The Post-Amalgam Era: Norwegian Dentists’ Experiences with Composite Resins and Repair of Defective Amalgam Restorations
Abstract
:1. Introduction
2. Material and Methods
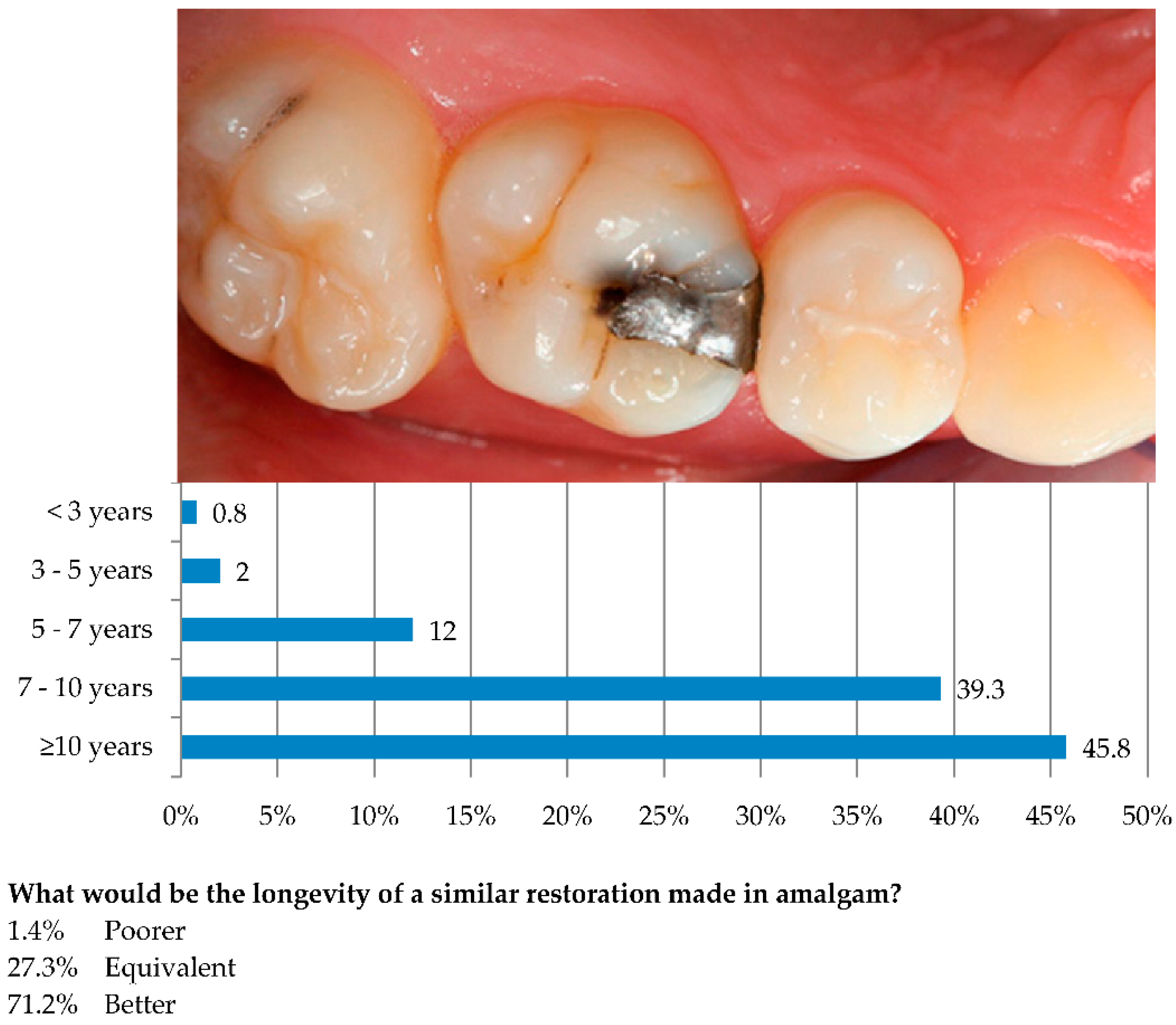
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| CAD/CAM | Computer-Aided Design/Computer-Aided Manufacturing |
| DMFT | Decayed, missing and filled teeth |
| GIC | Glass ionomer cement |
| MO | Mesial-occlusal |
| MOD | Mesial-occlusal-distal |
| NSD | The Norwegian Social Science Data Services |
| NTF | The Norwegian Dental Association |
| PDS | The Public Dental Service |
| SAFH | The Norwegian Registration Authority for Health Personnel |
References
- Norwegian Directorate of Health and Social Affairs. A National Clinical Guideline for the Use of Dental Filling Materials; Norwegian Directorate of Health and Social Affairs: Oslo, Norway, 2003. [Google Scholar]
- Norwegian Ministry of the Environment. Amendment of Regulations of 1 June 2004 no 922 Relating to Restrictions on the Use of Chemicals and Other Products Hazardous to Health and the Environment; Norwegian Ministry of the Environment: Oslo, Norway, 2008. [Google Scholar]
- Jones, D.W. Has dental amalgam been torpedoed and sunk? J. Dent. Res. 2008, 87, 101–102. [Google Scholar] [CrossRef] [PubMed]
- Larose, P.; Basciano, M. Dental mercury and Norway. J. Dent. Res. 2008, 87, 413. [Google Scholar] [CrossRef] [PubMed]
- Vidnes-Kopperud, S.; Tveit, A.B.; Gaarden, T.; Sandvik, L.; Espelid, I. Factors influencing dentists’ choice of amalgam and tooth-colored restorative materials for Class II preparations in younger patients. Acta Odontol. Scand. 2009, 67, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Vidnes-Kopperud, S.; Tveit, A.B.; Espelid, I. Changes in the treatment concept for approximal caries from 1983 to 2009 in Norway. Caries Res. 2011, 45, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Jokstad, A.; Mjör, I.A.; Qvist, V. The age of restorations in situ. Acta Odontol. Scand. 1994, 52, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Bogacki, R.E.; Hunt, R.J.; del Aguila, M.; Smith, W.R. Survival analysis of posterior restorations using an insurance claims database. Oper. Dent. 2002, 27, 488–492. [Google Scholar] [PubMed]
