Adult Psychotic Symptoms, Their Associated Risk Factors and Changes in Prevalence in Men and Women Over a Decade in a Poor Rural District of Kenya
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
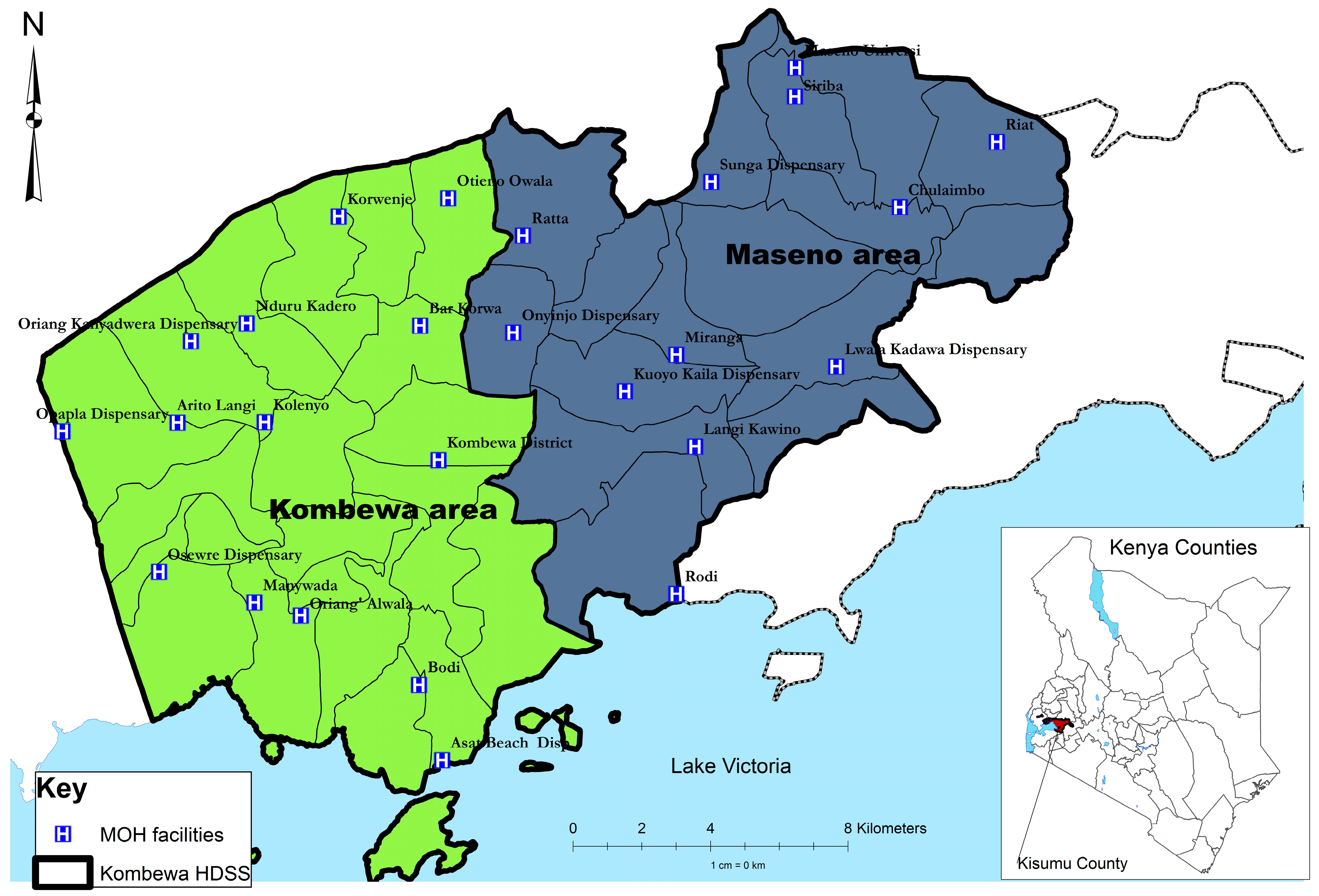
2.2. Study Site
2.3. Study Participants
2.4. Study Procedures
2.5. Statistical Analysis
2.6. Ethics
3. Results
| Psychosis Screening Questionnaire Items | N (%) | |
|---|---|---|
| Felt very happy indeed without a break for days on end:n(%) | 64 (5.7) | |
| Ever felt like your thoughts are interfered with or controlled: n (%) | 14 (1.3) | |
| Ever felt that people are against you: n (%) | 75 (6.7) | |
| Ever felt that something strange was going on: n (%) | 35 (3.1) | |
| Heard or seen things that others couldn’t: n (%) | 21 (1.9) | |
| Total PSQ score | 0 | 965 (86.1) |
| 1 and above | 156 (13.9) | |
| 2 and above | 43 (3.8) | |
| 3 and above | 8 (0.7) | |
| 4 | 2 (0.2) | |
| Factors | N | Prevalence of Psychotic Symptoms (%) | Unadjusted OR (95% CI) | p-Value | |
|---|---|---|---|---|---|
| One or more psychotic symptom * | 1121 | 156 (13.9) | |||
| Sex | Male | 595 | 63 (10.6) | 1 | - |
| Female | 524 | 93 (17.8) | 1.8 (1.29 to 2.57) | 0.001 | |
| Age group | <30 years (yrs) | 274 | 48 (17.5) | 1 | - |
| 30–60 yrs | 442 | 59 (13.4) | 0.7 (0.47 to 1.10) | 0.129 | |
| >60 yrs | 167 | 18 (10.8) | 0.6 (0.32 to 1.06) | 0.056 | |
| Household size | ≤6 people | 563 | 73 (13.0) | 1 | - |
| >6 people | 556 | 83 (14.9) | 1.2 (0.84 to 1.65) | 0.344 | |
| Marital Status | Married/cohabiting | 698 | 86 (12.3) | 1 | - |
| Single | 180 | 36 (20.0) | 1.8 (1.16 to 2.73) | 0.009 | |
| Widowed/divorced | 240 | 34 (14.2) | 1.2 (0.77 to 1.80) | 0.461 | |
| Education | None | 121 | 18 (14.9) | 1 | - |
| Primary | 612 | 78 (12.8) | 0.8 (0.48 to 1.45) | 0.526 | |
| Secondary | 318 | 45 (14.2) | 0.9 (0.52 to 1.70) | 0.846 | |
| Post secondary | 68 | 15 (22.1) | 1.6 (0.76 to 3.47) | 0.214 | |
| Employment status | Unemployed | 545 | 80 (14.7) | 1 | - |
| Self employed | 477 | 65 (13.6) | 0.9 (0.64 to 1.31) | 0.631 | |
| Employed | 97 | 11 (11.3) | 0.7 (0.38 to 1.45) | 0.387 | |
| Asset Groups | Lowest, Q1 | 397 | 59 (15.3) | 1 | - |
| Q2 | 395 | 50 (12.7) | 0.8 (0.54 to 1.21) | 0.303 | |
| Highest, Q3 | 329 | 47 (13.7) | 0.9 (0.58 to 1.34) | 0.556 | |
