Effects of Air Pollution on Hospital Emergency Room Visits for Respiratory Diseases: Urban-Suburban Differences in Eastern China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Data on Emergency Room Visits and Air Pollutants
2.3. Statistical Analysis
3. Results and Discussion
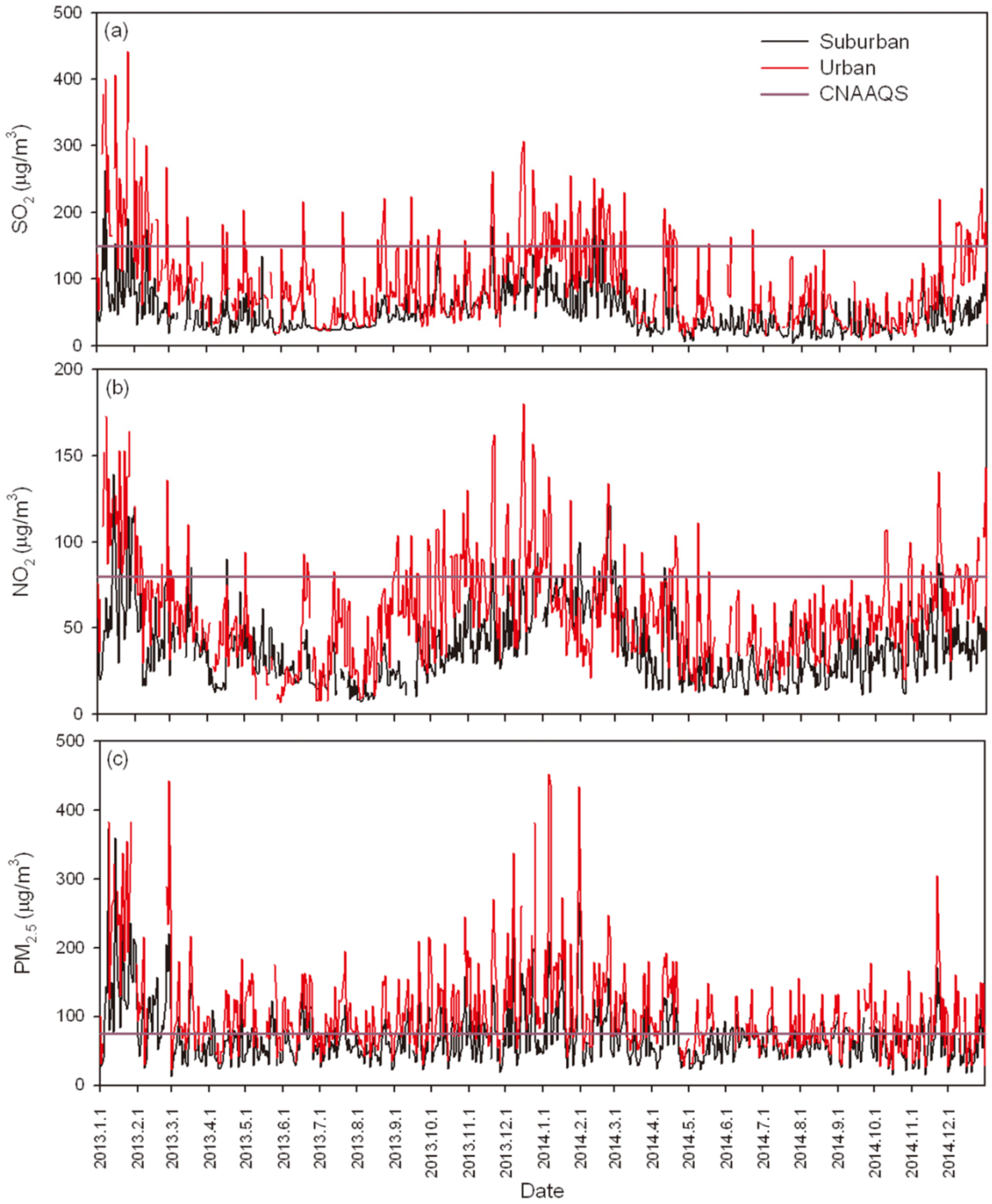
3.1. Descriptive Statistics
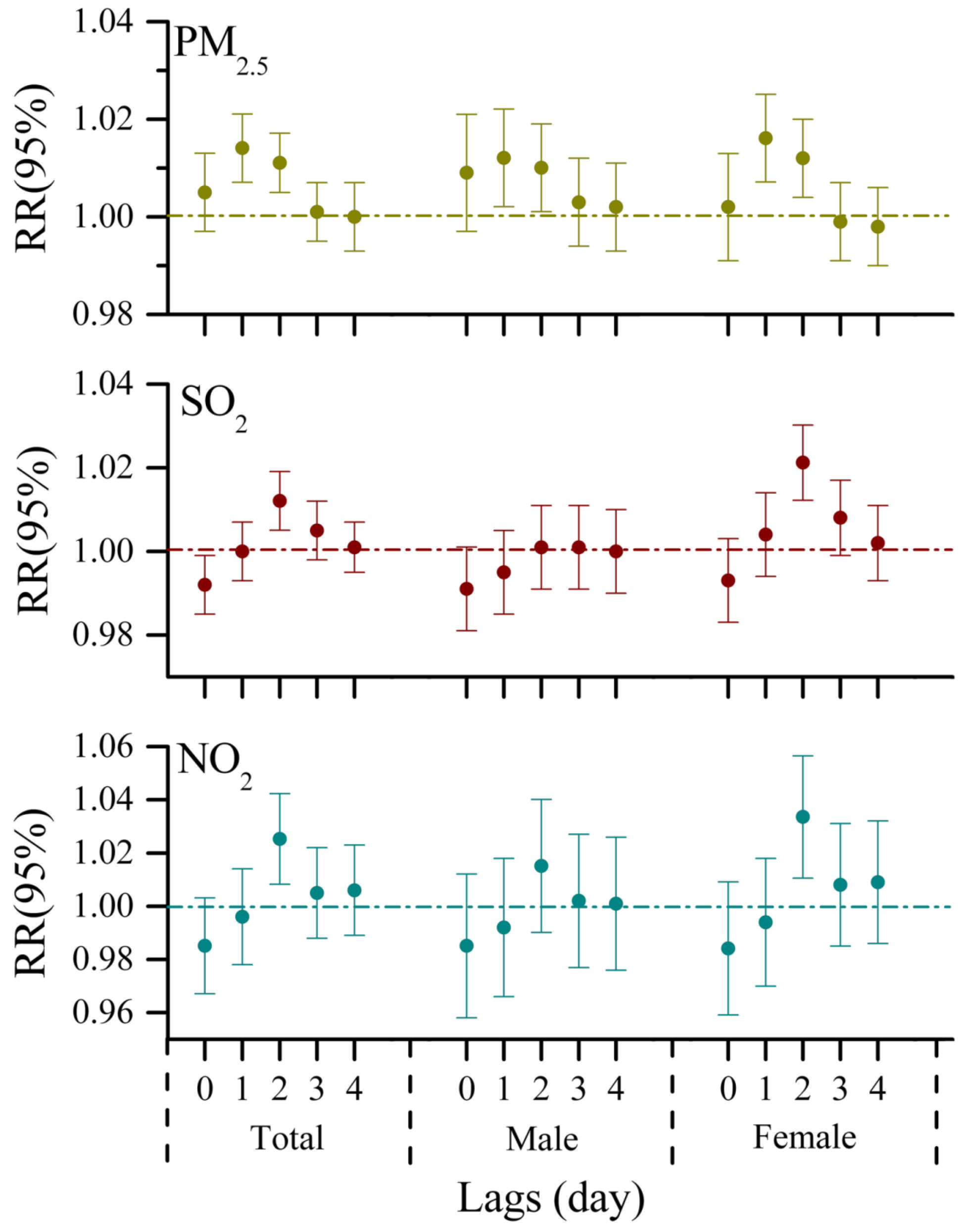
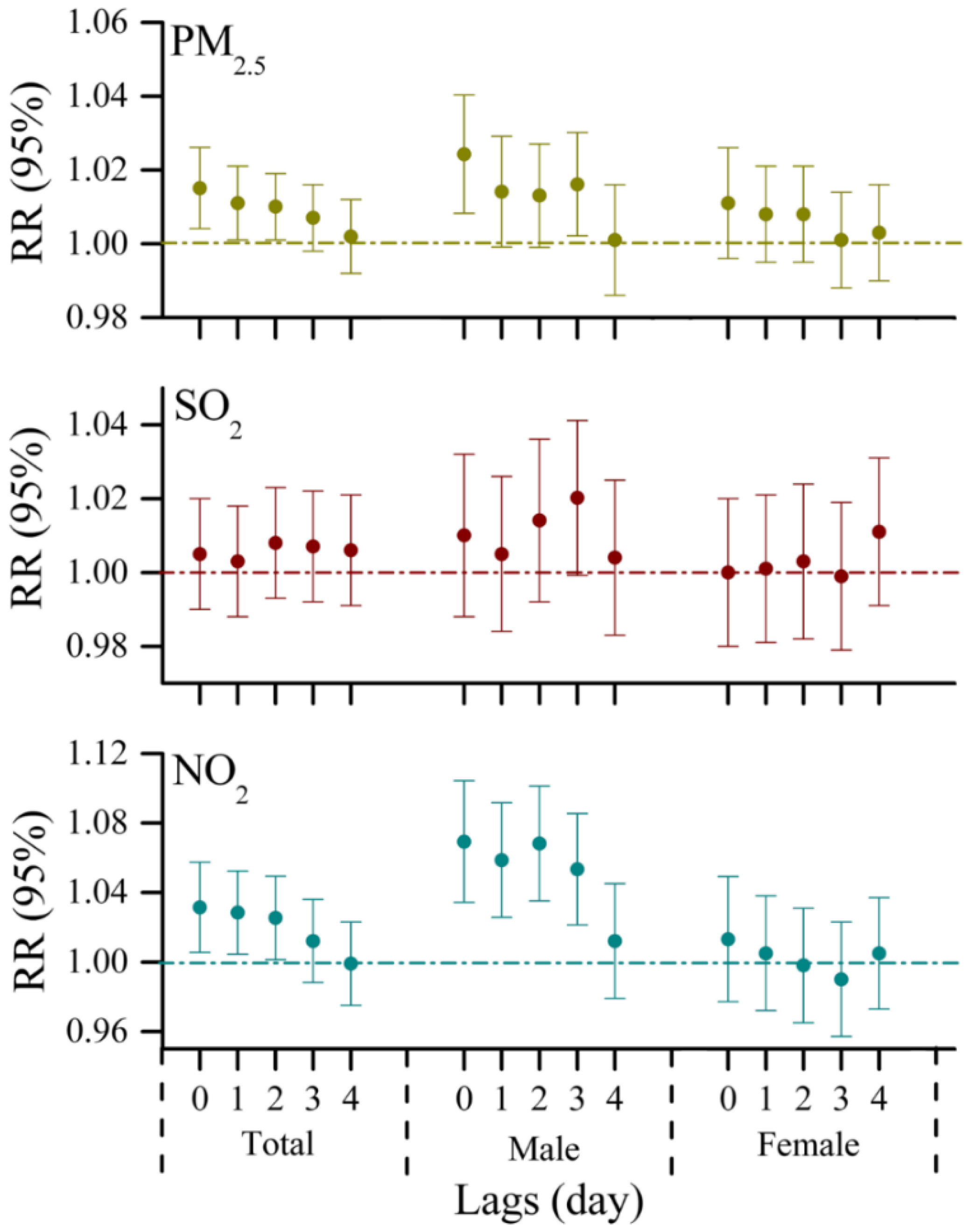
3.2. One-Pollutant Models
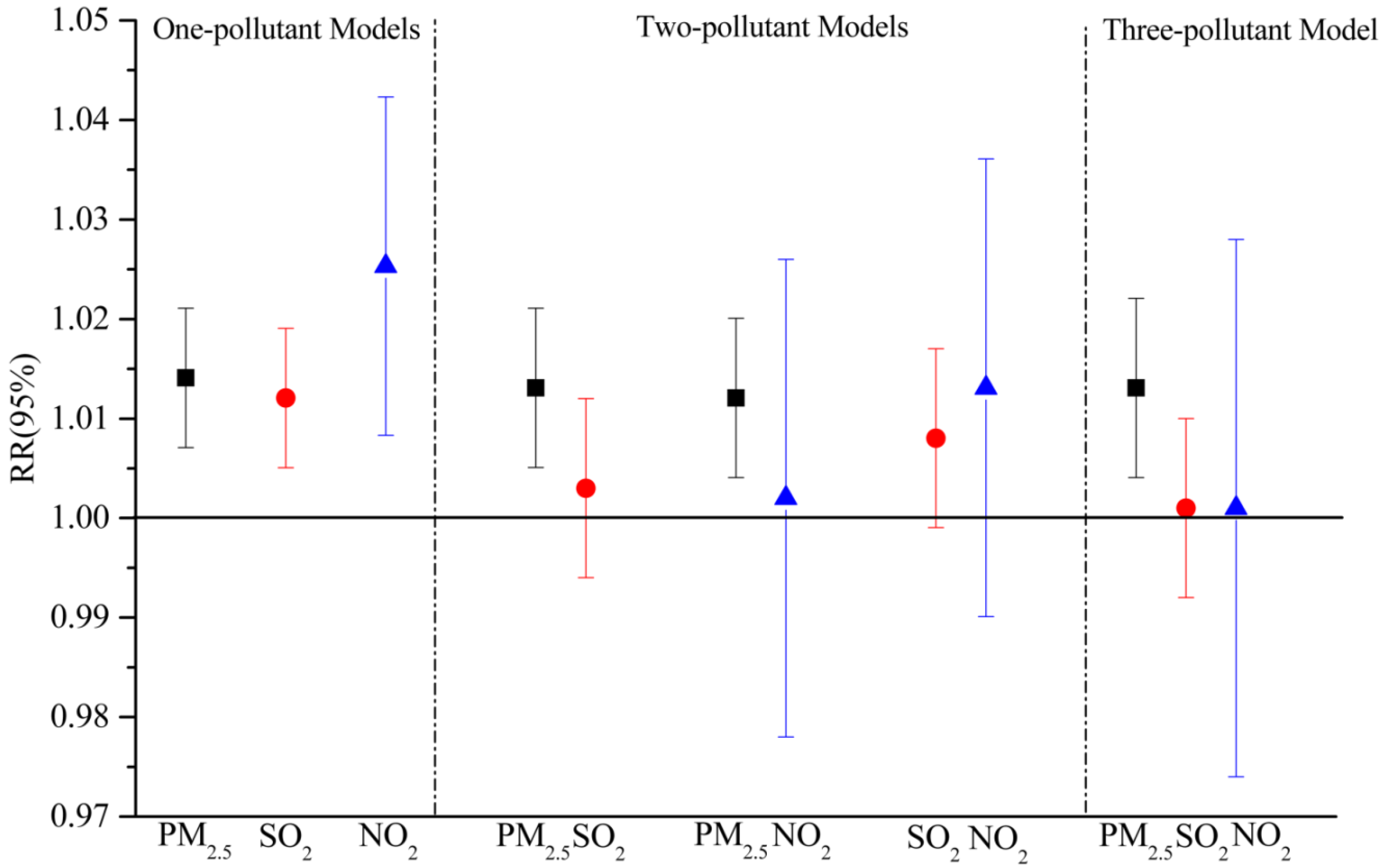
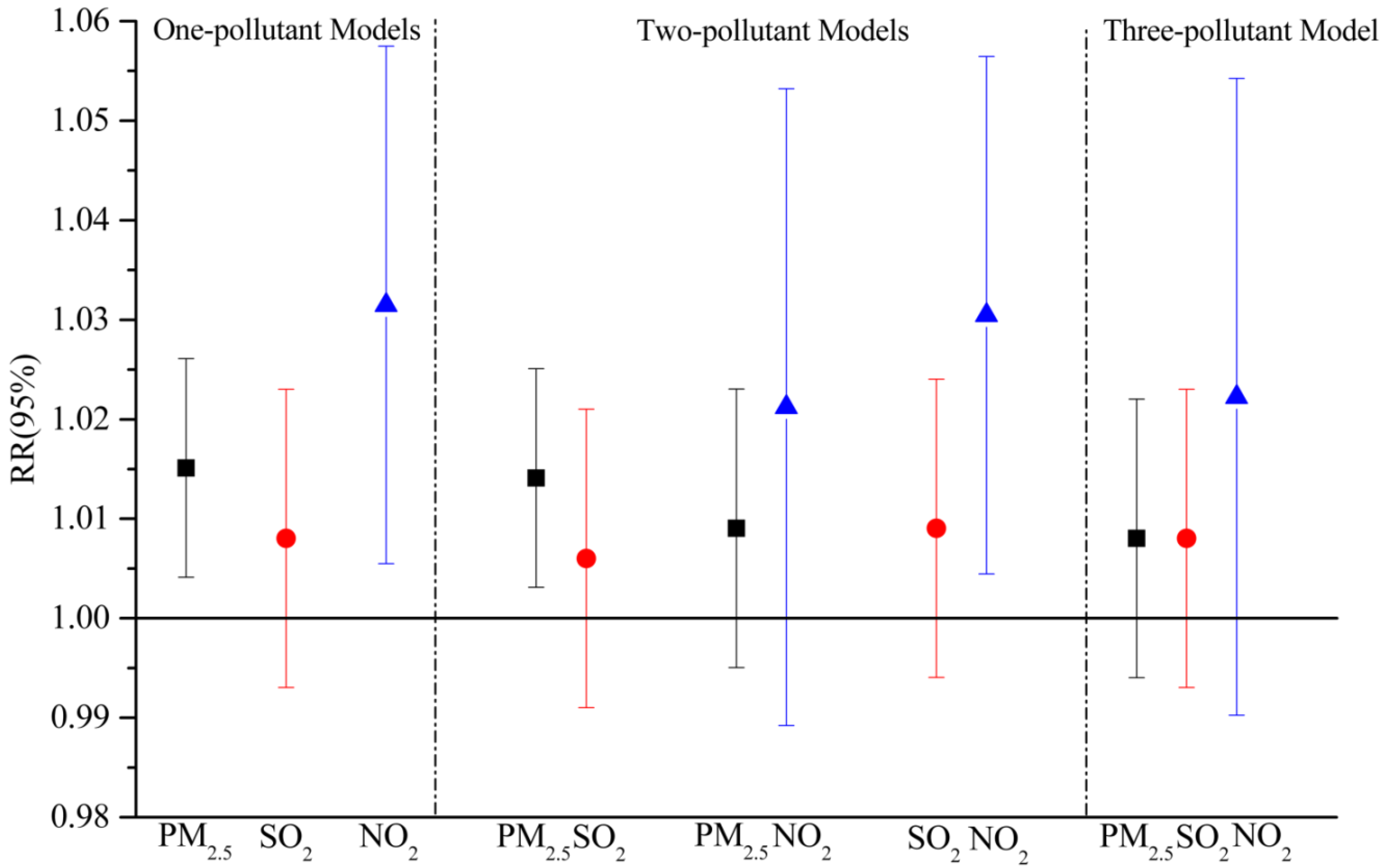
3.3. Muti-Pollutant Models
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| PM2.5 | Particulate matter less than 2.5 μm in diameter |
| ERVs | Emergency room visits |
| RR | Relative risk |
| HS | Hongjialou Subdistrict |
| ZT | Zhonggong Town |
Appendix

References
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010. Lancet 2013, 380, 2095–2128. [Google Scholar] [CrossRef]
- Maheswaran, R.; Haining, R.P.; Brindley, P.; Law, J.; Pearson, T.; Fryers, P.R.; Wise, S.; Campbell, M.J. Outdoor air pollution, mortality, and hospital admissions from coronary heart disease in Sheffield, UK: A small-area level ecological study. Eur. Hear. J. 2005, 26, 2543–2549. [Google Scholar] [CrossRef] [PubMed]
