Correlates of the Intention to Implement a Tailored Physical Activity Intervention: Perceptions of Intermediaries
Abstract
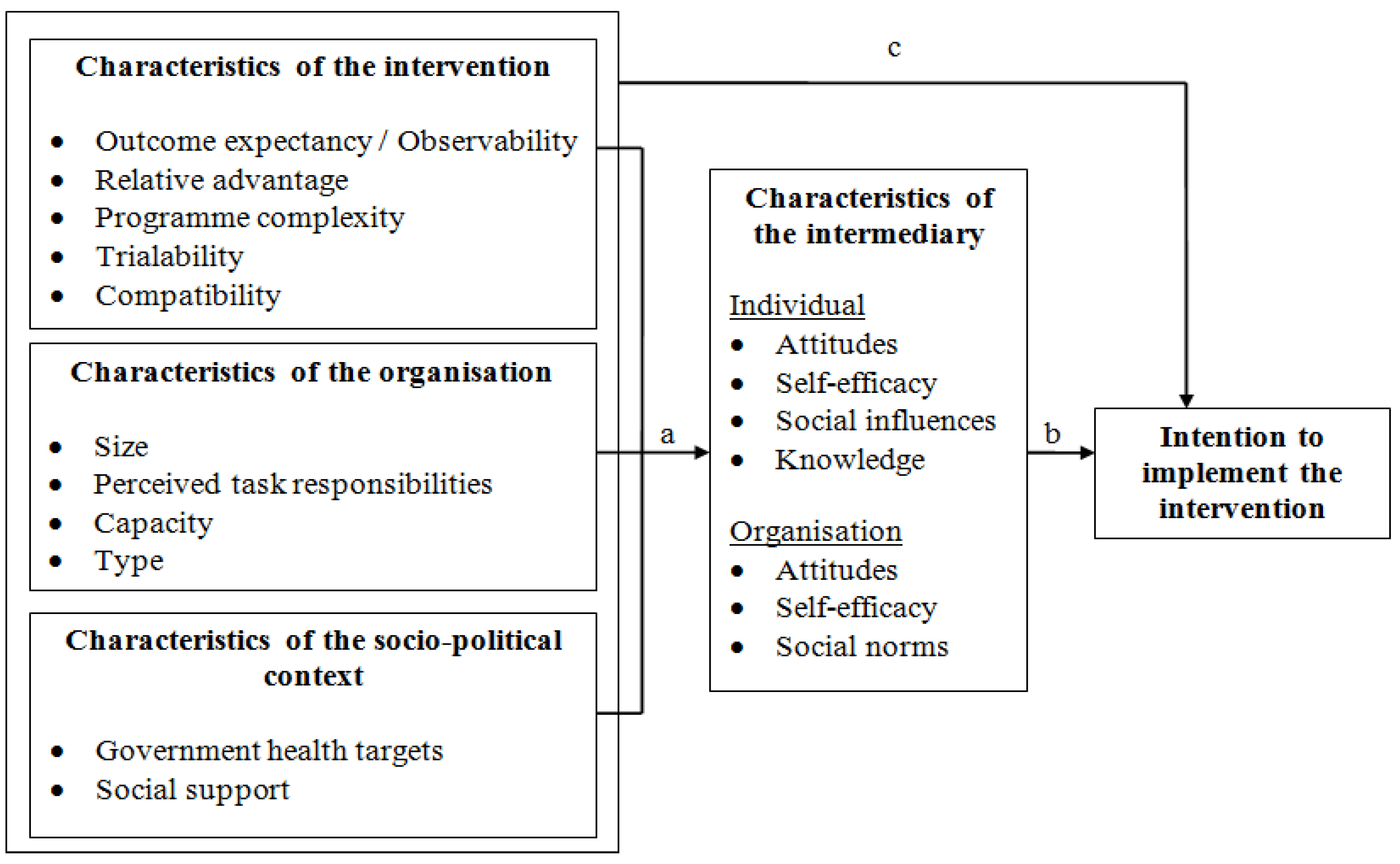
:1. Introduction
2. Methods
2.1. Study Population, Design and Procedure
2.2. Intervention
2.3. Measurement Instrument
| Concept | Items (N) | Example Question/Statement | α |
|---|---|---|---|
| Intervention characteristics | |||
| Relative advantage | 15 | Compared to other interventions, implementation costs for this intervention are low. Totally disagree (1) to Totally agree (5) | 0.67 |
| Trialability | 2 | Implementing this intervention requires large financial investments. Totally disagree (1) to Totally agree (5) | 0.70 |
| Outcome expectancy/Observability | 10 | By implementing this intervention, PA behaviour of people aged over 50 within our region will increase. Totally disagree (1) to Totally agree (5) | 0.88 |
| Programme complexity | 4 | Implementation the Active Plus intervention is uncomplicated. Totally disagree (1) to Totally agree (5) | 0.69 |
| Compatibility | 4 | The intervention corresponds with our targets. Totally disagree (1) to Totally agree (5) | 0.78 |
| Organisational characteristics | |||
| Size | 1 | How many employees has your organisation? | - |
| Perceived task responsibility | 6 | It is our organisation’s responsibility to stimulate PA among people aged over 50. Totally disagree (1) to Totally agree (5) | 0.73 |
| Capacity | 9 | Our organisation has sufficient staff capacity to implement the intervention. Totally disagree (1) to Totally agree (5) | 0.87 |
| Type | 1 | In which type of organisation are you working? Municipality/Sport-Service/MHC | - |
| Socio-political context | |||
| Governmental health targets | 2 | The Active Plus intervention corresponds to the national health targets. Totally disagree (1) to Totally agree (5) | 0.73 |
| Social support | 8 | I expect to get support for intervention implementation from (other) MHC’s. Certainly not (1) to Yes, definitely (5) | 0.76 |
| Intermediary characteristics | |||
| Individual | |||
| Attitude | 7 | The insecurities of new interventions are worrisome to me. Totally disagree (1) to Totally agree (5) | 0.71 |
| Self-efficacy | 4 | I am able to convince my colleagues of the need to implement a new intervention. Totally disagree (1) to Totally agree (5) | 0.76 |
| Social support | 1 | My colleagues will support me when I announce a new idea. Totally disagree (1) to Totally agree (5) | - |
| Intermediary characteristics | |||
| Subjective norm | 1 | My social environment welcomes innovations. Totally disagree (1) to Totally agree (5) | - |
| Knowledge | 5 | I have sufficient knowledge about the consequences of physical inactivity among persons aged over 50. Totally disagree (1) to Totally agree (5) | 0.82 |
| Organisation | |||