| Perceived social support | No lack : 0 | 3 | 2 (66.7) | 1 | - |
| Moderate lack: 1–7 | 309 | 43 (13.9) | 0.08 (0.07 to 0.91) | 0.042 | |
| Severe lack: 8+ | 804 | 111 (13.8) | 0.08 (0.07 to 0.89) | 0.040 | |
| Size of primary support group | 0–3 | 140 | 16 (11.4) | 1 | - |
| 4–8 | 506 | 67 (13.2) | 1.2 (0.66 to 2.11) | 0.571 | |
| 9 or more | 470 | 73 (15.5) | 1.4 (0.80 to 2.54) | 0.229 | |
| Number of life events in last 6 months | 0–1 | 345 | 28 (8.1) | 1 | - |
| 2–3 | 466 | 80 (17.2) | 2.3 (1.49 to 3.70) | <0.001 | |
| 4+ | 308 | 48 (15.6) | 2.1 (1.28 to 3.43) | 0.003 | |
| Any CMD | No | 1007 | 119 (11.8) | 1 | - |
| Yes | 112 | 37 (33.0) | 3.7 (2.38 to 5.70) | <0.001 | |
| Current alcohol | No | 1016 | 139 (13.7) | 1 | - |
| Yes | 103 | 17 (16.5) | 1.2 (0.72 to 2.16) | 0.431 | |
| Hazardous drinking | No | 1048 | 144 (13.7) | 1 | - |
| Yes | 71 | 12 (16.9) | 1.3 (0.67 to 2.43) | 0.458 | |
| Positive | 262 | 39 (14.9) | 1.1 (0.74 to 1.67) | 0.601 | |
| Carer for more than 4 hours a week | No | 26 | 2 (7.7) | 1 | - |
| Yes | 168 | 34 (20.2) | 3.0 (0.69 to 13.5) | 0.143 | |
| Spent time in institution before age 16 | No | 895 | 118 (13.2) | 1 | - |
| Yes | 217 | 36 (16.6) | 1.3 (0.87 to 2.0) | 0.194 | |
| Did not have both natural parents at home until age 16 | No | 945 | 123 (13.0) | 1 | - |
| Yes | 167 | 31 (18.6) | 1.5 (0.99 to 2.35) | 0.057 | |
| Variable | Adjusted OR (95% CI) | p-Value | |
|---|---|---|---|
| Sex (=female) | 1.7 (1.18 to 2.53) | 0.005 | |
| Marital Status | Single | 2.0 (1.28 to 3.13) | 0.002 |
| Widowed/divorced | 0.6 (0.40 to 1.05) | 0.078 | |
| Number of life events | 2–3 | 2.6 (1.61 to 4.13) | <0.001 |
| 4+ | 1.9 (1.15 to 3.19) | 0.013 | |
| Perceived social support | Moderate lack of support | 0.1 (0.01 to 1.25) | 0.075 |
| Severe lack of support | 0.1 (0.01 to 1.46) | 0.097 | |
| Any CMD | 4.0 (2.45 to 6.56) | <0.001 | |
| Psychotic Symptoms | Sex | Prevalence: 2004 | Prevalence: 2013 | p-Value * |
|---|---|---|---|---|
| PSQ (1+) | Total | 8.1 | 13.9 | 0.001 |
| Male | 9.4 | 10.6 | 0.582 | |
| Female | 6.9 | 17.8 | <0.001 |
| Factors | N | Prevalence: n (%) | Unadjusted OR (95% CI) | p-value | |
|---|---|---|---|---|---|
| Prevalence of PTSD | 1121 | 156 (13.9) | |||
| Serious illness, injury or assault to self | No | 791 | 121 (15.3) | 1 | - |