- Medina-Ramón, M.; Zanobetti, A.; Schwartz, J. The effect of ozone and PM10 on hospital admissions for pneumonia and chronic obstructive pulmonary disease: A national multicity study. Am. J. Epidemiol. 2006, 163, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; Davis, D.L. Reassessment of the lethal London fog of 1952: Novel indicators of acute and chronic consequences of acute exposure to air pollution. Environ. Health Perspect. 2001, 109, 389. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Dockery, D.W. Increased mortality in Philadelphia associated with daily air pollution concentrations. Am. Rev. Respir. Dis. 1992, 145, 600–604. [Google Scholar] [CrossRef] [PubMed]
- Pope, C., 3rd. Respiratory disease associated with community air pollution and a steel mill, Utah valley. Am. J. Public Health 1989, 79, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Wichmann, H.; Mueller, W.; Allhoff, P.; Beckmann, M.; Bocter, N.; Csicsaky, M.; Jung, M.; Molik, B.; Schoeneberg, G. Health effects during a smog episode in west Germany in 1985. Environ. Health Perspect. 1989, 79, 89. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.; Sizto, R. The Ontario air pollution study: Identification of the causative agent. Environ. Health Perspect. 1989, 79, 69. [Google Scholar] [CrossRef] [PubMed]
- Clancy, L.; Goodman, P.; Sinclair, H.; Dockery, D.W. Effect of air-pollution control on death rates in Dublin, Ireland: An intervention study. Lancet 2002, 360, 1210–1214. [Google Scholar] [CrossRef]
