Matrix Metalloproteinase 9 Gene Promoter (rs 3918242) Mutation Reduces the Risk of Diabetic Microvascular Complications
Abstract
:1. Introduction
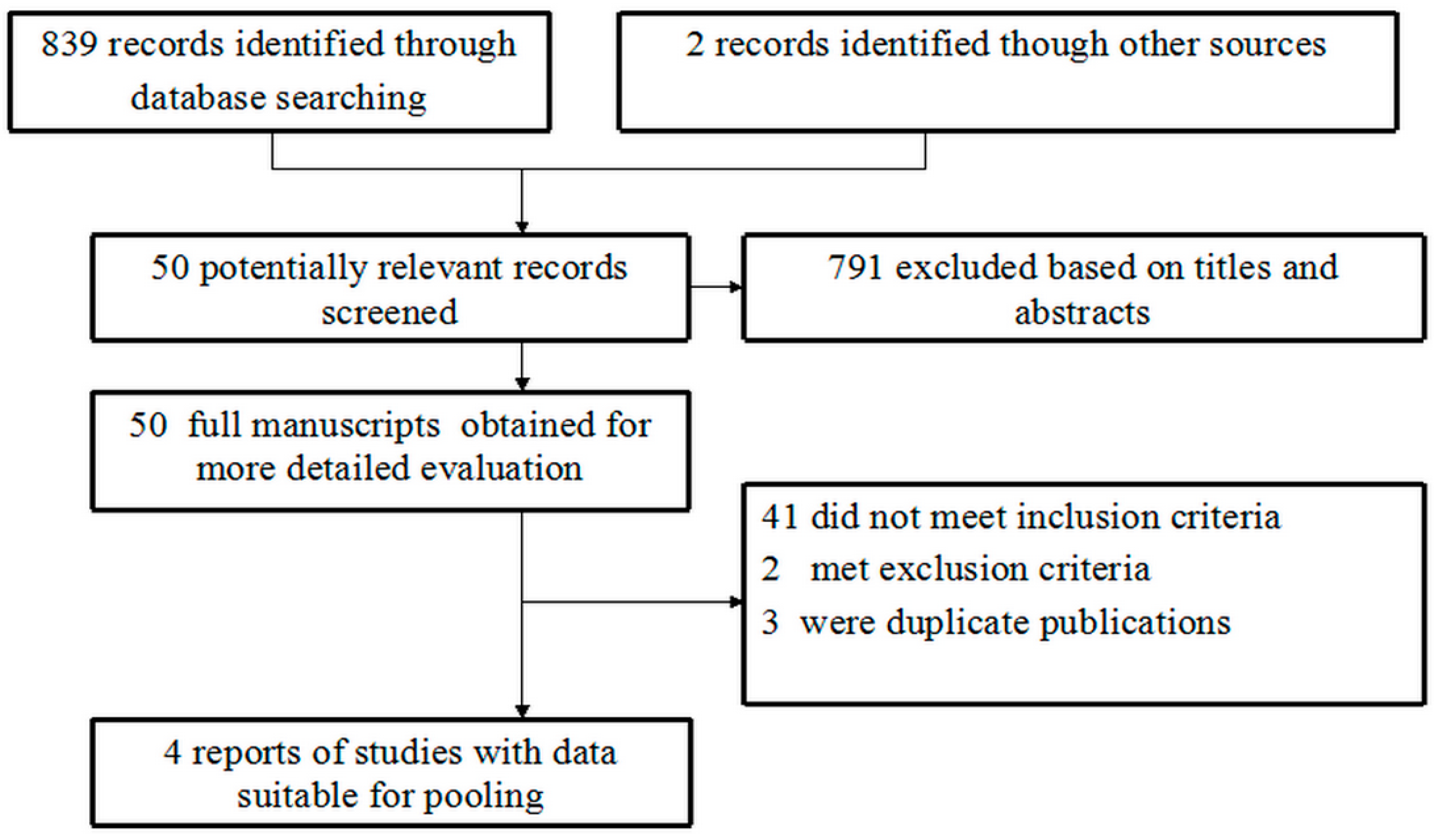
2. Experimental Section
2.1. Search Strategy
2.2. Inclusion Criteria and Information Extracted
2.3. Data Extraction
| First author | Ethnicity | Subjects, N cases/controls | Mean age, y cases/controls | Genotypes (CC/CT/TT) | % of male (cases/controls) | Test for HWE X2 P |
|---|---|---|---|---|---|---|
| cases/controls | ||||||
| ML Pang et al. (2010) | Asian | 150/52 | 57.4 ± 14.1/ 58.7 ± 15.3 | 77/30/43 24/6/22 | 52.5/22.4 | 29.3 p < 0.05 |
| M Beránek et al. (2008) | Caucasian | 304/186 | 62.3 ± 0.7/ 59.4 ± 0.9 | 220/79/5 134/49/3 | NA/NA | 1.08 p = 0.29 |
| K Singh et al. (2013) | Caucasian | 259/267 | 55.3 ± 8.9/ 51.4 ± 10.5 | 164/91/4 196/69/2 | 85.0/85.2 | 2.56 p = 0.10 |
| KZ Liu et al. (2003) | Asian | 230/110 | 63.4 ± 9.2/ 64.2 ± 11.0 | 196/31/3 85/23/2 | 57.4/45.5 | 0.16 p = 0.68 |
2.4. Statistical Analysis
3. Results and Discussion
3.1. Study Characteristics
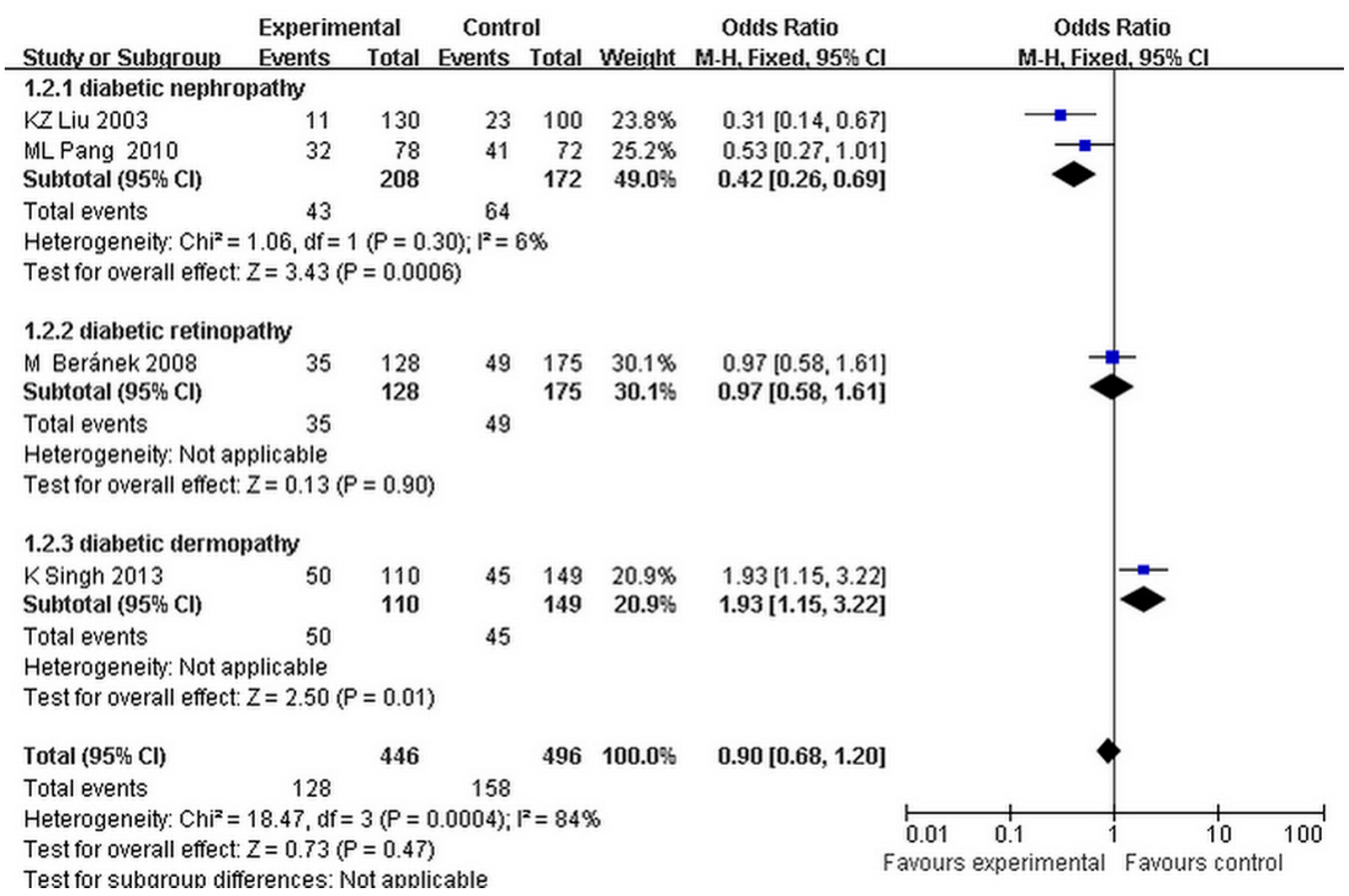
3.2. Main Meta-Analysis Results
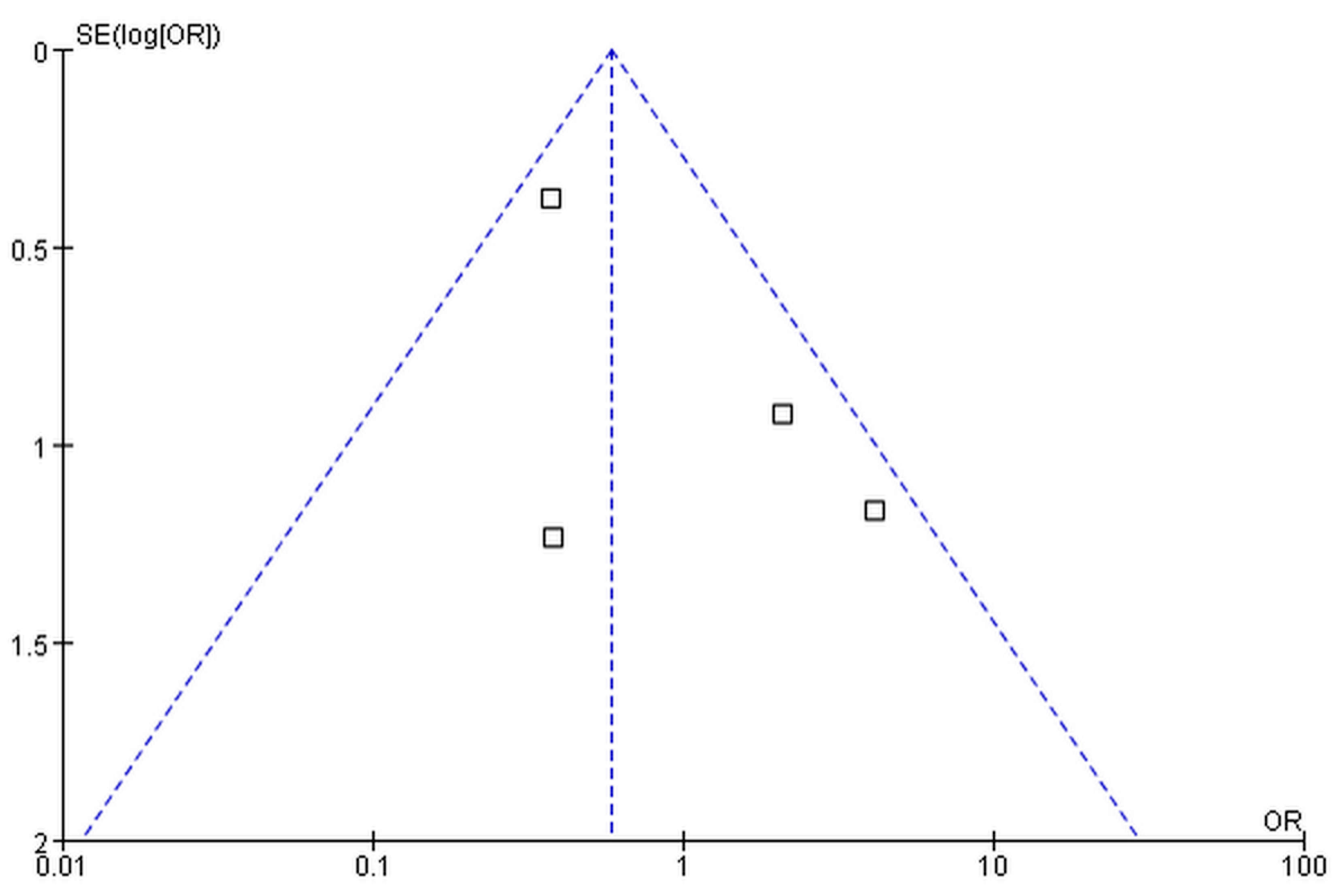
3.3. Publication Bias
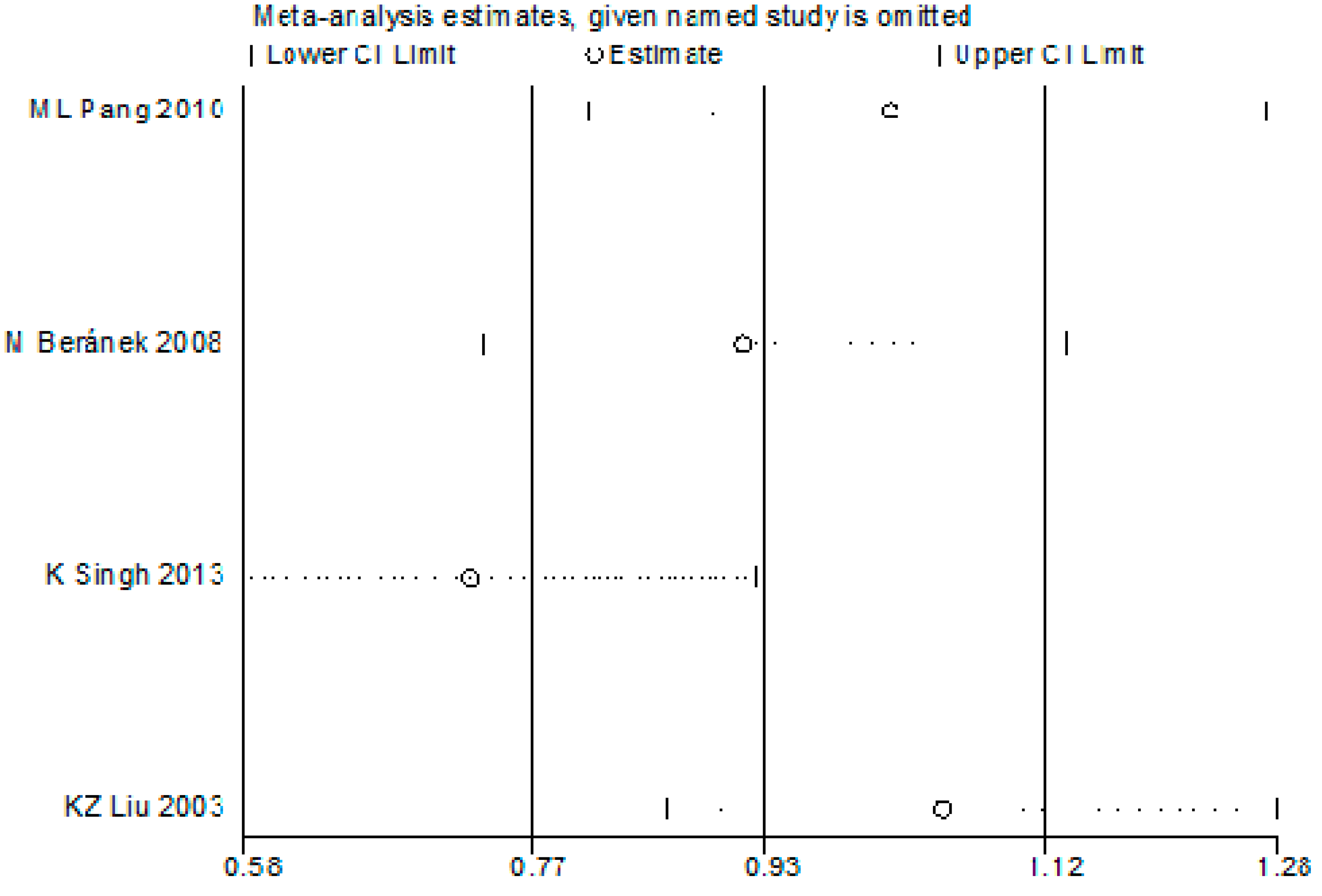
3.4. Sensitivity Analysis
3.5. Discussion
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Nathan, D.M. Navigating the choices for diabetes prevention. New Engl. J. Med. 2010, 362, 1533–1535. