Heterogeneous Trajectories of Physical and Mental Health in Late Middle Age: Importance of Life-Course Socioeconomic Positions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data and Sample
2.2. Measures
2.3. Statistical Analyses
3. Results
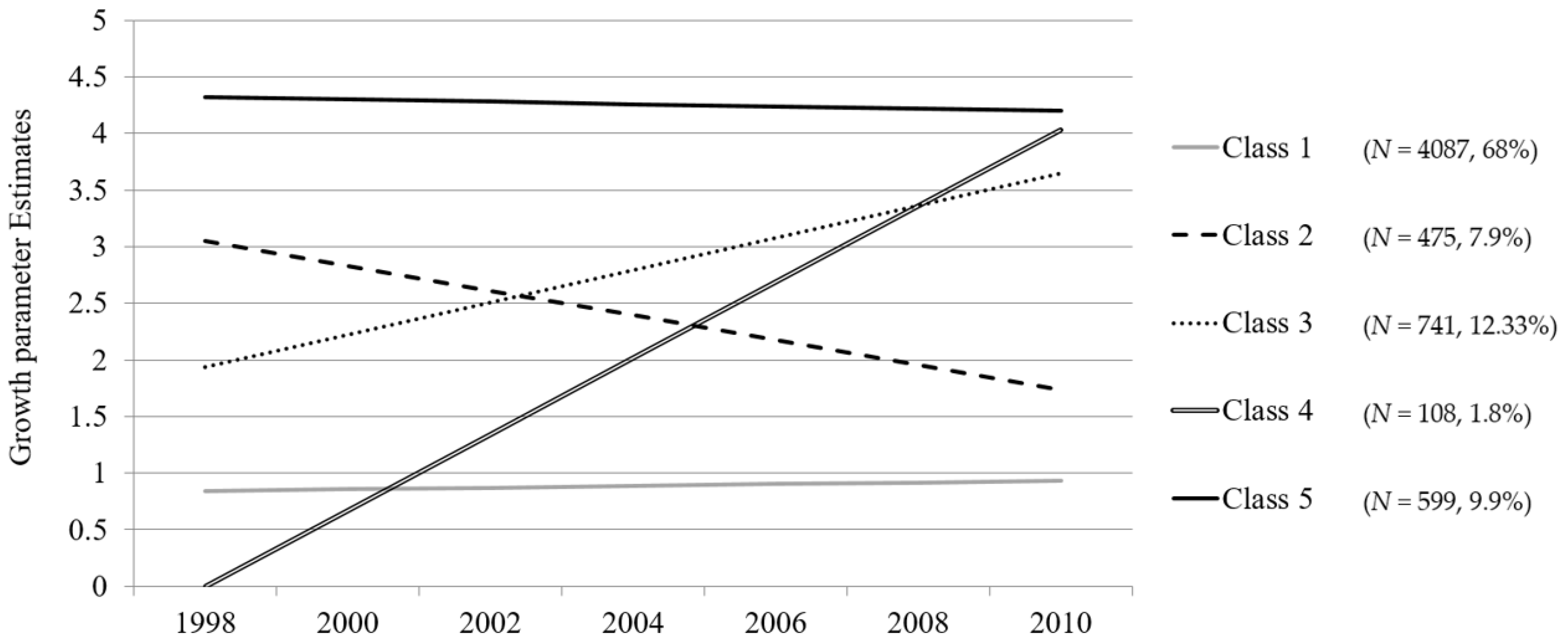
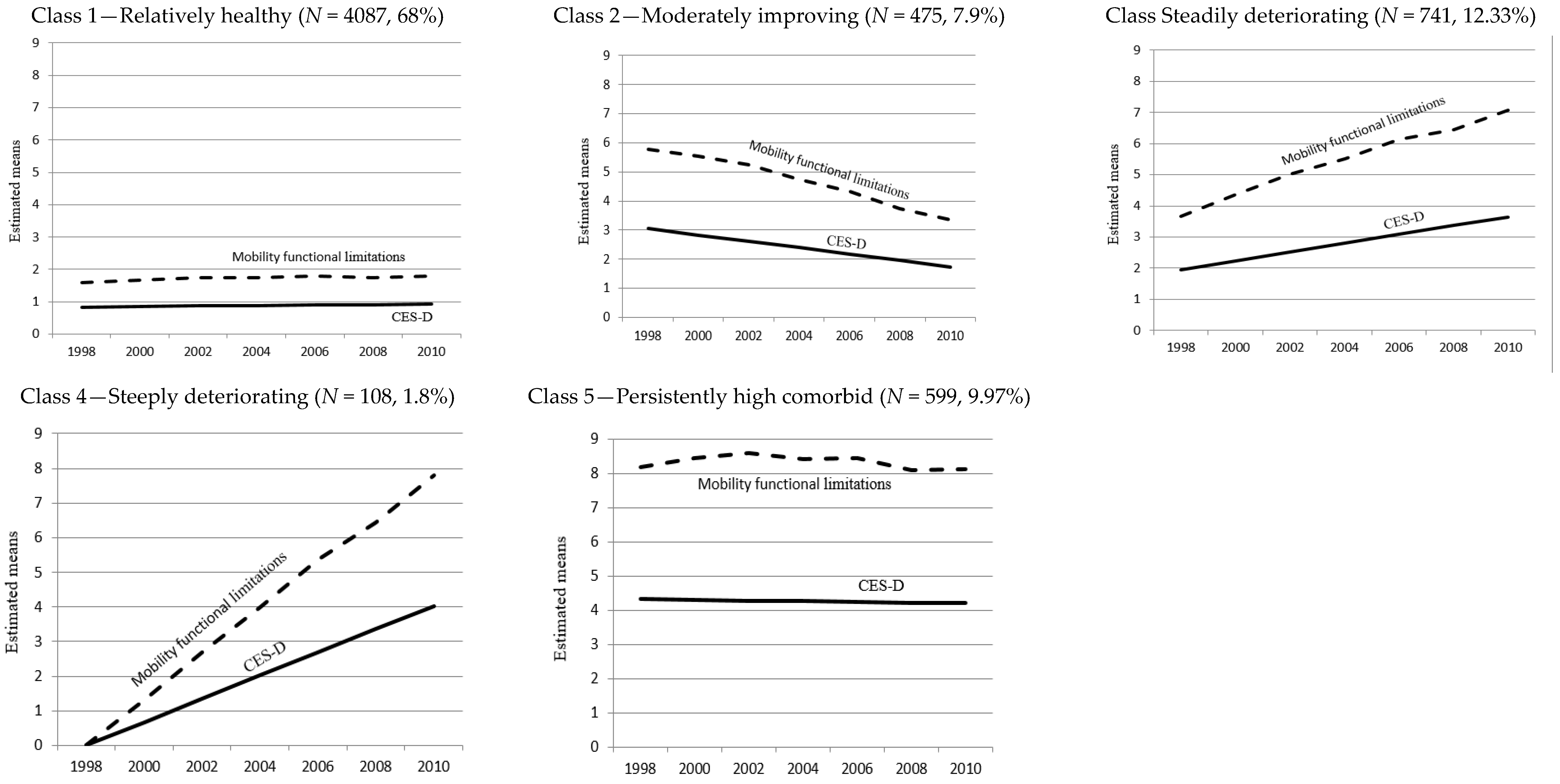
3.1. Trajectories of Mobility Functional Limitation and Depressive Symptoms
3.2. Characteristics of Trajectory Groups by Childhood and Adulthood Factors
3.3. Role of Childhood and Adulthood SES in Predicting Trajectory Membership
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Elwell-Sutton, T.M.; Jiang, C.Q.; Zhang, W.S.; Cheng, K.K.; Lam, T.H.; Leung, G.M.; Schooling, C.M. Socioeconomic influences at different life stages on health in Guangzhou, China. Soc. Sci. Med. 2011, 72, 1884–1892. [Google Scholar] [CrossRef] [PubMed]
- Ormel, J.; Von Korff, M.; Ustun, T.B.; Pini, S.; Korten, A.; Oldehinkel, T. Common mental disorders and disability across cultures: Results from the WHO collaborative study on psychological problems in general health care. JAMA 1994, 272, 1741–1748. [Google Scholar] [CrossRef] [PubMed]
- Ormel, J.; Von Korff, M. Synchrony of change in depression and disability: What next? Arch. Gen. Psychiatry 2000, 57, 381–382. [Google Scholar] [CrossRef] [PubMed]
- Buist-Bouwman, M.A.; de Graaf, R.; Vollebergh, W.A.M.; Ormel, J. Comorbidity of physical and mental disorders and the effect on work-loss days. Acta Psychiatr. Scand. 2005, 111, 436–443. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Butterworth, S.; Wadsworth, M.E.; Kuh, D. Childhood socioeconomic status predicts physical functioning a half century later. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Ferrucci, L.; Darer, J.; Williamson, J.D.; Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, M255–M263. [Google Scholar] [CrossRef]
- Millán-Calenti, J.C.; Maseda, A.; Rochette, S.; Vázquez, G.A.; Sánchez, A.; Lorenzo, T. Mental and psychological conditions, medical comorbidity and functional limitation: Differential associations in older adults with cognitive impairment, depressive symptoms and co-existence of both. Int. J. Geriatr. Psychiatry 2011, 26, 1071–1079. [Google Scholar] [CrossRef] [PubMed]
- Stansfeld, S.A.; Head, J.; Fuhrer, R.; Wardle, J.; Cattell, V. Social inequalities in depressive symptoms and physical functioning in the Whitehall II study: Exploring a common cause explanation. J. Epidemiol. Community Health 2003, 57, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Chao, S. Functional disability and depressive symptoms: Longitudinal effects of activity restriction, perceived stress, and social support. Aging Ment. Health 2014, 18, 767–776. [Google Scholar] [CrossRef] [PubMed]
- Wickrama, K.A.S.; Conger, R.D.; Abraham, W.T. Early adversity and later health: The intergenerational transmission of adversity through mental disorder and physical illness. J. Gerontol. B Psychol. Sci. Soc. Sci. 2005, 60, S125–S129. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Liang, J.; Bennett, J.M.; Botoseneanu, A.; Allore, H.G. Socioeconomic stratification and multidimensional health trajectories: Evidence of convergence in later old age. J. Gerontol. B Psychol. Sci. Soc. Sci. 2014, 70, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, W.; Gao, Q.; Wu, L.; Luo, Y.; Tang, Z.; Guo, X. The trajectories and correlation between physical limitation and depression in elderly residents of Beijing, 1992–2009. PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; George, L.K. Functional disability, disability transitions, and depressive symptoms in late life. J. Aging Health 2005, 17, 263–292. [Google Scholar] [CrossRef] [PubMed]
