Towards a European Framework to Monitor Infectious Diseases among Migrant Populations: Design and Applicability
Abstract
:1. Introduction
2. Methods
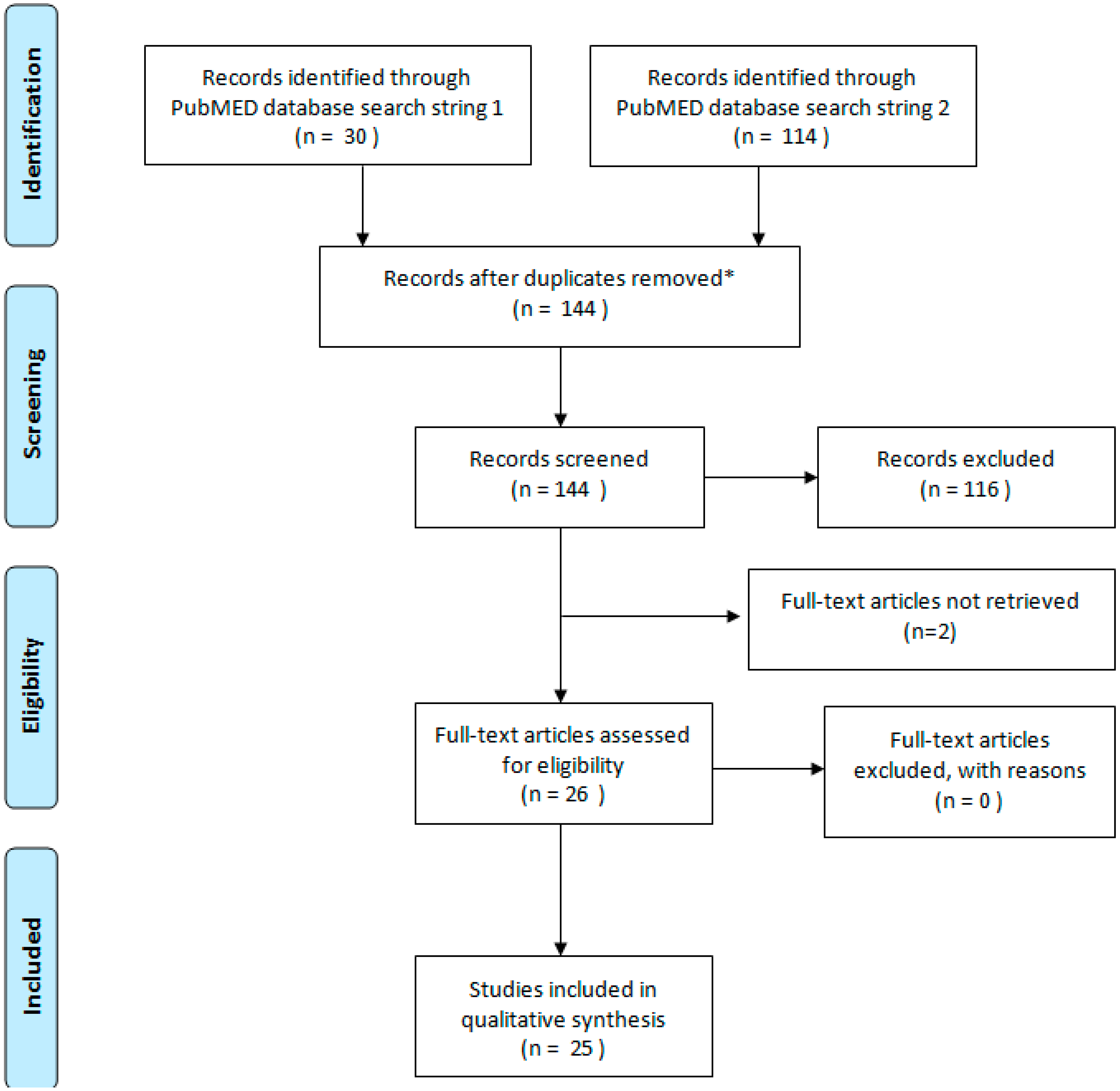
2.1. Systematic Literature Review
2.1.1. Inclusion Criteria
2.1.2. Search Strategy
| Key Words | Search String | Details | DB |
|---|---|---|---|
| Migrant + infectious | 1 | ((migrant[Title/Abstract]) AND infectious[Title/Abstract]) | Pubmed |
| Infectious diseases in newly arrived migrants or Asylum seekers or irregular migrants | 2 | ((((((((((((((((((((infection) OR infectious) OR outbreak) OR contagious) OR tuberculosis) OR TB) OR HIV) OR hepatitis) OR HBV) OR HCV) OR poliomyelitis) OR meningitis) OR gonorrhea) OR syphilis) OR malaria) OR chagas) OR measles) OR rubella) AND newly arrived migrants) OR asylum seekers) OR irregular migrants Filters: From 01/01/2010 to 31/12/2013, Humans | Pubmed |
2.1.3. Data Extraction and Analysis
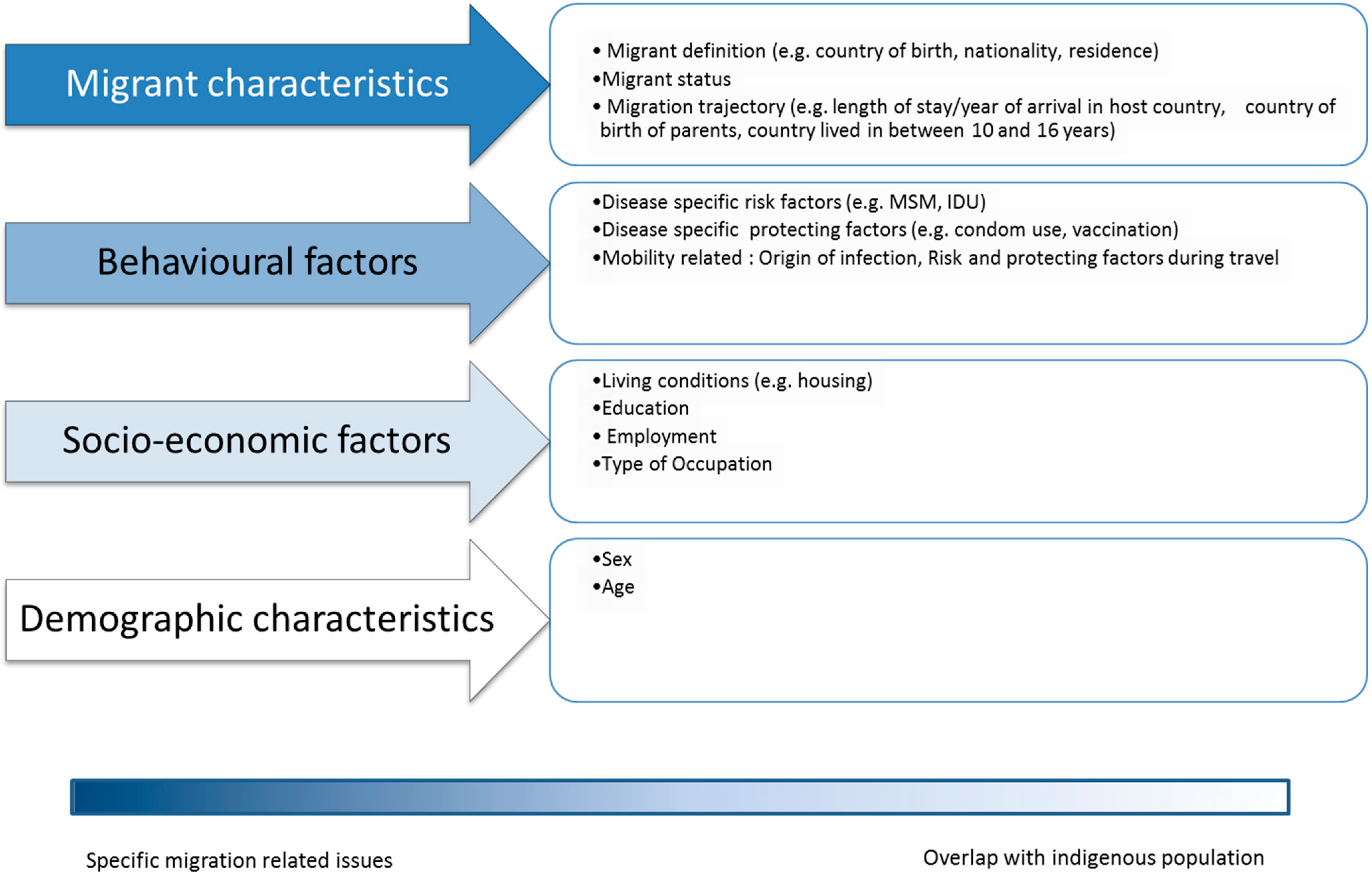
- “migration characteristics”, i.e., including variables/factors uniquely associated with being a migrant. These included: migrant legal status, migration trajectory (country of origin/travel route) and access to health care in the host country. For the purpose of this study the term “Variable” and “Factor” are used as synonyms. The first term is preferred to describe the type of information recorded in databases (either to be included in the hypothetical data collection framework or currently included in existing meta-datasets). The second is used when describing information presented in published studies (not datasets);
- “behavioral factors”, i.e., including variables/factors that could be more frequently associated with migrant communities but not exclusively. These included: disease specific risk factors and mobility (i.e., travel) related factors;
- “socioeconomic factors”, i.e., including variables/factors that could be more frequently associated with migrant communities but not exclusively. These included: poverty (living conditions/employment), education and (lack of) occupation;
- “demographic characteristics”, i.e., including variables/factors completely uninfluenced by being a migrant: such as age and/or sex when those were identified as a risk factor.
