2018, 15, 1895. https://doi.org/10.3390/ijerph15091895
Deguen S, Ahlers N, Gilles M, Danzon A, Carayol M, Zmirou-Navier D, Kihal-Talantikite W. Using a Clustering Approach to Investigate Socio-Environmental Inequality in Preterm Birth—A Study Conducted at Fine Spatial Scale in Paris (France). International Journal of Environmental Research and Public Health. 2018; 15(9):1895. https://doi.org/10.3390/ijerph15091895
Chicago/Turabian StyleDeguen, Severine, Nina Ahlers, Morgane Gilles, Arlette Danzon, Marion Carayol, Denis Zmirou-Navier, and Wahida Kihal-Talantikite. 2018. "Using a Clustering Approach to Investigate Socio-Environmental Inequality in Preterm Birth—A Study Conducted at Fine Spatial Scale in Paris (France)" International Journal of Environmental Research and Public Health 15, no. 9: 1895. https://doi.org/10.3390/ijerph15091895
APA StyleDeguen, S., Ahlers, N., Gilles, M., Danzon, A., Carayol, M., Zmirou-Navier, D., & Kihal-Talantikite, W. (2018). Using a Clustering Approach to Investigate Socio-Environmental Inequality in Preterm Birth—A Study Conducted at Fine Spatial Scale in Paris (France). International Journal of Environmental Research and Public Health, 15(9), 1895. https://doi.org/10.3390/ijerph15091895