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Guo, S.; He, F.; Zhang, M.; He, J.; Yan, Y.; Ding, Y.; Zhang, J.; Liu, J.; Guo, H.; et al. Prevalence of diabetes mellitus and impaired fasting glucose, associated with risk factors in rural Kazakh adults in Xinjiang, China. Int. J. Environ. Res. Public Health 2015, 12, 554–565. [Google Scholar] [CrossRef] [PubMed]
- Reusch, J.E. Diabetes, microvascular complications, and cardiovascular complications: What is it about glucose? J. Clin. Invest. 2003, 112, 986–988. [Google Scholar] [CrossRef] [PubMed]
- Rosenson, R.S.; Fioretto, P.; Dodson, P.M. Does microvascular disease predict macrovascular events in type 2 diabetes? Atherosclerosis 2011, 218, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Estacio, R.O.; Dale, R.A.; Schrier, R.; Krantz, M.J. Relation of reduction in urinary albumin excretion to ten-year cardiovascular mortality in patients with type 2 diabetes and systemic hypertension. Am. J. Cardiol. 2012, 109, 1743–1748. [Google Scholar] [CrossRef] [PubMed]
- Adler, A.I.; Stratton, I.M.; Neil, H.A.; Yudkin, J.S.; Matthews, D.R.; Cull, C.A.; Wright, A.D.; Turner, R.C.; Holman, R.R. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): Prospective observational study. BMJ 2000, 321, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Raman, R.; Gupta, A.; Krishna, S.; Kulothungan, V.; Sharma, T. Prevalence and risk factors for diabetic microvascular complications in newly diagnosed type II diabetes mellitus. Sankara Nethralaya diabetic retinopathy epidemiology and molecular genetic study (SN-Dreams, report 27). J. Diabetes Complication. 