| Attitude | 3 | Promoting PA in persons aged over 50 within our region is important for our organisation. Totally disagree (1) to Totally agree (5) | 0.77 |
| Self-efficacy | 4 | Our organisation is able to implement this intervention. Totally disagree (1) to Totally agree (5) | 0.74 |
| Subjective norm | 7 | Welfare organisations think it is—Very unimportant (1) to Very important (5)—that our organisation implements this intervention | 0.82 |
| Intention to implement Active Plus | |||
| 2 | When the Active Plus intervention is available, I will coordinate/execute the intervention implementation within one year. Certainly not (1) to Yes, definitely (5) | 0.79 | |
2.4. Analyses
3. Results
3.1. Characteristics of the Sample
3.2. Factors Associated with the Intentions to Implement the Intervention
| Potential Determinants | Number of Observations (N) | Mean | SD | % of Respondents Having a Positive Score |
|---|---|---|---|---|
| Intervention characteristics | ||||
| Outcome expectancy/Observability | 142 | 3.45 | 0.43 | 78.8 |
| Relative advantage | 136 | 3.09 | 0.26 | 45.9 |
| Programme complexity | 137 | 3.26 | 0.54 | 44.1 |
| Trialability | 135 | 2.76 | 0.59 | 20.5 |
| Compatibility | 140 | 3.54 | 0.62 | 74.7 |
| Organisational characteristics | ||||
| Size (amount of employees) | 126 | 268.89 | 373.61 | |
| Perceived task responsibility | 145 | 3.59 | 0.53 | 84.2 |
| Capacity | 137 | 2.85 | 0.70 | 35.6 |
| Socio-political context | ||||
| Governmental health targets | 140 | 3.83 | 0.61 | 82.9 |
| Social support | 132 | 3.28 | 0.44 | 67.1 |
| Intermediary characteristics | ||||
| Individual | ||||
| Attitude | 145 | 3.71 | 0.47 | 91.1 |
| Self-efficacy | 145 | 3.49 | 0.53 | 80.1 |
| Subjective norm | 146 | 3.69 | 0.64 | 69.2 |
| Social support | 146 | 3.67 | 0.64 | 67.1 |
| Knowledge | 143 | 3.56 | 0.63 | 80.8 |
| Organisation | ||||
| Attitude | 146 | 3.84 | 0.60 | 90.4 |
| Self-efficacy | 139 | 3.22 | 0.66 | 61.0 |
| Subjective norm | 133 | 3.52 | 0.46 | 82.2 |
| Intention to implement the intervention | 139 | 2.30 | 0.92 | 8.4 |
| Potential Determinants | Intermediairy Characteristics (a-path) | Intention to Implementation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Individual | Organisational | ||||||||||
| N | Attitude (SE) | Self-efficacy (SE) | Social norm (SE) | Social support (SE) | Knowledge (SE) | Attitude (SE) | Self-efficacy (SE) | Social norm (SE) | c’-path (SE) | c-path (SE) | |
| Intervention characteristics | |||||||||||
| Observability | 100 | 0.33 (0.09) *** | 0.36 (0.11) ** | 0.31 (0.13) * | 0.42 (0.13) ** | 0.16 (0.13) | 0.32 (0.12) ** | 0.32 (0.14) * | 0.33 (0.09) *** | 0.11 (0.17) | 0.53 (0.19) ** |
| Relative advantage | 121 | 0.52 (0.17) ** | 0.54 (0.20) ** | 0.71 (0.23) ** | 0.71 (0.23) ** | 0.03 (0.24) | −0.01 (0.22) | 0.57 (0.24) * | 0.78 (0.15) *** | 0.11 (0.33) | 0.79 (0.34) * |