- Forss, H. Reasons for restorative therapy and the longevity of restorations in adults. Acta Odontol. Scand. 2004, 62, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Mjör, I.A.; Moorhead, J.E. Selection of restorative materials, reasons for replacement, and longevity of restorations in Florida. J. Am. Coll. Dent. 1998, 65, 27–33. [Google Scholar] [PubMed]
- Opdam, N.J.; Bronkhorst, E.M.; Cenci, M.S.; Huysmans, M.C.; Wilson, N.H. Age of failed restorations: A deceptive longevity parameter. J. Dent. 2011, 39, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; Bronkhorst, E.M.; Roeters, J.M.; Loomans, B.A. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent. Mater. 2007, 23, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Hickel, R.; Brushaver, K.; Ilie, N. Repair of restorations—Criteria for decision making and clinical recommendations. Dent. Mater. 2013, 29, 28–50. [Google Scholar] [CrossRef] [PubMed]
- Blum, I.R.; Lynch, C.D. Repair versus replacement of defective direct dental restorations in posterior teeth of adults. Prim. Dent. J. 2014, 3, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Brantley, C.F.; Bader, J.D.; Shugars, D.A.; Nesbit, S.P. Does the cycle of rerestoration lead to larger restorations? J. Am. Dent. Assoc. 1995, 126, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
- Tyas, M.J.; Anusavice, K.J.; Frencken, J.E.; Mount, G.J. Minimal intervention dentistry—A review. FDI Commission Project 1–97. Int. Dent. J. 2000, 50, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Demarco, F.F.; Correa, M.B.; Cenci, M.S.; Moraes, R.R.; Opdam, N.J. Longevity of posterior composite restorations: Not only a matter of materials. Dent. Mater. 2012, 28, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Staxrud, F.; Dahl, J.E. Role of bonding agents in the repair of composite resin restorations. Eur. J. Oral. Sci. 2011, 119, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Moncada, G.; Martin, J.; Fernandez, E.; Hempel, M.C.; Mjör, I.A.; Gordan, V.V. Sealing, refurbishment and repair of Class I and Class II defective restorations: A three-year clinical trial. J. Am. Dent. Assoc. 2009, 140, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Gordan, V.V.; Riley, J.L., 3rd; Blaser, P.K.; Mondragon, E.; Garvan, C.W.; Mjör, I.A. Alternative treatments to replacement of defective amalgam restorations: Results of a seven-year clinical study. J. Am. Dent. Assoc. 