2.2. Feasibility of Applying the Identified Four Data Collection Domains
3. Results
3.1. Systematic Literature Review
| Authors | Language | Country | Focus | Type of Study | Geo-representativity | Study Size | |
|---|---|---|---|---|---|---|---|
| Search String 1 | Simon (2013) [31] | English | France | Severe cutaneous infections | Case series | Service based | 7 hospitalized patients |
| Wagner (2013) [32] | English | United Kingdom | Multiple conditions | Case series from surveillance data | National | TB > 6000 per year; HIV > 6000; Malaria between 1300 and 2000 per year; enteric fevers 400–500 per year | |
| Barnett (2013) [17] | English | United States | Multiple conditions | Case series from surveillance data | Service based | 7792 systematic migrant protocol screening records | |
| Zammarchi (2012) [33] | English | Italy | Syphilis | Case series | Service based | 187 records of pregnancy of which 143 followed to the end | |
| Rosales (2012) [34] | English | US And MEXICO | Seasonal farm workers | Cross sectional study | Subnational (intermediate level) | Survey on 233 jornaleros migrant workers | |
| Jaeger (2012) [35] | English | Switzerland | Children | Systematic literature review | National | Studies quoted included a study on TB on 234 children and HAV surveillance data. | |
| Kamper-Jørgensen (2012) [36] | English | Denmark | TB | Case series from surveillance data | National | 4631 genotyped TB cases | |
| Boulogne (2012) [28] | English | France | Mortality | Case series from mortality data | National | Complete mortality data Mainland France 2004–2007 (251, 665 foreign born) | |
| Kehr (2012) [27] | English | France and Germany | TB | Social/anthropologic qualitative study | International | NA | |
| Norredam (2012) [37] | English | Denmark | Mortality | Cohort study | National | 56,273 refugees and immigrants and 225,090 Danish controls | |
| Tafuri (2011) [38] | English | Italy | TB | Cross sectional study | Service based | 982 asylum seekers in a reception center (screening) | |
| Ott (2010) [39] | English | Germany, Israel | Mortality | Cohort study | International | Immigrants from former soviet union states: 34,393 randomly selected in North Rhine state Germany and 528,848 in Israel | |
| Search String 2 | Suurmond (2013) [40] | English | Netherlands | Multiple conditions | Social/anthropologic qualitative study | National | A purposive sample (non-probabilistic) of nurse practitioners and PH physicians in 50 asylum seeker centres (6 clusters) |
| Stoffels (2013) [41] | English | Belgium | TB | Cohort study | National | 174 MDR TB patients from National Tuberculosis register | |
| Kan (2013) [42] | English | Sweden | TB | Case series service based | Service based | 415 consecutive patients in a Swedish TB clinic | |
| Nyiri (2012) [43] | English | United Kingdom | Multiple conditions | Case series service based | Service based | First 112 patients who completed questionnaire seen at a refugee clinic London | |
| Sarivalasis (2012) [44] | English | Switzerland | TB | Cross sectional study | Subnational (intermediate level) | Interview and testing of 393 newly arrived asylum seekers in two Swiss hosting centers | |
| Chai (2013) [45] | English | United States | Chronic infectious diseases (ID) | Cohort study | Subnational (intermediate level) | 630 asylees and 151 refugees of the District of Columbia | |
| Fenner (2012) [46] | English | Switzerland | chronic ID | Cross sectional study | National | 381 TB patients (of whom 103 HIV co-infected) | |
| Takla (2012) [47] | English | Germany | Measles | Case series | Service based | Eight cases of measles in an asylum seekers’ shelter hosting 427 residents | |