| Complexity | 120 | 0.18 (0.08) * | 0.24 (0.09) * | 0.21 (0.11) ‡ | 0.10 (0.11) | 0.13 (0.11) | 0.24 (0.10) * | 0.71 (0.10) *** | 0.21 (0.08) ** | 0.32 (0.16) ‡ | 0.80 (0.15) *** |
| Trialability | 120 | 0.07 (0.07) | 0.07 (0.08) | 0.14 (0.10) | −0.01 (0.10) | −0.20 (0.10) * | −0.05 (0.09) | 0.27 (0.10) ** | −0.03 (0.07) | −0.03 (0.13) | 0.06 (0.14) |
| Compatibility | 120 | 0.29 (0.06) *** | 0.20 (0.08) * | 0.18 (0.09) ‡ | 0.19 (0.09) * | 0.24 (0.09) * | 0.47 (0.08) *** | 0.39 (0.09) *** | 0.35 (0.06) *** | 0.26 (0.14) ‡ | 0.70 (0.12) *** |
| Organisational characteristics | |||||||||||
| Type | 121 | 0.09 (0.06) | 0.05 (0.07) | 0.09 (0.09) | 0.10 (0.09) | 0.26 (0.08) ** | 0.12 (0.08) | 0.09 (0.09) | 0.01 (0.06) | 0.29 (0.10) ** | 0.38 (0.12) ** |
| Size | 105 | −0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) | −0.00 (0.00) | 0.00 (0.00) | 0.00 (0.00) * | −0.00 (0.00) | −0.00 (0.00) |
| Responsibility | 121 | 0.41 (0.07) *** | 0.31 (0.09) *** | 0.18 (0.11) ‡ | 0.22 (0.11) * | 0.43 (0.10) *** | 0.50 (0.09) *** | 0.49 (0.10) *** | 0.31 (0.07) *** | 0.09 (0.16) | 0.66 (0.14) *** |
| Capacity | 121 | 0.24 (0.07) *** | 0.30 (0.08) *** | 0.23 (0.09) * | 0.25 (0.09) ** | 0.39 (0.09) *** | 0.44 (0.08) *** | 0.66 (0.08) *** | 0.25 (0.06) *** | 0.38 (0.16) * | 0.83 (0.11) *** |
| Socio-political | |||||||||||
| Health targets | 120 | 0.23 (0.07) *** | 0.02 (0.08) | 0.07 (0.10) | −0.00 (0.10) | 0.30 (0.09) ** | 0.19 (0.09) * | 0.08 (0.10) | 0.22 (0.06) ** | −0.03 (0.13) | 0.23 (0.14) ‡ |
| Social support | 119 | 0.54 (0.09) *** | 0.48 (0.11) *** | 0.40 (0.14) ** | 0.48 (0.14) *** | 0.31 (0.14) * | 0.23 (0.13) ‡ | 0.27 (0.15) ‡ | 0.53 (0.09) *** | 0.50 (0.20) * | 0.81 (0.19) *** |
| Potential Determinants | Intention to Implement the Intervention (b-path) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention Characteristics | Organisational Characteristics | Socio-cognitive Characteristics | |||||||||
| Observability (SE) | Relative advantage (SE) | Complexity (SE) | Trialability (SE) | Compatibility (SE) | Type (SE) | Size (SE) | Responsibility (SE) | Capacity (SE) | Health targets (SE) | Social support (SE) | |
| Individual intermediary characteristics | |||||||||||
| Attitude | −0.15 (0.20) | −0.17 (0.20) | −0.16 (0.20) | −0.13 (0.20) | −0.15 (0.20) | −0.16 (0.19) | −0.06 (0.22) | −0.18 (0.21) | −0.10 (0.20) | −0.15 (0.20) | −0.29 (0.21) |
| Self-efficacy | 0.04 (0.16) | 0.06 (0.16) | 0.03 (0.16) | 0.06 (0.16) | 0.09 (0.16) | 0.07 (0.16) | 0.05 (0.17) | 0.06 (0.16) | 0.02 (0.16) | 0.05 (0.17) | 0.03 (0.16) |
| Social norm | 0.03 (0.16) | 0.05 (0.16) | −0.01 (0.16) | 0.06 (0.16) | 0.04 (0.16) | 0.04 (0.15) | 0.11 (0.17) | 0.05 (0.16) | 0.01 (0.16) | 0.06 (0.16) | 0.06 (0.16) |
