An Evaluation on the Effect of Health Education and of Low-Dose Statin in Dyslipidemia among Low-Income Rural Uyghur Adults in Far Western China: A Comprehensive Intervention Study
Abstract
:1. Introduction
2. Methods
2.1. Ethics Statement
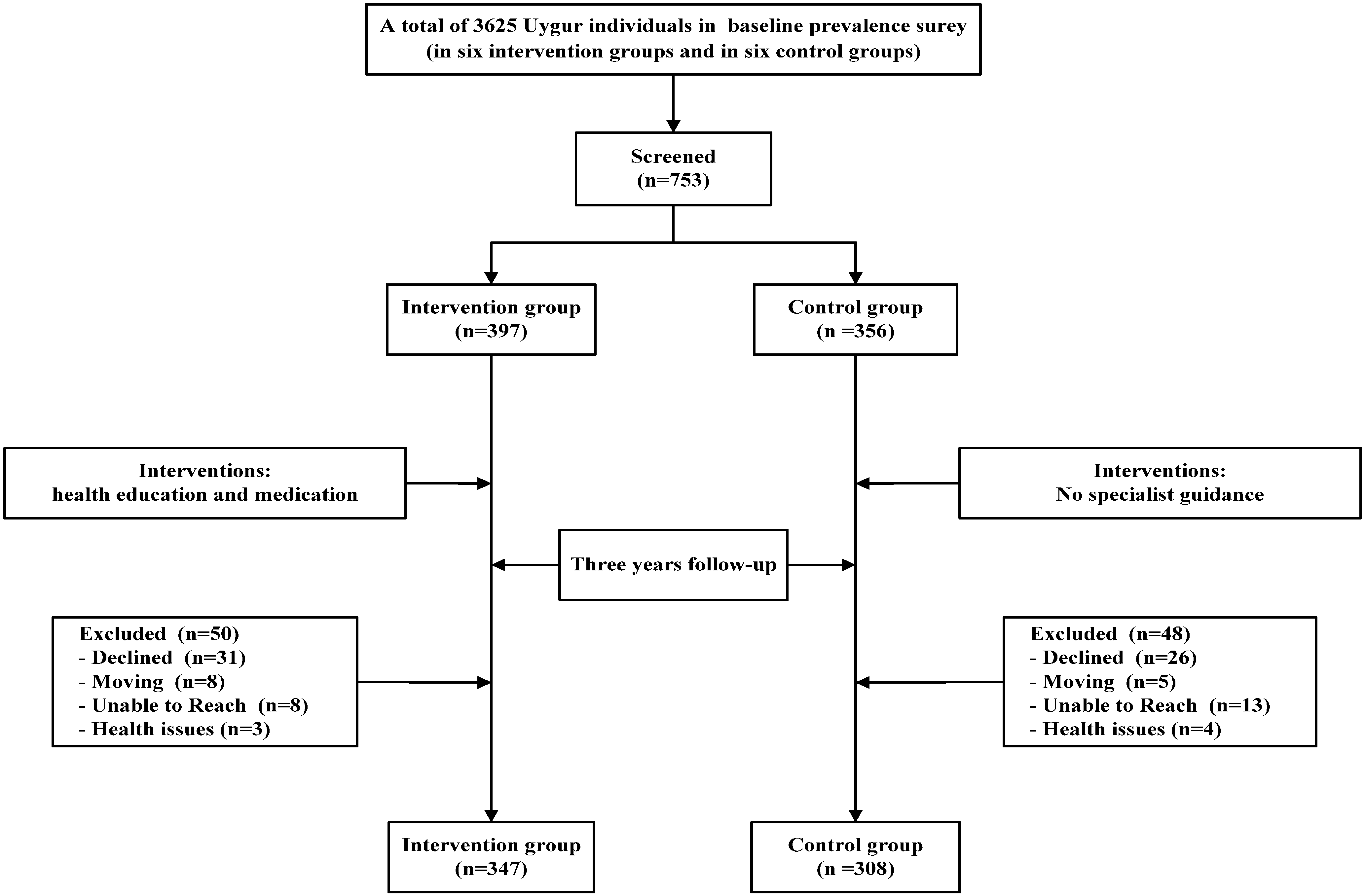
2.2. Study Design and Patients
2.3. Interventions
2.4. Data Collection
2.4.1. Questionnaire Survey
2.4.2. Physical Examination and Blood Lipid Examination
2.4.3. Definitions
2.4.4. Statistical Analysis
3. Result
3.1. Basic Characteristics of the Study Population
| Variables | Intervention Group (n = 347) | Control Group (n = 308) | t/χ2 | p |
|---|---|---|---|---|
| Sex (n,%) | 2.118 | 0.146 | ||
| male | 182(52.4%) | 144(46.8%) | ||
| female | 165(47.6%) | 164(53.2%) | ||
| Age (years) | 45.86 ± 15.32 | 45.37 ± 17.55 | 0.346 | 0.729 |
| Height (cm) | 163.44 ± 6.99 | 162.80 ± 10.34 | 0.187 | 0.853 |
| Weight (kg) | 65.46 ± 10.78 | 66.28 ± 11.91 | 1.803 | 0.093 |
| WHR | 0.85 ± 0.06 | 0.86 ± 0.07 | 1.841 | 0.066 |
| BMI (kg/m2) | 21.51 ± 2.61 | 21.54 ± 2.83 | 0.132 | 0.895 |
| TG (mmol/L) | 1.43 ± 0.78 | 1.29 ± 0.73 | 1.933 | 0.054 |
| TC ( mmol/L) | 4.39 ± 1.05 | 4.15 ± 1.20 | 2.891 | 0.089 |
| HDL-C ( mmol/L) | 0.96 ± 0.23 | 1.02 ± 0.22 | 1.796 | 0.073 |
| LDL-C (mmol/L) | 2.44 ± 0.69 | 2.39 ± 0.86 | 0.634 | 0.526 |
| SBP (mmHg) | 129.28 ± 22.73 | 130.76 ± 21.16 | 0.752 | 0.457 |
| DBP (mmHg) | 80.94 ± 13.79 | 81.00 ± 14.19 | 0.043 | 0.966 |
| FBG (mmol/L) | 4.23 ± 0.73 | 4.09 ± 0.78 | 1.695 | 0.091 |
| Current smoking state (%) | 1.345 | 0.510 | ||
| no | 323(93.1%) | 295(95.8%) | ||
| yes | 24(6.9%) | 13(4.2%) | ||
| Current drinking state (%) | 1.052 | 0.591 | ||
