1. Introduction
Hypertension is a major global health issue due to its magnitude and associated risks, difficulty of control, high medical and social costs, and the fact that it causes severe cardiovascular and renal complications [
1]. In 2010, hypertension caused 9.4 million deaths and led to the loss of 7% disability-adjusted life years [
2]. It has been proposed that non-communicable cardiovascular diseases (CVDs) will be the global leading cause of death and disability by 2020 [
3], and the number of hypertensive adults will reach 1.5 billion (approximately 30% of the world population) by 2025 [
4]. In addition to known risk factors for hypertension, such as prior family history, obesity, tobacco use, alcohol consumption, and a high intake of sodium [
5]; multiple factors, including age, gender, blood glucose, triglycerides, total cholesterol, high-density and low-density lipoprotein levels, are also closely correlated with the incidence of hypertension [
6,
7]. While genetic and behavioral factors leading to hypertension have been intensely studied, the etiology of hypertension is still largely unknown.
In recent years, agricultural and industrial advances have impacted lifestyle and social interaction, leading to greater psychological pressure. Epidemiologic studies have shown the workplace to be a high-pressure environment. The imbalance between work demand and work control in modern society is considered to be an important risk factor for hypertension in men [
8] and women [
9]. A recent study has demonstrated that long-term and excessive occupational stress promotes a number of unhealthy behaviors, such as cigarette smoking, alcohol consumption, high-fat diets, drug abuse, and a sedentary lifestyle [
10], which are all risk factors for hypertension.
Occupational stress combined with other risk factors is associated with a higher incidence of hypertension compared to occupational stress alone [
11]. Furthermore, there is an interaction between occupational stress and other risk factors, such as gender, age, alcohol consumption, and obesity, leading to hypertension [
11]. A cohort study conducted by Wiernik et al. [
12,
13], which included 122,816 adults, found that for women with a relatively low occupational status, occupational stress is a potential risk factor for hypertension. Additionally, the effects of stress are being studied in additional areas, such as marriage and low socioeconomic status. Associations between these other risk types and blood pressure (BP) outcomes have been reported, but the results vary, and ongoing exposure to stress may be more plausibly linked to sustained BP elevation and incidence of hypertension [
14]. However, occupational stress has also been identified as an independent risk factor for hypertension [
15,
16].
Previous studies often applied a cross-sectional approach and short-term follow-up to explore the relationship between occupational stress and blood pressure. In China, relevant studies have only recently been completed and cross-sectional studies have been limited. In addition, the cultural background, labor organization, and sources of stress in China differ from other countries. Therefore, the role of occupational stress in hypertension amongst the Chinese working population warrants more specific studies. The objective of this study was to investigate the correlation between occupational stress and hypertension in oil workers in Kelamayi City through a prospective cohort study.
4. Discussion
Oil workers in Kelamayi City of Xinjiang, China, have higher occupational stress and a high intensity of work that is associated with abnormal blood lipids, blood glucose, and immune function [
23,
24]. In the current study, we identified that the occupational stress of oil workers was higher than the Chinese general population [
25], with a total of 231 subjects developing hypertension during the study period, thus representing a 17.06% cumulative incidence. Wang et al. reported that the prevalence of hypertension was 29.6% in the Chinese general population in 2009 [
26] and a cohort study by Wiernik et al. reported that in France the prevalence of hypertension was 27.0% from 1996 to 2007 [
12]. The study participants who were male, older, worked a long number of years, smoked cigarettes, consumed alcohol, and were overweight had a higher incidence of hypertension. Previous studies have shown that the incidence of hypertension is primarily associated with age, gender, BMI, cigarette smoking, and genetic factors [
27,
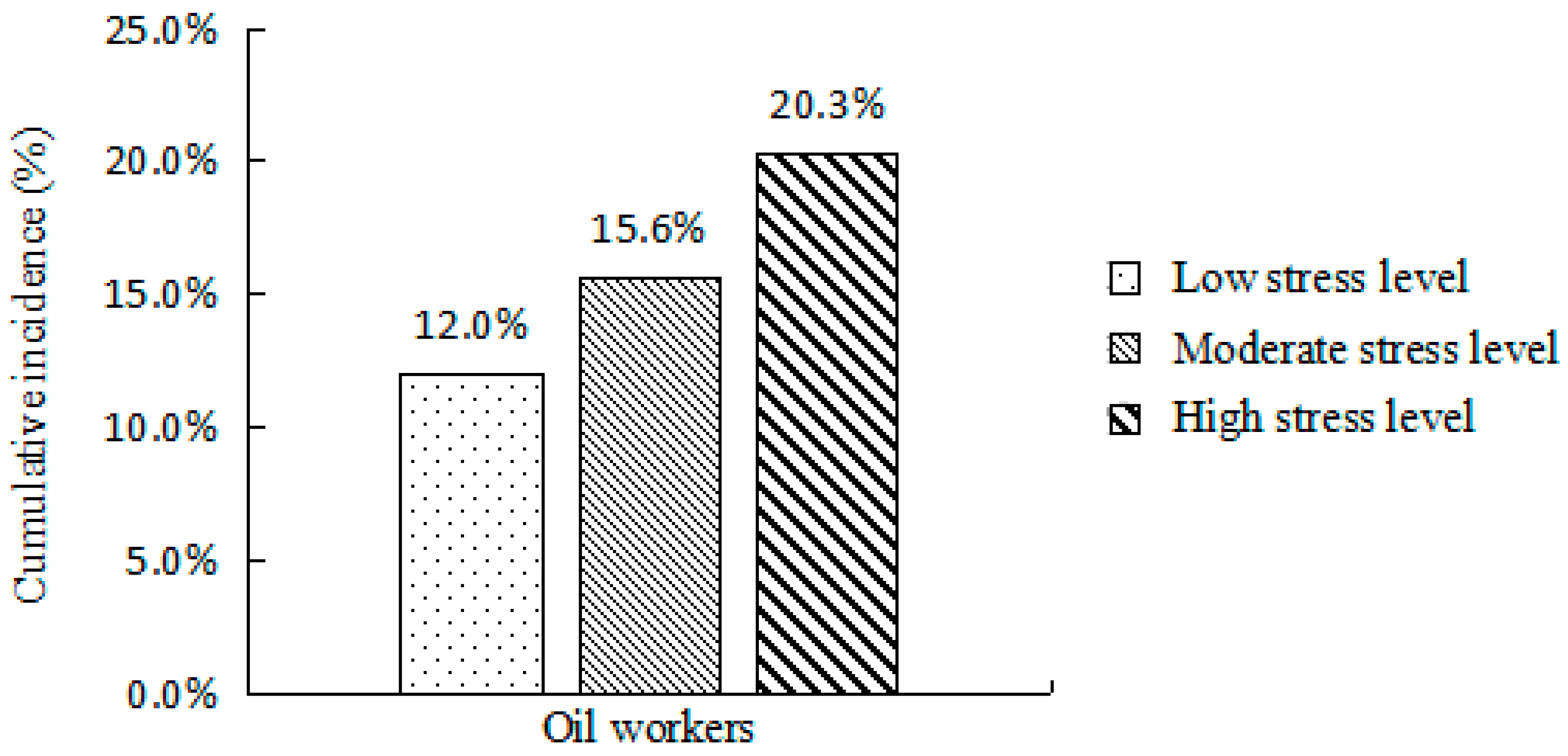
