Prevalence of Malocclusion in 3- to 5-Year-Old Children in Shanghai, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
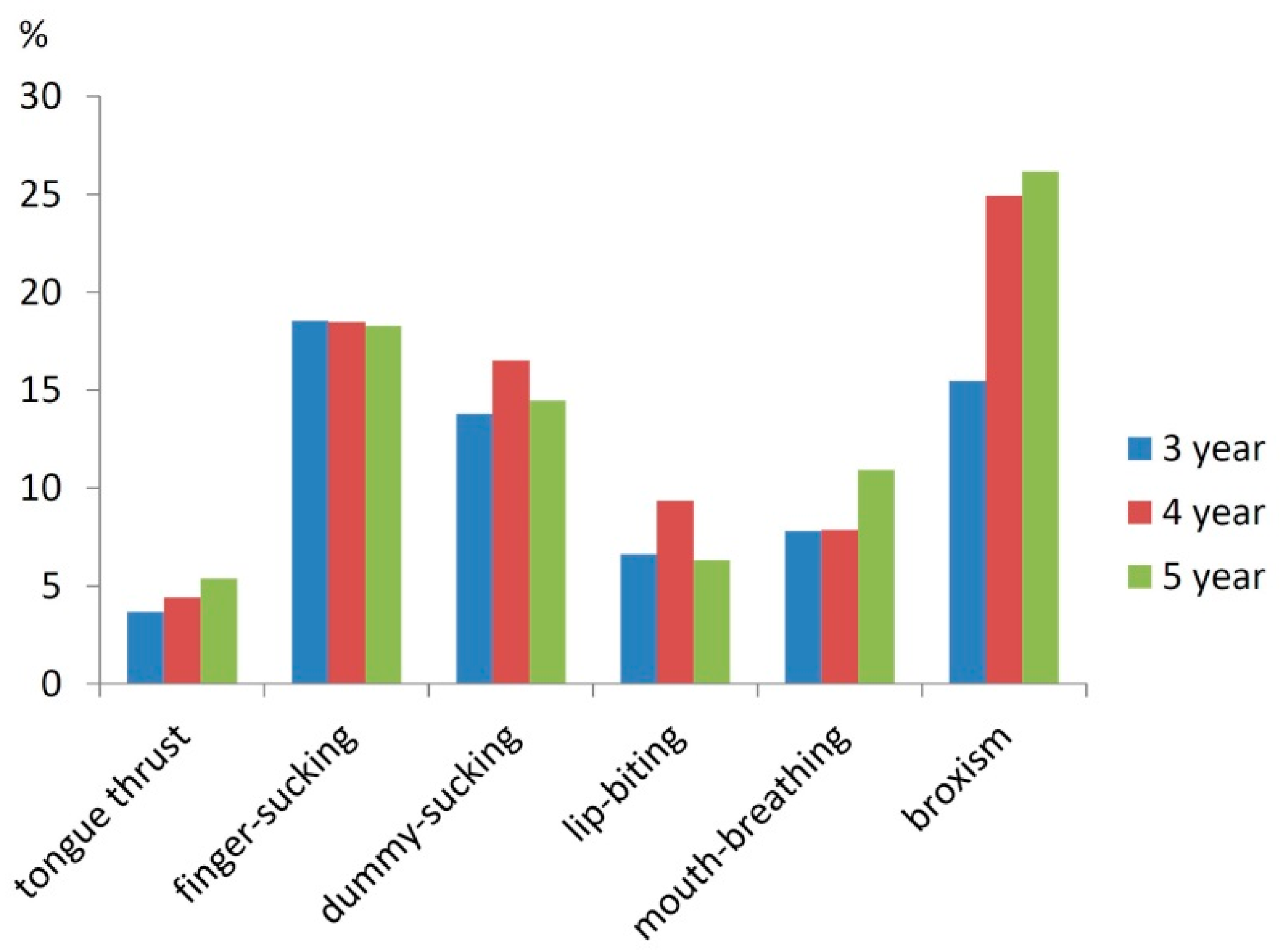
2.2. Questionnaire
2.3. Dental Examination
2.3.1. Sagittal Anomalies
- Deciduous canine relationship: Equal to Angel’s classification. The canine relationship was recorded as class II or class III, if it was class I on one side and class II or class III on the other. Children with class II canine relation on one side and class III on the other side were recorded as mixed.