| Yes | 328 | 35 (10.7) | 0.7 (0.44 to 0.99) | 0.043 | |
| Serious illness, injury or assault to a close relative | No | 794 | 96 (12.1) | 1 | - |
| Yes | 325 | 60 (18.5) | 1.6 (1.16 to 2.34) | 0.006 | |
| Death of an immediate family member of yours | No | 431 | 58 (13.5) | 1 | - |
| Yes | 688 | 98 (14.2) | 1.1 (0.75 to 1.52) | 0.711 | |
| Death of a close family friend or other relative | No | 669 | 101 (15.1) | 1 | - |
| Yes | 450 | 55 (12.2) | 0.8 (0.55 to 1.11) | 0.174 | |
| Separation due to marital differences, divorce or steady relationship broken | No | 1088 | 151 (13.9) | 1 | - |
| Yes | 31 | 5 (16.1) | 1.2 (0.45 to 3.16) | 0.722 | |
| Serious problem with a close friend, neighbour or relative | No | 1021 | 141 (13.8) | 1 | - |
| Yes | 98 | 15 (15.3) | 1.1 (0.63 to 2.01) | 0.683 | |
| Being made redundant or sacked from your job | No | 1066 | 152 (14.3) | 1 | - |
| Yes | 53 | 4 (7.6) | 0.5 (0.17 to 1.38) | 0.177 | |
| Looking for work without success for >1 month | No | 972 | 134 (13.8) | 1 | - |
| Yes | 147 | 22 (15.0) | 1.1 (0.68 to 1.79) | 0.700 | |
| Major financial crisis, like losing an equivalent of 3months income | No | 858 | 106 (12.4) | 1 | - |
| Yes | 261 | 50 (19.2) | 1.7 (1.16 to 2.43) | 0.006 | |
| Problem with police involving court appearance | No | 1082 | 152 (14.1) | 1 | - |
| Yes | 37 | 4 (10.8) | 0.7 (0.26 to 2.12) | 0.578 | |
| Something you valued being lost or stolen | No | 963 | 133 (13.8) | 1 | - |
| Yes | 156 | 23 (14.7) | 1.1 (0.67 to 1.74) | 0.755 | |
| Bullying | No | 1066 | 143 (13.4) | 1 | - |
| Yes | 53 | 13 (24.5) | 2.1 (1.10 to 4.02) | 0.025 | |
| Violence at work | No | 1071 | 150 (14.0) | 1 | - |
| Yes | 48 | 6 (12.5) | 0.9 (0.37 to 2.10) | 0.768 | |
| Violence at home | No | 911 | 116 (12.7) | 1 | - |
| Yes | 208 | 40 (19.2) | 1.6 (1.10 to 2.42) | 0.015 | |
| Sexual abuse | No | 1113 | 156 (14.0) | 1 | - |
| Yes | 6 | 0 (-) | - | - | |
| Being expelled from school | No | 1086 | 150 (13.8) | 1 | - |
| Yes | 33 | 6 (18.2) | 1.4 (0.56 to 3.41) | 0.477 | |
| Running away from your home | No | 1093 | 147 (13.5) | 1 | - |
| Yes | 26 | 9 (34.6) | 3.4 (1.49 to 7.76) | 0.004 | |
| Being homeless | No | 1105 | 154 (13.9) | 1 | - |
| Yes | 14 | 2 (14.3) | 1.0 (0.23 to 4.64) | 0.970 |
4. Discussion
5. Conclusions