| De Valliere (2011) [48] | English | Switzerland | Varicella | Case series | Service based | 16 cases of varicella in a housing facility for 125 asylum seekers | |
| Redman (2011) [49] | English | United Kingdom | Multiple conditions | Cross sectional study | Service based | Survey among 30 asylum seekers in an initial accommodation center in Wales | |
| Dudareva (2011) [50] | English | Germany | S. Aureus MRSA | Cross sectional study | Service based | Convenience sample of 232 of 427 residents in an asylum seekers center | |
| Wickramage (2013) [51,52] | English | Sri Lanka | Malaria | Cross sectional study | National | 287 screened returnees (first 6 months of following study); 534 irregular returnees screened for Malaria (32 positive P falciparum) | |
| Kaoutar (2012) [53] | French | France | Chronic ID | Cross sectional study | Service based | Survey among 536 immigrant patients in a facilitated access outpatient clinic |
| Infectious Disease Condition (IDC) Group | N. of Studies Addressing the IDC Group | Data Collection Domain 1 | Data Collection Domain 2 | Data Collection Domain 3 | Data Collection Domain 4 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| “Migration Characteristics” | “Behavioral Characteristics” | “Socioeconomic Factors” | “Demographic Characteristics” | |||||||
| Migrant Status | Migration Trajectory | Access to Health Care | Disease Specific Risk Factors | Mobility Related Factors | Poverty | Education | Occupation | Age/Sex | ||
| HAV | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| HBV | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| HIV | 4 | 3 | 2 | 3 | 1 | 0 | 2 | 1 | 0 | 1 |
| Infectious Hepatitis (not specified) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 |
| Intestinal Parasites | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Malaria | 2 | 1 | 2 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| Measles | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Multiple conditions | 6 | 6 | 4 | 6 | 0 | 0 | 3 | 2 | 1 | 2 |
| Skin infections | 2 | 2 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 |
| STD | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| TB | 11 | 9 | 6 | 3 | 4 | 1 | 5 | 1 | 0 | 3 |
| TB/HIV | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Typhoid | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Varicella | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Total | 35 | 28 | 17 | 15 | 10 | 4 | 11 | 5 | 1 | 6 |
| N. of studies per IDC reporting at least one factor in the domain | 33 | 14 | 11 | 6 | ||||||
3.2. Feasibility of Applying the Identified Four Data Collection Domains (DCD) to the Data Collected According to/EU Legislation
3.2.1. Data Collection Domain 1: Migration Characteristics
3.2.2. Data Collection Domain 2: Behavioral Factors
3.2.3. Data Collection Domain 3: Socio-economic Factors
3.2.4. Data Collection Domain 4: Demographic Characteristics
3.2.5. Denominators
4. Discussion
| Migrant Population Subgroups | Variable “Country of Birth” | Variable “Country of Nationality” |
|---|---|---|
| Intra EU mobile population * | EU/EEA country different from reporting country | EU/EEA country different from reporting country |
| EU/EEA first generation immigrants—non-nationals | Different from EU/EEA | Different from EU/EEA |
| Longer time EU/EEA resident first generation immigrants/immigrants born from EU/EEA citizens | Different from EU/EEA | EU/EEA country |
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- De la Rica, S.; Glitz, A.; Ortega, F. Immigration in Europe: Trends, Policies and Empirical Evidence. IZA Discussion Paper No. 7778. November 2013. Available online: http://www.econ.upf.edu/~glitz/ImmigrationEurope2013.pdf (accessed on 19 August 2015).
