Comparison of the Combined Obesity Indices to Predict Cardiovascular Diseases Risk Factors and Metabolic Syndrome in Northeast China
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Ethics Statement
2.3. Data Measurement
2.4. Assessment Criteria
2.5. Statistical Analyses
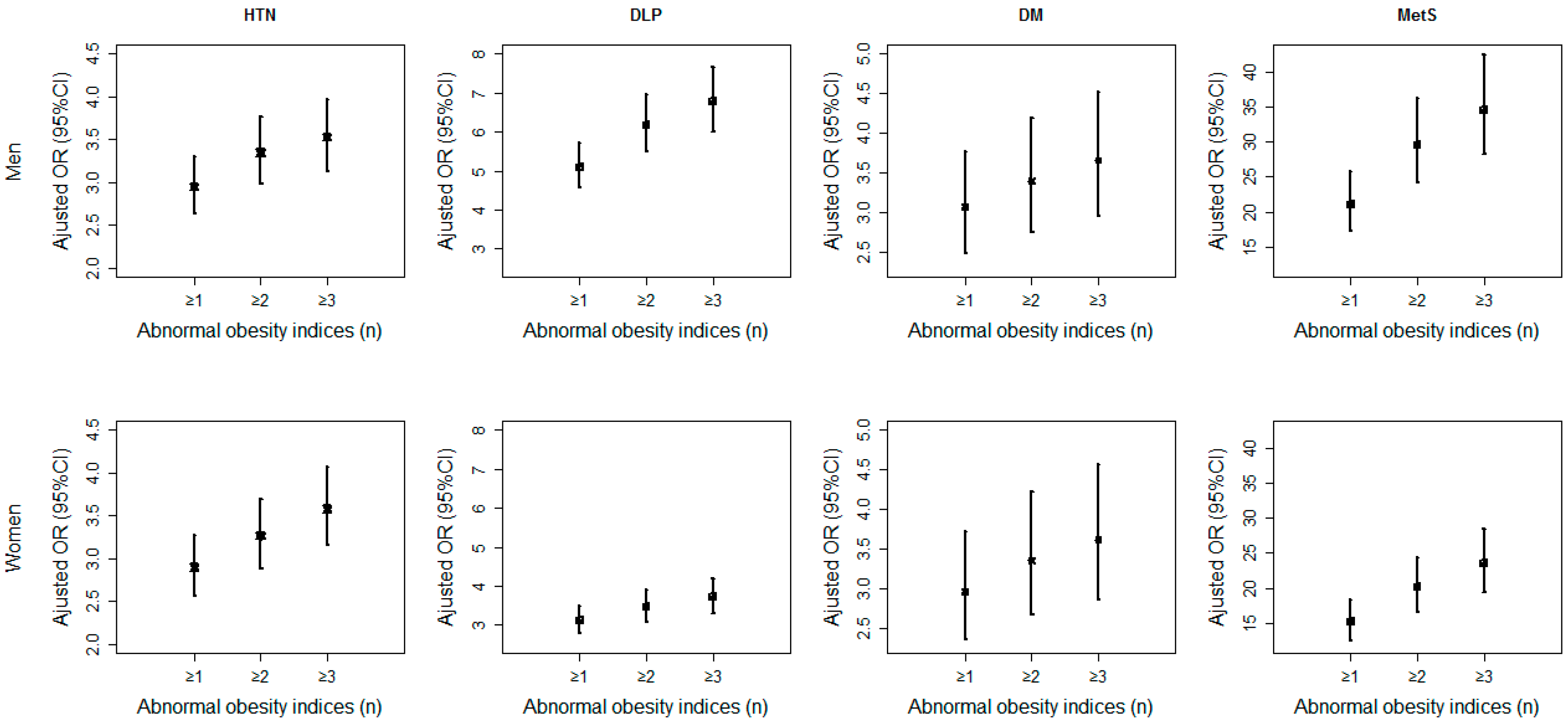
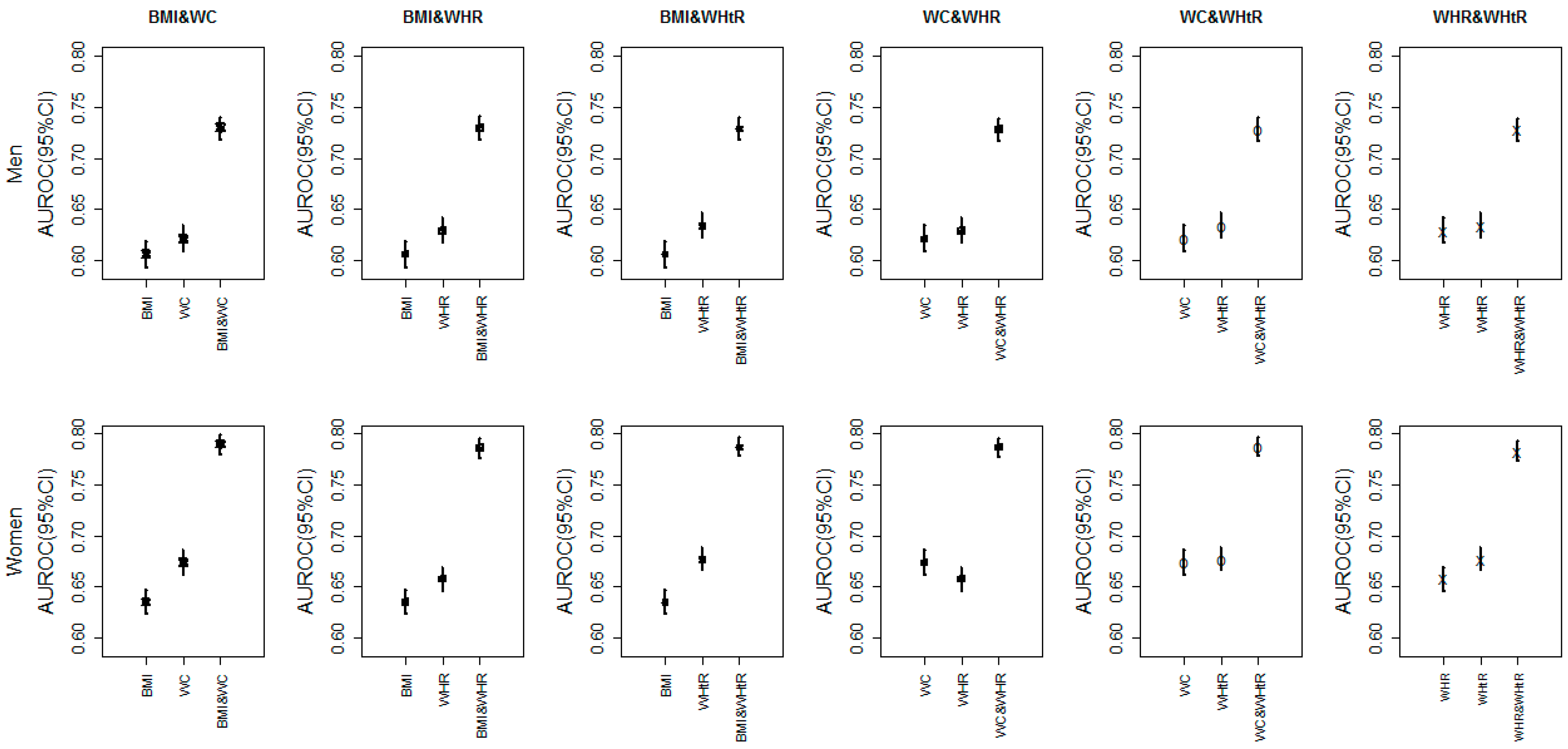
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| WC | waist circumference |
| BMI | body mass index |
| WHR | waist-hip ratio |
| WHtR | waist-to-height ratio |
| HC | hip circumference |
| BAI | body adiposity index |
| SBP | systolic blood pressure |
| DBP | diastolic blood pressure |
| TC | total cholesterol |
| TG | triglyceride |
| LDL-C | low-density lipoprotein cholesterol |
| HDL-C | high-density lipoprotein cholesterol |
| FBG | fasting blood glucose |
| CVD | cardiovascular disease |
| HTN | hypertension |
| DLP | dyslipidemia |
| DM | diabetes mellitus |
| MetS | metabolic syndrome |
| OR | odds ratio |
| CI | confidence interval |
| ROC | receiver operating characteristic curve |
| AUROC | area under ROC |
References
- Wang, Z.; Hao, G.; Wang, X.; Chen, Z.; Zhang, L.; Guo, M.; Tian, Y.; Shao, L.; Zhu, M. Current prevalence rates of overweight, obesity, central obesity, and related cardiovascular risk factors that clustered among middle-aged population of China. Zhonghua Liu Xing Bing Xue Za Zhi 2014, 35, 354–358. (In Chinese) [Google Scholar] [PubMed]
- Andegiorgish, A.K.; Wang, J.; Zhang, X.; Liu, X.; Zhu, H. Prevalence of overweight, obesity, and associated risk factors among school children and adolescents in Tianjin, China. Eur. J. Pediatr. 2012, 171, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Dankel, S.J.; Loenneke, J.P.; Loprinzi, P.D. The impact of overweight/obesity duration on the association between physical activity and cardiovascular disease risk: An application of the “fat but fit” paradigm. Int. J. Cardiol. 2015, 201, 88–89. [Google Scholar] [CrossRef] [PubMed]
