Significantly more community-dwellers consumed alcoholic beverages than the institutionalized elders (13.8% vs. 37.8%, p = 0.014). The only beverage consumed was wine and the mean 24-h consumption was not different between institutionalized and community-dwelling elderly people who commonly consumed alcoholic beverages.
The “Pain Score” showed a Cronbach’s Alpha of 0.66. The following five items composed this factor: (a) “Do you have difficulty moving your shoulders, arms or hands?”; (b) “In the past 2 weeks, did pain interfere with your daily activities?”; (c) “In the past 2 weeks, did you have problems with pain of any kind?”; (d) “In the past 2 weeks, did you drop something?”; and (e) “How many times have you had a headache in the past week?”.
Regarding the “Hydration Score”, it was composed by five items, all of them being potential indicators of a good hydration status: (a) “Do you ever feel thirsty?”; (b) “Did you feel thirsty yesterday?”; (c) “Do you like to drink water?”; (d) “If you have several beverages available, do you usually choose water?”; and (e) “Are you concerned about being well hydrated?”. This factor also showed a good reliability, since it showed a Cronbach’s Alpha of 0.58. One item was excluded from both scores (“Do you usually drink at meals?”) since it showed a loading below 0.4 for the two factors.
3.1. “Pain Score”, “Hydration Score” and Urinary Parameters
The mean total values of each factor (“Hydration Score” and “Pain Score”) are shown in
Table 4. Results showed significant differences between institutionalized and community-dwelling elderly, with institutionalized subjects showing higher scores. The older group (≥80 years) also showed higher “Hydration Score” and “Pain Score” than the younger group. Women showed significantly higher “Pain Score” than men (2
vs. 1,
p < 0.001), but there were no significant differences between sexes in what concerns to “Hydration Score”. “Hydration Score” and “Pain Score” were not significantly different between groups with different education levels and BMI.
The associations between urinary parameters and both the “Pain Score” and the “Hydration Score” are shown in
Table 5. Results are presented in institutionalized and community-dwelling elderly, considering that significant differences were found in urinary parameters between these groups.
In the total sample, none of the urinary parameters was significantly associated with “Pain Score” or “Hydration Score”. In the institutionalized elderly group, 24-h urine volume was significantly and positively associated with “Pain Score” (r2 = 0.17, p = 0.026), while 24-h UOSM was significantly and negatively associated with “Pain Score” (r2 = 0.25, p = 0.006). FWR was also positively associated with “Pain Score” in institutionalized elderly people (r2 = 0.32, p = 0.002). When adjusted for age and gender (Model 2), the associations remained significant for 24-h urine volume (r2 = 0.24, p = 0.011) and FWR (r2 = 0.46, p = 0.012), and lost the significance in what concerns to 24-h UOSM (r2 = 0.46, p = 0.051).
Table 4.
“Hydration Score” and “Pain Score” according to socio-demographic variables.
Table 4.
“Hydration Score” and “Pain Score” according to socio-demographic variables.
| Socio-Demographic Variables | n | Hydration Score | p-value * | Pain Score | p-value * |
|---|
| Settings | | | | | |
| Institutionalized | 29 | 3 (0, 5) | 0.013 | 3 (0, 5) | 0.003 |
| Community-dwelling | 74 | 2 (0, 5) | 1 (0, 5) |
| Age | | | | | |
| 60–79 years | 75 | 2 (0, 5) | 0.010 | 1 (0, 5) | 0.016 |
| ≥ 80 years | 28 | 3 (0, 5) | 3 (0, 5) |
| Sex | | | | | |
| Male | 41 | 2 (0, 5) | 0.989 | 1 (0, 4) | <0.001 |
| Female | 62 | 2 (0, 5) | 2 (0, 5) |
| Education level | | | | | |
| No schooling | 28 | 3 (0, 5) | 0.115 | 2 (0, 5) | 0.145 |
| At least primary level | 75 | 2 (0, 5) | 1 (0, 5) |
| BMI | | | | | |
| ≤27.0 kg/m2 | 52 | 2 (0, 5) | 0.793 | 1 (0, 5) | 0.774 |
| >27.0 kg/m2 | 51 | 2 (0, 5) | 1 (0, 5) |
Table 5.
Relation of “Pain Score” and “Hydration Score” with urinary parameters.
Table 5.