| no | 342(98.6%) | 304(98.7%) | ||
| yes | 5(1.4%) | 4(1.3%) |
3.2. Comparison of Lipid Levels
| Variable | Baseline | Post-1 Year | Post-2 Year | Outcome | F | p | |
|---|---|---|---|---|---|---|---|
| Intervention group | TG | 1.43 ± 0.78 | 1.42 ± 1.03 | 1.40 ± 1.11 * | 1.39 ± 0.81 *,## | 25.611 | 0.000 |
| TC | 4.39 ± 1.05 | 4.22 ± 0.94 ## | 4.10 ± 0.83 ## | 4.15 ± 0.92 ## | 0.603 | 0.547 | |
| HDL-C | 0.96 ± 0.23 | 1.01 ± 0.37 ** | 1.09 ± 0.25 * | 1.22 ± 0.41 *,## | 76.877 | 0.000 | |
| LDL-C | 2.44 ± 0.69 | 2.37 ± 0.59 **,## | 2.10 ± 0.50 *,# | 2.12 ± 0.62 *,# | 98.453 | 0.000 | |
| Control group | TG | 1.29 ± 0.73 | 1.37 ± 0.85 ** | 1.41 ± 0.72 ** | 1.50 ± 0.91 * | 22.493 | 0.000 |
| TC | 4.15 ± 0.72 | 4.01 ± 0.92 | 3.80 ± 0.86 | 3.95 ± 0.84 | 0.412 | 0.703 | |
| HDL-C | 1.02 ± 0.22 | 0.93 ± 0.32 ** | 1.06 ± 0.29 ** | 1.10 ± 0.36 ** | 2.385 | 0.032 | |
| LDL-C | 2.39 ± 0.86 | 2.43 ± 0.81 ** | 2.32 ± 0.70 ** | 2.24 ± 0.77 ** | 1.754 | 0.041 | |
3.3. Comparison of the Control Rate of Dyslipidemia
| Groups | n | Control | % | χ2 | p |
|---|---|---|---|---|---|
| Intervention Group | 347 | 134 | 38.61 | 116.263 | 0.000 |
| Control Group | 308 | 11 | 3.57 |
3.4. Lipid Changes in the Amplitude of the Survey Population
| Variable | Intervention Group (n = 347) | Mean Percent Change, % ± SE (Median) | Control Group (n = 308) | Mean Percent Change, % ± SE (Median) | |
|---|---|---|---|---|---|
| TG, mmol/L | Baseline | 1.43 ± 0.78 | −2.80 ± 0.08 (0.55) | 1.29 ± 0.73 | 16.28 ± 0.52 (10.99) |
| Outcome | 1.39 ± 0.81 | 1.50 ± 0.91 ** | |||
| TC, mmol/L | Baseline | 4.39 ± 1.05 | −5.47 ± 0.09 (−3.81) | 4.40 ± 0.12 | −4.55 ± 0.19 (−2.16) |