2012, 26, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Liu, J.; Wang, H.; Wu, H.; Wu, X.; Dong, J.; Liao, L. Association between chemokine receptor 5 (CCR5) Delta32 gene variant and atherosclerosis: A meta-analysis of 13 studies. Int. J. Clin. Exp. Med. 2015, 8, 658–665. [Google Scholar] [PubMed]
- McDonough, C.W.; Bostrom, M.A.; Lu, L.; Hicks, P.J.; Langefeld, C.D.; Divers, J.; Mychaleckyj, J.C.; Freedman, B.I.; Bowden, D.W. Genetic analysis of diabetic nephropathy on chromosome 18 in African Americans: Linkage analysis and dense SNP mapping. Hum. Genet. 2009, 126, 805–817. [Google Scholar] [CrossRef] [PubMed]
- Tian, C.; Fang, S.; Du, X.; Jia, C. Association of the c47t polymorphism in SOD2 with diabetes mellitus and diabetic microvascular complications: A meta-analysis. Diabetologia 2011, 54, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Abhary, S.; Hewitt, A.W.; Burdon, K.P.; Craig, J.E. A systematic meta-analysis of genetic association studies for diabetic retinopathy. Diabetes 2009, 58, 2137–2147. [Google Scholar] [CrossRef] [PubMed]
- Petrovic, D. Candidate genes for proliferative diabetic retinopathy. Bio. Med. Res. Int. 2013, 2013, 540416. [Google Scholar] [CrossRef] [PubMed]
- Lauria, G.; Ziegler, D.; Malik, R.; Merkies, I.S.; Waxman, S.G.; Faber, C.G.; group, P.S. The role of sodium channels in painful diabetic and idiopathic neuropathy. Cur. Diabetes Rep. 2014, 14, 538. [Google Scholar] [CrossRef] [PubMed]