- Lenze, E.J.; Schulz, R.; Martire, L.M.; Zdaniuk, B.; Glass, T.; Kop, W.J.; Jackson, S.A.; Reynolds, C.F., 3rd. The course of functional decline in older people with persistently elevated depressive symptoms: Longitudinal findings from the Cardiovascular Health Study. J. Am. Geriatr. Soc. 2005, 53, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P. Our Prime: The Invention of Middle Age; Scribner: New York, NY, USA, 2012. [Google Scholar]
- Lachman, M.E.; Teshale, S.; Agrigoroaei, S. Midlife as a pivotal period in the life course: Balancing growth and decline at the crossroads of youth and old age. Int. J. Behav. Dev. 2015, 39, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Helson, R.; Soto, C.J.; Cate, R.A. From young adulthood through the middle ages. In Handbook of Personality Development; Mroczek, D.K., Little, T., Eds.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2003; pp. 337–352. [Google Scholar]
- Choi, M.; Lee, Y.H. Depression, powerlessness, social support, and socioeconomic status in middle-aged community residents. J. Korean Acad. Psychiatri. Ment. Health Nurs. 2010, 19, 196–204. [Google Scholar] [CrossRef]
- Doshi, J.A.; Cen, L.; Polsky, D. Depression and retirement in late middle-aged U.S. workers. Health Serv. Res. 2008, 43, 693–713. [Google Scholar] [CrossRef] [PubMed]
- Wight, R.G.; Ko, M.J.; Aneshensel, C.S. Urban Neighborhoods and depressive symptoms in late middle age. Res. Aging 2011, 33, 28–50. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H. Group-based trajectories of depressive symptoms and the predictors in the older population. Int. J. Geriatr. Psychiatry 2012, 27, 854–862. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Xu, X.; Quiñones, A.R.; Bennett, J.M.; Ye, W. Multiple trajectories of depressive symptoms in middle and late life. Psychol. Aging 2011, 26, 761–777. [Google Scholar] [CrossRef] [PubMed]
- Deeg, D.J. Longitudinal characterization of course types of functional limitations. Disabil. Rehabil. 2005, 27, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Bennett, J.M.; Shaw, B.A.; Quinones, A.R.; Ye, W.; Xu, X.; Ofstedal, M.B. Gender differences in functional status in middle and older age: Are there any age variations? J. Gerontol. B Psychol. Sci. Soc. Sci. 2008, 63, S282–S292. [Google Scholar] [CrossRef] [PubMed]
- Miech, R.A.; Shanahan, M.J. Socioeconomic status and depression over the life course. J. Health Soc. Behav. 2000, 41, 162–176. [Google Scholar] [CrossRef]
- Sutin, A.R.; Terracciano, A.; Milaneschi, Y.; An, Y.; Ferrucci, L.; Zonderman, A.B. The trajectory of depressive symptoms across the adult lifespan. JAMA Psychiatry 2013, 70, 803–811. [Google Scholar] [CrossRef] [PubMed]
- He, X.Z.; Baker, D.W. Body Mass Index, physical activity, and the risk of decline in overall health and physical functioning in late middle age. Am. J. Public Health 2004, 94, 1567–1573. [Google Scholar] [CrossRef] [PubMed]
- Hillsdon, M.M.; Brunner, E.J.; Guralnik, J.M.; Marmot, M.G. Prospective study of physical activity and physical function in early old age. Am. J. Prev. Med. 2005, 28, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Kuh, D.; Ben-Shlomo, Y. A life Course Approach to Chronic Disease Epidemiology: Tracing the Origins of Ill-Health from Early to Adult Life, 1st ed.; Oxford University Press: New York, NY, USA, 1997; pp. 1–309. [Google Scholar]