- Pönkä, A. Asthma and low level air pollution in Helsinki. Arch. Environ. Health 1991, 46, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, N.; Fletcher, T. Respiratory diseases in children and outdoor air pollution in São Paulo, Brazil: A time series analysis. Occup. Environ. Med. 2000, 57, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Alberini, A.; Cropper, M.; Simon, N.B.; Sharma, P.K. The Health Effects of Air Pollution in Delhi, India: Policy Research Working Paper; World Bank Group: Washington, DC, USA, 1997. [Google Scholar]
- Loomis, D.; Castillejos, M.; Gold, D.R.; McDonnell, W.; Borja-Aburto, V.H. Air pollution and infant mortality in Mexico City. Epidemiology 1999, 10, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Vichit-Vadakan, N.; Ostro, B.D.; Chestnut, L.G.; Mills, D.M.; Aekplakorn, W.; Wangwongwatana, S.; Panich, N. Air pollution and respiratory symptoms: Results from three panel studies in Bangkok, Thailand. Environ. Health Perspect. 2001, 109, 381. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.-M.; Vichit-Vadakan, N.; Kan, H.; Qian, Z. Public health and air pollution in Asia (PAPA): A multicity study of short-term effects of air pollution on mortality. Environ. Health Perspect. 2008, 116, 1195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, Q.; Chen, Y.; Krewski, D.; Burnett, R.T.; Shi, Y.; McGrail, K.M. Effect of short-term exposure to low levels of gaseous pollutants on chronic obstructive pulmonary disease hospitalizations. Environ. Res. 2005, 99, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, R.; Anderson, H.; Strachan, D.; Bland, J.; Bremmer, S.; Ponce de Leon, A. Short-term associations between outdoor air pollution and visits to accident and emergency departments in London for respiratory complaints. Eur. Respir. J. 1999, 13, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, Y.-S. Air quality assessment by contingent valuation in Jinan, China. J. Environ. Manag. 2009, 90, 1022–1029. [Google Scholar] [CrossRef] [PubMed]
- Tao, Y.; Mi, S.; Zhou, S.; Wang, S.; Xie, X. Air pollution and hospital admissions for respiratory diseases in Lanzhou, China. Environ. Pollut. 2014, 185, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; He, G.; Fan, M.; Wang, Z.; Liu, Y.; Ma, J.; Ma, Z.; Liu, J.; Liu, Y.; Wang, L. Smog episodes, fine particulate pollution and mortality in China. Environ. Res. 2015, 136, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Breitner, S.; Schneider, A.; Cyrys, J.; Brüske, I.; Franck, U.; Schlink, U.; Leitte, A.M.; Herbarth, O.; Wiedensohler, A. Size-fractioned particulate air pollution and cardiovascular emergency room visits in Beijing, China. Environ. Res. 2013, 121, 52–63. [Google Scholar] [CrossRef] [PubMed]