- Terminal plane relationship of the second primary molars: The relationship of the distal surface between the upper and lower second deciduous molar including three types (flush type, mesial type and distal type). The relationship of molars and canines were recorded on the basis of bilateral occlusion.
- Maxillary overjet: This was measured from the palatal surface of the mesial corner of the most protruded maxillary incisor to the labial surface of the corresponding mandibular incisor. (0 mm: edge-to-edge; >3 mm, ≤5 mm: mild; >5 mm, ≤8 mm: moderate; >8 mm: severe).
- Mandibular overjet (anterior crossbite): This was recorded when one or more of the maxillary incisors or canine occluded lingual to the mandibular incisors.
2.3.2. Vertical Anomalies
- Overbite: This was graded according to coverage of the mandibular incisor by the most protruded fully erupted maxillary incisor. (<1/2: normal; >1/2, ≤3/4: mild; >3/4, <1: moderate; all cover: severe).
- Open bite, anterior (<3 mm: mild; >3 mm, ≤5 mm: moderate; >5 mm: severe).
2.3.3. Transversal Anomalies
- Posterior crossbite: This was recorded when one or more of the maxillary primary molars occluded the lingual to the buccal cusps of the opposing mandibular teeth.
- Scissors bite: This was recorded when one or more maxillary primary molars occluded the buccal to the buccal surfaces or the lingual to the lingual surfaces of the corresponding mandibular teeth.
- Midline displacement.
2.3.4. Space Discrepancies
- Crowding (anterior, posterior): >0, ≤2 mm: mild; >2 mm, ≤4 mm: moderate; >4 mm: severe
- Spacing: >0, ≤2 mm: mild; >2 mm, ≤4 mm: moderate; >4 mm: severe
2.3.5. Others
- Dental arch shape: triangular; U-shape; square-shape
- Tonsil: normal; antiadoncus I°; antiadoncus II°; antiadoncus III°
- Temporomandibular joint disorder
- Nasal ventilation
- Mandibular plane angle
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Kiliaridis, S.; Engström, C.; Thilander, B. The relationship between masticatory function and craniofacial morphology. I. A cephalometric longitudinal analysis in the growing rat fed a soft diet. Eur. J. Orthod. 1985, 7, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Peres, K.G.; Barros, A.J.; Peres, M.A.; Victora, C.G. Effects of breastfeeding and sucking habits on malocclusion in a birth cohort study. Rev. Saude Publica 2007, 41, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Nanda, R.S.; Khan, I.; Anand, R. Age changes in the occlusal pattern of deciduous dentition. J. Dent. Res. 1973, 52, 221–224. [Google Scholar] [CrossRef] [PubMed]
- Frazao, P.; Narvai, P.C.; Latorre, M.R.; Castellanos, R.A. Malocclusion prevalence in the deciduous and permanent dentition of schoolchildren in the city of São Paulo, Brazil. Cad. Saude Publica 2002, 18, 1197–1205. [Google Scholar] [PubMed]
- Da, S.F.O.; Ferrari Júnior, F.M.; Aiello, C.A.; Zopone, N. Correction of posterior crossbite in the primary dentition. J. Clin. Pediatr. Dent. 2007, 32, 73–78. [Google Scholar]