- Galobardes, B.; Lynch, J.W.; Davey Smith, G. Is the association between child-hood socioeconomic circumstances and cause-specific mortality established? Update of a systematic review. J. Epidemiol. Community Health 2008, 62, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Waite, L.J. The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2005, 60, S93–S101. [Google Scholar] [CrossRef] [PubMed]
- Harper, S.; Lynch, J.; Hsu, W.L.; Everson, S.A.; Hillemeier, M.M.; Raghunathan, T.E.; Salonen, J.T.; Kaplan, G.A. Life course socioeconomic conditions and adult psychosocial functioning. Int. J. Epidemiol. 2002, 31, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.W.; Kaplan, G.A.; Cohen, R.D.; Wilson, T.W.; Smith, N.; Kauhanen, J.; Salonen, J.T. Childhood and adult socioeconomic status as predictors of mortality in Finland. Lancet 1994, 343, 524–527. [Google Scholar] [CrossRef]
- Kwag, K.H. The Cumulative Influences of Socioeconomic Status on Health Outcomes in Late Adulthood: A Latent Growth Curve Analysis. Doctoral Thesis, Iowa State University, Iowa, IA, USA, 2009. [Google Scholar]
- Turrell, G.; Lynch, J.W.; Leite, C.; Raghunathan, T.; Kaplan, G.A. Socioeconomic disadvantage in childhood and across the life course and all-cause mortality and physical function in adulthood. J. Epidemiol. Community Health 2007, 61, 723–730. [Google Scholar] [CrossRef] [PubMed]
- Byers, A.L.; Vittinghoff, E.; Lui, L.; Hoang, T.; Blazer, D.G.; Covinsky, K.E.; Ensrud, K.E.; Cauley, J.A.; Hillier, T.A.; Fredman, L.; et al. Twenty-year depressive trajectories among older women. Arch. Gen. Psychiatry 2012, 69, 1073–1079. [Google Scholar] [CrossRef] [PubMed]
- Laaksonen, M.; Silventoinen, K.; Martikainen, P.; Rahkonen, O.; Pitkäniemi, J.; Lahelma, E. The effects of childhood circumstances, adult SES, and material circumstances on physical and mental functioning. Ann. Epidemiol. 2007, 17, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Mäkinen, T.; Laaksonen, M.; Lahelma, E.; Rahkonen, O. Associations of childhood circumstances with physical and mental functioning in adulthood. Soc. Sci. Med. 2006, 62, 1831–1839. [Google Scholar] [CrossRef] [PubMed]
- Grimard, F.; Laszlo, S.; Lim, W. Health, aging and childhood socio-economic conditions in Mexico. J. Health Econ. 2010, 29, 630–640. [Google Scholar] [CrossRef] [PubMed]
- Osler, M.; Nordentoft, M.; Andersen, A.N. Birth dimensions and risk of depression in adulthood: Cohort study of Danish men born in 1953. Br. J. Psychiatry 2005, 186, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Kwon, E.; Kim, B.; Lee, H.J.; Park, S. Heterogeneous trajectories of depressive symptoms in late middle-age: Critical period, accumulation, and social mobility life course perspectives. J. Aging Health 2017. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; John Wiley & Sons: New York, NY, USA, 1987. [Google Scholar]
- Haas, S.A. The long-term effects of poor childhood health: An assessment and application of retrospective reports. Demography 2007, 44, 113–135. [Google Scholar] [CrossRef] [PubMed]
- Elo, I. Childhood conditions and adult health: Evidence from the health and retirement study. In Population Aging Research Center Working Papers; University of Pennsylvania: Philadelphia, PA, USA, 1998. [Google Scholar]
