Factors Associated with No Dental Treatment in Preschoolers with Toothache: A Cross-Sectional Study in Outpatient Public Emergency Services
Abstract
:1. Introduction
2. Methods
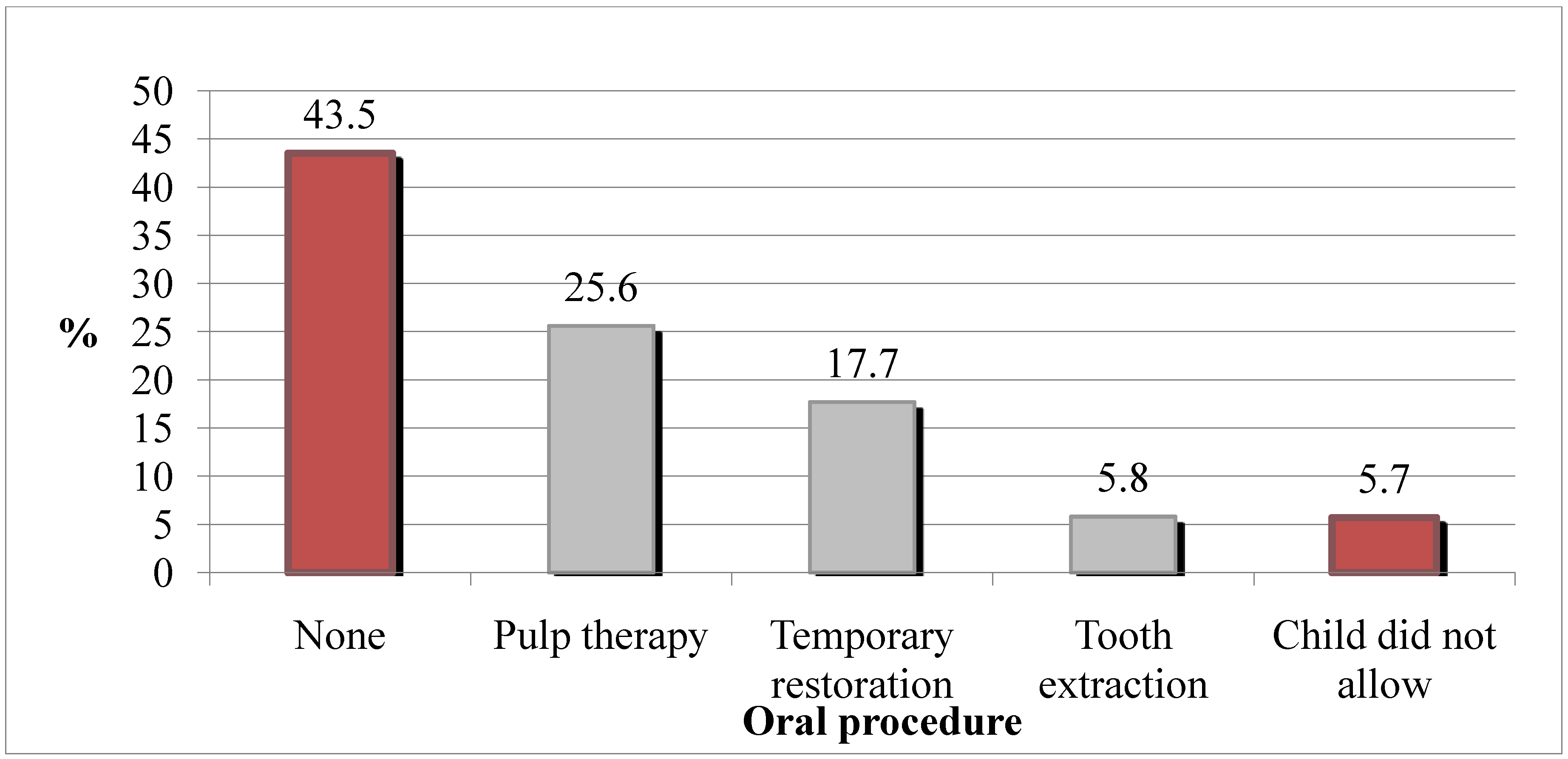
3. Results
| Prescription of Medication | Oral Procedure, n(%) | Total | |
|---|---|---|---|
| No | Yes | ||
| No | 96 (31.3%) | 211 (68.7%) | 307 (100%) |
| Yes | 161 (74.8%) | 54 (25.2%) | 215 (100%) |
| Total | 257 | 265 | 522 * |
| Independents Variables | Was There an Oral Procedure? n (% ) | p-value | |
|---|---|---|---|
| No | Yes | ||
| Age (categories) | 0.023 * | ||
| 1 to 2 years | 22 (8.6%) | 10 (3.8%) | |
| 3 to 5 years | 235 (91.4%) | 255 (96.2%) | |
| Sex | 0.140 * | ||
| Female | 125 (48.6%) | 146 (55.1%) | |
| Male | 132 (51.4%) | 119 (44.9%) | |
| Radiography requested | 40 (15.7%) | 11 (4.2%) | <0.001 * |
| Medication prescribed | 161 (63.4%) | 54 (20.5%) | <0.001 * |
| Patient referred to another service | 57 (22.4%) | 16 (6.1%) | <0.001 * |
| Variable | Odds Ratio | 95% Confidence Interval for Odds Ratio | p-value | |
|---|---|---|---|---|
| Minimum | Maximum | |||
| Male sex | 0.7 | 0.5 | 1.1 | 0.087 |
| Age (years, continuous variable) | 0.7 | 0.5 | 0.8 | <0.001 |
| Radiography requested | 3.8 | 1.7 | 8.2 | 0.001 |
| Medication prescribed | 7.5 | 4.9 | 11.5 | <0.001 |
| Patient referred to another service | 5.7 | 3.0 | 0.9 | <0.001 |
4. Discussion
5. Conclusions
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Sakai, V.T.; Magalhães, A.C.; Pessan, J.P.; Silva, S.M.B.; Machado, M.A.A.M. Urgency treatment profile of 0 to 15 year-old children assisted at urgency dental service from Bauru Dental School, University of São Paulo. J. Appl. Oral Sci. 2005, 13, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Davis, E.E.; Amos, S.D.; Eugenie, W.H.M. Doctor, my tooth hurts: The costs of incomplete dental care in the emergency room. J. Public Health Dent. 2010, 70, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, N.; Carnut, L.; Goes, P.S.A. Evaluation of out-of-hours dental service, Recife, Brazil. Int. J. Dent. 2010, 9, 114–119. [Google Scholar]
- Riggs, E.; Gussy, M.; Gibbs, L.; van Gemert, C.; Waters, E.; Kilpatrick, N. Hard to reach communities or hard to access services? Migrant mothers’ experiences of dental services. Aust. Dent. J. 2014, 59, 201–207. [Google Scholar] [CrossRef] [PubMed]
- Agostini, F.G.; Flaitz, C.M.; Hicks, M.J. Dental emergencies in a university based pediatric dentistry postgraduate outpatient clinic: A retrospective study. J. Dent. Child. 2001, 68, 316–321. [Google Scholar]