- Dhar, V.; Jain, A.; Van Dyke, T.E.; Kohli, A. Prevalenc of gingival diseases, malocclusion and fluorosis in school-going children of rural areas in Udaipur district. J. Indian Soc. Pedod. Prev. Dent. 2007, 25, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, M.H.R. Relationship between occlusal findings and orofacial myofunctional status in primary and mixed dentition. J. Orofac. Orthop. 2007, 68, 74–90. [Google Scholar] [CrossRef] [PubMed]
- Leite-Cavalcanti, A.; Medeiros-Bezerra, P.K.; Moura, C. Breast-feeding, bottle-feeding, sucking habits and malocclusion in Brazilian preschool children. Rev. Salud Pública 2007, 9, 194–204. [Google Scholar] [PubMed]
- Carvalho, A.C.; Paiva, S.M.; Scarpelli, A.C.; Viegas, C.M.; Ferreira, F.M.; Pordeus, I.A. Prevalence of malocclusion in primary dentition in a population-based sample of Brazilian preschool children. Eur. J. Paediatr. Dent. 2011, 12, 107–111. [Google Scholar] [PubMed]
- Wagner, Y.; Heinrichweltzien, R. Occlusal characteristics in 3-year-old children—Results of a birth cohort study. BMC Oral Health 2015, 15, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Fu, M.; Zhang, D.; Wang, B. The prevalence of malocclusion in China—An investigation of 25,392 children. Chin. J. Stomatol. 2002, 37, 371–373. [Google Scholar]
- Brandao, I.M.; Peres, A.S.; Saliba, N.A.; Moimaz, S.A. Prevalence of dental fluorosis in school children from Marinopolis, Sao Paulo. Cad. Saúde Pública 2002, 18, 877–881. [Google Scholar] [PubMed]
- World Health Organization. Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Thilander, B.; Pena, L.; Infante, C.; Parada, S.S.; De, M.C. Prevalence of malocclusion and orthodontic treatment need in children and adolescents in Bogota, Colombia. An epidemiological study related to different stages of dental development. Eur. J. Orthodont. 2001, 23, 153–167. [Google Scholar] [CrossRef]
- Stahl, F.; Grabowski, R. Malocclusion and caries prevalence: Is there a connection in the primary and mixed dentitions? Clin. Oral Investig. 2004, 8, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Infante, P.F. An epidemiologic study of deciduous molar relations in preschool children. J. Dent. Res. 1975, 54, 723–727. [Google Scholar] [CrossRef] [PubMed]
- Ravn, J.J. Longitudinal study of occlusion in the primary dentition in 3- and 7-year-old children. Eur. J. Oral Sci. 1980, 88, 165–170. [Google Scholar] [CrossRef]
- Onyeaso, C.O.; Isiekwe, M.C. Occlusal changes from primary to mixed dentitions in nigerian children. Angle Orthod. 2008, 78, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Foster, T.D.; Hamilton, M.C. Occlusion in the primary dentition. Study of children at 2 and one-half to 3 years of age. Br. Dent. J. 1969, 126, 76–79. [Google Scholar] [PubMed]
- Hegde, S.; Panwar, S.; Bolar, D.R.; Sanghavi, M.B. Characteristics of occlusion in primary dentition of preschool children of Udaipur, India. Eur. J. Dent. 2012, 6, 51–55. [Google Scholar] [PubMed]
- Moyers, R.E. Standards of Human Occlusal Development; University of Michigan CHGD: Ann Arbor, MI, USA, 1976. [Google Scholar]