- Bowen, M.E. Childhood socioeconomic status and racial differences in disability: Evidence from the Health and Retirement Study (1998–2006). Soc. Sci. Med. 2009, 69, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.T. Early-Life Characteristics, Psychiatric History, and Cognition Trajectories in Later Life. Gerontologist 2010, 50, 646–656. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Soldo, B.J.; Elo, I.T. Do early-life conditions predict functional health in adulthood? The case of Mexico. Soc. Sci. Med. 2011, 72, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Walsemann, K.M.; Geronimus, A.T.; Gilbert, C.G. Accumulating disadvantage over the life course: Evidence from a longitudinal study investigating the relationship between educational advantage in youth and health in middle-age. Res. Aging 2008, 30, 169–199. [Google Scholar] [CrossRef]
- Haas, S. Trajectories of functional health: The ‘long arm’ of childhood health and socioeconomic factors. Soc. Sci. Med. 2008, 66, 849–861. [Google Scholar] [CrossRef] [PubMed]
- Nagi, S.Z. Disability and Rehabilitation: Legal, Clinical, and Self-Concepts and Measurement, 1st ed.; Ohio State University Press: Columbus, Ohio, USA, 1969. [Google Scholar]
- Wickrama, K.K.; Mancini, J.A.; Kwag, K.; Kwon, J. Heterogeneity in multidimensional health trajectories of late old years and socioeconomic stratification: A latent trajectory class analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2012, 68, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Giele, J.Z. Life stories to understand diversity: Variations by class, race, and gender. In The Craft of Life Course Research; Elder, G.H., Jr., Giele, J.Z., Eds.; Guilford: New York, NY, USA, 2009; pp. 236–257. [Google Scholar]
- Massagli, M.; Hauser, R.M. Response variability in self and proxy reports of paternal and filial socioeconomic characteristics. Am. J. Sociol. 1983, 89, 420–431. [Google Scholar] [CrossRef]
- Islam, M.M.; Valderas, J.M.; Yen, L.; Dawda, P.; Jowsey, T. Multimorbidity and comorbidity of chronic diseases among the senior Australians: Prevalence and patterns. PLoS ONE 2014, 9. [Google Scholar] [CrossRef] [PubMed]
- Forman-Hoffman, V.L.; Richardson, K.K.; Yankey, J.W.; Hillis, S.L.; Wallace, R.B.; Wolinsky, F.D. Impact of functional limitations and medical comorbidity on subsequent weight changes and increased depressive symptoms in older adults. J. Aging Health 2008, 20, 367–384. [Google Scholar] [CrossRef] [PubMed]
- Tomey, K.; Sowers, M.R.; Harlow, S.; Jannausch, M.; Zheng, H.; Bromberger, J. Physical functioning among mid-life women: Associations with trajectory of depressive symptoms. Soc. Sci. Med. 2010, 71, 1259–1267. [Google Scholar] [CrossRef] [PubMed]
- Muthén, B.; Muthén, LK. Mplus Users Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2015; pp. 1–870. [Google Scholar]
- Jung, T.; Wickrama, K. An introduction to latent class growth analysis and growth mixture modeling. Soc. Personal. Psychol. Compass 2008, 2, 302–317. [Google Scholar] [CrossRef]
- Xie, H.; Gregory, J.M.; He, X.; Drake, R.E. Using the group-based dual trajectory to analyze two related longitudinal outcomes. J. Drug Issues 2010, 40, 45–62. [Google Scholar] [CrossRef]
- Muthén, B. Latent variable analysis. In The SAGE Handbook of. Quantitative Methodology for the Social Sciences, 1st ed.; Kaplan, D., Ed.; SAGE Publications: Thousand Oaks, CA, USA, 2004; pp. 345–368. [Google Scholar]
- Clark, S.L.; Muthén, B.O. Relating Latent Class Analysis Results to Variables not Included in the Analysis. Unpublished Manuscript. 2009. Available online: https://www.statmodel.com/download/relatinglca.pdf (accessed on 16 May 2017).