Relation of “Pain Score” and “Hydration Score” with urinary parameters.
| 24-h Urine Volume (mL) |
| Total Sample (n = 103) | Institutionalized (n = 29) | Community-Dwelling (n = 74) |
| B (95% CI) | p value | B (95% CI) | p value | B (95% CI) | p value |
| Model 1 * | | | | | | |
| Pain Score | −5.0 (−88.1, 78.2) | 0.906 | 124.0 (15.7, 232.3) | 0.026 | −32.7 (−146.7, 81.2) | 0.569 |
| Hydration Score | 61.9 (−39.1, 162.8) | 0.227 | 69.4 (−60.3, 199.1) | 0.282 | 123.8 (−20.9, 268.4) | 0.092 |
| Model 2 † | | | | | | |
| Pain Score | 25.1 (−65.9, 116.1) | 0.060 | 155.6 (39.6, 271.6) | 0.011 | −11.4 (−138.4, 115.6) | 0.858 |
| Hydration Score | 69.5 (−31.5, −170.5) | 0.135 | 75.9 (−62.5, 214.2) | 0.270 | 119.8 (−26.7, 266.3) | 0.107 |
| 24-h Urine Osmolality (mOsm/kg) |
| Total Sample (n = 103) | Institutionalized (n = 29) | Community-dwelling (n = 74) |
| B (95% CI) | p value | B (95% CI) | p value | B (95% CI) | p value |
| Model 1 * | | | | | | |
| Pain Score | −13.0 (−33.4, 7.4) | 0.208 | −45.9 (−77.2, −14.6) | 0.006 | −6.0 (−32.8, 20.8) | 0.658 |
| Hydration Score | −19.3 (−44.1, 5.5) | 0.126 | −15.4 (−55.3, 24.4) | 0.435 | −37.4 (−70.9, −3.8) | 0.029 |
| Model 2 † | | | | | | |
| Pain Score | −1.1 (−22.9, 20.7) | 0.921 | −29.6 (−59.4, 0.1) | 0.051 | 1.3 (−27.2, 29.7) | 0.929 |
| Hydration Score | −19.6 (−43.7, 4.5) | 0.109 | −10.3 (−44.5, 23.8) | 0.539 | −40.9 (−72.9, −9.0) | 0.013 |
| Free Water Reserve (mL/24-h) |
| Total Sample (n = 103) | Institutionalized (n = 29) | Community-dwelling (n = 74) |
| B (95% CI) | p value | B (95% CI) | p value | B (95% CI) | p value |
| Model 1 * | | | | | | |
| Pain Score | 17.4 (−62.8, 97.7) | 0.668 | 144.6 (60.4, 228.8) | 0.002 | 11.2 (−98.0, 120.5) | 0.838 |
| Hydration Score | 67.0 (−30.3, 164.4) | 0.175 | 72.2 (−37.7, 182.0) | 0.189 | 154.7 (18.3, 291.1) | 0.027 |
| Model 2 † | | | | | | |
| Pain Score | 7.5 (−79.0, 93.9) | 0.864 | 110.1 (26.6, 193.6) | 0.012 | −1.3 (−122.9, 120.3) | 0.983 |
| Hydration Score | 79.6 (−15.8, 175.0) | 0.101 | 45.8 (−54.1, 145.7) | 0.354 | 160.8 (23.1, 298.4) | 0.023 |
In community-dwelling subjects, none of the urinary indicators of hydration status was significantly associated with the “Pain Score”. However, in this group, 24-h UOSM was significantly associated with the “Hydration Score”, both in the unadjusted (r2 = 0.06, p = 0.029) and in the adjusted model (r2 = 0.18, p = 0.013). The 24-h urine volume did not show significant association with “Hydration Score” (p = 0.107) among community-dwelling elderly people, but FWR was positively associated with “Hydration Score” both in the unadjusted (r2 = 0.07, p = 0.027) and in the adjusted (r2 = 0.08, p = 0.023) models.
Table 6 shows that only six institutionalized and six community-dwelling elderly subjects were hypohydrated and that there were no significant differences in “Pain Score” and “Hydration Score” between euhydrated and hypohydrated subjects. However, among institutionalized subjects, those with “Pain Score” <4 showed a significantly lower FWR, when compared with those with “Pain Score” ≥4 (244.2 ± 358.1
vs. 765.6 ± 343.8 mL/24-h,
p = 0.002). Moreover, community-dwelling subjects with “Hydration Score” <3 showed a significantly lower FWR when compared with those with “Hydration Score ≥ 3 (1004.9 ± 604.4
vs. 673.9 ± 613.6,
p = 0.031).
Table 6.
“Pain Score” and “Hydration Score” in euhydrated and hypohydrated elderly people.