| Social support | −0.11 (0.17) | −0.14 (0.17) | −0.07 (0.17) | −0.12 (0.17) | −0.11 (0.17) | −0.16 (0.16) | −0.09 (0.18) | −0.13 (0.17) | −0.11 (0.16) | −0.15 (0.17) | −0.19 (0.17) |
| Knowledge | 0.16 (0.12) | 0.16 (0.12) | 0.14 (0.12) | 0.13 (0.12) | 0.13 (0.12) | 0.07 (0.12) | 0.11 (0.13) | 0.14 (0.12) | 0.06 (0.12) | 0.16 (0.12) | 0.14 (0.12) |
| Organisational intermediary characteristics | |||||||||||
| Attitude | 0.26 (0.14) ‡ | 0.29 (0.14) * | 0.29 (0.14) * | 0.27 (0.14) ‡ | 0.14 (0.15) | 0.26 (0.13) ‡ | 0.17 (0.15) | 0.26 (0.14) ‡ | 0.20 (0.14) | 0.28 (0.14) * | 0.31 (0.14) * |
| Self-efficacy | 0.53 (0.11) *** | 0.53 (0.12) *** | 0.40 (0.13) ** | 0.52 (0.12) *** | 0.51 (0.11) *** | 0.52 (0.11) *** | 0.54 (0.12) *** | 0.52 (0.12) *** | 0.37 (0.13) ** | 0.53 (0.12) *** | 0.54 (0.11) *** |
| Social norm | 0.65 (0.18) *** | 0.64 (0.18) *** | 0.62 (0.17) *** | 0.63 (0.17) *** | 0.54 (0.19) ** | 0.68 (0.17) *** | 0.50 (0.20) * | 0.64 (0.18) *** | 0.56 (0.17) ** | 0.67 (0.18) *** | 0.48 (0.18) * |
| Potential Deteminants | Individual Intermediary Characteristics | Organisational Intermediary Characteristics | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Attitude | Self-efficacy | Social norm | Social support | Knowledge | Attitude | Self-efficacy | Social norm | ||||
| ab-path (95% CI) | ab-path (95% CI) | ab-path (95% CI) | ab-path (95% CI) | ab-path (95% CI) | ab-path (95% CI) | % ME | ab-path (95% CI) | % ME | ab-path (95% CI) | % ME | |
| Intervention characteristics | |||||||||||
| Observability | −0.05 (−0.26–0.07) | 0.02 (−0.12–0.17) | 0.01 (−0.12-0.15) | −0.05 (−0.24–0.09) | 0.03 (−0.01–0.13) | 0.08 (0.00–0.26) | 43.8 | 0.17 (0.01–0.38) | 61.4 | 0.21 (0.10–0.40) | 66.7 |
| Relative advantage | −0.09 (−0.35–0.10) | 0.03 (−0.12–0.34) | 0.03 (−0.21–0.34) | −0.10 (−0.50–0.09) | 0.00 (−0.05–0.11) | −0.00 (−0.17–0.10) | - | 0.30 (0.10–0.62) | 73.2 | 0.50 (0.21–0.88) | 81.7 |
| Complexity | −0.03 (−0.18–0.02) | 0.01 (−0.08–0.09) | −0.00 (−0.09–0.08) | −0.01 (−0.09–0.03) | 0.02 (−0.01–0.11) | 0.07 (−0.00–0.22) | - | 0.29 (0.10–0.52) | 47.2 | 0.13 (0.04–0.31) | 29.2 |
| Trialability | −0.01 (−0.08–0.01) | 0.00 (−0.02–0.06) | 0.01 (−0.03–0.12) | 0.00 (−0.03–0.06) | −0.03 (−0.12–0.01) | −0.01 (−0.12–0.03) | - | 0.14 (0.05–0.29) | 84.2 | −0.02 (−0.14–0.06) | - |
| Compatibility | −0.04 (−0.19–0.06) | 0.02 (−0.04–0.13) | 0.01 (−0.05–0.10) | −0.02 (−0.16–0.03) | 0.03 (−0.02–0.11) | 0.07 (−0.07–0.23) | - | 0.20 (0.10–0.34) | 43.8 | 0.19 (0.06–0.37) | 42.8 |
| Organisational characteristics | |||||||||||
| Type | −0.01 (−0.10–0.02) | 0.00 (−0.02–0.06) | 0.00 (−0.03–0.06) | −0.02 (−0.11–0.01) | 0.02 (−0.04–0.09) | 0.03 (−0.00–0.11) | - | 0.05 (−0.02–0.13) | - | 0.01 (−0.09–0.13) | - |
| Size | 0.00 (0.00–0.00) | 0.00 (0.00–0.00) | 0.00 (0.00–0.00) | 0.00 (−0.00–0.00) | 0.00 (0.00–0.00) | 0.00 (−0.00–0.00) | - | 0.00 (−0.00–0.00) | - | −0.00 (−0.00–0.00) | - |