- Baldasano, J.; Valera, E.; Jimenez, P. Air quality data from large cities. Sci. Total. Environ. 2003, 307, 141–165. [Google Scholar] [CrossRef]
- Gao, X.; Yang, L.; Cheng, S.; Gao, R.; Zhou, Y.; Xue, L.; Shou, Y.; Wang, J.; Wang, X.; Nie, W. Semi-continuous measurement of water-soluble ions in PM2.5 in Jinan, China: Temporal variations and source apportionments. Atmos. Environ. 2011, 45, 6048–6056. [Google Scholar] [CrossRef]
- Zhu, Y.; Yang, L.; Meng, C.; Yuan, Q.; Yan, C.; Dong, C.; Sui, X.; Yao, L.; Yang, F.; Lu, Y.; et al. Indoor/outdoor relationships and diurnal/nocturnal variations in water-soluble ion and PAH concentrations in the atmospheric PM2.5 of a business office area in Jinan, a heavily polluted city in China. Atmos. Res. 2015, 153, 276–285. [Google Scholar] [CrossRef]
- Shi, L.; Zanobetti, A.; Kloog, I.; Coull, B.A.; Koutrakis, P.; Melly, S.J.; Schwartz, J.D. Low-concentration PM2.5 and mortality: Estimating acute and chronic effects in a population-based study. Environ. Health Perspect. 2015, 124, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Symons, J.; Wang, L.; Guallar, E.; Howell, E.; Dominici, F.; Schwab, M.; Ange, B.; Samet, J.; Ondov, J.; Harrison, D. A case-crossover study of fine particulate matter air pollution and onset of congestive heart failure symptom exacerbation leading to hospitalization. Am. J. Epidemiol. 