- Schwarz, G. Estimating the dimension of a model. Ann. Stat. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Sclove, S.L. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika 1987, 52, 333–343. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.M. Mplus Version 2.13. Addendum to Mplus User’s Guide; Muthén &Muthén: Los Angeles, CA, USA, 2003. [Google Scholar]
- Lo, Y.; Mendell, N.R.; Rubin, D.B. Testing the number of components in a normal mixture. Biometrika 2001, 88, 767–778. [Google Scholar] [CrossRef]
- McLachlan, G.; Peel, D. Mixtures of Factor Analyzers. In Fite Mixture Models, 1st ed.; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2000; pp. 238–254. [Google Scholar]
- Glisky, E.L. Changes in Cognitive Function in Human Aging. In Brain Aging: Models, Methods, and Mechanisms, 1st ed.; Riddle, D.R., Ed.; CRC Press: Florida, FL, USA, 2007; pp. 3–20. [Google Scholar]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- McLoyd, V.C. Socioeconomic disadvantage and child development. Am. Psychol. 1998, 53, 185–204. [Google Scholar] [CrossRef] [PubMed]
- Turrell, G.; Lynch, J.W.; Kaplan, G.A.; Everson, S.A.; Helkala, E.L.; Kauhanen, J.; Salonen, J.T. Socioeconomic position across the lifecourse and cognitive function in late middle age. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002, 57, S43–S51. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Wilkinson, R.G. Psychosocial and material pathways in the relation between income and health: A response to Lynch et al. BMJ 2006, 322, 1233–1236. [Google Scholar] [CrossRef]
- Bruce, M.L. Depression and disability in late life: Directions for future research. Am. J. Geriatr. Psychiatry 2001, 9, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Ormel, J.; Rijsdijk, F.V.; Sullivan, M.; van Sonderen, E.; Kempen, G.I. Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2002, 57, P338–P347. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.G.; Lynch, S.M. Trajectories of impairment, social support, and depressive symptoms in later life. J. Gerontol. B Psychol. Sci. Soc. Sci. 2004, 59, S238–S246. [Google Scholar] [CrossRef] [PubMed]
- Uchino, B.N. Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of Perceived and Received Support. Perspect. Psychol. Sci. 2009, 4, 236–255. [Google Scholar] [CrossRef] [PubMed]
- Melchior, M.; Chastang, J.F.; Head, J.; Goldberg, M.; Zins, M.; Nabi, H.; Younes, N. Socioeconomic position predicts long-term depression trajectory: A 13-year follow-up of the GAZEL cohort study. Mol. Psychiatry 2013, 18, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Musliner, K.L.; Munk-Olsen, T.; Eaton, W.W.; Zandi, P.P. Heterogeneity in long-term trajectories of depressive symptoms: Patterns, predictors and outcomes. J. Affect. Disord. 2016, 192, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Bosma, H.; van Boxtel, M.P.J.; Ponds, R.W.H.M.; Houx, P.J.H.; Jolles, J. Education and age-elated cognitive decline: The contribution of mental workload. Educ. Gerontol. 2003, 29, 165–173. [Google Scholar] [CrossRef]
| Number of Classes | Log Likelihood | AIC | BIC | SA-BIC | Entropy | LRT p Value | Class Proportions | |
|---|---|---|---|---|---|---|---|---|
| 1 | −109,191.729 | 218,433.458 | 218,602.897 | 218,523.453 | a | a | ||
| 2 | −106,864.897 | 213,785.794 | 213,975.566 | 213,886.589 | 0.891 | 0.0000 | Class 1: 5709 (95.5%) | Class 2: 301 (4.5%) |
| 3 | −105,982.392 | 212,026.785 | 212,236.889 | 212,138.379 | 0.853 | 0.0000 | Class 1: 4531 (75.4%) Class 2: 1189 (19.8%) | Class 3: 290 (4.8%) |
| 4 | −105,776.791 | 211,621.583 | 211,852.020 | 211,743.976 | 0.828 | 0.0000 | Class 1: 3966 (66.3%) Class 2: 1142(19.4%) | Class 3: 240 (3.1%) Class 4: 661 (11.2%) |
| 5 | −105,584.119 | 211,242.238 | 211,493.008 | 211,375.431 | 0.799 | 0.0084 | Class 1: 4087 (68%) Class 2: 475 (7.9%) Class 3: 741 (12.3%) | Class 4: 108 (1.8%) Class 5: 599 (9.9%) |