| Responsibility | −0.07 (−0.27–0.08) | 0.02 (−0.09–0.16) | 0.01 (−0.06–0.10) | −0.03 (−0.15–0.04) | 0.06 (−0.04–0.20) | 0.13 (−0.01–0.31) | - | 0.25 (0.13–0.43) | 73.5 | 0.20 (0.08–0.39) | 68.5 |
| Capacity | −0.02 (−0.13–0.06) | 0.01 (−0.11–0.11) | 0.00 (−0.09–0.10) | −0.03 (−0.18–0.04) | 0.02 (−0.07–0.12) | 0.09 (−0.03–0.24) | - | 0.24 (−0.08–0.45) | 39.3 | 0.14 (0.05–0.27) | 27.1 |
| Socio-political | |||||||||||
| Health targets | −0.03 (−0.15–0.05) | 0.00 (−0.03–0.06) | 0.00 (−0.02–0.07) | 0.00 (−0.04–0.04) | 0.05 (−0.02–0.15) | 0.05 (−0.00–0.19) | - | 0.04 (−0.07–0.17) | - | 0.15 (0.04–0.31) | 123.7 |
| Social support | −0.16 (−0.43–0.03) | 0.01 (−0.15–0.19) | 0.03 (−0.10–0.21) | −0.09 (−0.37–0.06) | 0.04 (−0.01–0.19) | 0.07 (−0.01–0.24) | - | 0.14 (0.02–0.33) | 0.26 (0.02–0.52) | 34.0 | |
3.3. Direct versus Indirect Associations
4. Discussion and Conclusions
4.1. Strengths and Limitations
4.2. Implications for Practice
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wilson, P.; Petticrew, M.; Calnan, M.; Nazareth, I. Disseminating research findings: What should researchers do? A systematic scoping review of conceptual frameworks. Implement. Sci. 2010, 5. [Google Scholar] [CrossRef]
- Wandersman, A.; Duffy, J.; Flaspohler, P.; Noonan, R.; Lubell, K.; Stillman, L.; Blanchman, M.; Dunville, R.; Saul, J. Bridging the gap between prevention research and practice: The interactive system framework for dissemination and implementation. Amer. J. Commun. Psychol. 2008, 41, 171–181. [Google Scholar] [CrossRef]
- Rabin, B.A.; Brownson, R.C.; Kerner, J.F.; Glasgow, R.E. Methodological challenges in disseminating evidence-based interventions to promote physical activity. Amer. J. Prev. Med. 2006, 31, 24–34. [Google Scholar] [CrossRef]
- Paulussen, T.; Wiefferink, K.; Mesters, I. Invoering van effectief gebleken interventies. In Gezondheidsvoorlichting en Gedragsverandering; Brug, J., van Assema, P., Lechner, L., Eds.; Van Gorcum: Assen, The Netherlands, 2008. [Google Scholar]
- Health and Development through Physical Activity and Sport; World Health Organization: Geneva, Switzerland, 2003.
- At Least Five a Week: Evidence on the Impact of Physical Activity and Its Relationship to Health; Department of Health: London, UK, 2004.
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the american college of sports medicine and the american heart association. Med. Sci. Sport. Exercise 2007, 39, 1435–1445. [Google Scholar] [CrossRef]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the american college of sports medicine and the american heart association. Circulation 2007, 116, 1081–1093. [Google Scholar]