2011, 142, 842–849. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; Bronkhorst, E.M.; Loomans, B.A.; Huysmans, M.C. Longevity of repaired restorations: A practice based study. J. Dent. 2012, 40, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Norway, S. Dental Health. StatBank, Norway, 2009. Available online: https://statbank.ssb.no/en/statistikkbanken (accessed on 21 January 2010).
- American Association for Public Opinion Research. Standard Definitions. 2010. Available online: http://www.aapor.org/Standard_Definitions/2687.htm (accessed on 10 March 2016).
- Baraba, A.; Doméjean-Orliaguet, S.; Espelid, I.; Tveit, A.; Miletic, I. Survey of Croatian dentists’ restorative treatment decisions on approximal caries lesions. Croat. Med. J. 2010, 51, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Doméjean, S.; Leger, S.; Maltrait, M.; Espelid, I.; Tveit, A.B.; Tubert-Jeannin, S. Changes in Occlusal Caries Lesion Management in France from 2002 to 2012: A Persistent Gap between Evidence and Clinical Practice. Caries Res. 2015, 49, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Doméjean-Orliaguet, S.; Tubert-Jeannin, S.; Riordan, P.J.; Espelid, I.; Tveit, A.B. French dentists’ restorative treatment decisions. Oral. Health Prev. Dent. 2004, 2, 125–131. [Google Scholar] [PubMed]
- Heaven, T.J.; Gordan, V.V.; Litaker, M.S.; Fellows, J.L.; Brad Rindal, D.; Firestone, A.R.; Gilbert, G.H.; National Dental PBRN Collaborative Group. Agreement among dentists’ restorative treatment planning thresholds for primary occlusal caries, primary proximal caries, and existing restorations: Findings from The National Dental Practice-Based Research Network. J. Dent. 2013, 41, 718–725. [Google Scholar] [CrossRef] [PubMed]
- Kakudate, N.; Sumida, F.; Matsumoto, Y.; Manabe, K.; Yokoyama, Y.; Gilbert, G.H.; Gordan, V.V. Restorative treatment thresholds for proximal caries in dental PBRN. J. Dent. Res. 2012, 91, 1202–1208. [Google Scholar] [CrossRef] [PubMed]
- The Swedish Government Chemicals Policy. Available online: http://www.government.se/contentassets/12c4d85c2ca64d05827fc131f1a47ab9/sweden-will-ban-the-use-of-mercury (accessed on 10 March 2016).
- UNEP. Minimata Convention on Mercury. 2016. Available online: http://www.mercuryconvention.org/ (accessed on 10 March 2016).