2006, 164, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.-B.; Sun, X.-L.; Ming, L.; Yu, J.-M.; Yi, S.-Y.; Ji, Q.; Li, Z.-L.; Xu, L.; Xing, L.-H.; Qiao, S.; et al. Jinan Statistical Yearbook 2013; China Statistics Press: Beijing, China, 2013. [Google Scholar]
- Wang, L.; Wen, L.; Xu, C.; Chen, J.; Wang, X.; Yang, L.; Wang, W.; Yang, X.; Sui, X.; Yao, L. HONO and its potential source particulate nitrite at an urban site in north China during the cold season. Sci. Total. Environ. 2015, 538, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Cheng, S.; Wang, X.; Nie, W.; Xu, P.; Gao, X.; Yuan, C.; Wang, W. Source identification and health impact of PM2.5 in a heavily polluted urban atmosphere in China. Atmos. Environ. 2013, 75, 265–269. [Google Scholar] [CrossRef]
- Yang, L.; Zhou, X.; Wang, Z.; Zhou, Y.; Cheng, S.; Xu, P.; Gao, X.; Nie, W.; Wang, X.; Wang, W. Airborne fine particulate pollution in Jinan, China: Concentrations, chemical compositions and influence on visibility impairment. Atmos. Environ. 2012, 55, 506–514. [Google Scholar] [CrossRef]
- The Bureau of Land and Resources of Jinan. Available online: http://www.jndlr.gov.cn/tabid/62/InfoID/13159/frtid/123/Default.aspx (accessed on 12 October 2011).