- Baume, L.J. Physiological tooth migration and its significance for the development of occlusion. III. The biogenesis of the successional dentition. J. Dent. Res. 1950, 29, 338–348. [Google Scholar] [CrossRef] [PubMed]
- Karjalainen, S.; Rönning, O.; Lapinleimu, H.; Simell, O. Association between early weaning, non-nutritive sucking habits and occlusal anomalies in 3-year-old Finnish children. Int. J. Paediatr. Dent. 1999, 9, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Almeida, E.R.; Narvai, P.C.; Frazão, P.; Guedes-Pinto, A.C. Revised criteria for the assessment and interpretation of occlusal deviations in the deciduous dentition: A public health perspective. Cad. Saúde Pública 2008, 24, 10148–10152. [Google Scholar] [CrossRef]
- Macena, M.C.; Katz, C.R.; Rosenblatt, A. Prevalence of a posterior crossbite and sucking habits in Brazilian children aged 18–59 months. Eur. J. Orthod. 2009, 31, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Bjoerk, A.; Krebs, A.; Solow, B. A method for epidemiological registration of malocclusion. Acta Odontol. Scand. 1964, 22, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Katz, C.R.; Rosenblatt, A.; Gondim, P.P. Nonnutritive sucking habits in Brazilian children: Effects on deciduous dentition and relationship with facial morphology. Am. J. Orthod. Dentofac. 2004, 126, 53–57. [Google Scholar] [CrossRef]
- Kerosuo, H. Occlusion in the primary and early mixed dentitions in a group of Tanzanian and Finnish children. ASDC J. Dent. Child. 1990, 57, 293–298. [Google Scholar] [PubMed]
- Jones, M.L.; Mourino, A.P.; Bowden, T.A. Evaluation of occlusion, trauma, and dental anomalies in African-American children of metropolitan headstart programs. J. Clin. Pediatr. Dent. 1993, 18, 51–54. [Google Scholar] [PubMed]
- Petrén, S.; Bondemark, L.; Söderfeldt, B. A systematic review concerning early orthodontic treatment of unilateral posterior crossbite. Angle Orthod. 2003, 73, 588–596. [Google Scholar] [PubMed]
- Bhat, S.S.; Rao, H.A.; Hegde, K.S.; Kumar, B.K. Characteristics of primary dentition occlusion in preschool children: An epidemiological study. Int. J. Clin. Pediatr. Dent. 2012, 5, 93–97. [Google Scholar]
- Farsi, N.M.A.; Salama, F.S. Characteristics of primary dentition occlusion in a group of Saudi children. Int. J. Paediatr. Dent. 1996, 6, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Otuyemi, O.D.; Sote, E.O.; Isiekwe, M.C.; Jones, S.P. Occlusal relationships and spacing or crowding of teeth in the dentitions of 3–4-year-old Nigerian children. Int. J. Paediatr. Dent. 1997, 7, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Góis, E.G.; Ribeirojúnior, H.C.; Vale, M.P.; Paiva, S.M.; Serranegra, J.M.; Ramosjorge, M.L.; Pordeus, I.A. Influence of nonnutritive sucking habits, breathing pattern and adenoid size on the development of malocclusion. Angle Orthod. 2008, 78, 647–654. [Google Scholar] [CrossRef]