| Outcome | 4.15 ± 0.92 | 4.20 ± 0.84 ** | |||
| HDL-C, mmol/L | Baseline | 0.96 ± 0.23 | 27.08 ± 0.07 (17.40) | 1.02 ± 0.22 | 7.84 ± 0.02 (6.32) |
| Outcome | 1.22 ± 0.41 | 1.10 ± 0.36 ** | |||
| LDL-C, mmol/L | Baseline | 2.44 ± 0.69 | −13.11 ± 0.20 (−9.26) | 2.43 ± 0.86 | −6.17 ± 0.06 (−6.57) |
| Outcome | 2.12 ± 0.62 | 2.28 ± 0.77 * |
3.5. Comparison of Body Mass Index
3.6. Comparison of Knowledge, Attitude, Behavior Score
| Scores | Intervention Group | Control Group | ||
|---|---|---|---|---|
| Baseline | Outcome | Baseline | Outcome | |
| Knowledge scores | 1.00 ± 1.19 * | 3.32 ± 1.29 # | 1.05 ± 1.15 | 1.39 ± 1.18 |
| Attitude scores | 0.60 ± 0.73 * | 2.07 ± 0.87 # | 0.66 ± 0.80 | 0.82 ± 0.92 |
| Behavior scores | 0.45 ± 0.71 * | 1.11 ± 0.83 # | 0.50 ± 0.81 | 0.70 ± 0.96 |
| Total average scores | 2.05 ± 1.82 * | 6.50 ± 3.30 # | 2.20 ± 1.92 | 2.91 ± 2.31 * |
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Murray, C.J.; Lopez, A.D. Mortality by cause for eight regions of the world: Global burden of disease study. Lancet 1997, 349, 1269–1276. [Google Scholar] [CrossRef]
- Strong, K.; Mathers, C.; Leeder, S.; Beaglehole, R. Preventing chronic diseases: How many lives can we save? Lancet 2005, 366, 1578–1582. [Google Scholar] [CrossRef]
- Abegunde, D.O.; Mathers, C.D.; Adam, T.; Ortegon, M.; Strong, K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet 2007, 370, 1929–1938. [Google Scholar] [CrossRef]
- World Health Organization. New Data Highlight Increases in Hypertension, Diabetes Incidence. Available online: http://www.who.int/mediacentre/news/releases/2012/world_health_statistics_20120516/zh/ (accessed on 13 June 2012).