- Kielbassa, A.M.; Lynch, C.D.; Wilson, N.H. Editorial: The Minamata convention: The beginning of the (amalgam-free) future? Quintessence Int. 2014, 45, 547–548. [Google Scholar] [PubMed]
- Lynch, C.D.; Wilson, N.H. Managing the phase-down of amalgam: Part II. Implications for practising arrangements and lessons from Norway. Br. Dent. J. 2013, 215, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Eklund, S.A. Trends in dental treatment, 1992 to 2007. J. Am. Dent. Assoc. 2010, 141, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Forss, H.; Widstrom, E. From amalgam to composite: Selection of restorative materials and restoration longevity in Finland. Acta Odontol. Scand. 2001, 59, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Friedl, K.H.; Hiller, K.A.; Schmalz, G. Placement and replacement of composite restorations in Germany. Oper. Dent. 1995, 20, 34–38. [Google Scholar] [PubMed]
- Sunnegårdh-Grönberg, K.; van Dijken, J.W.; Funegard, U.; Lindberg, A.; Nilsson, M. Selection of dental materials and longevity of replaced restorations in Public Dental Health clinics in northern Sweden. J. Dent. 2009, 37, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C.D.; McConnell, R.J.; Wilson, N.H. Trends in the placement of posterior composites in dental schools. J. Dent. Educ. 2007, 71, 430–434. [Google Scholar] [PubMed]
- Nascimento, M.M.; Gordan, V.V.; Qvist, V.; Litaker, M.S.; Rindal, D.B.; Williams, O.D.; Fellows, J.L.; Ritchie, L.K.; Mjör, I.A.; McClelland, J.; et al. Reasons for placement of restorations on previously unrestored tooth surfaces by dentists in The Dental Practice-Based Research Network. J. Am. Dent. Assoc. 2010, 141, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Hickel, R.; Manhart, J.; Garcia-Godoy, F. Clinical results and new developments of direct posterior restorations. Am. J. Dent. 2000, 13, 41D–54D. [Google Scholar] [PubMed]
- Da Rosa Rodolpho, P.A.; Donassollo, T.A.; Cenci, M.S.; Loguercio, A.D.; Moraes, R.R.; Bronkhorst, E.M.; Opdam, N.J.; Demarco, F.F. 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent. Mater. 2011, 27, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Soncini, J.A.; Maserejian, N.N.; Trachtenberg, F.; Tavares, M.; Hayes, C. The longevity of amalgam versus compomer/composite restorations in posterior primary and permanent teeth: Findings from the New England children’s amalgam trial. J. Am. Dent. Assoc. 2007, 138, 763–772. [Google Scholar] [CrossRef] [PubMed]
- Pallesen, U.; van Dijken, J.W.; Halken, J.; Hallonsten, A.L.; Hoigaard, R. A prospective 8-year follow-up of posterior resin composite restorations in permanent teeth of children and adolescents in Public Dental Health Service: Reasons for replacement. Clin. Oral. Investig. 2014, 18, 819–827. [Google Scholar] [CrossRef] [PubMed]