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Knapp, M.; Mangalore, R.; Simon, J. The global costs of schizophrenia. Schizophr. Bull. 2004, 30, 279–293. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Neurological, Psychiatric, and Developmental Disorders: Meeting the Challenge in the Developing World; National Academy Press: Washington, DC, USA, 2001. [Google Scholar]
- Kebede, D.; Alem, A. Major mental disorders in Addis Ababa, Ethiopia: I. Schizophrenia, schizoaffective and cognitive disorders. Acta Psychiatr. Scand. 1999, 100, 11–17. [Google Scholar] [CrossRef]
- Patel, V.; Simbine, A.P.F.; Soares, I.C.; Weiss, H.A.; Wheeler, E. Prevalence of severe mental and neurological disorders in Mozambique: A population-based survey. Lancet 2007, 370, 1055–1060. [Google Scholar] [CrossRef] [PubMed]
- Johns, L.C.; Cannon, M.; Singleton, N.; Murray, R.M.; Farrell, M.; Brugha, T.; Bebbington, P.; Jenkins, R.; Meltzer, H. Prevalence and correlates of self-reported psychotic symptoms in the British population. Brit. J. Psychiatr. 2004, 185, 298–305. [Google Scholar] [CrossRef]
- Brugha, T.; Singleton, N.; Melzer, H.; Bebbington, T.; Farrell, M.; Jenkins, R.; Coid, J.; Fryers, T.; Melzer, D.; Lewis, G. Psychosis in the community and in prisons: A report from the British national survey of psychiatric morbidity. Am. J. Psychiatry 2005, 162, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, R.; Njenga, F.; Okonji, M.; Kigamwa, P.; Baraza, M.; Ayuyo, J.; Singleton, N.; McManus, S.; Kiima, D. Psychotic symptoms in Kenya—Prevalence and risk factors, including their relationship with common mental disorders. Int. J. Environ. Res. Public Health 2012, 9, 1748–1756. [Google Scholar] [CrossRef] [PubMed]
- Sifuna, P.; Oyugi, M.; Ogutu, B.; Andagalu, B.; Otieno, A.; Owira, V.; Otsyula, N.; Oyieko, J.; Cowden, J.; Otieno, L.; et al. Health & demographic surveillance system profile: The Kombewa Health and Demographic Surveillance System (Kombewa HDSS). Int. J. Epidemiol. 2014. [Google Scholar] [CrossRef]
- Kish, L. A procedure for objective respondent selection within households. J. Am. Stat. Assoc. 1949, 46, 380–387. [Google Scholar] [CrossRef]
- National Mental Health Surveys Carried Out in Great Britain. Available online: www.mentalhealthsurveys.co.uk (accessed on 12 May 2015).