- Kan, H.; London, S.J.; Chen, G.; Zhang, Y.; Song, G.; Zhao, N.; Jiang, L.; Chen, B. Season, sex, age, and education as modifiers of the effects of outdoor air pollution on daily mortality in Shanghai, China: The public health and air pollution in Asia (PAPA) study. Environ. Health Perspect. 2008, 116, 1183. [Google Scholar] [CrossRef] [PubMed]
- Akaike, H. Factor analysis and AIC. Psychometrika 1987, 52, 317–332. [Google Scholar] [CrossRef]
- Luginaah, I.N.; Fung, K.Y.; Gorey, K.M.; Webster, G.; Wills, C. Association of ambient air pollution with respiratory hospitalization in a government-designated “area of concern”: The case of Windsor, Ontario. Environ. Health. Perspect. 2005, 290–296. [Google Scholar] [CrossRef]
- Bakke, P.S.; Hanoa, R.; Gulsvik, A. Educational level and obstructive lung disease given smoking habits and occupational airborne exposure: A Norwegian community study. Am. J. Epidemiol. 1995, 141, 1080–1088. [Google Scholar] [PubMed]
- Prescott, E.; Vestbo, J. Socioeconomic status and chronic obstructive pulmonary disease. Thorax 1999, 54, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Zhong, N.; Wang, C.; Yao, W.; Chen, P.; Kang, J.; Huang, S.; Chen, B.; Wang, C.; Ni, D.; Zhou, Y. Prevalence of chronic obstructive pulmonary disease in China: A large, population-based survey. Am. J. Respir. Crit. Care Med. 2007, 176, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Schols, A.M.; Broekhuizen, R.; Weling-Scheepers, C.A.; Wouters, E.F. Body composition and mortality in chronic obstructive pulmonary disease. Am. J. Clin. Nutr. 2005, 82, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Yin, X.; Zhang, M.; Shen, H.; Lu, L.; Xu, Y. Prevalence of physician-diagnosed COPD and its association with smoking among urban and rural residents in regional mainland China. Chest 2005, 128, 2818–2823. [Google Scholar] [CrossRef] [PubMed]
- Peel, J.L.; Tolbert, P.E.; Klein, M.; Metzger, K.B.; Flanders, W.D.; Todd, K.; Mulholland, J.A.; Ryan, P.B.; Frumkin, H. Ambient air pollution and respiratory emergency department visits. Epidemiology 2005, 16, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Steenland, K.; Savitz, D.A. Topics in environmental epidemiology. Epidemiology 1998, 9, 213–214. [Google Scholar] [CrossRef]
- Horstman, D.H.; Folinsbee, L.J. Sulfur dioxide-induced bronchoconstriction in asthmatics exposed for short durations under controlled conditions: A selected review. In Susceptibility to Inhaled Pollutants; ASTM International: West Conshohocken, PA, USA, 1989. [Google Scholar]
- Winterton, D.L.; Kaufman, J.; Keener, C.V.; Quigley, S.; Farin, F.M.; Williams, P.V.; Koenig, J.Q. Genetic polymorphisms as biomarkers of sensitivity to inhaled sulfur dioxide in subjects with asthma. Ann. Allergy Asthma Immunol. 2001, 86, 232–238. [Google Scholar] [CrossRef]
- Chauhan, A.; Inskip, H.M.; Linaker, C.H.; Smith, S.; Schreiber, J.; Johnston, S.L.; Holgate, S.T. Personal exposure to nitrogen dioxide (NO2) and the severity of virus-induced asthma in children. Lancet 2003, 361, 1939–1944. [Google Scholar] [CrossRef]
- Sandstrom, T.; Stjernberg, N.; Eklund, A.; Ledin, M.; Bjermer, L.; Kolmodin-Hedman, B.; Lindstrom, K.; Rosenhall, L.; Angstrom, T. Inflammatory cell response in bronchoalveolar lavage fluid after nitrogen dioxide exposure of healthy subjects: A dose-response study. Eur. Respir. J. 1991, 4, 332–339. [Google Scholar] [PubMed]