- Kuper, N.K.; Opdam, N.J.; Bronkhorst, E.M.; Huysmans, M.C. The influence of approximal restoration extension on the development of secondary caries. J. Dent. 2012, 40, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Bernardo, M.; Luis, H.; Martin, M.D.; Leroux, B.G.; Rue, T.; Leitao, J.; DeRouen, T.A. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J. Am. Dent. Assoc. 2007, 138, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Opdam, N.J.; van de Sande, F.H.; Bronkhorst, E.; Cenci, M.S.; Bottenberg, P.; Pallesen, U.; Gaengler, P.; Lindberg, A.; Huysmans, M.C.D.N.J.M.; Van Dijken, J.W. Longevity of posterior composite restorations: A systematic review and meta-analysis. J. Dent. Res. 2014, 93, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Kidd, E.A. Diagnosis of secondary caries. J. Dent. Educ. 2001, 65, 997–1000. [Google Scholar] [PubMed]
- Mjör, I.A. Clinical diagnosis of recurrent caries. J. Am. Dent. Assoc. 2005, 136, 1426–1433. [Google Scholar] [CrossRef] [PubMed]
- Kidd, E.A.; Beighton, D. Prediction of secondary caries around tooth-colored restorations: A clinical and microbiological study. J. Dent. Res. 1996, 75, 1942–1946. [Google Scholar] [CrossRef] [PubMed]
- Magalhaes, C.S.; Freitas, A.B.; Moreira, A.N.; Ferreira, E.F. Validity of staining and marginal ditching as criteria for diagnosis of secondary caries around occlusal amalgam restorations: An in vitro study. Braz. Dent. J. 2009, 20, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Palotie, U.; Vehkalahti, M.M. Reasons for replacement of restorations: Dentists’ perceptions. Acta Odontol. Scand. 2012, 70, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Haj-Ali, R.; Walker, M.P.; Williams, K. Survey of general dentists regarding posterior restorations, selection criteria, and associated clinical problems. Gen. Dent. 2005, 53, 369–375. [Google Scholar] [PubMed]
- Hickel, R.; Manhart, J. Longevity of restorations in posterior teeth and reasons for failure. J. Adhes. Dent. 2001, 3, 45–64. [Google Scholar] [PubMed]
- Björkman, L.; Gjerdet, N.R.; Lygre, G.B.; Berge, T.L.L.; Svahn, J.; Lundekvam, B.F. National Reporting of Adverse Reactions to Dental Biomaterials in Norway. Available online: https://www.researchgate.net/publication/266761514_National_Reporting_of_Adverse_Reactions_to_Dental_Biomaterials_in_Norway (accessed on 10 March 2016).
- The Norwegian Climate and Pollution Agency. Review of Norwegian Experiences with the Phase-Out of Dental Amalgam Use; The Norwegian Climate and Pollution Agency: Oslo, Norway, 2012. [Google Scholar]

| Restorative Material | Never | Seldom | Sometimes | Often | Always | n |
|---|---|---|---|---|---|---|
| Composite | 0.1 | 0.1 | 0.6 | 36.8 | 62.3 | 2019 |
| Compomer | 76.9 | 14.6 | 6.3 | 1.9 | 0.3 | 1560 |
| GIC conventional | 60.6 | 26.6 | 11.3 | 1.5 | - | 1607 |
| GIC resin-modified | 60.0 | 27.6 | 11.5 | 0.8 | 0.1 | 1602 |
| Composite inlay | 90.6 | 7.5 | 1.8 | 0.1 | - | 1591 |
| Ceramic inlay | 56.3 | 31.8 | 10.8 | 1.1 | 0.1 | 1617 |
| Ceramic inlay (CAD/CAM) | 85.6 | 9.2 | 4.0 | 1.2 | 0.1 | 1592 |
| Gold inlay | 52.5 | 36.7 | 10.3 | 0.4 | 0.1 | 1662 |
| Reasons for Replacement | Never | Seldom | Sometimes | Often | Always | n |
|---|---|---|---|---|---|---|
| Secondary caries | 0.1 | 1.8 | 25.4 | 70.6 | 2.1 | 2006 |