- Peels, D.A.; Bolman, C.; Golsteijn, R.H.J.; De Vries, H.; Mudde, A.N.; Van Stralen, M.M.; Lechner, L. Long-term efficacy of a tailored physical activity intervention among older adults. Int. J. Behav. Nutr. Phys. Act. 2013, 10. [Google Scholar] [CrossRef]
- Bartholomew, L.; Parcel, G.; Kok, G.; Gottlieb, N.; Fernandez, M. Planning Health Promotyion Programs: An Intervention Mapping Approach; Jossey-Bass: San Francisco, CA, USA, 2011. [Google Scholar]
- Rogers, E.M. Diffusion of Innovations; The Free Press: New York, NY, USA, 2003. [Google Scholar]
- Paulussen, T.; Pin, R.; Mesters, I. Interventiedisseminatie en -implementatie. In Gezondheidsvoorlichting en Gedragsverandering: Een Planmatige Aanpak; Brug, J., van Assema, P., Lechner, L., Eds.; Van Gorcum: Assen, The Netherlands, 2011. [Google Scholar]
- Berndt, N.; Bolman, C.; de Vries, H.; Segaar, D.; van Boven, I.; Lechner, L. Smoking cessation treatment practices: Recommendations for improved adoption on cardiology wards. J. Cardiovasc. Nurs. 2013, 28, 35–47. [Google Scholar] [CrossRef]
- Segaar, D.; Bolman, C.; Willemsen, M.; de Vries, H. Identifying determinants of protocol adoption by midwives. Health Educ. Res. 2007, 22, 14–26. [Google Scholar]
- Bessems, K.M.H.H. Determinants of completeness of teachers’ implementation of the cutch school-based krachtvoer healthy diet programme. In The Dissemination of the Healthy Diet Programme Krachtvoer for Dutch Prevocational Schools; Datawyse/Universitaire Pers Maastricht: Maastricht, The Netherlands, 2011. [Google Scholar]
- Van Stralen, M.M.; Kok, G.; de Vries, H.; Mudde, A.N.; Bolman, C.; Lechner, L. The active plus protocol: Systematic development of two theory and evidence-based tailored physical activity interventions for the over-fifties. BMC Public Health 2008, 8. [Google Scholar] [CrossRef]
- Van Stralen, M.M.; de Vries, H.; Mudde, A.N.; Bolman, C.; Lechner, L. The working mechanisms for an environmentally tailored physical activity intervention for older adults: A randomized controlled trial. IJBNPA 2009, 6. [Google Scholar] [CrossRef]
- Peels, D.A.; van Stralen, M.M.; Bolman, C.; Golsteijn, R.H.J.; de Vries, H.; Mudde, A.N.; Lechner, L. The development of a web-based computer tailored advice to promote physical activity among people older than 50 years. J. Med. Internet Res. 2012, 14. [Google Scholar] [CrossRef]
- Peels, D.A.; Bolman, C.; Golsteijn, R.H.J.; de Vries, H.; Mudde, A.N.; van Stralen, M.M.; Lechner, L. Differences in reach and attrition between web-based or print-delivered tailored interventions among adults aged over fifty. J. Med. Internet Res. 2012, 14. [Google Scholar] [CrossRef]
- Mackinnon, D.P. Introduction to Statistical Mediation Analysis; Lawrence Erlbaum Associates: New York, NY, USA, 2008. [Google Scholar]
- MacKinnon, D.P. Mediation FAQ. Available online: http://www.public.asu.edu/~davidpm/ripl/maloy.htm (accessed on 7 January 2014).