- Roberts, V.H.J.; Frias, A.E.; Grove, K.L. Impact of maternal obesity on fetal programming of cardiovascular disease. Physiology 2015, 30, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Chang, H.J.; Sung, J.; Kim, K.J.; Shin, S.; Cho, I.J.; Shim, C.Y.; Hong, G.R.; Chung, N. The impact of obesity on subclinical coronary atherosclerosis according to the risk of cardiovascular disease. Obesity 2014, 22, 1762–1768. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; McDermott, R.A. Using anthropometric indices to predict cardio-metabolic risk factors in Australian indigenous populations. Diabetes Res. Clin. Pract. 2010, 87, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Liu, Y.; Yang, J.; Sun, Y.; Chen, L. Efficiency of anthropometric indicators of obesity for identifying cardiovascular risk factors in a Chinese population. Postgrad. Med. J. 2011, 87, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Choi, S.J.; Lee, K.S.; Park, H.Y. Waist circumference and waist-to-height ratio as predictors of cardiovascular disease risk in Korean adults. Circ. J. 2009, 73, 1643–1650. [Google Scholar] [CrossRef] [PubMed]
- Lam, B.C.C.; Koh, G.C.H.; Chen, C.; Wong, M.T.K.; Fallows, S.J. Comparison of body mass index (BMI), body adiposity index (BAI), waist circumference (WC), waist-to-hip ratio (WHR) and waist-to-height ratio (WHTR) as predictors of cardiovascular disease risk factors in an adult population in Singapore. PLoS ONE 2015, 10, e0122985. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Sui, X.M.; Lavie, C.J.; Blair, S.N. Body mass index, the most widely used but also widely criticized index: Would a criterion standard measure of total body fat be a better predictor of cardiovascular disease mortality? Mayo Clin. Proc. 2016, 91, 443–455. [Google Scholar] [CrossRef] [PubMed]
- Bennasar-Veny, M.; Lopez-Gonzalez, A.A.; Tauler, P.; Cespedes, M.L.; Vicente-Herrero, T.; Yanez, A.; Tomas-Salva, M.; Aguilo, A. Body adiposity index and cardiovascular health risk factors in Caucasians: A comparison with the body mass index and others. PLoS ONE 2013, 8, e63999. [Google Scholar]