- He, H.; Yu, Y.Q.; Li, Y.; Kou, C.Q.; Li, B.; Tao, Y.C.; Zhen, Q.; Wang, C.; Joseph, S.K.; Huang, X.F.; et al. Dyslipidemia awareness, treatment, control and influence factors among adults in the Jilin province in China: A cross-sectional study. Lipids Health Dis. 2014, 13. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.X.; Gao, L.; Xie, X.P.; Tan, S.C. Epidemiology of dyslipidemia in Chinese adults: Meta-analysis of prevalence, awareness, treatment, and control. Popul. Health Metr. 2014, 12. [Google Scholar] [CrossRef] [PubMed]
- Cai, L.; Zhang, L.; Liu, A.P.; Li, S.P.; Wang, P.Y. Prevalence, awareness, treatment, and control of dyslipidemia among adults in Beijing, China. J. Atheroscler. Thromb. 2012, 19, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.Y.; Duan, X.Y.; Li, L.; Dai, F.; Li, Y.Y.; Li, X.J.; Fan, J.G. Dyslipidemia in Shanghai, China. Prev. Med. 2010, 51, 412–415. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; World Heart Federation; World Stroke Organization. Global Atlas on Cardiovascular Disease Prevention and Control: Policies, Strategies and Interventions. Available online: http://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/ (accessed on 11 February 2014).
- Guo, S.X.; Ma, R.L.; Guo, H.; Ding, Y.S.; Liu, J.M.; Zhang, M.; Zhang, J.Y.; Xu, S.Z.; Li, S.G.; Rui, D.S.; et al. Epidemiological analysis of dyslipidemia in adults of three ethnicities in Xinjiang, China. Genet. Mol. Res. 2014, 13, 2385–2393. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.P.; Ma, R.L.; Zhang, M.; Liu, J.M.; Ding, Y.S.; Guo, H.; Zhang, J.Y.; Li, S.G.; Sun, F.; Guo, S.X. Epidemic features of dyslipidemia among Uygur, Kazakh, and Han adults in Xinjiang, China in 2010. Chin. J. Prev. Med. 2013, 47, 949–953. [Google Scholar]
- Yao, X.G.; Frommlet, F.; Zhou, L.; Zu, F.; Wang, H.M.; Yan, Z.T.; Luo, W.L.; Hong, J.; Wang, X.L.; Li, N.F. The prevalence of hypertension, obesity and dyslipidemia in individuals of over 30 years of age belonging to minorities from the pasture area of Xinjiang. BMC Public Health 2010, 10. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.H.; Zhang, J.; Zhai, Y.; You, Y.; Man, Q.Q.; Wang, C.R.; Li, H.; Li, Y.; Yang, X.G. Blood lipid profile and prevalence of dyslipidemia in Chinese adults. Biomed. Environ. Sci. 2007, 20, 329–335. [Google Scholar] [PubMed]
- Zhao, W.H.; Zhang, J.; You, Y.; Man, Q.Q.; Li, G.; Wang, C.R.; Di, Y.; Li, Y.; Jin, S.G.; Yang, X.G. Epidemiologic characteristics of dyslipidemia in people aged 18 years and over in China. Chin. J. Prev. Med. 2005, 35, 306–310. [Google Scholar]
- Li, J.H.; Wang, L.R.; Li, Y.C.; Bi, Y.F.; Jiang, Y.; Mi, S.Q.; Dai, M.; Xu, Y.; Ning, G.; Zhao, W.H. Epidemioiogic characteristics of dyslipidemia in Chinese adults in 2010. Chin. J. Prev. Med. 2012, 46, 414–418. [Google Scholar]