- Lewis, G.; Pelosi, A.; Araya, R.C.; Dunn, G. Measuring psychiatric disorder in the community: A standardised assessment for use by lay interviewers. Psychol. Med. 1992, 22, 465–489. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, R.; Bebbington, P.; Brugha, T.; Farrell, M.; Gill, B.; Lewis, G.; Meltzer, H.; Petticrew, M. The national psychiatric morbidity surveys of Great Britain—Strategy and methods. Psychol. Med. 1997, 27, 765–774. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, H.; Gill, B.; Petticrew, M.; Hinds, K. OPCS Survey of Psychiatric Morbidity: Report 1. The Prevalence of Psychiatric Morbidity among Adults Ages 16–64 Living in Private Households in Great Britain; HMSO: London, UK, 1995. [Google Scholar]
- Singleton, N.; Bumpstead, R.; O’Brien, M.; Lee, A.; Meltzer, H. Psychiatric morbidity among adults living in private households, 2000. Int. Rev. Psychiatr. 2003, 15, 65–73. [Google Scholar] [CrossRef]
- Patel, V.; Kirkwood, B.R.; Pednekar, S.; Weiss, H.; Mabey, D. Risk factors for common mental disorders in women: Population-based longitudinal study. Brit. J. Psychiat. 2006, 189, 547–555. [Google Scholar] [CrossRef] [PubMed]
- Wickramasinghe, S.C.; Rajapakse, L.; Abeysinghe, R.; Prince, M. The clinical interview schedule-Sinhala version: Validation in a community setting in Sri Lanka. Int. J. Method. Psychiatr. Res. 2002, 11, 169–177. [Google Scholar] [CrossRef]
- Araya, R.; Rojas, G.; Aritsch, R.; Acuna, J.; Lewis, G. Common mental disorders in Santiago, Chile: Prevalence and socio-demographic correlates. Brit. J. Psychiat. 2001, 178, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Ngoma, M.C.; Prince, M.; Mann, A. Common mental disorders among those attending primary health clinics and traditional healers in urban Tanzania. Brit. J. Psychiat. 2003, 183, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, R.; Mbatia, J.; Singleton, N.; White, B. Common mental disorders and risk factors in urban Tanzania. Int. J. Environ. Res. Public Health 2010, 7, 2543–2558. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, R.; Njenga, F.; Okonji, M.; Kigamwa, P.; Baraza, M.; Ayuyo, J.; Singleton, N.; McManus, S.; Kiima, D. Prevalence of common mental disorders in a rural district of Kenya, and socio-demographic risk factors. Int. J. Environ. Res. Public Health 2012, 9, 1810–1819. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems. Tenth Revision; World Health Organization: Geneva, Switzerland, 1993. [Google Scholar]
- Bebbington, P.E.; Nayani, T. The psychosis screening questionnaire. Int. J. Methods Psychiatr. Res. 1995, 5, 11–19. [Google Scholar]
- Jenkins, R.; Mbatia, J.; Singleton, N.; White, B. Prevalence of psychotic symptoms and their risk factors in urban Tanzania. Int. J. Environ. Res. Public Health 2010, 7, 2514–1525. [Google Scholar] [CrossRef] [PubMed]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, R.; Lewis, G.; Bebbington, P.; Brugha, T.; Farrell, M.; Gill, B.; Meltzer, H. The national psychiatric morbidity surveys of Great Britain—Initial findings from the household survey. Psychol. Med. 1997, 27, 775–790. [Google Scholar] [CrossRef] [PubMed]