- Napoli, C.; Riccardo, F.; Declich, S.; Dente, M.G.; Pompa, M.G.; Rizzo, C.; Rota, M.C.; Bella, A.; The National Working Group. An early warning system based on syndromic surveillance to detect potential health emergencies among migrants: Results of a two-year experience in Italy. Int. J. Environ. Res. Public Health 2014, 11, 8529–8541. [Google Scholar] [PubMed]
- International Organization for Migration. Global Migration Trends: An Overview. 2014. Available online: http://missingmigrants.iom.int/sites/default/files/documents/Global_Migration_Trends_PDF_FinalVH_with%20References.pdf (accessed on 19 August 2015).
- UNHCR. Global Report 2012—Europe Regional Summary. Available online: http://www.unhcr.org/51b1d6260.html (accessed on 1 September 2015).
- UNHCR. Regional Operations Profile—Europe. Available online: http://www.unhcr.org/pages/4a02d9346.html (accessed on 19 August 2015).
- EUROSTAT. Migration and Citizenship Data. Available online: http://ec.europa.eu/eurostat/web/population-demography-migration-projections/migration-and-citizenship-data (accessed on 19 August 2015).
- EUROSTAT. Migration and Migrant Population Statistics. Available online: http://ec.europa.eu/eurostat/statistics-explained/index.php/Migration_and_migrant_population_statistics (accessed on 19 August 2015).
- Agreement on the European Economic Area OJ No L 1, 3.1.1994, p. 3; and EFTA States’ Official Gazettes. Available online: http://www.efta.int/sites/default/files/documents/legal-texts/eea/the-eea-agreement/Main%20Text%20of%20the%20Agreement/EEAagreement.pdf (accessed on 19 August 2015).
- Riccardo, F.; Napoli, C.; Bella, A.; Rizzo, C.; Rota, M.C.; Dente, M.G.; de Santis, S.; Declich, S. Syndromic surveillance of epidemic-prone diseases in response to an influx of migrants from North Africa to Italy. Euro Surveill. 2011, 16. Available online: http://www.eurosurveillance.org/images/dynamic/EE/V16N46/art20016.pdf (accessed on 31 July 2015). [Google Scholar]
- Norredam, M.; Agyemang, C.; Hoejbjerg Hansen, O.K.; Petersen, J.H.; Byberg, S.; Krasnik, A.; Kunst, A.E. Duration of residence and disease occurrence among refugees and family reunited immigrants: Test of the “healthy migrant effect” hypothesis. Trop. Med. Int. Health 2014, 19, 958–967. [Google Scholar] [CrossRef] [PubMed]
- Antiretroviral Therapy Cohort Collaboration (ART-CC). Influence of geographical origin and ethnicity on mortality in patients on antiretroviral therapy in Canada, Europe, and the United States. Clin. Infect. Dis. 2013, 56, 1800–1809. [Google Scholar]
- Solé-Auró, A.; Crimmins, E.M. Health of immigrants in European countries. Int. Migr. Rev. 2008, 42, 861–876. [Google Scholar] [CrossRef] [PubMed]
- HPA Presentation at the Workshop on Migrant Health and Infectious Diseases in the EU/EEA. Lisbon, Portugal, 8–9 October 2012; Available online: http://ecdc.europa.eu/en/press/events/Documents/ECDC-INSA-UK-country-presentation.pdf (accessed on 31 July 2015).
- Consumers, Health and Food Executive Agency. Action on Health Inequalities in the European Union. The EU Health Programme’s Contribution to Fostering Solidarity in Health and Reducing Health Inequalities in the European Union 2003–2013. European Union: Belgium, 2014. Available online: http://ec.europa.eu/chafea/documents/health/health-inequality-brochure_en.pdf (accessed on 31 July 2015).