28]. In this study there were 44, 112, and 75 new cases of hypertension in the low, intermediate, and high occupational stress groups, which represented a 12.0%, 15.6%, and 20.3% cumulative incidence, respectively. The scores of occupational role and personal strain of the subjects with hypertension were significantly higher than for subjects without hypertension. Moreover, the incidence of hypertension was positively correlated with occupational stress. Our study is in agreement with previous studies [
29,
30] and further supports the notion that high occupational stress in oil workers could increase the risk of hypertension. A multivariate Cox proportional hazards model showed that type of work, cigarette smoking, excess body weight, and obesity are risk factors that increase the incidence of hypertension. After adjustment for confounding factors, such as type of work, cigarette smoking, alcohol consumption, and BMI, the HR of high occupational stress was 1.549 (1.072–2.236) compared to the low-exposure group, and 2.337 (1.191–4.585) in female subjects. Our results are consistent with Wiernik et al. [
12], who included 122,816 adult subjects (average age, 46.8 ± 9.9; and male subjects, 69.2%) and concluded that occupational stress is associated with the incidence of hypertension (OR = 1.06, 95% CI = 1.03–1.09) after other factors, except occupational status, were adjusted.
Why do the oil workers have the high prevalence of both hypertension and occupational stress? With the increase in the demand of oil in China, the expansion of personnel cannot satisfy the demand, which leads to a continuous increase in the workload of oil workers. The working conditions for oil workers can be harsh, working in an oilfield that is far from a city and often in the desert requires they often live in the staff dormitory for work in the field, leading to long-term separation from families and development of negative psychological states including loneliness, anxiety, and depression. Meanwhile, mechanical automation is constantly improving, requiring oil workers to acquire new knowledge and techniques by enrolling in training courses in their spare time, further increasing their physical and psychological stress. An unhealthy lifestyle, such as irregular diet, excessive alcohol consumption, cigarette smoking, and other unhealthy behaviors, is also common in the oil worker population. All of these factors have a negative impact on the physical and mental health of oil workers. In severe circumstances, the workers may develop sleep disorders, physical pain, or other symptoms seriously affecting their work and lives.
We recognize that there are limitations associated with our study. The follow-up time was relatively short and approximately 7% of subjects were censored, which may have influenced the results. Moreover, hypertension is associated with genetic and environmental factors. In this study, we focused our investigation on occupational stress (occupational psychological factors in the work environment), with genetic factors as well as the interaction between genetic factors and the environment not covered. Furthermore, occupational stress is a form of chronic psychological stress, promoting constant stimulation of the hypothalamus-pituitary-adrenal (HPA) axis leading to accelerated secretion of adrenaline, norepinephrine and other substances. These substances can increase blood pressure, heart and respiratory rate, and when secreted and accumulated in an abnormal manner this can lead to metabolic disorders.
Important advantages of this study include the following: (1) The subjects were oil workers in a special work environment, and the sample size was large; (2) Preliminary studies provided reliable supporting data for the present study; (3) In addition to occupational stress, the current study also investigated other lifestyle factors that may affect the incidence of hypertension. By controlling other confounding factors, the study clarified the relationship between occupational stress and hypertension.
The correlation between occupational stress and the pathogenesis of hypertension revealed in this study may have an important impact on the health of the population. At the population level, a decrease of 2 mmHg from the average SBP reduces the number of deaths due to stroke and cardiovascular diseases by approximately 10% and 7%, respectively [
31]. Therefore, applying active and effective measures to reduce the levels of these risk factors will have a significantly beneficial effect on public health.