The Relationship between C-Reactive Protein Level and Discharge Outcome in Patients with Acute Ischemic Stroke
Abstract
:1. Introduction
2. Methods
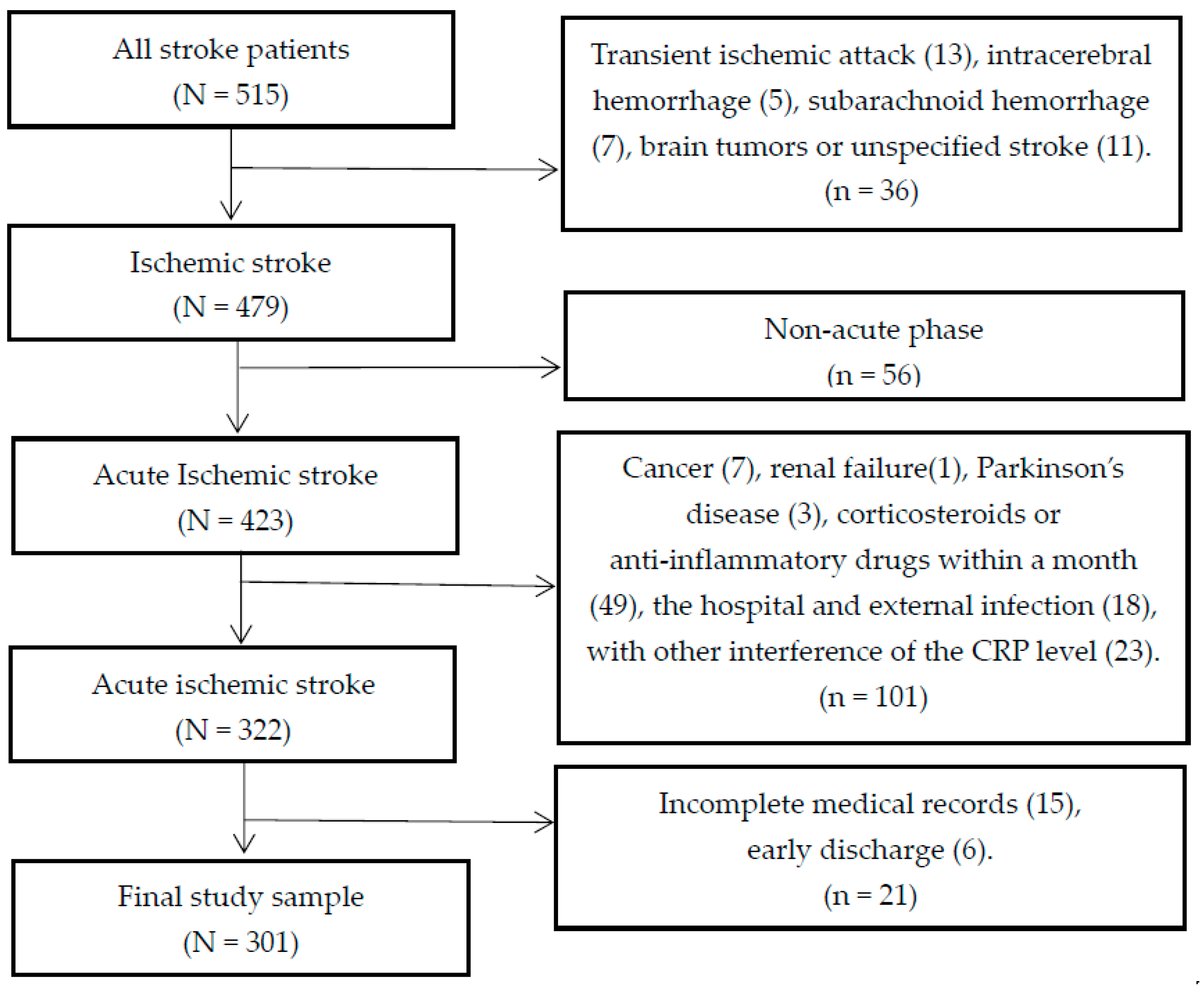
2.1. Study Population
2.2. Study Procedure
2.2.1. Sociodemographic Data and Lifestyle Variables
2.2.2. Possible Stroke-Related Clinical Parameters
2.2.3. Outcome Measurement
2.2.4. Blood Sampling
2.2.5. CRP Assay
2.3. Ethics Statement
2.4. Data Analysis
3. Results
3.1. Demographic Characteristics
3.2. Clinical Risk Factors and Blood Biochemical Indexes for Discharge Outcome
3.3. Logistic Regression Analyses
4. Discussion
Strengths and Weaknesses of the Study
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Mukherjee, D.; Patil, C.G. Epidemiology and the global burden of stroke. World Neurosurg. 2011, 76, S85–S90. [Google Scholar] [CrossRef] [PubMed]
- Bonita, R.; Mendis, S.; Truelsen, T.; Truelsen, T.; Bogousslavsky, J.; Toole, J.; Yatsu, F. The global stroke initiative. Lancet Neurol. 2004, 3, 391–393. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.; Adams, R.J.; Brown, T.M.; Carnethon, M.; Dai, S.; De Simone, G.; Ferguson, T.B.; Ford, E.; Furie, K.; Gillespie, C.; Go, A.; et al. Heart disease and stroke statistics—2010 update: A report from the American Heart Association. Circulation 2010, 121, e46–e215. [Google Scholar] [PubMed]
- Seo, W.K.; Yu, S.W.; Kim, J.H.; Park, K.W.; Koh, S.B. The impact of hyperthermia and infection on acute ischemic stroke patients in the intensive care unit. Neurocrit. Care 2008, 9, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Nakase, T.; Yamazaki, T.; Ogura, N.; Suzuki, A.; Nagata, K. The impact of inflammation on the pathogenesis and prognosis of ischemic stroke. J. Neurol. Sci. 2008, 271, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Danton, G.H.; Dietrich, W.D. Inflammatory mechanisms after ischemia and stroke. J. Neuropathol. Exp. Neurol. 2003, 62, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Di Napoli, M.; Papa, F.; Bocola, V. C-reactive protein in ischemic stroke: An independent prognostic factor. Stroke 2001, 32, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Tang, X.N.; Yenari, M.A. The inflammatory response in stroke. J. Neuroimmunol. 2007, 184, 53–68. [Google Scholar] [CrossRef] [PubMed]
- Elkind, M.S. Inflammation, atherosclerosis, and stroke. Neurologist 2006, 12, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Di Napoli, M.; Schwaninger, M.; Cappelli, R.; Ceccarelli, E.; Di Gianfilippo, G.; Donati, C.; Emsley, H.C.; Forconi, S.; Hopkins, S.J.; Masotti, L.; et al. Evaluation of C-reactive protein measurement for assessing risk and prognosis in ischemic stroke: A statement for health care professional from the CRP Pooling Project. Stroke 2005, 36, 1316–1329. [Google Scholar] [CrossRef] [PubMed]