- Cai, L.; Liu, A.P.; Zhang, Y.M.; Wang, P.Y. Waist-to-height ratio and cardiovascular risk factors among Chinese adults in Beijing. PLoS ONE 2013, 8, e69298. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Hsieh, S.D. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int. J. Food Sci. Nutr. 2005, 56, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Mbanya, V.N.; Kengne, A.P.; Mbanya, J.C.; Akhtar, H. Body mass index, waist circumference, hip circumference, waist-hip-ratio and waist-height-ratio: Which is the better discriminator of prevalent screen-detected diabetes in a Cameroonian population? Diabetes Res. Clin. Pract. 2015, 108, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Bergman, R.N.; Stefanovski, D.; Buchanan, T.A.; Sumner, A.E.; Reynolds, J.C.; Sebring, N.G.; Xiang, A.H.; Watanabe, R.M. A better index of body adiposity. Obesity 2011, 19, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.; He, Y.; Dong, S.Y.; Zhao, X.L.; Chen, Z.H.; Song, Z.Y.; Chang, G.; Yang, F.; Wang, Y.J. Optimal cut-off values of BMI, waist circumference and waist: Height ratio for defining obesity in Chinese adults. Br. J. Nutr. 2014, 112, 1735–1744. [Google Scholar] [CrossRef] [PubMed]
- Gao, B.; Xu, Q.T.; Li, Y.B. Dynamic change and analysis of driving factors of carbon emissions from traffic and transportation energy consumption in Jilin Province. Appl. Mech. Mater. 2014, 472, 851–855. [Google Scholar] [CrossRef]
- Yip, G.W.; Li, A.M.; So, H.K.; Choi, K.C.; Leung, L.C.; Fong, N.C.; Lee, K.W.; Li, S.P.; Wong, S.N.; Sung, R.Y. Oscillometric 24-h ambulatory blood pressure reference values in Hong Kong Chinese children and adolescents. J. Hypertens. 2014, 32, 606–619. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.F.; Gupta, A.; Muntner, P.; Hu, S.S.; Duan, X.F.; Chen, J.C.; Reynolds, R.F.; Whelton, P.K.; He, J. Prevalence of cardiovascular disease risk factor clustering among the adult population of China—Results from the international collaborative study of cardiovascular disease in Asia (Interasia). Circulation 2005, 112, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Gao, B.X.; Zhang, L.X.; Wang, H.Y.; China National Survey of Chronic Kidney Disease Working Group. Clustering of major cardiovascular risk factors and the association with unhealthy lifestyles in the Chinese adult population. PLoS ONE 2013, 8, e66780. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Yu, S.; Wang, S.; Shi, J.; Xu, Z.; Zhang, Q.; Fu, Y.; Qi, Y.; Liu, J.; Fu, R.; et al. Zinc finger protein 259 (ZNF259) polymorphisms are associated with the risk of metabolic syndrome in a Han Chinese population. Clin. Lab. 2015, 61, 615–621. [Google Scholar] [PubMed]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 Could be a suitable global boundary value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.F. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—Study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. BES 2002, 15, 83–96. [Google Scholar] [PubMed]
- Appropriate body-mass index for asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163.
- Ford, E.S.; Giles, W.H.; Dietz, W.H. Prevalence of the metabolic syndrome among us adults—Findings from the third national health and nutrition examination survey. JAMA 2002, 287, 356–359. [Google Scholar] [CrossRef] [PubMed]
- Ezquerra, E.A.; Vazquez, J.M.C.; Barrero, A.A. Obesity, metabolic syndrome and diabetes: Cardiovascular implications and therapy. Rev. Esp. Cardiol. 2008, 61, 752–764. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the metabolic syndrome a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; american heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Wang, S.H.; Wang, L.; Zhou, Y.; Guo, Y.J.; Yuan, Y.; Li, F.F.; Huang, Y.; Xia, W.Q. Prevalence and control of dyslipidaemia among diabetic patients with microalbuminuria in a Chinese hospital. Diabetes Vasc. Dis. Res. 2013, 10, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Palazon-Bru, A.; Gil-Guillen, V.F.; Orozco-Beltran, D.; Pallares-Carratala, V.; Valls-Roca, F.; Sanchis-Domenech, C.; Martin-Moreno, J.M.; Redon, J.; Navarro-Perez, J.; Fernandez-Gimenez, A.; et al. Is the physician’s behavior in dyslipidemia diagnosis in accordance with guidelines? Cross-sectional escarval study. PLoS ONE 2014, 9, e91567. [Google Scholar] [CrossRef] [PubMed]
- Executive summary: Standards of medical care in diabetes—2012. Diabetes Care 2012, 35, S4–S10.