| 6 | −105,471.078 | 211,022.156 | 211,293.258 | 211,166.148 | 0.788 | 0.0051 | Class 1: 3546 (58.8%) Class 2: 541 (9.3%) Class 3: 300 (4.5%) | Class 4: 901 (15.5%) Class 5: 60 (0.9%) Class 6: 662 (11%) |
| Total | Class 1 | Class 2 | Class 3 | Class 4 | Class 5 | Statistics | ||
|---|---|---|---|---|---|---|---|---|
| Sample | Relatively Healthy | Moderately Improving | Steadily Deteriorating | Steeply Deteriorating | Persistently High Comorbid | |||
| n = 6010 | n = 4087 (68%) | n = 475 (7.9%) | n = 741 (12.33%) | n = 108 (1.8%) | n = 599 (9.97%) | |||
| Ascribed factor | Age | 55.05 (3.13) | 54.99 (3.17) | 55.46 (3.02) | 54.97 (3.04) | 53.81 (2.31) | 55.50 (3.08) | F(6010) = 11.20 *** |
| Race | (8) = 106.31 *** | |||||||
| Caucasian | 4635 (77.12) | 3296 (80.65) | 339 (71.37) | 537 (72.47) | 75 (69.45) | 388 (64.77) | ||
| African American | 1016 (16.91) | 580 (14.19) | 100 (21.05) | 158 (21.32) | 21 (19.44) | 157 (26.21) | ||
| Others | 359 (5.97) | 211 (5.16) | 36 (7.58) | 46 (6.21) | 12 (11.11) | 54 (9.02) | ||
| Female | 3545 (58.98) | 2288 (55.98) | 271 (57.05) | 511 (68.96) | 57 (52.77) | 418 (69.78) | (4) = 153.18 *** | |
| Childhood factor | Poverty | 1608 (26.76) | 923 (22.58) | 145 (30.53) | 246 (33.20) | 41 (37.96) | 253 (42.24) | (4) = 135.62 *** |
| Self-rated health a | 1.95 (0.01) | 1.77 (0.94) | 2.26 (1.13) | 2.15 (1.08) | 2.22 (1.14) | 2.63 (1.23) | F(6010) = 119.33*** | |
| Parental education | (8) = 206.82 *** | |||||||
| Less than HS | 1181 (19.65) | 895 (21.90) | 72 (15.15) | 118 (15.92) | 16 (14.82) | 80 (13.36) | ||
| HS graduates | 3498 (58.20) | 2132 (52.16) | 336 (70.73) | 504 (68.02) | 71 (65.74) | 455 (95.96) | ||
| College or higher | 1331 (22.15) | 1060 (25.94) | 67 (14.11) | 119 (16.06) | 21 (19.44) | 64 (10.68) | ||
| Adulthood factor | Marital status b | (8) = 146.66 *** | ||||||
| Constantly married | 3178 (52.88) | 2349 (57.47) | 229 (48.21) | 341 (46.02) | 48 (44.44) | 211 (35.22) | ||
| Constantly unmarried | 2014 (33.51) | 1197 (29.29) | 185 (38.95) | 291 (39.27) | 42 (38.89) | 299 (49.92) | ||
| Status changed | 818 (13.61) | 541 (13.24) | 61 (12.84) | 109 (14.71) | 18 (16.67) | 89 (14.86) | ||
| Work status b | (8) = 1.10 *** | |||||||
| Constantly worked | 2428 (40.40) | 2057 (50.33) | 134 (28.21) | 179 (24.16) | 20 (18.52) | 38 (6.34) | ||
| Never worked | 1463 (24.34) | 599 (14.66) | 176 (37.05) | 243 (32.79) | 26 (24.07) | 419 (69.95) | ||
| Status changed | 2119 (35.26) | 1431 (35.01) | 165 (34.74) | 319 (43.05) | 62 (57.41) | 142 (23.71) | ||
| Education | (8) = 593.42 *** | |||||||
| Less than HS | 1075 (17.89) | 463 (11.33) | 123 (25.89) | 182 (24.56) | 31 (28.70) | 276 (46.08) | ||
| HS graduates | 2051 (34.12) | 1349 (33.01) | 185 (38.95) | 304 (41.03) | 34 (31.48) | 179 (29.88) | ||
| College or higher | 2884 (47.99) | 2275 (55.66) | 167 (35.16) | 255 (34.41) | 43 (39.81) | 144 (24.04) | ||
| Monthly income ($) | 5883.11 (8665.44) | 7050.52 (11,406.2) | 4143.79 (7127.3) | 3835.93 (3947.54) | 4111.71 (5789.76) | 2148.95 (3426.09) | F(6010) = 48.86 *** | |
| Logged income | 10.47 (0.02) | 10.77 (1.48) | 10.06 (1.84) | 10.13 (1.69) | 9.94 (2.29) | 9.31 (2.02) | F(6010) = 130.97 *** | |
| Income change b | (12) = 534.62 *** | |||||||
| High maintaining Increased | 765 (12.73) 2156 (35.87) | 654 (16.00) 1549 (37.90) | 40 (8.42) 158 (33.26) | 55 (7.42) 248 (33.47) | 4 (3.70) 32 (29.63) | 12 (2.00) 169 (28.21) | ||
| Decreased | 2206 (36.71) | 1516 (37.09) | 174 (36.63) | 283 (38.19) | 54 (50.00) | 179 (29.88) | ||
| Low maintaining | 883 (14.69) | 368 (9.00) | 103 (21.68) | 155 (20.92) | 18(16.67) | 239 (39.90) | ||
| Health status | ||||||||
| CES-D | 1.71 (2.11) | 1.04 (1.52) | 3.06 (2.38) | 2.27 (2.09) | 1.31 (1.55) | 4.59 (2.36) | F(6010) = 629.17 *** | |
| Functional limitation | 2.88 (2.76) | 1.51 (1.36) | 6.02 (1.77) | 4.23 (2.04) | 1.46 (1.31) | 8.35 (1.72) | F(6010) = 3390.53 *** | |