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-based Approach; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Fleuren, M.; Wiefferink, K.; Paulussen, T. Determinants of innovations within health care organisations: Literature review and delphi study. Int. J. Qual. Health Care 2004, 16, 107–123. [Google Scholar] [CrossRef]
- Durlak, J.A.; DuPre, E.P. Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. Amer. J. Commun. Psychol. 2008, 41, 327–350. [Google Scholar] [CrossRef]
- Helmink, J.H.M.; Kremers, S.P.J.; van Boekel, L.C.; van Brussel-Visser, F.N.; de Vries, N.K. Factors determining the motivation of primary health care professionals to implement and continue the “beweegkuur” lifestyle intervention programme. J. Eval. Clin. Pract. 2011, 18, 682–688. [Google Scholar]
- Crone, M.R.; Verlaan, M.; Willemsen, M.C.; van Soelen, P.; Reijneveld, S.A.; Hira Sing, R.A.; Puaulussen, T.G.W.M. Sustainability of the prevention of passive infant smoking within well-baby clinics. Health Educ. Behav. 2013, 33. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Goodrich, D.E.; Robinson, C.H.; Fletcher, C.E.; Lowery, J.C. A systematic exploration of differences in contextual factors related to implementing the MOVE! Weight management program in VA: A mixed methods study. BMC Health Serv. Res. 2011, 11. [Google Scholar] [CrossRef]
- Smit, E.S.; de Vries, H.; Hoving, C. Determinants of practice nurses’ intention to implement a new smoking cessation intervention: The importance of attitude and innovation characteristics. J. Adv. Nurs. 2013. [Google Scholar] [CrossRef]
- Bartholomew, L.K.; Parcel, G.S.; Kok, G.; Gottlieb, N.H. Planning Health Promotion Programs; An Intervention Mapping Approach; Jossey-Bass: San Francisco, CA, USA, 2006. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Peels, D.; Mudde, A.; Bolman, C.; Golsteijn, R.; De Vries, H.; Lechner, L. Correlates of the Intention to Implement a Tailored Physical Activity Intervention: Perceptions of Intermediaries. Int. J. Environ. Res. Public Health 2014, 11, 1885-1903. https://doi.org/10.3390/ijerph110201885
Peels D, Mudde A, Bolman C, Golsteijn R, De Vries H, Lechner L. Correlates of the Intention to Implement a Tailored Physical Activity Intervention: Perceptions of Intermediaries. International Journal of Environmental Research and Public Health. 2014; 11(2):1885-1903. https://doi.org/10.3390/ijerph110201885
Chicago/Turabian StylePeels, Denise, Aart Mudde, Catherine Bolman, Rianne Golsteijn, Hein De Vries, and Lilian Lechner. 2014. "Correlates of the Intention to Implement a Tailored Physical Activity Intervention: Perceptions of Intermediaries" International Journal of Environmental Research and Public Health 11, no. 2: 1885-1903. https://doi.org/10.3390/ijerph110201885