- Rechel, B.; Mladovsky, P.; Ingleby, D.; Mackenbach, J.P.; McKee, M. Migration and health in an increasingly diverse Europe. Lancet 2013, 381, 1235–1245. [Google Scholar] [CrossRef]
- Marschall, T.; Kretzschmar, M.; Mangen, M.J.; Schalm, S. High impact of migration on the prevalence of chronic hepatitis B in the Netherlands. Eur. J. Gastroenterol. Hepatol. 2008, 20, 1214–1225. [Google Scholar] [CrossRef] [PubMed]
- Barnett, E.D.; Weld, L.H.; McCarthy, A.E.; So, H.; Walker, P.F.; Stauffer, W.; Cetron, M.; GeoSentinel Surveillance Network. Spectrum of illness in international migrants seen at GeoSentinel clinics in 1997–2009, part 1: US-bound migrants evaluated by comprehensive protocol-based health assessment. Clin. Infect. Dis. 2013, 56, 913–924. [Google Scholar] [CrossRef] [PubMed]
- Gushulak, B.D.; MacPherson, D.W. Globalization of infectious diseases: The impact of migration. Clin. Infect. Dis. 2004, 38, 1742–1748. [Google Scholar] [CrossRef] [PubMed]
- Regional Office for Europe of the World Health Organization. The Vector-borne Human Infections of Europe: Their Distribution and Burden on Public Health; WHO Regional Office for Europe: Copenhagen, Denmark, 2004. [Google Scholar]
- Vakali, A.; Patsoula, E.; Spanakos, G.; Danis, K.; Vassalou, E.; Tegos, N.; Economopoulou, A.; Baka, A.; Pavli, A.; Koutis, C.; et al. Malaria in Greece, 1975 to 2010. Euro Surveill. 2012, 17. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20322 (accessed on 31 July 2015). [Google Scholar]
- Odolini, S.; Parola, P.; Gkrania-Klotsas, E.; Caumes, E.; Schlagenhauf, P.; López-Vélez, R.; Burchard, G.D.; Santos-O’Connor, F.; Weld, L.; von Sonnenburg, F.; et al. Travel-related imported infections in Europe, EuroTravNet 2009. Clin. Microbiol. Infect. 2012, 18, 468–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Centre for Disease Prevention and Control. Mission report Dengue outbreak in Madeira, Portugal; ECDC: Stockholm, Sweden, 2013. [Google Scholar]
- EC Legal Framework for Communicable Disease Surveillance. Available online: http://ecdc.europa.eu/en/activities/surveillance/Pages/legal_framework.aspx (accessed on 31 July 2015).
- Decision No 2119/98/EC of the European Parliament and of the Council of 24 September 1998 Setting up a Network for the Epidemiological Surveillance and Control of Communicable Diseases in the Community Official Journal L 268, 03/10/1998 P. 0001–0007. Available online: http://eur-lex.europa.eu/legal-content/EN/ALL/?uri=CELEX:31998D2119 (accessed on 31 July 2015).
- Decision No 1082/2013/EU of the European Parliament and of the council of 22 October 2013 on Serious Cross-Border Threats to Health Official Journal of the European Union L.293. Available online: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2013:293:0001:0015:EN:PDF (accessed on 31 July 2015).
- European Centre for Disease Prevention and Control. Assessing the Burden of Key Infectious Diseases Affecting Migrant Populations in the EU/EEA; ECDC: Stockholm, Sweden, 2014. [Google Scholar]
- Kehr, J. Blind spots and adverse conditions of care: Screening migrants for tuberculosis in France and Germany. Sociol Health Illn. 2012, 34, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Boulogne, R.; Jougla, E.; Breem, Y.; Kunst, A.E.; Rey, G. Mortality differences between foreign born and locally born population in France (2004–2007). Soc. Sci. Med. 2012, 74, 1213–1223. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.; Pereira Miguel, J. Health and Migration in European Union: Better Health for all in an Inclusive Society; ISBN 978-972-8643-41-6. Instituto Nacional de Saúde Doutor Ricardo Jorge: Lisboa, Portugal, 2009. [Google Scholar]
- Transparent Reporting of Systematic Reviews and Meta-Analyses (PRISMA) Statement. Available online: http://www.prisma-statement.org/statement.htm (accessed on 31 July 2015).