Table 6.
“Pain Score” and “Hydration Score” in euhydrated and hypohydrated elderly people.
| Scores | Euhydrated | Hypohydrated | p-value |
|---|
| Total Sample, n | 91 | 12 | -- |
| Pain Score | 1 (0, 5) | 1 (0,3) | 0.280 † |
| Hydration Score | 2 (0, 5) | 2 (0, 5) | 0.290 † |
| Institutionalized, n | 23 | 6 | -- |
| Pain Score | 3 (0, 5) | 1.5 (0, 3) | 0.065 * |
| Hydration Score | 3 (0, 5) | 2.5 (0, 5) | 0.670 * |
| Community-dwelling, n | 68 | 6 | -- |
| Pain Score | 1 (0, 5) | 1 (0, 3) | 0.623 † |
| Hydration Score | 2 (0, 5) | 1.5 (1, 2) | 0.065 † |
3.2. Discussion
The main achievement of this study was the contribution to the development of a new DST that could be used in the identification of elders at greater risk of dehydration both in institutionalized and in community-dwelling populations. Two factors emerged in the validation analysis, which were called “Hydration Score”, consisting of five questions about thirst sensation and preferences related to fluid consumption, and “Pain Score”, consisting of five items about mobility and pain. These 10 questions were considered in the new DST. Although Cronbach’s alpha should be higher than 0.70, considering the relatively small number of items in each subscale and the sample size, the reliability of both scores was considered to be acceptable because, according to Kehoe (1995) [
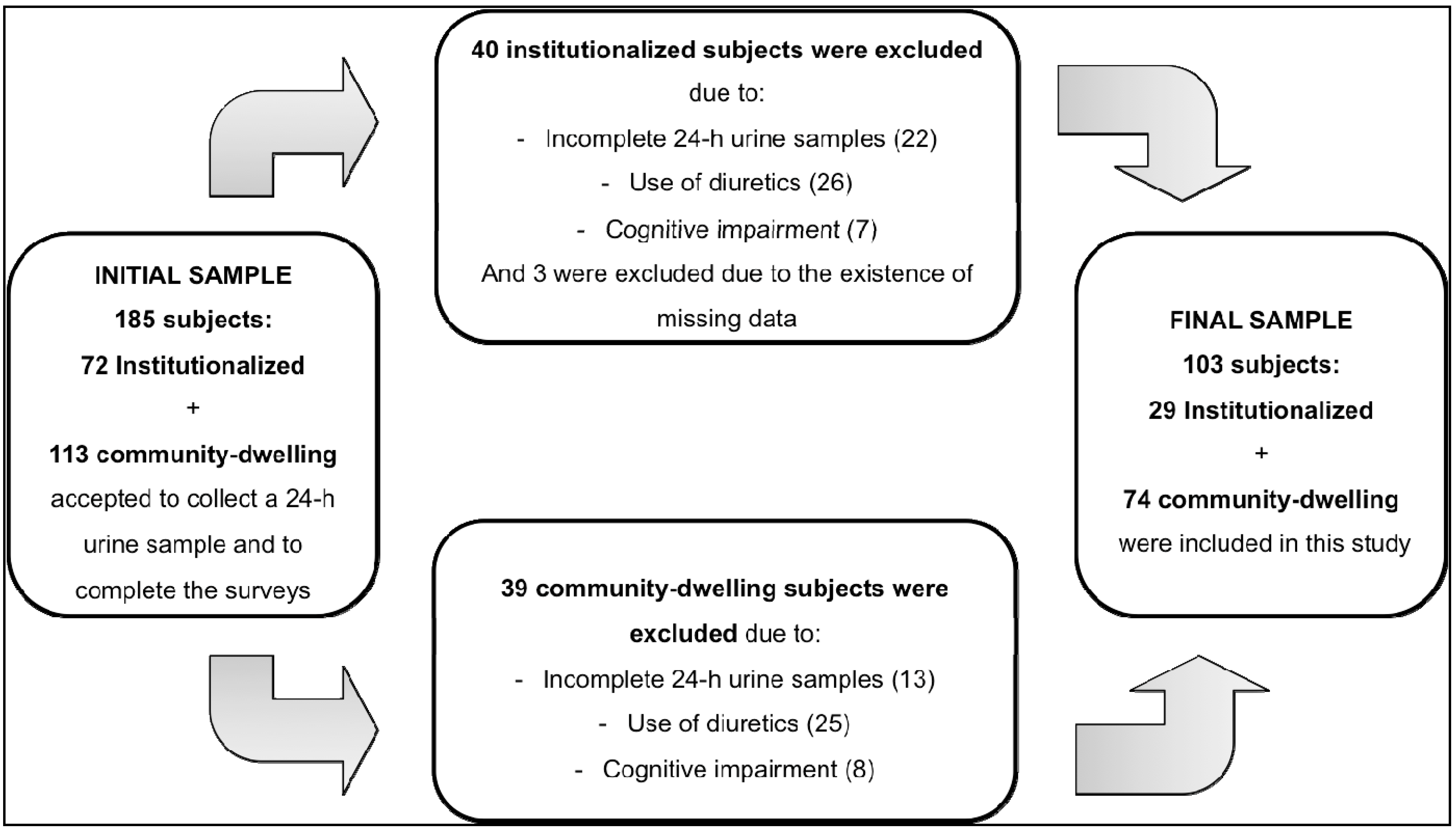
27], reliabilities of 0.5 are satisfactory for short dichotomous scales. The reliability and validity were tested in the overall sample and not among subpopulations since our main objective was to create and test a tool able to measure hydration status in elderly individuals regardless their age, other socio-demographic characteristics or living conditions. In our view, the dehydration construct does not vary between elderly groups, while the intensity of the dehydration is expected to be different among subgroups. Therefore we opted to include a relatively heterogeneous sample of 103 elderly individuals, aged 60–94 years, with approximately one third institutionalized. However, the resulting constructs did not show association with urinary parameters in the total sample. Considering the existence of two different sub-populations, analysis was performed to ascertain the existence of associations in each sub-sample, adjusting for age and gender to eliminate the possible confound effect of these variables.
The two resulting scores showed different associations with urinary parameters in both elderly populations. The “Hydration Score” did not show any association with urinary parameters in institutionalized elderly people, while in the community-dwellers, it showed a negative association with the 24-h urine osmolality (18% of the variance being explained by the adjusted model) and a positive weak association with FWR (the adjusted model explained only 8% of the variance), which suggests that “Hydration Score” may have an association with hydration