- Bour-Jordan, H.; Thompson, H.L.; Giampaolo, J.R.; Davini, D.; Rosenthal, W.; Bluestone, J.A. Distinct genetic control of autoimmune neuropathy and diabetes in the non-obese diabetic background. J. Autoimmun. 2013, 45, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Makuc, J.; Petrovic, D. A review of oxidative stress related genes and new antioxidant therapy in diabetic nephropathy. Cardiovasc. Hematol. Agents. Med. 2011, 9, 253–261. [Google Scholar]
- McAuley, A.K.; Wang, J.J.; Dirani, M.; Connell, P.P.; Lamoureux, E.; Hewitt, A.W. Replication of genetic loci implicated in diabetic retinopathy. Invest. Ophthalmol. Visual Sci. 2014, 55, 1666–1671. [Google Scholar]
- McKnight, A.J.; Currie, D.; Patterson, C.C.; Maxwell, A.P.; Fogarty, D.G.; Warren 3/UK GoKinD Study Group. Targeted genome-wide investigation identifies novel snps associated with diabetic nephropathy. HUGO J. 2009, 3, 77–82. [Google Scholar] [CrossRef] [PubMed]
- McKnight, A.J.; Maxwell, A.P.; Fogarty, D.G.; Sadlier, D.; Savage, D.A.; Warren 3/UK GoKinD Study Group. Genetic analysis of coronary artery disease single-nucleotide polymorphisms in diabetic nephropathy. Nephrol. Dialysis Transplant. 2009, 24, 2473–2476. [Google Scholar] [Green Version]
- Pfeiffer, A.; Schatz, H. Diabetic microvascular complications and growth factors. Exp. Clin. Endocrinol. Diabetes 1995, 103, 7–14. [Google Scholar]
- Zhang, Z.; Dong, J.; Lobe, C.G.; Gong, P.; Liu, J.; Liao, L. Ccr5 facilitates endothelial progenitor cell recruitment and promotes the stabilization of atherosclerotic plaques in APOE(-/-) mice. Stem Cell Res. Ther. 2015, 6, 36. [Google Scholar] [CrossRef] [PubMed]