- Bian, S.S.; Gao, Y.X.; Zhang, M.L.; Wang, X.; Liu, W.Q.; Zhang, D.L.; Huang, G.W. Dietary nutrient intake and metabolic syndrome risk in Chinese adults: A case-control study. Nutr. J. 2013, 12, 106. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; de Courten, M.; Jiao, S.F.; Wang, Y. Prevalence and characteristics of the metabolic syndrome among adults in Beijing, China. Asia Pac. J. Clin. Nutr. 2010, 19, 98–102. [Google Scholar] [PubMed]
- Chen, J.; Gu, D.F.; Huang, J.F.; Rao, D.C.; Jaquish, C.E.; Hixson, J.E.; Chen, C.S.; Chen, J.C.; Lu, F.H.; Hu, D.S.; et al. Metabolic syndrome and salt sensitivity of blood pressure in non-diabetic people in China: A dietary intervention study. Lancet 2009, 373, 829–835. [Google Scholar] [CrossRef]
- Yu, J.X.; Ma, Y.H.; Yang, S.; Pang, K.; Yu, Y.Q.; Tao, Y.C.; Jin, L.N. Risk factors for cardiovascular disease and their clustering among adults in Jilin (China). Int. J. Environ. Res. Pubulic Health 2016, 13. [Google Scholar] [CrossRef] [PubMed]
- Bastien, M.; Poirier, P.; Lemieux, I.; Despres, J.P. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog. Cardiovasc. Dis. 2014, 56, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Gunn, P.; Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2012, 13, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, S.D.; Muto, T. The superiority of waist-to-height ratio as an anthropometric index to evaluate clustering of coronary risk factors among non-obese men and women. Prev. Med. 2005, 40, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Can, A.S.; Bersot, T.P.; Gonen, M. Anthropometric indices and their relationship with cardiometabolic risk factors in a sample of Turkish adults. Public Health Nutr. 2009, 12, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Oanh, T.H.T.; Nguyen, D.N.; Phongsavan, P.; Dibley, M.J.; Bauman, A.E. Prevalence and risk factors with overweight and obesity among Vietnamese adults: Caucasian and Asian cut-offs. Asia Pac. J. Clin. Nutr. 2009, 18, 226–233. [Google Scholar]
- Zhu, S.K.; Heshka, S.; Wang, Z.M.; Shen, W.; Allison, D.B.; Ross, R.; Heymsfield, S.B. Combination of BMI and waist circumference for identifying cardiovascular risk factors in whites. Obes. Res. 2004, 12, 633–645. [Google Scholar] [CrossRef] [PubMed]
- Du, S.M.; Ma, G.S.; Li, Y.P.; Fang, H.Y.; Hu, X.Q.; Yang, X.G.; Hu, Y.H. Relationship of body mass index, waist circumference and cardiovascular risk factors in Chinese adult. Biomed. Environ. Sci. 2010, 23, 92–101. [Google Scholar] [CrossRef]
- Ricketts, T.A.; Sui, X.M.; Lavie, C.J.; Blair, S.N.; Ross, R. Addition of cardiorespiratory fitness within an obesity risk classification model identifies men at increased risk of all-cause mortality. Am. J. Med. 2016, 129, e13–e20. [Google Scholar] [CrossRef] [PubMed]
- Barry, V.W.; Baruth, M.; Beets, M.W.; Durstine, J.L.; Liu, J.H.; Blair, S.N. Fitness vs. fatness on all-cause mortality: A meta-analysis. Prog. Cardiovasc. Dis. 2014, 56, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Milani, R.V.; Ventura, H.O. Effects of obesity and weight changes on cardiac and vascular structure and function does the clinical impact carry any weight? JACC Heart Fail. 2014, 2, 509–511. [Google Scholar] [CrossRef] [PubMed]