- Simon, F.; Gautret, P.; Nicolas, X.; Ausset, P.; de Pina, J.J.; Demortiere, E. Crossing the Gulf of Aden: Cutaneous infections in African migrant shipwreck survivors. Travel Med. Infect. Dis. 2013, 11, 431–434. [Google Scholar] [CrossRef] [PubMed]
- Wagner, K.S.; Lawrence, J.; Anderson, L.; Yin, Z.; Delpech, V.; Chiodini, P.L.; Redman, C.; Jones, J. Migrant health and infectious diseases in the UK: Findings from the last 10 years of surveillance. J. Public Health 2014, 36, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Zammarchi, L.; Borchi, B.; Chiappini, E.; Galli, L.; Brogi, M.; Sterrantino, G.; Trotta, M. Syphilis in pregnancy in Tuscany, description of a case series from a global health perspective. J. Matern. Fetal Neonatal Med. 2012, 25, 2601–2605. [Google Scholar] [CrossRef] [PubMed]
- Rosales, C.; Ortega, M.I.; de Zapien, J.G.; Contreras Paniagua, A.D.; Zapien, A.; Ingram, M.; Aranda, P. The US/Mexico Border: A binational approach to framing challenges and constructing solutions for improving farmworkers’ lives. Int. J. Environ. Res. Public Health 2012, 9, 2159–2174. [Google Scholar] [CrossRef] [PubMed]
- Jaeger, F.N.; Hossain, M.; Kiss, L.; Zimmerman, C. The health of migrant children in Switzerland. Int. J. Public Health 2012, 57, 659–671. [Google Scholar] [CrossRef] [PubMed]
- Kamper-Jørgensen, Z.; Andersen, A.B.; Kok-Jensen, A.; Kamper-Jorgensen, M.; Bygbjerg, I.C.; Andersen, P.H.; Thomsen, V.O.; Lillebaek, T. Migrant tuberculosis: The extent of transmission in a low burden country. BMC Infect. Dis. 2012, 12, 60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Norredam, M.; Olsbjerg, M.; Petersen, J.H.; Bygbjerg, I.; Krasnik, A. Mortality from infectious diseases among refugees and immigrants compared to native Danes: A historical prospective cohort study. Trop. Med. Int. Health 2012, 17, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Tafuri, S.; Martinelli, D.; Melpignano, L.; de Palma, M.; Quarto, M.; Prato, R.; Germinario, C. Tuberculosis screening in migrant reception centers: Results of a 2009 Italian survey. Am. J. Infect. Control 2011, 39, 495–499. [Google Scholar] [CrossRef] [PubMed]
- Ott, J.J.; Paltiel, A.M.; Winkler, V.; Becher, H. The impact of duration of residence on cause-specific mortality: A cohort study of migrants from the Former Soviet Union residing in Israel and Germany. Health Place 2010, 16, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Suurmond, J.; Rupp, I.; Seeleman, C.; Goosen, S.; Stronks, K. The first contacts between healthcare providers and newly-arrived asylum seekers: A qualitative study about which issues need to be addressed. Public Health 2013, 127, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Stoffels, K.; Allix-Beguec, C.; Groenen, G.; Wanlin, M.; Berkvens, D.; Mathys, V.; Supply, P.; Fauville-Dufaux, M. From multidrug- to extensively drug-resistant tuberculosis: Upward trends as seen from a 15-year nationwide study. PLoS ONE 2013, 8. [Google Scholar] [CrossRef]
- Kan, B.; Kalin, M.; Bruchfeld, J. Completing treatment for latent tuberculosis: Patient background matters. Int. J. Tuberc. Lung Dis. 2013, 17, 597–602. [Google Scholar] [CrossRef] [PubMed]
- Nyiri, P.; Eling, J. A specialist clinic for destitute asylum seekers and refugees in London. Br. J. Gen. Pract. 2012, 62, 599–600. [Google Scholar] [CrossRef] [PubMed]
- Sarivalasis, A.; Zellweger, J.P.; Faouzi, M.; Daher, O.; Deslarzes, C.; Bodenmann, P. Factors associated with latent tuberculosis among asylum seekers in Switzerland: A cross-sectional study in Vaud County. BMC Infect. Dis. 2012, 12, 285. [Google Scholar] [CrossRef] [PubMed]
- Chai, S.J.; Davies-Cole, J.; Cookson, S.T. Infectious disease burden and vaccination needs among asylees versus refugees, district of Columbia. Clin. Infect. Dis. 2013, 56, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Fenner, L.; Gagneux, S.; Janssens, J.P.; Fehr, J.; Cavassini, M.; Hoffmann, M.; Bernasconi, E.; Schrenzel, J.; Bodmer, T.; Böttger, E.C.; et al. Tuberculosis in HIV-negative and HIV-infected patients in a low-incidence country: Clinical characteristics and treatment outcomes. PLoS ONE 2012, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takla, A.; Barth, A.; Siedler, A.; Stocker, P.; Wichmann, O.; Delere, Y. Measles outbreak in an asylum-seekers’ shelter in Germany: Comparison of the implemented with a hypothetical containment strategy. Epidemiol. Infect. 2012, 140, 1589–1598. [Google Scholar] [CrossRef] [PubMed]