- Van Gieson, E.J.; Skalak, T.C. Chronic vasodilation induces matrix metalloproteinase 9 (MMP-9) expression during microvascular remodeling in rat skeletal muscle. Microcirculation 2001, 8, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Wang, Q.; Ma, Z.W.; Chen, F.M.; Chen, Y.; Xie, G.Y.; Wang, Q.T.; Wu, Z.F. MMP-2, MMP-9 and TIMP-2 gene polymorphisms in Chinese patients with generalized aggressive periodontitis. J. Clin. Periodontol. 2007, 34, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Schveigert, D.; Valuckas, K.P.; Kovalcis, V.; Ulys, A.; Chvatovic, G.; Didziapetriene, J. Significance of MMP-9 expression and MMP-9 polymorphism in prostate cancer. Tumori 2013, 99, 523–529. [Google Scholar] [PubMed]
- Singh, K.; Agrawal, N.K.; Gupta, S.K.; Singh, K. A functional single nucleotide polymorphism -1562c > t in the matrix metalloproteinase-9 promoter is associated with type 2 diabetes and diabetic foot ulcers. Int. J. Lower Extremity Wounds 2013, 12, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Ahluwalia, T.S.; Khullar, M.; Ahuja, M.; Kohli, H.S.; Bhansali, A.; Mohan, V.; Venkatesan, R.; Rai, T.S.; Sud, K.; Singal, P.K. Common variants of inflammatory cytokine genes are associated with risk of nephropathy in type 2 diabetes among Asian Indians. PLoS ONE 2009, 4, e5168. [Google Scholar] [CrossRef] [PubMed]