- Pepys, M.B.; Hirschfield, G.M. C-reactive protein: A critical update. J. Clin. Investig. 2003, 111, 1805–1812. [Google Scholar] [CrossRef] [PubMed]
- Elias-Smale, S.E.; Kardys, I.; Oudkerk, M.; Hofman, A.; Witteman, J.C. C-reactive protein is related to extent and progression of coronary and extra-coronary atherosclerosis; results from the Rotterdam study. Atherosclerosis 2007, 195, e195–e202. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, H.; Kitagawa, K.; Hougaku, H.; Etani, H.; Hori, M. Relationship between C-reactive protein and progrossion of early carotidathemsclemsis in hypertensive subjects. Stroke 2004, 35, 1625–1630. [Google Scholar] [CrossRef] [PubMed]
- Pai, J.K.; Pischon, T.; Ma, J.; Manson, J.E.; Hankinson, S.E.; Joshipura, K.; Curhan, G.C.; Rifai, N.; Cannuscio, C.C.; Stampfer, M.J.; et al. Inflammatory markers and the risk of coronary heart disease in men and women. N. Engl. J. Med. 2004, 351, 2599–2610. [Google Scholar] [CrossRef] [PubMed]
- Men, X.; Li, J.; Zhang, B.; Zhang, L.; Li, H.; Lu, Z. Homocysteine and C-reactive protein associated with progression and prognosis of intracranial branch atheromatous disease. PLoS ONE 2013, 8, e73030. [Google Scholar] [CrossRef] [PubMed]
- Whiteley, W.; Chong, W.L.; Sengupta, A.; Sandercock, P. Blood markers for the prognosis of ischemic stroke: A systematic review. Stroke 2009, 40, e380–e389. [Google Scholar] [CrossRef] [PubMed]
- Pola, R. Inflammatory markers for ischaemic stroke. Thromb. Haemost. 2009, 101, 800–801. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.Q.; Kang, A.Y. Relationship of the changing amount of hs-CRP and IL-6 with ischemic stroke. J. Fourth Mil. Med. Univ. 2005, 26, 2–3. (In Chinese) [Google Scholar]
- Rost, N.S.; Wolf, P.A.; Kase, C.S.; Kelly-Hayes, M.; Silbershatz, H.; Massaro, J.M.; D'Agostino, R.B.; Franzblau, C.; Wilson, P.W. Plasma concentration of CRP and risk of ischaemic stroke and transient ischaemic attack: Framinghan study. Stroke 2001, 32, 2575–2579. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, P.M.; Howard, S.C.; Power, D.A.; Gutnikov, S.A.; Algra, A.; Gijn, J.; Clark, T.G.; Murphy, M.F.; Warlow, C.P. Fibrinogen concentration and risk of ischemic stroke and acute coronary events in 5113 patients with transient ischemic attack and minor ischemic stroke. Stroke 2004, 35, 2300–2305. [Google Scholar] [CrossRef] [PubMed]
- Elkind, M.S.; Tai, W.; Coates, K.; Paik, M.C.; Sacco, R.L. High-sensitivity C-reactive protein, lipoprotein-associated phospholipase A2, and outcome after ischemic stroke. Arch. Intern. Med. 2006, 166, 2073–2080. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.R.; Choi, I.S.; Bian, R.X.; Kim, J.H.; Han, J.Y.; Lee, S.G. The effect of C-reactive protein on functional outcome in ischemic stroke patients. Int. J. Neurosci. 2009, 119, 336–344. [Google Scholar] [CrossRef] [PubMed]