- Breeze, E.; Maidment, A.; Bennett, N.; Flatley, J.; Carey, S. Health Survey for England, 1992; HMSO: London, UK, 1994. [Google Scholar]
- Statacorp. Stata Statistical Software: Release 11.2.; StataCorp. LP: College Station, TX, USA, 2003. [Google Scholar]
- Moser, C. The asset vulnerability framework: Reassessing urban poverty reduction strategies. World Dev. 1998, 26, 1–19. [Google Scholar] [CrossRef]
- Morris, S.S.; Carletto, C.; Hoddinott, J.; Christiaensen, L.J.M. Validity of rapid estimates of household wealth and income for health surveys in rural Africa. J. Epidemiol. Commun. Health 2000, 54, 381–387. [Google Scholar] [CrossRef]
- McManus, S.; Meltzer, T.; Bebbington, P.; Jenkins, R. Adult Psychiatric Morbidity in England 2007. Results of a Household Survey. 2009. Available online: http://www.hscic.gov.uk/pubs/psychiatricmorbidity07 (accessed on 12 May 2015). [Google Scholar]
- Subramaniam, M.; Abdin, E.; Vaingankar, J.A.; Verma, S.; Chong, S.A. Latent structure of psychosis in the general population: Results from the Singapore mental health study. Psychol. Med. 2014, 44, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Perla, J.; Suvisaari, J.; Saarni, S.I.; Kuoppasalmi, K.; Isometsa, E.; Pirkola, S.; Partonen, T.; Tuulio-Henriksson, A.; Hinlikka, J.; Kiseppa, T.; et al. Lifetime prevalence of psychotic and bipolar disorders in a general population. Arch. Gen. Psychiatr. 2007, 64, 19–28. [Google Scholar] [CrossRef]
- Ochoa, S.; Haro, J.M.; Torres, J.V.; Pinto-Meza, A.; Palacin, C.; Bernai, M.; Brigha, T.; Prat, B.; Usall, J.; Alonso, J.; Autonell, J. What is the relative importance of self reported psychotic symptoms in epidemiological studies > results from the ESEMeD-Catalonia Study. Schizophrenic Res. 2008, 102, 261–269. [Google Scholar] [CrossRef]
- Scott, J.; Chant, D.; Andrews, G.; McGrath, J. Psychotic like experiences in the general community: The correlates of CIDI psychosis screen items in an Australian sample. Psychol. Med. 2006, 2, 231–236. [Google Scholar]
- Temmingh, H.; Stein, D.J.; Seedat, S.; Williams, D.R. The prevalence and correlates of hallucinations in a general population sample: findings from the South African Stress and Health Study. Afr. J. Psychiatr. 2011. [Google Scholar] [CrossRef]
- Johns, L.C.; Nazroo, J.Y.; Bebbington, P.; Kuipers, E. Occurrence of hallucinatory experiences in a community sample and ethnic variations. Brit. J. Psychiat. 2002, 180, 174–178. [Google Scholar] [CrossRef] [PubMed]
- Mamah, D.; Mbwayo, A.; Mutiso, V.; Barch, B.M.; Constantino, J.N.; Nsofor, T.; Khasakhala, L.; Ndetei, D.M. A survey of psychosis-risk symptoms in Kenya. Compr. Psychiatr. 2012, 53, 516–524. [Google Scholar] [CrossRef]