| N of chronic diseases | 1.24 (1.23) | 0.86 (0.94) | 1.74 (1.22) | 1.81 (1.19) | 1.25 (1.06) | 2.76 (1.50) | F(6010) = 515.14 *** | |
| Obesity (N, %) | 2057 (34.23) | 1121 (27.43) | 200 (42.11) | 370 (49.93) | 35 (32.41) | 331 (55.26) | (4) = 296.05 *** | |
| Self-rated health | 2.68 (1.15) | 2.25 (0.93) | 3.48 (0.96) | 3.26 (0.97) | 2.81 (1.02) | 4.28 (0.81) | F(6010) = 826.19 *** |
| Model 1: Ascribed Factors | Model 2: + Childhood Factors | Model 3: + Adulthood Factors | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Class 2: Moderately Improving | Class 3: Steadily Deteriorating | Class 4: Steeply Deteriorating | Class 5: Persistently High comorbid | Class 2: Moderately Improving | Class 3: Steadily Deteriorating | Class 4: Steeply Deteriorating | Class 5: Persistently High comorbid | Class 2: Moderately Improving | Class 3: Steadily Deteriorating | Class 4: Steeply Deteriorating | Class 5: Persistently High Comorbid | |||||||||||||
| RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | RRR (SE) | p | |
| Person-ascribed | ||||||||||||||||||||||||
| Age | 0.96 | 0.000 | 1.01 | 0.044 | .96 | 0.008 | 1.02 | 0.000 | 1.03 | 0.000 | 1.00 | 0.524 | 0.96 | 0.002 | 1.01 | 0.013 | 1.02 | 0.000 | 0.98 | 0.059 | 0.94 | 0.000 | 0.99 | 0.466 |
| (0.01) | (0.00) | (0.01) | (0.00) | (0.00) | (0.00) | (0.01) | (0.00) | (0.00) | (0.00) | (0.01) | (0.00) | |||||||||||||
| Female | 0.98 | 0.000 | 1.55 | 0.000 | 0.98 | 0.902 | 1.77 | 0.000 | 1.71 | 0.000 | 1.54 | 0.000 | 0.99 | 0.964 | 1.76 | 0.000 | 2.49 | 0.000 | 2.07 | 0.000 | 1.11 | 0.369 | 3.90 | 0.000 |
| (0.11) | (0.08) | (0.11) | (0.11) | (0.12) | (0.08) | (0.11) | (0.11) | (0.19) | (0.13) | (0.13) | (0.36) | |||||||||||||
| Race (Caucasian) | ||||||||||||||||||||||||
| African American | 1.52 | 0.000 | 1.66 | 0.000 | 1.52 | 0.001 | 2.46 | 0.000 | 1.41 | 0.000 | 1.40 | 0.000 | 1.25 | 0.062 | 1.85 | 0.000 | 0.86 | 0.041 | 0.81 | 0.001 | 0.96 | 0.808 | 0.73 | 0.000 |
| (0.18) | (0.08) | (0.18) | (0.13) | (0.08) | (0.07) | (0.15) | (0.10) | (0.06) | (0.04) | (0.12) | (0.05) | |||||||||||||
| Others | 2.39 | 0.000 | 1.52 | 0.000 | 2.39 | 0.000 | 2.43 | 0.000 | 1.50 | 0.000 | 1.21 | 0.027 | 1.85 | 0.000 | 1.61 | 0.000 | 1.00 | 0.967 | 0.87 | 0.187 | 1.50 | 0.015 | 0.73 | 0.012 |
| (0.38) | (0.12) | (0.38) | (0.020) | (0.14) | (0.10) | (0.30) | (0.07) | (0.11) | (0.08) | (0.25) | (0.09) | |||||||||||||
| Childhood SES | ||||||||||||||||||||||||
| Poverty | 1.03 | 0.492 | 1.30 | 0.000 | 1.70 | 0.000 | 1.49 | 0.000 | 0.99 | 0.939 | 1.23 | 0.000 | 1.57 | 0.000 | 1.24 | 0.001 | ||||||||
| (0.05) | (0.05) | (0.17) | (0.07) | (0.06) | (0.06) | (0.16) | (0.08) | |||||||||||||||||
| Parental education | ||||||||||||||||||||||||
| <High school | 1.57 | 0.000 | 1.56 | 0.000 | 1.53 | 0.002 | 1.86 | 0.000 | 1.25 | 0.003 | 1.24 | 0.000 | 1.31 | 0.049 | 1.28 | 0.007 | ||||||||
| (0.10) | (0.08) | (0.20) | (0.12) | (0.09) | (0.07) | (0.18) | (0.12) | |||||||||||||||||
| College or higher | 0.72 | 0.000 | 0.91 | 0.197 | 1.23 | 0.182 | 0.73 | 0.001 | 0.86 | 0.126 | 1.16 | 0.050 | 1.54 | 0.007 | 1.06 | 0.611 | ||||||||
| (0.06) | (0.06) | (0.19) | (0.06) | (0.08) | (0.08) | (0.025) | (0.12) | |||||||||||||||||
| Adulthood SES | ||||||||||||||||||||||||
| Income change b | ||||||||||||||||||||||||
| Increased | 1.27 | 0.016 | 1.41 | 0.000 | 2.42 | 0.000 | 2.55 | 0.000 | ||||||||||||||||
| (0.12) | (0.12) | (0.16) | (0.42) | |||||||||||||||||||||
| Decreased | 1.33 | 0.004 | 1.41 | 0.000 | 3.54 | 0.000 | 2.41 | 0.000 | ||||||||||||||||
| (0.13) | (0.12) | (0.88) | (0.40) | |||||||||||||||||||||
| Low maintaining | 1.70 | 0.000 | 2.16 | 0.000 | 2.98 | 0.000 | 3.91 | 0.000 | ||||||||||||||||
| (0.19) | (0.21) | (0.82) | (0.68) | |||||||||||||||||||||
| Education a | ||||||||||||||||||||||||
| <High school | 1.07 | 0.356 | 1.04 | 0.475 | 1.66 | 0.000 | 1.47 | 0.000 | ||||||||||||||||