- Beranek, M.; Kolar, P.; Tschoplova, S.; Kankova, K.; Vasku, A. Genetic variations and plasma levels of gelatinase a (matrix metalloproteinase-2) and gelatinase b (matrix metalloproteinase-9) in proliferative diabetic retinopathy. Mol. Vis. 2008, 14, 1114–1121. [Google Scholar] [PubMed]
- Liu, K.Z.; Chen, Y.J.; Wang, Z.J.; Li, Y.K.; Wen, J.K. Association of matrix metalloproteinase-9 gene polymorphism to angiopathy in type 2 diabetes mellitus. Chin. J. Endocrinol. Metab. 2003, 19, 442–444. [Google Scholar]
- Pang, M.L.; Zhang, X.M.; Sun, W.H.; Xu, H.B.; Shi, Z.M.; Tian, G. Study on the relationship between matrix metalloproteinase-9 gene-1562C/T polymorphism and diabetic nephropathy. Tianjin Med. J. 2010, 38, 644–647. [Google Scholar]
- Hao, P.P.; Chen, Y.G.; Wang, J.L.; Wang, X.L.; Zhang, Y. Meta-analysis of aldehyde dehydrogenase 2 gene polymorphism and Alzheimer's disease in East Asians. Can. J. Neurol. Sci. 2011, 38, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Khairoun, M.; de Koning, E.J.; van den Berg, B.M.; Lievers, E.; de Boer, H.C.; Schaapherder, A.F.; Mallat, M.J.; Rotmans, J.I.; van der Boog, P.J.; van Zonneveld, A.J.; et al. Microvascular damage in type 1 diabetic patients is reversed in the first year after simultaneous pancreas-kidney transplantation. Am. J. Transplant. 2013, 13, 1272–1281. [Google Scholar] [CrossRef] [PubMed]
- Uemura, S.; Matsushita, H.; Li, W.; Glassford, A.J.; Asagami, T.; Lee, K.H.; Harrison, D.G.; Tsao, P.S. Diabetes mellitus enhances vascular matrix metalloproteinase activity: Role of oxidative stress. Circ. Res. 2001, 88, 1291–1298. [Google Scholar] [CrossRef] [PubMed]