- De Valliere, S.; Cani, N.; Grossenbacher, M.; Puig, F.; Masserey, E.; Bodenmann, P. Comparison of two strategies to prevent varicella outbreaks in housing facilities for asylum seekers. Int. J. Infect. Dis. 2011, 15, e716–e721. [Google Scholar] [CrossRef] [PubMed]
- Redman, E.A.; Reay, H.J.; Jones, L.; Roberts, R.J. Self-reported health problems of asylum seekers and their understanding of the national health service: A pilot study. Public Health 2011, 125, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Dudareva, S.; Barth, A.; Paeth, K.; Krenz-Weinreich, A.; Layer, F.; Delere, Y.; Eckmanns, T. Cases of community-acquired meticillin-resistant Staphylococcus aureus in an asylum seekers centre in Germany, November 2010. Euro Surveill. 2011, 16. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19777 (accessed on 31 July 2015). [Google Scholar]
- Wickramage, K.; Galappaththy, G.N. Malaria burden in irregular migrants returning to Sri Lanka from human smuggling operations in West Africa and implications for a country reaching malaria elimination. Trans. R. Soc. Trop. Med. Hyg. 2013, 107, 337–340. [Google Scholar] [CrossRef] [PubMed]
- Wickramage, K.; Premaratne, R.G.; Peiris, S.L.; Mosca, D. High attack rate for malaria through irregular migration routes to a country on verge of elimination. Malar. J. 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Kaoutar, B.; Mathieu-Zahzam, L.; Lebas, J.; Chauvin, P. La santé des migrants consultant la policlinique Baudelaire de l’hôpital Saint-Antoine à Paris, France. Bull. Soc. Pathol. Exot. 2012, 105, 86–94. [Google Scholar] [CrossRef] [PubMed]
- EUROSTAT. Migration and Migrant Population Statistics. Available online: http://epp.eurostat.ec.europa.eu/statistics_explained/index.php/Migration_and_migrant_population_statistics#Methodology_.2F_Metadata (accessed on 31 July 2015).
- United Nations Population Division Department of Economic and Social Affairs (UNDESA) Population Division. International Migration. Available online: http://www.un.org/en/development/desa/population/migration/data/estimates2/estimatesage.shtml (accessed on 31 July 2015).
- United Nations High Commissioner for Refugees (UNHCR). Statistics and Operational Data. Available online: http://www.unhcr.org/pages/4a013eb06.html (accessed on 15 September 2015).
- European University Institute EUDO Observatory on Citizenship Comparing Citizenship Laws: Mode A02a: Birth in Country (2nd Generation). Available online: http://eudo-citizenship.eu/databases/modes-of-acquisition?p=dataEUCIT&application=modesAcquisition&search=1&modeby=idmode&idmode=A02a (accessed on 31 July 2015).
- World Health Organization. Health of Migrants—The Way Forward; Report of a Global Consultation; WHO: Madrid, Spain, 2010. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riccardo, F.; Dente, M.G.; Kärki, T.; Fabiani, M.; Napoli, C.; Chiarenza, A.; Rossi, P.G.; Munoz, C.V.; Noori, T.; Declich, S. Towards a European Framework to Monitor Infectious Diseases among Migrant Populations: Design and Applicability. Int. J. Environ. Res. Public Health 2015, 12, 11640-11661. https://doi.org/10.3390/ijerph120911640
Riccardo F, Dente MG, Kärki T, Fabiani M, Napoli C, Chiarenza A, Rossi PG, Munoz CV, Noori T, Declich S. Towards a European Framework to Monitor Infectious Diseases among Migrant Populations: Design and Applicability. International Journal of Environmental Research and Public Health. 2015; 12(9):11640-11661. https://doi.org/10.3390/ijerph120911640
Chicago/Turabian StyleRiccardo, Flavia, Maria Grazia Dente, Tommi Kärki, Massimo Fabiani, Christian Napoli, Antonio Chiarenza, Paolo Giorgi Rossi, Cesar Velasco Munoz, Teymur Noori, and Silvia Declich. 2015. "Towards a European Framework to Monitor Infectious Diseases among Migrant Populations: Design and Applicability" International Journal of Environmental Research and Public Health 12, no. 9: 11640-11661. https://doi.org/10.3390/ijerph120911640