status in community-dwellers, but not in institutionalized elderly people. The questions composing this score are mainly related to water intake and do not consider the consumption of other beverages, particularly the alcoholic beverages, which were consumed by 37.8% of community-dwellers (significantly more than in institutionalized elderly people). Despite alcohol consumption might be underestimated by dietary recall, these differences are considerable because drinks containing higher amounts of alcohol contribute less to improve hydration status [
19], but their consumption increases diuresis [
20], and this may be on the basis of the lack of association between the “Hydration Score” and the 24-h urine volume in community-dwellers. Moreover, considering that institutionalized elders are significantly older, the first two items about thirst composing the “Hydration Score” may contribute for the difference between community-dwelling and institutionalized elderly people. Thirst sensation had previously shown to be a bad predictor of hydration status among elderly people [
15,
28,
29], due to the recognized decline in thirst sensation with aging [
28,
30,
31,
32]. In addition, the items “Do you ever feel thirsty?” and “Did you feel thirsty yesterday?” can be interpreted in two different forms: on one hand, elderly individuals who respond “yes” to those questions may drink more to compensate thirst sensation and consequently be better hydrated or, on the other hand, they can feel thirsty due to a poorer hydration status. It is difficult to establish a direct relationship between thirst and hydration status [
33]. These results suggest that “Hydration Score” may be useful in the assessment of hydration status in community-dwelling, but not in institutionalized elderly people.
The “Pain Score” showed an association with hydration status in institutionalized elderly people,
i.e., individuals with a higher “Pain Score” (reflecting more difficulties with pain and mobility) were more likely to show a better hydration status, characterized by a higher 24-h urine volume, a lower 24-h urine osmolality and a higher FWR. These associations were independent of age and sex, except in what concerns to the 24-h urine osmolality, which lost the statistical significance in the adjusted model (
p = 0.051). In addition to age and gender, Vivanti (2007) [
15] had described that body mass index might confound the hydration status. Other authors have argued that hydration needs for elderly people should take in account their body weight [
34]. However, in this study, despite BMI was initially considered to be a confounding variable, this adjustment was disregarded because there were no significant differences in urinary parameters between individuals with different BMI’s. The adjusted model of “Pain Score” explained 46% of the variance of FWR, and 24% of the variance of 24-h urine volume in institutionalized elderly individuals.
