Health Professionals’ Alcohol-Related Professional Practices and the Relationship between Their Personal Alcohol Attitudes and Behavior and Professional Practices: A Systematic Review
Abstract
:1. Introduction
1.1. Why is Alcohol-Related Health Promotion Important?
1.2. Alcohol Use in Health Professionals
1.3. Health Professionals’ Personal Alcohol Attitudes and Behaviors
1.4. Using Screening Tools to Intervene with Patients Who have Alcohol-Related Problems
| The 5-As | Description |
|---|---|
| Assess | Alcohol use with a brief screening tool followed by clinical assessment as needed |
| Advise | Patients to reduce alcohol use to moderate levels |
| Agree | On individual goals for reducing alcohol use or abstinence (if indicated) |
| Assist | Patients with acquiring the motivation, self-help skills, and support needed for behavior change |
| Arrange | Follow-up support and repeated counseling, including referring dependent drinkers for specialty treatment |
1.5. Review Aims
2. Methods
2.1. Search Strategies
| Facets | Search terms |
|---|---|
| Alcohol | Alcohol; substance; drink |
| Health professional | Health professional; healthcare professional; healthcare provider; medical professional; medical staff; doctor; physician; nurse |
| Attitudes and behavior | Attitude; belief; perception; view; behavior; consumption |
| Practices | Practice; health promotion; prevention; health education; intervention; healthcare delivery; counseling; advice |
2.2. Eligibility Criteria
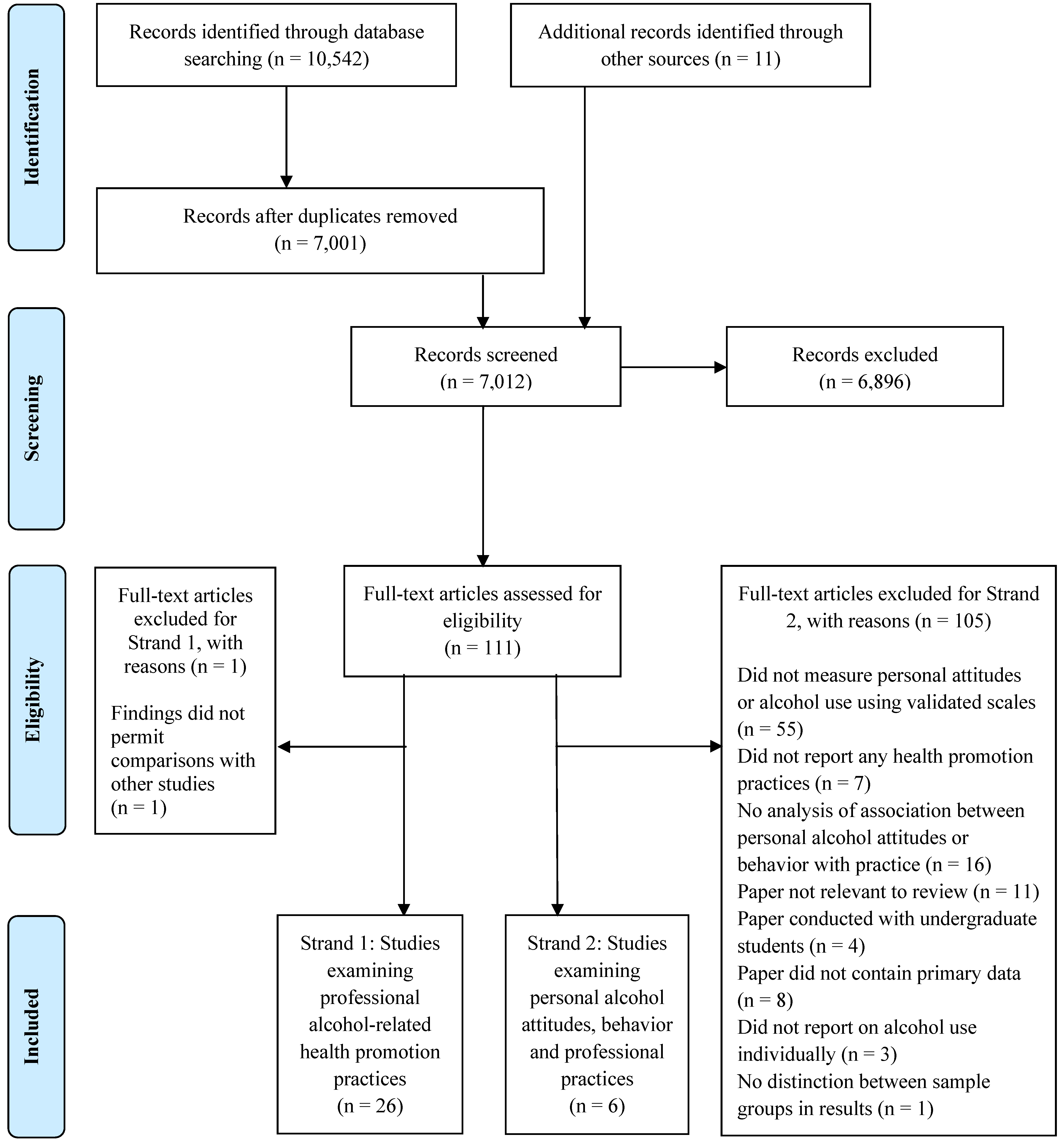
2.3. Study Identification
2.4. Data Extraction and Analysis
3. Results
3.1. Strand 1: Professional Alcohol-Related Health Promotion Practices
3.1.1. Overview of Selected Papers
3.1.2. Professional Alcohol-Related Health Promotion Practices
| Reference and location | Design and sample | Data collected | Quality rating |
|---|---|---|---|
| Aalto and Seppa, 2007, Finland [43] |
|
| Moderate |
| Amaral-Sabadini et al., 2010, Brazil [44] |
|
| Weak |
| Chun et al., 2011, USA [45] |
|
| Moderate |
| Demmert et al., 2011, Germany [46] |
|
| Weak |
| Fitzgerald et al., 2009, UK [47] |
|
| Weak |
| Freeman et al., 2011, Australia [48] |
|
| Moderate |
| Geirsson et al., 2009, Sweden [49] |
|
| Weak |
| Gross et al., 2012, UK [50] |
|
| Weak |
| Holmqvist et al., 2008, Sweden [51] |
|
| High |
| Holmqvist et al., 2008, Sweden [52] |
|
| Moderate |
| Indig, 2009, Australia [53] |
|
| Weak |
| Kesmodel and Kesmodel, 2011, Denmark [54] |
|
| Weak |
| Koopman et al., 2008, South Africa [55] |
|
| Weak |
| Lynagh et al., 2010, Australia [56] |
|
| Weak |
| McCaig et al., 2011, UK [57] |
|
| Moderate |
| Nilsen et al., 2011, Sweden [58] |
|
| Moderate |
| Nygaard et al., 2010, Norway [59] |
|
| Moderate |
| Payne et al., 2010, Australia [60] |
|
| Weak |
| Raistrick et al., 2008, UK [61] |
|
| Moderate |
| Seppanen et al., 2012, Finland [62] |
|
| Weak |
| Shepherd et al., 2011, UK [63] |
|
| Weak |
| Tsai et al., 2011, Taiwan [40] |