| Restoration fracture | 0.8 | 23.5 | 50.8 | 24.3 | 0.8 | 2001 |
| Poor approximal contact | 0.4 | 12.6 | 63.5 | 22.7 | 0.7 | 2006 |
| Marginal gaps | 1.1 | 29.7 | 53.3 | 15.4 | 0.5 | 2008 |
| Tooth fracture | 1.6 | 34.2 | 48.9 | 14.7 | 0.6 | 2009 |
| Marginal defects | 1.3 | 32.5 | 52.2 | 13.8 | 0.2 | 2008 |
| Lost restoration | 3.4 | 46.6 | 39.0 | 9.9 | 1.0 | 2010 |
| Restoration wear | 4.3 | 47.3 | 40.0 | 8.1 | 0.3 | 2008 |
| Marginal discoloration | 8.7 | 47.8 | 36.3 | 7.1 | 0.1 | 1992 |
| Pain/sensitivity | 2.2 | 48.3 | 43.8 | 5.4 | 0.3 | 2005 |
| Poor aesthetics | 7.4 | 55.6 | 33.6 | 3.4 | 0.0 | 2003 |
| Restoration deficiency | 5.0 | 58.4 | 33.7 | 2.5 | 0.4 | 2009 |
| Porosities | 8.8 | 62.2 | 27.0 | 1.8 | 0.2 | 2010 |
| Overhang | 9.7 | 63.8 | 24.8 | 1.6 | 0.2 | 2001 |
| Allergic reactions | 45.1 | 52.7 | 1.1 | 0.2 | 0.9 | 1999 |
| Factors Relevant for Longevity | Do Not Know | None | Minor | Medium | High | Very High | n |
|---|---|---|---|---|---|---|---|
| Moisture control | 0.1 | 0.1 | 0.7 | 4.8 | 35.4 | 58.9 | 2009 |
| High caries activity | - | - | 0.6 | 5.3 | 41.9 | 52.1 | 2005 |
| Poor oral hygiene | - | - | 1.1 | 11.5 | 46.2 | 41.0 | 2003 |
| Poor matrix technique | 0.3 | 0.1 | 1.0 | 11.6 | 50.4 | 36.4 | 2001 |
| Patient cooperation | 0.5 | 1.0 | 11.5 | 30 | 39.6 | 17.5 | 1999 |
| Cavity design | 0.1 | 0.3 | 11.1 | 37.6 | 40.8 | 10.1 | 2006 |
| Hard bite (patient) | 0.6 | 0.2 | 11.3 | 42.9 | 35.7 | 9.4 | 1992 |
| Following manufacturer’s instructions | 0.2 | 0.5 | 7.9 | 51.0 | 40.3 | 0.2 | 2008 |
| Dentist’ s experience | 0.6 | 1.5 | 11.0 | 54.4 | 32.4 | 0.6 | 2010 |
| Type of adhesive | 1.9 | 1.0 | 26.8 | 43.7 | 21.8 | 4.8 | 2008 |
| Type of composite | 1.8 | 2.2 | 37.4 | 44.3 | 12.0 | 2.3 | 2008 |
| Statements | Do Not Know | Totally Disagree | Disagree | Neutral | Agree | Totally Agree | n |
|---|---|---|---|---|---|---|---|
| Moisture control is the most important factor to achieve successful restorations | 0.1 | 0.5 | 2.9 | 13.6 | 47.7 | 35.3 | 2014 |
| Composite is a good alternative to amalgam | 0.3 | 0.5 | 6.2 | 18.9 | 44.4 | 29.6 | 2016 |
| Secondary caries is more commonly seen in composite restorations compared with amalgams | 1.9 | 2.4 | 13.8 | 23.4 | 40.1 | 18.4 | 2003 |
| Composite is not suitable in patients with high caries activity | 0.4 | 2.8 | 31.5 | 35.8 | 23.7 | 5.7 | 2009 |
| Lining is not necessary in deep composite restorations | 0.2 | 13.2 | 40.9 | 17.9 | 21.6 | 6.2 | 2002 |
| I often experience that my composite restorations need replacement | 0.4 | 6.0 | 43.4 | 30.3 | 17.8 | 2.1 | 2010 |
| Composite is not suitable in patients with poor oral hygiene | 0.3 | 7.3 | 39.2 | 35.2 | 15.7 | 2.2 | 2003 |
| Composite is not suitable in patients with a hard bite | 0.4 | 6.0 | 48.5 | 34.4 | 9.9 | 0.8 | 2002 |
| Composite is only suitable in small cavities | 0.2 | 24.0 | 57.6 | 12.8 | 3.8 | 1.7 | 2015 |
| Composite is not suitable in molars | - | 39.0 | 53.9 | 5.6 | 1.1 | 0.3 | 2001 |
| Independent Variables | % (n) | Minimal Invasive Treatment | Invasive Treatment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | ||||||||||