Our results regarding “Pain Score” are in agreement with the findings of Vivanti (2007) [
15], who found that the individuals clinically assessed as dehydrated indicated no headaches during the previous week, fewer problems with pain of any kind in the past two weeks and less often reported pain interfering with daily activities. However, there are no other evidences supporting this relationship and the mechanisms behind them remain unknown. These findings are controversial because other authors have previously described that mobility impairment was associated with lower fluid intakes [
35,
36,
37,
38], but two studies found that nursing home residents with better physical function were at greater risk of dehydration [
39,
40]. According to Mentes (2006) [
41], they “may reflect environmental factors in nursing homes, where caregivers may be more attuned to highly dependent residents who cannot drink independently, leaving those who are able to care for themselves to do so. Such an approach may not work with residents who are physically functional but cognitively impaired.” The association in this study between pain absence and a poor hydration status should be explored, since it could be used in the development of a practical and easy tool to detect institutionalized elders at greater risk and early prevent dehydration.
Nevertheless, the “Pain Score” did not show any association with urinary parameters in the community-dwelling elderly people. This can be explained by the fact that this population, namely the ones enrolled in PA programs, commonly shows fewer problems with pain and mobility than either those institutionalized (in the present study) or hospitalized (in the study by Vivanti [
15]). Pain and mobility impairments have been identified as predictor factors for institutionalization [
42,
43]. According to this, an explanation for the difference in the findings between institutionalized and community-dwelling elderly people may be related to physical activity and this should be explored in next studies.
Overall, the previously described factors, such as advanced age, the low education level, the high number of prescription drugs and others, have been considered to be predictive factors for institutionalization [
42] and they can also be putative contributors for the higher risk of dehydration in institutionalized individuals. The results of the present study regarding urinary parameters confirmed that community-dwelling elderly men were better hydrated than the institutionalized men, according the higher 24-h urine volumes, lower 24-h urine osmolality and higher FWR in the community-dwellers. These results are supported by the findings of Leiper
et al. (2005) [
36] who found higher 24-h urine volumes in community-dwellers when compared to institutionalized elderly people. In the study by Leiper and colleagues [
36], community-dwellers showed an average 24-h urine volume of 1.7 L and institutionalized elderly people showed mean values of 0.9 to 1.1 L, while in this study the community-dwellers had mean 24-h urine volumes of 1.8 to 2.0 L and the institutionalized individuals of 1.6 L. Other studies have shown high prevalences of inadequate fluid intake [
34,
38,
44,
45] and consequently of dehydration among institutionalized elderly people [
46,
47].
To characterize the hydration status, we used the concept of FWR [
9] calculated from the 24-h urine osmolality, which is considered an appropriate marker of hydration status [
25], and no significant differences in scores (Pain Score and Hydration Score) were found when comparing hypohydrated and euhydrated subjects. Based in this result, the scores seem to be associated with different levels of euhydration, but do not allow the identification of hypohydrated older people. In an attempt to develop a useful tool for hydration assessment in older people, future studies should include other questions, such as more specific questions about drinking habits, and other physical signs, such as axillary moisture, which has been recently described to be a good marker of hydration status [
48,
49]. Moreover, next studies should also involve larger samples, particularly including a larger number of subjects in a hypohydrated state.
Almost all of the items from the DST used in the present study were based on previous work developed by Vivanti
et al. (2010) [
5]. The authors applied this instrument in older people admitted in rehabilitative care units of metropolitan hospitals and found that tongue dryness was the parameter that showed the better combination of sensibility and specificity for dehydration detection. They concluded that the assessment of tongue dryness was a simple and quick method, which could be used in individuals with minimal cognitive and physical capacity. However, in the present study our results led to the exclusion of tongue dryness and other three physical signs (postural hypotension, reduced skin turgor, and low body weight). Other authors had previously concluded that physical signs are not useful in the assessment of dehydration in the elderly [
31,
48,
50,
51] because they are generally associated with common physiologic age-related changes or with conditions that are more prevalent in elderly individuals, such as polymedication or chronic diseases. Moreover, physical signs of dehydration may be absent or misleading in older people [
50]. Recent evidence has supported the use of axillary moisture as a physical sign that is easy to assess hydration status in older people admitted to hospitals [
48,
49]. However, the validation of its use in community-dwellers and institutionalized elderly people is lacking. The majority of the previous studies regarding physical signs that showed positive outcomes were performed in clinical settings, where the degree of dehydration is expected to be more accentuated. In non-clinical settings, severe dehydration should be prevented and early stages of mild dehydration should be detected. In these stages, physical signs of dehydration may be absent.