- Easton, J.A.; Landgraf, J.M.; Casamassimo, P.S.; Wilson, S.; Ganzberg, S. Evaluation of a generic quality of life instrument for early childhood caries-related pain. Community Dent. Oral Epidemiol. 2008, 36, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Lewis, C.; Stout, J. Toothache in U.S. children. Arch. Pediatr. Adolesc. Med. 2010, 164, 1059–1063. [Google Scholar]
- Shqair, A.; Gomes, G.B.; Oliveira, A.; Goettems, M.L.; Romano, A.R.; Schardozim, L.R.; Bonow, M.L.M.; Torriani, D.D. Dental emergencies in a university pediatric dentistry clinic: A retrospective study. Braz. Oral Res. 2012, 26, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Hocker, M.B.; Villani, J.J.; Borawski, J.B.; Evans, C.S.; Nelson, S.M.; Gerardo, C.J.; Limkakeng, A.T. Dental visits to a north Carolina emergency department: A painful problem. N. C. Med. J. 2012, 73, 346–351. [Google Scholar] [PubMed]
- Thikkurissy, S.; Allen, P.H.; Smiley, M.K.; Casamassimo, P.S. Waiting for the pain to get worse: Characteristics of a pediatric population with acute dental pain. Pediatr. Dent. 2012, 34, 289–294. [Google Scholar] [PubMed]
- Cachovan, G.; Phark, J.H.; Schön, G.; Pohlenz, P.; Platzer, U. Odontogenic infections: An 8-year epidemiologic analysis in a dental emergency outpatient care unit. Acta Odontol. Scand. 2013, 71, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Curzon, M.E.J.; Pollard, M.A. Do we still care about children’s teeth? Brit. Dent. J. 1997, 182, 242–244. [Google Scholar] [CrossRef]
- Ferreira, S.H.; Béria, J.U.; Kramer, P.F.; Feldens, E.G.; Feldens, C.A. Dental caries in 0- to 5-years-old Brazilian children: Prevalence, severity, and associated factors. Int. J. Paediatr. Dent. 2007, 17, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, M.A.; Nadanovsky, P.; Sheiham, A. The prevalence and impact of dental pain in 8-years-old school children in Harrow, England. Brit. Dent. J. 1999, 187, 38–41. [Google Scholar] [PubMed]
- Moura-Leite, F.R.; Ramos-Jorge, M.L.; Bonanato, K.; Paiva, S.M.; Vale, M.P.; Pordeus, I.A. Prevalence, intensity and impact of dental pain in 5-years-old preschool children. Oral Health Prev. Dent. 2008, 6, 295–301. [Google Scholar] [PubMed]
- Tulip, D.E.; Palmer, N.O. A retrospective investigation of the clinical management of patients attending an out of hours dental clinic in Merseyside under the new NHS dental contract. Brit. Dent. J. 2008, 205, 659–664. [Google Scholar] [CrossRef] [PubMed]