| (0.07) | (0.06) | (0212) | (0.11) | |||||||||||||||||||||
| College or higher | 0.81 | 0.002 | 0.64 | 0.000 | 0.83 | 0.114 | 0.70 | 0.000 | ||||||||||||||||
| (0.05) | (0.03) | (0.09) | (0.05) | |||||||||||||||||||||
| Covariates | ||||||||||||||||||||||||
| Marital status | ||||||||||||||||||||||||
| Constantly unmarried | 1.41 | 0.000 | 1.56 | 0.000 | 1.55 | 0.000 | 2.08 | 0.000 | ||||||||||||||||
| (0.08) | (0.08) | (0.17) | (0.15) | |||||||||||||||||||||
| Status changed | 1.22 | 0.021 | 1.28 | 0.001 | 1.70 | 0.000 | 1.55 | 0.000 | ||||||||||||||||
| (0.10) | (0.09) | (0.23) | (0.16) | |||||||||||||||||||||
| Work status | ||||||||||||||||||||||||
| Constantly not work | 2.12 | 0.000 | 2.959 | 0.000 | 3.28 | 0.000 | 11.87 | 0.000 | ||||||||||||||||
| (0.15) | (0.16) | (0.49) | (1.29) | |||||||||||||||||||||
| Status changed | 1.33 | 0.000 | 2.23 | 0.000 | 3.54 | 0.000 | 4.24 | 0.000 | ||||||||||||||||
| (0.08) | (0.12) | (0.44) | (0.46) | |||||||||||||||||||||
| Childhood health c | 1.53 | 0.000 | 1.36 | 0.000 | 1.41 | 0.000 | 1.93 | 0.000 | 1.15 | 0.000 | 1.06 | 0.007 | 1.20 | 0.000 | 1.23 | 0.000 | ||||||||
| (0.03) | (0.02) | (0.05) | (0.03) | (0.02) | (0.02) | (0.05) | (0.03) | |||||||||||||||||
| (Baseline) Adult health | ||||||||||||||||||||||||
| Self-rated health c | 2.72 | 0.000 | 2.03 | 0.000 | 1.28 | 0.000 | 5.34 | 0.000 | ||||||||||||||||
| (0.08) | (0.05) | (0.06) | (0228) | |||||||||||||||||||||
| Number of chronic diseases | 1.49 | 0.000 | 1.60 | 0.000 | 1.29 | 0.000 | 2.02 | 0.000 | ||||||||||||||||
| (0.03) | (0.03) | (0.06) | (0.05) | |||||||||||||||||||||
| Obesity | 1.36 | 0.000 | 1.91 | 0.000 | 1.06 | 0.515 | 2.18 | 0.000 | ||||||||||||||||
| (0.07) | (0.08) | (0.11) | (0.14) | |||||||||||||||||||||
| Died during follow-up | 2.77 | 0.001 | 4.25 | 0.000 | 5.41 | 0.000 | 7.44 | 0.000 | 3.02 | 0.000 | 4.56 | 0.000 | 5.91 | 0.000 | 8.72 | 0.000 | 1.61 | 0.150 | 2.62 | 0.000 | 4.17 | 0.001 | 2.50 | 0.003 |
| (0.81) | (0.95) | (2.22) | (1.56) | (0.89) | (1.04) | (2.44) | (1.92) | (0.54) | (0.70) | (1.77) | (0.77) | |||||||||||||
| Ever attrited | 1.08 | 0.390 | 1.08 | 0.280 | 0.89 | 0.560 | 1.07 | 0.384 | 1.07 | 0.457 | 1.07 | 0.367 | 0.89 | 0.539 | 1.07 | 0.406 | 1.01 | 0.857 | 0.99 | 0.976 | 0.79 | 0.240 | 0.99 | 0.972 |
| (0.09) | (0.08) | (0.16) | (0.09) | (0.09) | (0.08) | (0.16) | (0.09) | (0.10) | (0.08) | (0159) | (0.11) | |||||||||||||
| Constant | 0.00 | 0.000 | 0.03 | 0.000 | 0.18 | 0.027 | 0.00 | 0.000 | 0.00 | 0.000 | 0.02 | 0.000 | 0.002 | 0.00 | 0.000 | 0.00 | 0.000 | 0.00 | 0.000 | 0.01 | 0.000 | 0.00 | 0.000 | |
| (0.00) | (0.01) | (0.14) | (0.00) | (0.00) | (0.00) | (0.00) | (0.00) | (0.00) | (0.01) | (0.00) | ||||||||||||||
| Pseudo R2 | 0.0160 | 0.0592 | 0.2818 | |||||||||||||||||||||
| Log Likelihood chi2 | 797.69 (24) *** | 2946.84 (40) *** | 14,039.84(88) *** | |||||||||||||||||||||
| (df) | 2149.15 (16) *** | 11,093.00(48) *** | ||||||||||||||||||||||
| ∆χ2 | ||||||||||||||||||||||||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, E.; Park, S. Heterogeneous Trajectories of Physical and Mental Health in Late Middle Age: Importance of Life-Course Socioeconomic Positions. Int. J. Environ. Res. Public Health 2017, 14, 582. https://doi.org/10.3390/ijerph14060582
Kwon E, Park S. Heterogeneous Trajectories of Physical and Mental Health in Late Middle Age: Importance of Life-Course Socioeconomic Positions. International Journal of Environmental Research and Public Health. 2017; 14(6):582. https://doi.org/10.3390/ijerph14060582
Chicago/Turabian StyleKwon, Eunsun, and Sojung Park. 2017. "Heterogeneous Trajectories of Physical and Mental Health in Late Middle Age: Importance of Life-Course Socioeconomic Positions" International Journal of Environmental Research and Public Health 14, no. 6: 582. https://doi.org/10.3390/ijerph14060582