- Masotti, L.; Ceccarelli, E.; Forconi, S.; Cappelli, R. Prognostic role of C-reactive protein in very old patients with acute ischemic stroke. J. Intern. Med. 2005, 258, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Hertog, H.M.; Rossum, J.A.; Worp, H.B.; Gemert, H.M.; Jonge, R.; Koudstaal, P.J.; Dippel, D.W. C-reactive protein in the very early phase of acute ischemic stroke: Association with poor outcome and death. J. Neurol. 2009, 256, 2003–2008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abubakar, S.A.; Okubadejo, N.U.; Ojo, O.O.; Oladipo, O.; Ojini, F.I.; Danesi, M.A. Relationship between admission serum C-reactive protein and short term outcome following acute ischemic stroke at a tertiary health institution in Nigeria. Niger. J. Clin. Pract. 2013, 16, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Yu, L.; Zhang, J.; Chen, N.; Zhou, M.; He, L. CRP gene polymorphism predicts post-stroke functional outcome in Han Chinese. Acta Neurol. Scand. 2014, 129, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Song, I.U.; Kim, J.S.; Kim, Y.I.; Lee, K.S.; Jeong, D.S.; Chung, S.W. Relationship between high-sensitivity C-reactive protein and clinical functional outcome after acute ischemic stroke in a Korean population. Cerebrovasc. Dis. 2009, 28, 545–550. [Google Scholar] [CrossRef] [PubMed]
- Wakugawa, Y.; Kiyohara, Y.; Tanizaki, Y.; Kubo, M.; Ninomiya, T.; Hata, J.; Doi, Y.; Okubo, K.; Oishi, Y.; Shikata, K.; et al. C-reactive protein and risk of first-ever ischemic and hemorrhagic stroke in a general Japanese population: The Hisayama Study. Stroke 2006, 37, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Montaner, J.; Fernandez-Cadenas, I.; Molina, C.A.; Ribó, M.; Huertas, R.; Rosell, A.; Penalba, A.; Ortega, L.; Chacón, P.; Alvarez-Sabín, J. Poststroke C-reactive protein is a powerful prognostic tool among candidates for thrombolysis. Stroke 2006, 37, 1205–1210. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Jing, J.; Zhao, X.Q.; Wang, C.X.; Wang, Y.L.; Liu, G.F.; Wang, C.J.; Liu, L.P.; Yang, X.M.; Jiao, Y.; et al. High-sensitivity C-reactive protein is a strong risk factor for death after acute ischemic stroke among Chinese. CNS Neurosci. Ther. 2012, 18, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Koçer, A.; Canbulat, C.; Gözke, E.; Ilhan, A. C-reactive protein is an indicator for fatal outcomes in first-time stroke patients. Med. Sci. Monit. 2005, 11, CR540–CR544. [Google Scholar] [PubMed]
- Dewan, K.R.; Rana, P.V.S. C-reactive protein and early mortality in acute ischemic stroke. Kathmandu Univ. Med. J. 2011, 36, 252–255. [Google Scholar] [CrossRef]