- Balasubramaniam, R.; Turner, L.N; Fischer, D.; Klasser, G.D.; Okeson, J.P. Non-odontogenic toothache revisited. Open J. Stomatol. 2011, 1, 92–102. [Google Scholar] [CrossRef]
- Oguntebi, B.R.; DeSchepper, E.J.; Taylor, T.S.; White, C.L.; Pink, F.E. Postoperative pain incidence related to the type of emergency treatment of symptomatic pulpitis. Oral Surg. Oral Med. Oral Pathol. 1992, 73, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Pourat, N.; Nicholson, G. Unaffordable Dental Care is Linked to Frequent School Absences; Center for Health Policy Research: LosAngeles, CA, USA, 2009. [Google Scholar]
- Alkarimi, H.A.; Watt, R.G.; Pikhart, H.; Jawadi, A.H.; Sheiham, A.; Tsakos, G. Impact of treating dental caries on school children’s anthropometric, dental, satisfaction and appetite outcomes: A randomized controlled trial. BMC Public Health 2012, 12, 706–719. [Google Scholar] [CrossRef] [PubMed]
- McGrath, C.; Bedi, R. A national study of the importance of oral health to life quality to inform scales of oral health related quality of life. Qual. Life Res. 2004, 13, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Cohen, L.A.; Harris, S.L.; Bonito, A.J.; Manski, R.J.; Macek, M.D.; Edwards, R.R.; Cornelius, L.J. Coping with toothache pain: A qualitative study of low-income persons and minorities. AAPHD 2007, 67, 28–35. [Google Scholar]
- Milsom, K.M.; Tickle, M.; Blinkhorn, A.S. Dental pain and dental treatment of young children attending the general dental service. Brit. Dent. J. 2002, 192, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Blinkhorn, A.; Zadeh-Kabir, R. Dental care of a child in pain—A comparison of treatment planning options offered by GDPs in California and the north-west of England. Int. J. Paediatr. Dent. 2003, 13, 165–171. [Google Scholar] [PubMed]
- Wong, N.H.Y.; Tran, C.; Pukallus, M.; Holcombe, T.; Seow, W.K. A three-year retrospective study of emergency visits at an oral health clinic in south-east Queensland. Aust. Dent. J. 2012, 57, 132–137. [Google Scholar] [PubMed]
- Ministry of Health of Brazil, SB Brazil 2010 Project: National Research on Oral Health. Main Results, Ministry of Health, Brasilia, Brazil, 2011. Available online: http://189.28.128.100/dab/docs/geral/projeto_sb2010_relatorio_final.pdf (accessed on 26 February 2012).
- Oral Health Surveys: Basic Methods, 4th ed.; World Health Organization: Geneva, Switzerland, 1997.