- Tunnicliffe, W.; Burge, P.; Ayres, J. Effect of domestic concentrations of nitrogen dioxide on airway responses to inhaled allergen in asthmatic patients. Lancet 1994, 344, 1733–1736. [Google Scholar] [CrossRef]
- Tolbert, P.E.; Klein, M.; Peel, J.L.; Sarnat, S.E.; Sarnat, J.A. Multipollutant modeling issues in a study of ambient air quality and emergency department visits in Atlanta. J. Expo. Sci. Environ. Epidemiol. 2007, 17, S29–S35. [Google Scholar] [CrossRef] [PubMed]
- Halonen, J.I.; Lanki, T.; Yli-Tuomi, T.; Kulmala, M.; Tiittanen, P.; Pekkanen, J. Urban air pollution and asthma and COPD hospital emergency room visits. Thorax 2008, 63, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Slaughter, J.C.; Kim, E.; Sheppard, L.; Sullivan, J.H.; Larson, T.V.; Claiborn, C. Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. J. Expo. Sci. Environ. Epidemiol. 2005, 15, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Guo, Y.; Zhang, Y.; Westerdahl, D.; Mo, Y.; Liang, F.; Pan, X. Spatiotemporal analysis of particulate air pollution and ischemic heart disease mortality in Beijing, China. Environ. Health 2014, 13, 1–12. [Google Scholar] [CrossRef] [PubMed]
| Area | Pollutant | Mean ± SD | Min | 25%th | 50%th | 75%th | Max | ESR 1 (%) |
|---|---|---|---|---|---|---|---|---|
| Urban | SO2 | 95.4 ± 67.3 | 9.0 | 45.0 | 76.0 | 129.0 | 456.0 | 20.3 |
| NO2 | 60.0 ± 29.6 | 7.0 | 39.0 | 57.0 | 76.0 | 180.0 | 20.4 | |
| PM2.5 | 108.0 ± 64.6 | 21.0 | 67.0 | 91.0 | 132.0 | 452.0 | 67.2 | |
| Suburban | SO2 | 49.9 ± 32.4 | 4.0 | 26.0 | 41.0 | 66.0 | 263.0 | 1.6 |
| NO2 | 38.9 ± 21.5 | 8.0 | 22.0 | 34.0 | 49.0 | 140.0 | 5.7 | |
| PM2.5 | 70.7 ± 41.2 | 13.0 | 44.0 | 60.0 | 84.0 | 373.0 | 33.9 |
| Pollutant | SO2 | NO2 | PM2.5 | Temperature |
|---|---|---|---|---|
| NO2 | 0.677 * (0.706 *) 1 | |||
| PM2.5 | 0.563 * (0.656 *) | 0.628 * (0.659 *) | ||
| Temperature | −0.534 * (−0.534 *) | −0.626 * (−0.466 *) | −0.251 * (−0.289 *) | |
| Relative humidity | −0.059 (0.008) | 0.123 * (−0.001) | 0.354 * (0.259 *) | 0.129 * (0.129 *) |
| Area | Pollutant | Total (%) | Female (%) | Male (%) |
|---|---|---|---|---|
| Urban | PM2.5 | 1.4 (0.7, 2.1) | 1.6 (0.7, 2.5) | 1.2 (0.2, 2.2) |
| SO2 | 1.2 (0.5,1.9) | 2.1 (1.2, 3.0) | 0.1 (−0.9, 1.1) | |
| NO2 | 2.5 (0.8, 4.2) | 3.4 (1.1, 5.7) | 1.5 (−1.0, 4.0) | |
| Suburban | PM2.5 | 1.5 (0.4, 2.6) | 1.1 (−0.4, 2.6) | 2.4 (0.8, 4.0) |
| SO2 | 0.8 (−0.7, 2.3) | 1.1 (−0.9, 3.1) | 2.0 (−0.1, 4.1) | |
| NO2 | 3.1 (0.5, 5.7) | 1.3 (−2.3, 4.9) | 6.9 (3.4, 10.4) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, P.; Wang, X.; Fan, J.; Xiao, W.; Wang, Y. Effects of Air Pollution on Hospital Emergency Room Visits for Respiratory Diseases: Urban-Suburban Differences in Eastern China. Int. J. Environ. Res. Public Health 2016, 13, 341. https://doi.org/10.3390/ijerph13030341
Liu P, Wang X, Fan J, Xiao W, Wang Y. Effects of Air Pollution on Hospital Emergency Room Visits for Respiratory Diseases: Urban-Suburban Differences in Eastern China. International Journal of Environmental Research and Public Health. 2016; 13(3):341. https://doi.org/10.3390/ijerph13030341
Chicago/Turabian StyleLiu, Peng, Xining Wang, Jiayin Fan, Wenxin Xiao, and Yan Wang. 2016. "Effects of Air Pollution on Hospital Emergency Room Visits for Respiratory Diseases: Urban-Suburban Differences in Eastern China" International Journal of Environmental Research and Public Health 13, no. 3: 341. https://doi.org/10.3390/ijerph13030341