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||
| Dentist’s Age | |||||||||||||
| ≥35 years | 27.5 (557) | - | - | - | - | - | - | - | - | - | - | - | - |
| 36–47 years | 27.0 (548) | 0.73 | 0.56–0.95 | 0.02 | 0.80 | 0.61–1.05 | 0.10 | 0.76 | 0.42–0.95 | 1.41 | 0.71 | 0.39–1.32 | 0.28 |
| ≥48 years | 45.5 (921) | 0.51 | 0.40–0.65 | <0.01 | 0.54 | 0.42–0.69 | <0.01 | 0.87 | 0.51–0.65 | 1.46 | 0.74 | 0.43–1.27 | 0.28 |
| Dentist’s Gender | |||||||||||||
| Female | 48.1 (974) | - | - | - | - | - | - | - | - | - | - | - | - |
| Male | 51.9 (1052) | 0.62 | 0.51–0.76 | <0.01 | 0.82 | 0.65–1.02 | 0.07 | 1.97 | 1.23–3.18 | <0.01 | 2.06 | 1.24–3.42 | 2.06 |
| Practice Type | |||||||||||||
| Private Practice | 64.1 (1299) | - | - | - | - | - | - | - | - | - | - | - | - |
| Public Dental Service | 34.1 (690) | 2.36 | 1.92–2.91 | <0.01 | 2.19 | 1.76–2.72 | <0.01 | 0.62 | 0.37–1.03 | 0.07 | 0.79 | 0.46–1.35 | 0.38 |
| Other | 1.8 (37) | 1.37 | 0.64–2.94 | 0.42 | 1.52 | 0.70–3.30 | 0.29 | ||||||
| DMFT in County | |||||||||||||
| Continuous Variable | 100 (2026) | 1.03 | 0.88–1.19 | 0.73 | 0.89 | 0.63–1.24 | 0.49 | - | - | - | |||
| Number of Patients per Dentist in County | |||||||||||||
| Continuous Variable | 100 (2026) | 1.01 | 1.00–1.01 | 0.01 | 1.01 | 1.00–1.01 | 0.03 | 1.01 | 1.00–1.01 | 0.01 | 1.01 | 1.00–1.01 | 0.01 |
| Treatment decisions in Patient Case 2 |  |  |  |
|---|---|---|---|
| Enamel Caries | Caries in Outer Third of Dentin | Caries in Middle and Inner Third of Dentin | |
| Minimally invasive (repair) (n = 501) | 4.8% | 50.5% | 44.7% |
| Medium invasive (restoration/inlay) (n = 1428) | 7.1% | 58.8% | 34.1% |
| Invasive (crown) (n = 79) | 10.1% | 63.3% | 26.6% |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kopperud, S.E.; Staxrud, F.; Espelid, I.; Tveit, A.B. The Post-Amalgam Era: Norwegian Dentists’ Experiences with Composite Resins and Repair of Defective Amalgam Restorations. Int. J. Environ. Res. Public Health 2016, 13, 441. https://doi.org/10.3390/ijerph13040441
Kopperud SE, Staxrud F, Espelid I, Tveit AB. The Post-Amalgam Era: Norwegian Dentists’ Experiences with Composite Resins and Repair of Defective Amalgam Restorations. International Journal of Environmental Research and Public Health. 2016; 13(4):441. https://doi.org/10.3390/ijerph13040441
Chicago/Turabian StyleKopperud, Simen E., Frode Staxrud, Ivar Espelid, and Anne Bjørg Tveit. 2016. "The Post-Amalgam Era: Norwegian Dentists’ Experiences with Composite Resins and Repair of Defective Amalgam Restorations" International Journal of Environmental Research and Public Health 13, no. 4: 441. https://doi.org/10.3390/ijerph13040441
APA StyleKopperud, S. E., Staxrud, F., Espelid, I., & Tveit, A. B. (2016). The Post-Amalgam Era: Norwegian Dentists’ Experiences with Composite Resins and Repair of Defective Amalgam Restorations. International Journal of Environmental Research and Public Health, 13(4), 441. https://doi.org/10.3390/ijerph13040441