- Ndetei, D.M.; Muriungi, S.K.; Owoso, A.; Mutiso, V.N.; Mbwayo, A.W.; Khasakhala, L.I.; Barch, D.M.; Mamah, D. Prevalence and characteristics of psychotic-like experiences in Kenyan youth. Psychiatry Res. 2012, 196, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Tien, A.Y. Distributions of hallucinations in the population. Soc. Psychiatry Psychiatr. Epidemiol. 1991, 26, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Romme, M.A.; Escher, A.D. Hearing voices. Schizophr Bull. 1989, 15, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Kimenyi, M.S.; Ndung’U, N.S. “Sporadic Ethnic Violence: Why Has Kenya Not Experienced a Full-blown Civil War?”. In Understanding Civil War (Volume 1: Africa); Collier, P., Sambanis, N., Eds.; World Bank: Washington, DC, USA, 2005. [Google Scholar]
- Johnson, K.; Scott, J.; Sasyniuk, T.; Ndetei, D.; Kisielewski, M.; Rouhani, S.; Bartels, S.; Mutiso, V.; Mbwayo, A.; Rae, D.; et al. A national population-based assessment of 2007–2008 election-related violence in Kenya. Conflict Health 2014, 8. [Google Scholar] [CrossRef]
- Kenya Open Data Poverty Rate, by District, Based on District Poverty Data. Available online: https://opendata.go.ke/Poverty/Poverty-Rate-by-District/i5bp-z9aq (accessed on 12 May 2015).
- Arseneault, L.; Cannon, M.; Fisher, H.L.; Polanczyk, G.; Moffitt, T.E.; Caspi, A. Childhood trauma and children’s emerging psychotic symptoms: A genetically sensitive longitudinal cohort study. Amer. J. Psychiat. 2010, 168, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Burns, J.K.; Jhazbhay, K.; Esterhuizen, T.; Emsley, R. Exposure to trauma and the clinical presentation of first-episode psychosis in South Africa. J. Psychiatr Res. 2010, 45, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Fisher, H.; Morgan, C.; Dazzan, P.; Craig, T.K.; Morgan, K.; Hutchinson, G.; Jones, P.B.; Doody, G.A.; Pariante, C.; McGuffin, P. Gender differences in the association between childhood abuse and psychosis. Brit. J. Psychiat. 2009, 194. [Google Scholar] [CrossRef] [PubMed]
- Kenya National Bureau of Statistics. Kenya AIDS Indicator Survey 2012. Available online: http://statistics.knbs.or.ke/nada/index.php/catalog/82 (accessed on 14 May 2015).
- Philips, D.L.; Segal, B.E. Sexual status and psychiatric symptoms. Am. Sociol. Rev. 1969, 34, 58–72. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, A. The pathways into psychiatric treatment: Some differences between men and women. J. Health Soc. Behav. 1977, 18, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Clancey, K.; Gove, W. Sex differences in respondents reports of psychiatric symptoms: An analysis of response bias. Am. Sociol. Rev. 1974, 80, 205–216. [Google Scholar] [CrossRef]
- Myers, N.L. Update: Schizophrenia across cultures. Curr. Psychiatr. Rep. 2011. [Google Scholar] [CrossRef]
- Al-Issa, I. The illusion of reality or the reality of illusion. Hallucinations and culture. Brit. J. Psychiat. 1995, 166, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Bourque, F.; van der Ven, E.; Malla, A. A meta-analysis of the risk for psychotic disorders among first-and second-generation immigrants. Psychol. Med. 2011, 41, 897–910. [Google Scholar] [CrossRef] [PubMed]
- Okoth, D. Luo Animistic Beliefs and Religious Practices and How to Reconcile Them to Christ. Available online: http://www.missiology.org/old/folkreligion/articleokoth.htm (accessed on 15 May 2015).