- McAuley, P.A.; Beavers, K.M. Contribution of cardiorespiratory fitness to the obesity paradox. Prog. Cardiovasc. Dis. 2014, 56, 434–440. [Google Scholar] [CrossRef] [PubMed]
- DeFina, L.F.; Haskell, W.L.; Willis, B.L.; Barlow, C.E.; Finley, C.E.; Levine, B.D.; Cooper, K.H. Physical activity versus cardiorespiratory fitness: Two (partly) distinct components of cardiovascular health? Prog. Cardiovasc. Dis. 2015, 57, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.; McAuley, P.; Lavie, C.J.; Despres, J.P.; Arena, R.; Kokkinos, P. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: Their independent and interwoven importance to health status. Prog. Cardiovasc. Dis. 2015, 57, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; De Schutter, A.; Parto, P.; Jahangir, E.; Kokkinos, P.; Ortega, F.B.; Arena, R.; Milani, R.V. Obesity and prevalence of cardiovascular diseases and prognosis-the obesity paradox updated. Prog. Cardiovasc. Dis. 2016, 58, 537–547. [Google Scholar] [CrossRef] [PubMed]

| Index | Cut-off | Category | Abbreviation |
|---|---|---|---|
| BMI | 24 | BMI ≤ 24 kg/m2 | BMI0 |
| BMI > 24 kg/m2 | BMI1 | ||
| WC | 85 (male) | WC ≤ 85(male) or WC ≤ 80 (female) | WC0 |
| 80 (female) | WC > 85(male) or WC > 80 (female) | WC1 | |
| WHR | 0.88 (male) | WHR ≤ 0.88(male) or WHR ≤ 0.85 (female) | WHR0 |
| 0.85 (female) | WHR > 0.88(male) or WHR > 0.85 (female) | WHR1 | |
| WHtR | 0.5 | WHtR ≤ 0.5 | WHtR0 |
| WHtR > 0.5 | WHtR1 |
| Variable | All | Male | Female | t/χ2 | p-Value |
|---|---|---|---|---|---|
| (n = 16,766) | (n = 7697) | (n = 9069) | |||
| Age (year) | 47.80 ± 13.18 | 47.00 ± 13.74 | 48.47 ± 12.66 | −7.20 | <0.001 |
| BMI1 | 8467 (50.50%) | 3982 (51.73%) | 4485 (49.45%) | 8.66 | 0.003 |
| WC1 | 8077 (48.17%) | 3651 (47.43%) | 4426 (48.80%) | 3.13 | 0.077 |
| WHR1 | 8550 (50.00%) | 4152 (53.94%) | 4398 (48.49%) | 49.45 | <0.001 |
| WHtR1 | 8826 (52.64%) | 3856 (50.10%) | 4970 (54.80%) | 36.96 | <0.001 |
| HTN | 6249 (37.27%) | 3162 (41.08%) | 3087 (34.04%) | 88.31 | <0.001 |
| DLP | 6679 (39.76%) | 3410 (44.30%) | 3269 (36.05%) | 118.44 | <0.001 |
| DM | 1688 (10.07%) | 820 (10.65%) | 868 (9.57%) | 5.39 | 0.020 |
| MetS | 5535 (33.01%) | 2638 (34.27%) | 2897 (31.94%) | 10.21 | 0.001 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tao, Y.; Yu, J.; Tao, Y.; Pang, H.; Yu, Y.; Yu, Y.; Jin, L. Comparison of the Combined Obesity Indices to Predict Cardiovascular Diseases Risk Factors and Metabolic Syndrome in Northeast China. Int. J. Environ. Res. Public Health 2016, 13, 801. https://doi.org/10.3390/ijerph13080801
Tao Y, Yu J, Tao Y, Pang H, Yu Y, Yu Y, Jin L. Comparison of the Combined Obesity Indices to Predict Cardiovascular Diseases Risk Factors and Metabolic Syndrome in Northeast China. International Journal of Environmental Research and Public Health. 2016; 13(8):801. https://doi.org/10.3390/ijerph13080801
Chicago/Turabian StyleTao, Yuchun, Jianxing Yu, Yuhui Tao, Hui Pang, Yang Yu, Yaqin Yu, and Lina Jin. 2016. "Comparison of the Combined Obesity Indices to Predict Cardiovascular Diseases Risk Factors and Metabolic Syndrome in Northeast China" International Journal of Environmental Research and Public Health 13, no. 8: 801. https://doi.org/10.3390/ijerph13080801