- Naess, H.; Nyland, H.; Idicula, T.; Waje-Andreassen, U. C-reactive protein and homocysteine predict long-term mortality in young ischemic stroke patients. J. Stroke Cerebrovasc. Dis. 2013, 22, e435–e440. [Google Scholar] [CrossRef] [PubMed]
- Everett, B.M.; Kurth, T.; Buring, J.E.; Ridker, P.M. The relative strength of C-reactive protein and lipid level as determinants of ischemic stroke as compared to coronary heart disease in women. J. Am. Coll. Cardiol. 2006, 48, 2235–2242. [Google Scholar] [CrossRef] [PubMed]
- VanGilder, R.L.; Davidov, D.M.; Stinehart, K.R.; Huber, J.D.; Turner, R.C.; Wilson, K.S.; Haney, E.; Davis, S.M.; Chantler, P.D.; Theeke, L.; et al. C-reactive protein and long-term ischemic stroke prognosis. J. Clin. Neurosci. 2014, 21, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Idicula, T.T.; Brogger, J.; Naess, H.; Waje-Andreassen, U.; Thomassen, L. Admission C-reactive protein after acute ischemic stroke is associated with stroke severity and mortality: The ‘Bergen stroke study’. BMC Neurol. 2009, 9. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Huang, W.J.; Yu, Z.G. Relationship between the hypersensitive C-reactive protein (hs-CRP) level and the prognosis of acute brainstem infarction. Cell Biochem. Biophys. 2015, 72, 107–110. [Google Scholar] [CrossRef] [PubMed]
- The neuroscience society. The nerve surgery to learn. All kinds of cerebrovascular disease diagnosis points. Chin. J. Neurol. 1996, 29, 379. [Google Scholar]
- Seo, W.K.; Seok, H.Y.; Kim, J.H.; Park, M.H.; Yu, S.W.; Oh, K.; Koh, S.B.; Park, K.W. C-reactive protein is a predictor of early neurologic deterioration in acute ischemic stroke. J. Stroke Cerebrovasc. Dis. 2012, 21, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Tanne, D.; Haim, M.; Goldbourt, U.; Boyko, V.; Doolman, R.; Adler, Y.; Brunner, D.; Behar, S.; Sela, B.A. Prospective study of serum homocysteine and risk of ischemic stroke among patients with preexisting coronary heart disease. Stroke 2003, 34, 632–636. [Google Scholar] [CrossRef] [PubMed]
- Brott, T.; Adams, H.P., Jr.; Olinger, C.P.; Marler, J.R.; Barsan, W.G.; Biller, J.; Spilker, J.; Holleran, R.; Eberle, R.; Hertzberg, V.; et al. Measurements of acute cerebral infarction: A clinical examination scale. Stroke 1989, 20, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Wityke, R.J.; Pessin, M.S.; Kaplan, R.F.; Caplan, L.R. Serial assessment of acute stroke using the NIH Stroke Scale. Stroke 1994, 25, 362–365. [Google Scholar]
- Youssef, M.Y.; Mojiminiyi, O.A.; Abdella, N.A. Plasma concentrations of C-reactive protein and total homocysteine in relation to the severity and risk factors for cerebrovascular disease. Transl. Res. 2007, 150, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Zhang, M. Correlation between C-reactive protein and serious level and prognosis in acute period in ischemic stroke patients. Chin. J. Pract. Nerv. Dis. 2006, 9, 18–20. [Google Scholar]