- Tickle, M.; Milsom, K.; King, D.; Kearney-Mitchell, P.; Blinkhorn, A. The fate of the carious primary teeth of children who regularly attend the general dental service. Brit. Dent. J. 2002, 192, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Levine, R.S.; Pitts, N.B.; Nugent, Z.J. The fate of 1587 unrestored carious deciduous teeth: A retrospective general dental practice based study from northern England. Brit. Dent. J. 2002, 193, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Lewis, M.A.O. Why we must reduce dental prescription of antibiotics: European Union Antibiotic Awareness Day. Br. Dent. J. 2008, 205, 537–538. [Google Scholar] [CrossRef] [PubMed]
- Sheiham, A. Dental caries affects body weight, growth and quality of life in pre-school children. Brit. Dent. J. 2006, 201, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Pine, C.M.; Harris, R.V.; Burnside, G.; Merrett, M.C.W. An investigation of the relationship between untreated decayed teeth and dental sepsis in 5-year-old children. Brit. Dent. J. 2006, 200, 45–47. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.C.B.; Silva, R.A.; Ribeiro, C.C.C.; Cruz, M.C.F.N. Profile of public dental care for children and adolescents in São Luís, Maranhão State. Cienc. Saúde. Colet 2007, 12, 1237–1246. [Google Scholar]
- Duggal, M. Carious primary teeth in children: Can or should they be left unrestored? Faculty Dent J. 2011, 2, 8–13. [Google Scholar]
- Cohen, L.A. The role of non-dental health professionals in providing access to dental care for low-income and minority patients. Dent. Clin. N. Amer. 2009, 53, 451–468. [Google Scholar] [CrossRef]
- Gift, H.C. Quality of life—An outcome of oral healthcare? J. Public Health Dent. 1996, 56, 67–68. [Google Scholar] [CrossRef]
- Xia, B.; Wang, C.; Ge, L. Factors associated with dental behavior management problems in children age 2–8 years in Beijing, China. Int. J. Paediatr. Dent. 2011, 21, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Okunseri, C.; Okunseri, E.; Thorpe, J.M.; Xiang, Q.; Szabo, A. Medications prescribed in emergency departments for nontraumatic dental condition visits in the United States. Med. Care 2012, 50, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Palmer, N.A.; Dailey, Y.M.; Martin, M.V. Can audit improve antibiotic prescribing in general dental practice? Brit. Dent. J. 2001, 191, 253–255. [Google Scholar]
- Dailey, Y.M.; Martin, M.V. Are antibiotics being used appropriately for emergency dental treatment? Brit. Dent. J. 2001, 191, 391–393. [Google Scholar]
- Nagle, N.D.; Reader, A.; Beck, M.; Weaver, J.; Ohio, C. Effect of systemic penicillin on pain in untreatedirreversible pulpitis. Oral Surg. Oral Med. Oral Pathol. 2000, 90, 636–640. [Google Scholar] [CrossRef]
- Fedorowicz, Z.; van Zuuren, E.J.; Farman, A.G.; Agnihotry, A.; Al-Langawi, J.H. Antibiotic use for irreversible pulpitis. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef]
- Klaassen, M.A.; Veerkamp, J.S.J.; Hoogstraten, J. Dental fear, communication, and behavioral management problems in children referred for dental problems. Int. J. Paediatr. Dent. 2007, 17, 469–477. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Machado, G.C.M.; Daher, A.; Costa, L.R. Factors Associated with No Dental Treatment in Preschoolers with Toothache: A Cross-Sectional Study in Outpatient Public Emergency Services. Int. J. Environ. Res. Public Health 2014, 11, 8058-8068. https://doi.org/10.3390/ijerph110808058
Machado GCM, Daher A, Costa LR. Factors Associated with No Dental Treatment in Preschoolers with Toothache: A Cross-Sectional Study in Outpatient Public Emergency Services. International Journal of Environmental Research and Public Health. 2014; 11(8):8058-8068. https://doi.org/10.3390/ijerph110808058
Chicago/Turabian StyleMachado, Geovanna C. M., Anelise Daher, and Luciane R. Costa. 2014. "Factors Associated with No Dental Treatment in Preschoolers with Toothache: A Cross-Sectional Study in Outpatient Public Emergency Services" International Journal of Environmental Research and Public Health 11, no. 8: 8058-8068. https://doi.org/10.3390/ijerph110808058
APA StyleMachado, G. C. M., Daher, A., & Costa, L. R. (2014). Factors Associated with No Dental Treatment in Preschoolers with Toothache: A Cross-Sectional Study in Outpatient Public Emergency Services. International Journal of Environmental Research and Public Health, 11(8), 8058-8068. https://doi.org/10.3390/ijerph110808058