|
| Moderate |
| Vadlamudi et al., 2008, USA [42] |
|
| Weak |
| van Beurden et al., 2012, The Netherlands [41] |
|
| High |
| Vederhus et al., 2009, Norway [64] |
|
| High |
| Wilson et al., 2011, UK [65] |
|
| Moderate |
| Coverage of patients (>50%) | |||||||
|---|---|---|---|---|---|---|---|
| ASSESS | ADVISE | AGREE | ASSIST | ARRANGE | |||
| Study/5-A Element | Assess general a (%) | Assess using a screening tool b(%) | Advise general c (%) | Advise specific d (%) | Agree general e (%) | Assist general f (%) | Arrange referral g (%) |
| Aalto and Seppa, 2007 [43] | − | − | − | 19.6 Drs | 60.4 Drs | − | − |
| Amaral-Sabadini et al., 2010 [44] | − | 6.2 | − | − | 28.0 | − | − |
| Chun et al., 2011 [45] | 10.4 RNs | − | − | 24.2 RNs | − | − | 18.4 RNs |
| Demmert et al., 2011 [46] | 33.6 Drs | − | − | − | 35.0 Drs | − | 36.0 Drs |
| Fitzgerald et al., 2009 [47] | Not quantified Pharm | − | − | − | − | − | − |
| Freeman et al., 2011 [48] | 52.0 RNs | − | 58.5 RNs | 79.0 RNs | − | 41.0 RNs j | 21.0 RNs k |
| Geirsson et al., 2009 [49] | − | − | − | 12.0 Drs h 64.0 Drs i | 88.0 Drs h 36.0 Drs i | − | 90.0 Drs h 63.0 Drs i |
| Gross et al., 2012 [50] | 28.0 MS | 35.0 MS | − | − | − | − | 59.0 Drs |
| Holmqvist et al., 2008 [51] | 28.0 RNs 50.0 Drs | − | − | − | − | − | − |
| Holmqvist et al., 2008 [52] | 85.0 RNs 70.0 Drs | 80.0 RNs 50.0 Drs | − | − | − | − | − |
| Indig, 2009 [53] | 91.7 Drsv45.2 RNs | 5.7 Drs 4.9 RNs | − | − | 17.7 Drs 14.6 RNs | 25.7 Drs 42.9 RNs | 28.6 Drs 26.2 RNs |
| Kesmodel and Kesmodel, 2011 [54]l | − | − | − | 61.0 RMs | − | − | − |
| Koopman et al., 2008 [55] | 86.0 Drs | − | 82.0 Drs | 76.0 Drs | − | − | − |
| Lynagh et al., 2010 [56] | 40.0 MS | 1.0 MS | − | 4.0 MS | − | − | 4.0 MS m |
| McCaig et al., 2011 [57] | 18.9 Pharm | − | 15.5 Pharm | 18.9 Pharm | − | 2.0 Pharm | − |
| Nygaard et al., 2010 [59] | − | 5.5 Drs | − | 84.0 Drs | 67.5 Drs | − | 50.3 Drs |
| Raistrick et al., 2008 [61] | 40.0 MS | − | − | − | − | − | − |
| Shepherd et al., 2011 [63] | − | − | − | 17.0 Dents | − | − | − |
| Vederhus et al., 2009 [64] | − | − | − | − | − | − | 38.4 MS |
| Wilson et al., 2011 [65] l | 40.0 Drs | − | − | − | − | − | − |
| Coverage of patients (>50%) | |||||||
|---|---|---|---|---|---|---|---|
| ASSESS | ADVISE | AGREE | |||||
| Study/5-A Element | Intervention description | Time points | Assess general a (%) | Assess using a screening tool b(%) | Advise general c (%) | Advise specific d (%) | Agree general e (%) |
| Nilsen et al., 2011 [58] | Risk Drinking Project (training, seminars and information provision) | Baseline | − | 80.0 RNs f 50.0 Drs f | − | − | − |
| 3 years follow-up | − | 92.0 RNs f 79.0 Drs f | − | − | − | ||
| Payne et al., 2010 [60] | Educational resources | Baseline | 22.4 Dr s g | − | 5.3 Drs h | 50.1 Drs i | 88.9 Drs j |
| 6 months follow-up | 21.7 Drs g | − | 10.1 Drs h | 28.1 Drs i | 68.3 Drs j | ||