- Adams, H.P., Jr.; Bendixen, B.H.; Kappelle, L.J.; Biller, J.; Love, B.B.; Gordon, D.L.; Marsh, E.E. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993, 24, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Van Swieten, J.C.; Koudstaal, P.J.; Visser, M.C.; Schouten, H.J.; van Gijn, J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988, 19, 604–607. [Google Scholar] [CrossRef] [PubMed]
- Uyttenboogaart, M.; Stewart, R.E.; Vroomen, P.; De Keyser, J.; Luijckx, G.J. Optimizing cut off score for the Barthel index and Modified Rankin scale for defining outcome in stroke trials. Stroke 2005, 36, 1984–1987. [Google Scholar] [CrossRef] [PubMed]
- Sulter, G.; Steen, C.; De Keyser, J. Use of the Barthel index and modified Rankin scale in acute stroke trials. Stroke 1999, 30, 1538–1541. [Google Scholar] [CrossRef] [PubMed]
- Tsai, N.W.; Lee, L.H.; Huang, C.R.; Chang, W.N.; Chen, S.D.; Wang, H.C.; Lin, Y.J.; Lin, W.C.; Chiang, Y.F.; Lin, T.K.; et al. The association of statin therapy and high-sensitivity C-reactive protein level for predicting clinical outcome in acute non-cardioembolic ischemic stroke. Clin. Chim. Acta 2012, 413, 1861–1865. [Google Scholar] [CrossRef] [PubMed]
- Tu, W.J.; Zhao, S.J.; Liu, T.G.; Yang, D.G.; Chen, H. Combination of high-sensitivity C-reactive protein and homocysteine predicts the short-term outcomes of Chinese patients with acute ischemic stroke. Neurol. Res. 2013, 35, 912–921. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Wu, L.; Wang, X.; Zhao, X.; Wang, C.; Liu, L.; Zheng, H.; Cao, Y.; Wang, Y.; Wang, Y.; et al. Effect of recurrent stroke on poor functional outcome in transient ischemic attack or minor stroke. Int. J. Stroke 2016, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Erdur, H.; Scheitz, J.F.; Ebinger, M.; Rocco, A.; Grittner, U.; Meisel, A.; Rothwell, P.M.; Endres, M.; Nolte, C.H. In-hospital stroke recurrence and stroke after transient ischemic attack: Frequency and risk factors. Stroke 2015, 46, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, E.J.; Prins, N.D.; Vermeer, S.E.; Vrooman, H.A.; Hofman, A.; Koudstaal, P.J.; Breteler, M.M. C-reactive protein and cerebral small-vessel disease: The Rotterdam Scan Study. Circulation 2005, 112, 900–905. [Google Scholar] [CrossRef] [PubMed]
- Pineda, S.; Bang, O.Y.; Saver, J.L.; Starkman, S.; Yun, S.W.; Liebeskind, D.S.; Kim, D.; Ali, L.K.; Shah, S.H.; Ovbiagele, B. Association of serum bilirubin with ischemic stroke outcomes. J. Stroke Cerebrovasc. Dis. 2008, 17, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Song, G.; Jin, Y.; Liu, H.; Li, C.; Han, C.; Ren, S. Higher level of heme oxygenase-1 in patients with stroke than TIA. J. Thorac. Dis. 2014, 6, 772–777. [Google Scholar] [PubMed]