- Larøi1, F.; Luhrmann, T.M.; Bell, V.; Christian, W.A.; Deshpande, S.; Fernyhough, C.; Jenkins, J.; Woods, A. Culture and hallucinations: Overview and future directions. Schizophr. Bull. 2014, 40, S213–S220. [Google Scholar] [CrossRef] [PubMed]
- Kendall, R.E.; Chalmers, J.C.; Platz, C. Epidemiology of puerperal psychosis. Brit. J. Psychiat. 1987, 150, 662–673. [Google Scholar] [CrossRef] [PubMed]
- Index Mundi: Kenya Birth Rate. Available online: http://www.indexmundi.com/facts/kenya/birth-rate (accessed on 15 May 2015).
- Jenkins, R.; Othieno, C.; Okeyo, S.; Kaseje, D.; Aruwa, J.; Oyugi, H.; Bassett, P. Short structured general mental health in service training programme in Kenya improves patient health and social outcomes but not detection of mental health problems—A pragmatic cluster randomised controlled trial. Int. J. Mental Health Syst. 2013, 7. [Google Scholar] [CrossRef]
- Jenkins, R.; Kiima, D.; Okonji, M.; Njenga, F.; Kingora, J.; Lock, S. Integration of mental health into primary care and community health working in Kenya: Context, rationale, coverage and sustainability. Ment. Health Fam. Med. 2012, 7, 37–47. [Google Scholar]
- Kiima, D.; Jenkins, R. Short report mental health policy in Kenya—An integrated approach to scaling up equitable care for poor populations. Int. J. Ment. Health Syst. 2010, 4, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, R.; Kiima, D.; Njenga, F.; Okonji, M.; Kingora, J.; Kathuku, D.; Lock, S. Integration of mental health into primary care in Kenya. World Psychiatr. 2010, 9, 118–120. [Google Scholar]
- Wing, J.K.; Babor, T.; Brugha, T.; Burke, J.; Cooper, J.E.; Giel, R.; Jablenski, A.; Regier, D.; Sartorius, N. SCAN: Schedules for clinical assessment in neuropsychiatry. Arch. Gen. Psychiatr. 1990, 47, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Myers, N.L. Update: Schizophrenia across cultures. Curr. Psychiatry Rep. 2011. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jenkins, R.; Othieno, C.; Ongeri, L.; Ogutu, B.; Sifuna, P.; Kingora, J.; Kiima, D.; Ongecha, M.; Omollo, R. Adult Psychotic Symptoms, Their Associated Risk Factors and Changes in Prevalence in Men and Women Over a Decade in a Poor Rural District of Kenya. Int. J. Environ. Res. Public Health 2015, 12, 5310-5328. https://doi.org/10.3390/ijerph120505310
Jenkins R, Othieno C, Ongeri L, Ogutu B, Sifuna P, Kingora J, Kiima D, Ongecha M, Omollo R. Adult Psychotic Symptoms, Their Associated Risk Factors and Changes in Prevalence in Men and Women Over a Decade in a Poor Rural District of Kenya. International Journal of Environmental Research and Public Health. 2015; 12(5):5310-5328. https://doi.org/10.3390/ijerph120505310
Chicago/Turabian StyleJenkins, Rachel, Caleb Othieno, Linnet Ongeri, Bernards Ogutu, Peter Sifuna, James Kingora, David Kiima, Michael Ongecha, and Raymond Omollo. 2015. "Adult Psychotic Symptoms, Their Associated Risk Factors and Changes in Prevalence in Men and Women Over a Decade in a Poor Rural District of Kenya" International Journal of Environmental Research and Public Health 12, no. 5: 5310-5328. https://doi.org/10.3390/ijerph120505310
APA StyleJenkins, R., Othieno, C., Ongeri, L., Ogutu, B., Sifuna, P., Kingora, J., Kiima, D., Ongecha, M., & Omollo, R. (2015). Adult Psychotic Symptoms, Their Associated Risk Factors and Changes in Prevalence in Men and Women Over a Decade in a Poor Rural District of Kenya. International Journal of Environmental Research and Public Health, 12(5), 5310-5328. https://doi.org/10.3390/ijerph120505310