- Salanti, G.; Sanderson, S.; Higgins, J.P. Obstacles and opportunities in meta-analysis of genetic association studies. Genet. Med. 2005, 7, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Mooyaart, A.L.; Valk, E.J.; van Es, L.A.; Bruijn, J.A.; de Heer, E.; Freedman, B.I.; Dekkers, O.M.; Baelde, H.J. Genetic associations in diabetic nephropathy: A meta-analysis. Diabetologia 2011, 54, 544–553. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Z.; Wu, X.; Cai, T.; Gao, W.; Zhou, X.; Zhao, J.; Yao, J.; Shang, H.; Dong, J.; Liao, L. Matrix Metalloproteinase 9 Gene Promoter (rs 3918242) Mutation Reduces the Risk of Diabetic Microvascular Complications. Int. J. Environ. Res. Public Health 2015, 12, 8023-8033. https://doi.org/10.3390/ijerph120708023
Zhang Z, Wu X, Cai T, Gao W, Zhou X, Zhao J, Yao J, Shang H, Dong J, Liao L. Matrix Metalloproteinase 9 Gene Promoter (rs 3918242) Mutation Reduces the Risk of Diabetic Microvascular Complications. International Journal of Environmental Research and Public Health. 2015; 12(7):8023-8033. https://doi.org/10.3390/ijerph120708023
Chicago/Turabian StyleZhang, Zhongwen, Xiaoyun Wu, Tian Cai, Weiyi Gao, Xiaojun Zhou, Junyu Zhao, Jinming Yao, Hongxia Shang, Jianjun Dong, and Lin Liao. 2015. "Matrix Metalloproteinase 9 Gene Promoter (rs 3918242) Mutation Reduces the Risk of Diabetic Microvascular Complications" International Journal of Environmental Research and Public Health 12, no. 7: 8023-8033. https://doi.org/10.3390/ijerph120708023