| Variable | Good Outcome (MRS ≤ 2) (n = 223) | Poor Outcome (MRS > 2) (n = 78) | Total | t/χ2 | p |
|---|---|---|---|---|---|
| Mean age ± SD, year | 63.08 ± 10.44 | 67.13 ± 10.27 | 64.13 ± 10.53 | −2.961 a | 0.003 |
| Gender | 0.901 b | 0.342 | |||
| Male | 131 (58.7%) | 41 (52.6%) | 172 (57.1%) | ||
| Female | 92 (41.3%) | 37 (47.4%) | 129 (42.9%) | ||
| Residence | 7.228 b | 0.007 | |||
| Rural | 95 (42.6%) | 47 (60.3%) | 142 (47.2%) | ||
| Urban | 128 (57.4%) | 31 (39.7%) | 159 (52.8%) | ||
| Working | 0.448 b | 0.503 | |||
| Yes | 72 (32.3%) | 22 (28.2%) | 94 (31.2%) | ||
| No | 151 (67.7%) | 56 (71.8%) | 207 (68.8%) | ||
| Marital status | 0.349 b | 0.554 | |||
| Single | 18 (8.1%) | 8 (10.3%) | 26 (8.6%) | ||
| Married | 205 (91.9%) | 70 (89.7%) | 275 (91.4%) | ||
| Smoking | 3.799 b | 0.051 | |||
| Yes | 78 (35.0%) | 37 (47.4%) | 115 (38.2%) | ||
| No | 145 (65.0%) | 41 (52.6%) | 186 (61.8%) | ||
| Alcohol drinking | 2.575 b | 0.109 | |||
| Yes | 41 (18.4%) | 21 (26.9%) | 62 (20.6%) | ||
| No | 182(81.6%) | 57 (73.1%) | 239 (79.4%) |
| Variable | Good Outcome (MRS ≤ 2) (n = 223) | Poor Outcome (MRS > 2) (n = 78) | Total | χ2/z | p |
|---|---|---|---|---|---|
| Mean HOD ± SD, day | 11.45 ± 3.25 | 12.08 ± 3.67 | 11.61 ± 3.37 | −1.436 a | 0.151 |
| Recurrent ischemic stroke | 12.854 b | <0.001 | |||
| Yes | 85 (38.1%) | 48 (61.5%) | 133 (44.2%) | ||
| No | 138 (61.9%) | 30 (38.5%) | 168 (55.8%) | ||
| Comorbid conditions | |||||
| Hypertension | 0.024 b | 0.876 | |||
| Yes | 135 (60.5%) | 48 (61.5%) | 183 (60.8%) | ||
| No | 88 (39.5%) | 30 (38.5%) | 118 (39.2%) | ||
| Diabetes mellitus (DM) | 0.432 b | 0.511 | |||
| Yes | 41 (18.4%) | 17 (21.8%) | 58 (19.3%) | ||
| No | 182 (81.6%) | 61 (78.2%) | 243 (80.7%) | ||
| Coronary heart disease | 4.042 b | 0.044 | |||
| Yes | 64 (28.7%) | 32 (41.0%) | 96 (31.9%) | ||
| No | 159 (71.3%) | 46 (59.0%) | 205 (68.1%) | ||
| NIHSS score at admission | 10.228 b | 0.001 | |||
| NIHSS ≤ 15 | 138 (61.9%) | 32 (41.0%) | 170 (56.5%) | ||
| NIHSS > 15 | 85 (38.1%) | 46 (59.0%) | 131 (43.5%) | ||
| Lacunar stroke | 7.685 b | 0.006 | |||
| Yes | 109 (48.9%) | 24 (30.8%) | 133 (44.2%) | ||
| No | 114 (51.1%) | 54 (69.2%) | 168 (55.8%) | ||
| Time from onset of stroke to admission (h) | 6.323 b | 0.042 | |||
| Time ≤ 12 | 89 (39.9%) | 32 (41.0%) | 121 (40.2%) | ||
| 12 < time ≤ 24 | 37 (16.6%) | 22 (28.2%) | 59 (19.6%) | ||
| Time > 24 | 97 (43.5%) | 24 (30.8%) | 121 (40.2%) |
| Variable Mean ± SD | Good Outcome (MRS ≤ 2) (n = 223) | Poor Outcome (MRS > 2) (n = 78) | Total | t/z | P |
|---|---|---|---|---|---|