- Hermont, A.P. Breastfeeding, bottle feeding practices and malocclusion in the primary dentition: A systematic review of cohort studies. Int. J. Environ. Res. Public Health 2015, 12, 3133–3151. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, J.C.; Vinker, F.; Declerck, D. Malocclusion, dental injuries and dental anomalies in the primary dentition of Belgian children. Int. J. Paediatr. Dent. 1998, 8, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Borzabadi-Farahani, A.; Eslamipour, F. An investigation into the association between facial profile and maxillary incisor trauma, a clinical non-radiographic study. Dent. Traumatol. 2010, 26, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Borzabadi-Farahani, A. The association between orthodontic treatment need and maxillary incisor trauma, a retrospective clinical study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, e75–e80. [Google Scholar] [CrossRef] [PubMed]
- Bastone, E.B.; Freer, T.J.; McNamara, J.R. Epidemiology of dental trauma: A review of the literature. Aust. Dent. J. 2000, 45, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.S.; Lee, K.H. Intrusion of over-erupted molars by corticotomy and magnets. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Prabhakar, R.R.; Saravanan, R.; Karthikeyan, M.K.; Vishnuchandran, C.; Sudeepthi. Prevalence of malocclusion and need for early orthodontic treatment in children. J. Clin. Diagn. Res. 2014, 8, ZC60–ZC61. [Google Scholar] [PubMed]
- Taslan, S.; Biren, S.; Ceylanoglu, C. Tongue pressure changes before, during and after crib appliance therapy. Angle Orthod. 2010, 80, 533–539. [Google Scholar] [CrossRef] [PubMed]
| Age & Gender | n | Normal Occlusion | Malocclusion | p | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Age | 0.121 | |||||
| 3 | 846 | 124 | 14.7 | 722 | 85.3 | |
| 4 | 728 | 112 | 15.4 | 616 | 84.6 | |
| 5 | 761 | 139 | 18.3 | 622 | 81.7 | |
| Gender | 0.886 | |||||
| Boys | 1247 | 199 | 53.1 | 1048 | 53.5 | |
| Girls | 1088 | 176 | 46.9 | 912 | 46.5 | |
| Total | 2335 | 375 | 16.1 | 1960 | 83.9 | |
| Sagittal Occlusal Characteristic | Age 3 (Year) | Age 4 (Year) | Age 5 (Year) | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Canine relationship | |||||||||
| Normal (class I) | 496 | 58.6 | 415 | 57.0 | 419 | 55.1 | 1330 | 57.0 | |
| Distal (class II) | 254 | 30.0 | 239 | 32.8 | 264 | 34.7 | 757 | 32.4 | |
| Mesial (class III) | 83 | 9.8 | 69 | 9.5 | 75 | 9.9 | 227 | 9.7 | |
| Mix 1 | 13 | 1.5 | 5 | 0.7 | 3 | 0.4 | 21 | 0.9 | |
| Second deciduous molar terminal plane | |||||||||
| Bilateral symmetry | 751 | 88.8 | 643 | 88.3 | 671 | 88.2 | 2065 | 88.4 | |
| Flush | 332 | 39.2 | 265 | 36.4 | 306 | 40.2 | 903 | 38.7 | |
| Distal | 70 | 8.3 | 129 | 17.7 | 65 | 8.5 | 264 | 11.3 | |
| Mesial | 349 | 41.3 | 249 | 32.7 | 300 | 39.4 | 898 | 38.5 | |
| Deep overjet | 294 | 34.8 | 264 | 36.3 | 233 | 30.6 | 791 | 33.9 | |
| Edge to edge | 16 | 1.9 | 15 | 2.1 | 23 | 3.0 | 54 | 2.3 | |
| Mild (>3 mm, ≤5 mm) | 222 | 26.2 | 202 | 27.7 | 183 | 24.0 | 607 | 26.0 | |
| Moderate (>5 mm, ≤8 mm) | 61 | 7.2 | 58 | 8.0 | 43 | 5.7 | 162 | 6.9 | |