- Luo, J.Y.; Ma, Y.T.; Yu, Z.X.; Yang, Y.N.; Xie, X.; Ma, X.; Liu, F.; Li, X.M.; Chen, B.D. Prevalence, awareness, treatment and control of dyslipidemia among adults in Northwestern China: The cardiovascular risk survey. Lipids Health Dis. 2014, 13. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.P.; Ding, Y.S.; Ma, R.L.; Guo, H.; Liu, J.M.; Zhang, M.; Zhang, J.Y.; Guo, S.X. Distribution and influencing factors of dyslipidemia in Uygur adults. Chin. J. Endocrinol. Metabol. 2013, 29, 690–692. [Google Scholar]
- Zhang, J.D.; Zhuang, N.; Gao, L.J. Evaluation of the effectiveness of dyslipidemia health management in a community. Chin. J. Gen. Pract. 2011, 10, 890–891. [Google Scholar]
- Nishiwaki, M.; Ikewaki, K.; Ayaori, M.; Mizuno, K.; Ohashi, Y.; Ohsuzu, F.; Ishikawa, T.; Nakamura, H.; MEGA Study Group. Risk reductions for cardiovascular disease with pravastatin treatment by dyslipidemia phenotype: A post hoc analysis of the MEGA Study. J. Cardiol. 2013, 61, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Li, J.H.; Wang, L.M.; Mi, S.Q.; Zhang, M.; Li, Y.C.; Jiang, Y.; Xu, Y.; Dai, M.; Wang, L.H. Awareness rate, treatment rate and control rate of dyslipidemia in Chinese adults, 2010. Chin. J. Prev. Med. 2012, 46, 687–691. [Google Scholar]
- Lai, J.T.; Wu, B.F.; Xuan, T.M.; Liu, Z.; Chen, J.Z. Efficacy and tolerability of adding coenzyme A400 U/d capsule to stable statin therapy for the treatment of patients with mixed dyslipidemia: An 8-week, multicenter, double-Blind, randomized, placebo-controlled study. Lipids Health Dis. 2014, 13, 1–9. [Google Scholar] [CrossRef]
- Koren, M.J.; Hunninghake, D.B.; ALLIANCE Investigators. Clinical outcomes in managed-care patients with coronary heart disease treated aggressively in lipid-lowering disease management clinics: The alliance study. J. Am. Coll. Cardiol. 2004, 44, 1772–1779. [Google Scholar] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, J.; Guo, S.; Ma, R.; Zhang, J.; Liu, J.; Ding, Y.; Zhang, M.; Guo, H.; He, J.; Yan, Y.; et al. An Evaluation on the Effect of Health Education and of Low-Dose Statin in Dyslipidemia among Low-Income Rural Uyghur Adults in Far Western China: A Comprehensive Intervention Study. Int. J. Environ. Res. Public Health 2015, 12, 11410-11421. https://doi.org/10.3390/ijerph120911410
Ma J, Guo S, Ma R, Zhang J, Liu J, Ding Y, Zhang M, Guo H, He J, Yan Y, et al. An Evaluation on the Effect of Health Education and of Low-Dose Statin in Dyslipidemia among Low-Income Rural Uyghur Adults in Far Western China: A Comprehensive Intervention Study. International Journal of Environmental Research and Public Health. 2015; 12(9):11410-11421. https://doi.org/10.3390/ijerph120911410
Chicago/Turabian StyleMa, Jiaolong, Shuxia Guo, Rulin Ma, Jingyu Zhang, Jiaming Liu, Yusong Ding, Mei Zhang, Heng Guo, Jia He, Yizhong Yan, and et al. 2015. "An Evaluation on the Effect of Health Education and of Low-Dose Statin in Dyslipidemia among Low-Income Rural Uyghur Adults in Far Western China: A Comprehensive Intervention Study" International Journal of Environmental Research and Public Health 12, no. 9: 11410-11421. https://doi.org/10.3390/ijerph120911410