| Routine blood | |||||
| CRP (mg/L) | 4.97 ± 6.35 | 18.86 ± 19.05 | 8.57 ± 12.65 | −8.892 a | <0.001 |
| WBC (109/L) | 7.42 ± 2.15 | 7.82 ± 2.64 | 7.52 ± 2.29 | −1.332 b | 0.184 |
| RBC (1012/L) | 4.45 ± 0.50 | 4.40 ± 0.60 | 4.44 ± 0.53 | 0.783 b | 0.434 |
| HGB (g/L) | 137.49 ± 18.86 | 137.60 ± 15.23 | 137.52 ± 17.96 | −0.046 b | 0.963 |
| Biochemical Items | |||||
| ESR (mm/h) | 19.99 ± 13.27 | 23.37 ± 16.51 | 20.87 ± 14.23 | −1.815 b | 0.071 |
| TBIL (umol/L) | 13.51 ± 5.22 | 15.41 ± 5.75 | 14.00 ± 5.42 | −2.701 b | 0.007 |
| DBIL (umol/L) | 4.25 ± 1.81 | 5.34 ± 1.78 | 4.53 ± 1.86 | −4.579 b | <0.001 |
| ALB (g/L) | 40.17 ± 2.91 | 38.45 ± 7.04 | 39.73 ± 4.42 | −5.738 a | <0.001 |
| CHOL (mmol/L) | 4.71 ± 1.03 | 4.63 ± 1.12 | 4.69 ± 1.05 | 0.510 b | 0.610 |
| TG (mmol/L) | 1.67 ± 1.28 | 1.31 ± 0.60 | 1.57 ± 1.15 | −1.893 a | 0.058 |
| HDL (mmol/L) | 1.12 ± 0.39 | 1.12 ± 0.25 | 1.12 ± 0.36 | 0.023 b | 0.982 |
| LDL (mmol/L) | 3.03 ± 0.91 | 2.91 ± 1.10 | 3.00 ± 0.96 | 0.954 b | 0.341 |
| GLU(mmol/L) | 6.48 ± 2.56 | 6.54 ± 1.96 | 6.50 ± 2.41 | −0.197 b | 0.844 |
| HCY (umol/L) | 20.20 ± 13.64 | 23.51 ± 12.82 | 21.06 ± 13.49 | −1.869 b | 0.063 |
| Blood Coagulation | |||||
| FIB (mg/dL) | 307.41 ± 81.53 | 346.60 ± 91.46 | 317.56 ± 85.80 | −3.538 b | <0.001 |
| D-dimer (ng/mL) | 442.40 ± 534.64 | 930.35 ± 954.95 | 568.85 ± 701.03 | −5.916 a | <0.001 |
| Variable | OR * | 95% CI | p |
|---|---|---|---|
| Recurrent ischemic stroke | |||
| Yes | 2.115 | 1.094–4.087 | 0.026 |
| No | reference | ||
| Lacunar stroke | |||
| Yes | reference | ||
| No | 2.943 | 1.436–6.032 | 0.003 |
| DBIL (per 1 SD increase) | 1.795 | 1.311–2.458 | <0.001 |
| CRP (per 1 SD increase) | 4.890 | 3.063–7.808 | <0.001 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Geng, H.-H.; Wang, X.-W.; Fu, R.-L.; Jing, M.-J.; Huang, L.-L.; Zhang, Q.; Wang, X.-X.; Wang, P.-X. The Relationship between C-Reactive Protein Level and Discharge Outcome in Patients with Acute Ischemic Stroke. Int. J. Environ. Res. Public Health 2016, 13, 636. https://doi.org/10.3390/ijerph13070636
Geng H-H, Wang X-W, Fu R-L, Jing M-J, Huang L-L, Zhang Q, Wang X-X, Wang P-X. The Relationship between C-Reactive Protein Level and Discharge Outcome in Patients with Acute Ischemic Stroke. International Journal of Environmental Research and Public Health. 2016; 13(7):636. https://doi.org/10.3390/ijerph13070636
Chicago/Turabian StyleGeng, He-Hong, Xin-Wang Wang, Rong-Li Fu, Meng-Juan Jing, Ling-Ling Huang, Qing Zhang, Xiao-Xiao Wang, and Pei-Xi Wang. 2016. "The Relationship between C-Reactive Protein Level and Discharge Outcome in Patients with Acute Ischemic Stroke" International Journal of Environmental Research and Public Health 13, no. 7: 636. https://doi.org/10.3390/ijerph13070636