| Severe (>8 mm) | 11 | 1.3 | 4 | 0.5 | 7 | 0.9 | 22 | 0.9 | |
| Anterior crossbite | 68 | 8.0 | 49 | 6.7 | 70 | 9.2 | 187 | 8.0 | |
| Vertical Anomalies | Age 3 (Year) | Age 4 (Year) | Age 5 (Year) | Total | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Deep overbite | 532 | 62.9 | 499 | 68.5 | 457 | 60.1 | 1488 | 63.7 |
| Mild (>1/2, ≤3/4) | 204 | 24.1 | 172 | 23.6 | 144 | 18.9 | 520 | 22.3 |
| Moderate (>3/4, <1) | 202 | 23.9 | 224 | 30.8 | 185 | 24.3 | 611 | 26.2 |
| Severe (all cover) | 126 | 14.9 | 103 | 14.1 | 128 | 16.8 | 357 | 15.3 |
| Open bite | 5 | 0.6 | 3 | 0.4 | 2 | 0.3 | 10 | 0.4 |
| Moderate (>3 mm, ≤5 mm) | 4 | 0.5 | 3 | 0.4 | 1 | 0.1 | 8 | 0.3 |
| Severe (>5 mm) | 1 | 0.1 | 0 | 0.0 | 1 | 0.1 | 2 | 0.1 |
| Transversal Anomalies | Age 3 (Year) | Age 4 (Year) | Age 5 (Year) | Total | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Midline displacement | 224 | 26.5 | 190 | 26.1 | 206 | 27.1 | 620 | 26.6 |
| Posterior Teeth Malocclusion | ||||||||
| Posterior crossbite | 1 | 0.1 | 5 | 0.7 | 0 | 0.0 | 6 | 0.3 |
| Edge to edge | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Scissors bite | 3 | 0.4 | 2 | 0.3 | 2 | 0.3 | 7 | 0.3 |
| Opposite Scissors bite | 0 | 0.0 | 1 | 0.1 | 0 | 0.0 | 1 | 0.0 |
| Anterior Teeth Malocclusion | Age 3 (Year) | Age 4 (Year) | Age 5 (Year) | Total | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Crowding | 46 | 5.4 | 33 | 4.5 | 72 | 9.5 | 151 | 6.5 |
| Maxillary | 38 | 4.5 | 17 | 2.3 | 23 | 3.0 | 78 | 3.3 |
| >2 mm, ≤4 mm | 36 | 4.3 | 15 | 2.1 | 19 | 2.5 | 70 | 3.0 |
| >4 mm | 2 | 0.2 | 2 | 0.3 | 4 | 0.5 | 8 | 0.3 |
| Mandibular | 59 | 7.0 | 26 | 3.6 | 61 | 8.0 | 146 | 6.3 |
| >2 mm, ≤4 mm | 56 | 6.6 | 21 | 2.9 | 55 | 7.2 | 132 | 5.7 |
| >4 mm | 3 | 0.4 | 5 | 0.7 | 6 | 0.8 | 14 | 0.6 |
| Spacing | 349 | 41.3 | 348 | 47.8 | 349 | 45.9 | 1046 | 44.8 |
| Maxillary | 306 | 36.2 | 317 | 43.5 | 297 | 39.0 | 920 | 39.4 |
| >2 mm, ≤4 mm | 168 | 19.9 | 173 | 23.8 | 157 | 20.6 | 498 | 21.3 |
| >4 mm | 138 | 16.3 | 144 | 19.8 | 140 | 18.4 | 422 | 18.1 |
| Mandibular | 211 | 24.9 | 204 | 28.0 | 221 | 29.0 | 636 | 27.2 |
| >2 mm, ≤4 mm | 144 | 17.0 | 133 | 18.3 | 152 | 20.0 | 429 | 18.4 |
| >4 mm | 67 | 7.9 | 71 | 9.8 | 69 | 9.1 | 207 | 8.9 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, X.; Zhang, Y.; Wang, Y.; Zhang, H.; Chen, L.; Liu, Y. Prevalence of Malocclusion in 3- to 5-Year-Old Children in Shanghai, China. Int. J. Environ. Res. Public Health 2017, 14, 328. https://doi.org/10.3390/ijerph14030328
Zhou X, Zhang Y, Wang Y, Zhang H, Chen L, Liu Y. Prevalence of Malocclusion in 3- to 5-Year-Old Children in Shanghai, China. International Journal of Environmental Research and Public Health. 2017; 14(3):328. https://doi.org/10.3390/ijerph14030328
Chicago/Turabian StyleZhou, Xinhua, Ying Zhang, Yan Wang, Hao Zhang, Li Chen, and Yuehua Liu. 2017. "Prevalence of Malocclusion in 3- to 5-Year-Old Children in Shanghai, China" International Journal of Environmental Research and Public Health 14, no. 3: 328. https://doi.org/10.3390/ijerph14030328