| Seppanen et al., 2012 [62] | The Finnish Alcohol Programme (2004-2007) (information and support provision) | Baseline | − | − | − | − | 9.3 Drs k |
| 5 years follow-up | − | − | − | − | 17.2 Drs k | ||
| Tsai et al., 2011 [40] | Alcohol Training Program (information provision and discussions) | Baseline | 62.8 RNs l | − | − | − | − |
| 1 month follow-up | 61.5 RNsm | − | − | − | − | ||
| 3 months follow-up | 65.8 RNsn | ||||||
| Van Beurden et al., 2012 [41] | Professionals, organizational and patient-directed activities program | Baseline | − | 4.0 Drs o | − | 1.5 Drs q | − |
| 1 year follow-up | − | 9.0 Drs p | − | 3.5 Drs r | − | ||
Professional Activity Levels
The Effect of Interventions upon Professional Activity
3.2. Strand 2: Relationships between Professional Alcohol-Related Health Promotion Practices, Personal Attitudes and/or Alcohol Use
3.2.1. Overview of Selected Papers
| Reference and location | Design and sample | Instruments and data collected | Key findings | Quality rating |
|---|---|---|---|---|
| Aalto & Seppa, 2007,Finland [43] | Cross-sectional survey National census sample of doctors in primary health care centers n = 3,193 (61.0% response rate) |
|
| Moderate |
| Freeman et al., 2011, Australia [48] | Cross-sectional survey National convenience sample of nurses in EDs n = 125 (40.0% response rate) |
|
| Moderate |
| Geirsson et al., 2009, Sweden [49] | Cross-sectional survey Census sample of doctors in primary care in Skaraborg (Regional) n = 68 (52.0% response rate) |
|
| Weak |
| Raistrick et al., 2008, UK [61] | Cross-sectional survey Census sample of staff in six health authorities in Yorkshire and Humberside (Regional) n = 1,141 (42.0% response rate) (n = 100 doctors; n = 788 nurses; n = 228 healthcare assistants; n = 25 other medical staff) |
|
| Moderate |
| Shepherd et al., 2011, UK [63] | Cross-sectional survey National random sample of dentists in Scotland n = 175 (60.0% response rate) |
|
| Weak |
| Vadlamudi et al., 2008, USA [42] | Quasi-experiment Convenience sample of graduate nursing students at a single university n = 181 (response rate not reported) |
|
| Weak |
3.2.2. Instruments Used to Measure Personal Attitudes and Alcohol Use
3.2.3. Association between Personal Attitudes towards Alcohol and Professional Alcohol-Related Health Promotion Practices
3.2.4. Association between Personal Alcohol Use and Professional Alcohol-Related Health Promotion Practices
4. Discussion
4.1. Overview of Findings
4.2. Methodological Quality of the Included Studies
4.3. Strengths and Limitations of the Review
4.4. Implications for Practice and Future Research
5. Conclusions
Conflicts of Interest
References
- World Health Organization. Global Status Report on Alcohol and Health. WHO Press: Geneva, Switzerland, 2011. Available online: http://www.who.int/substance_abuse/publications/global_alcohol_report/msbgsruprofiles.pdf (accessed on 18 September 2013).
- World Health Organization. Alcohol Fact Sheet. WHO Media Centre: Geneva, Switzerland, 2011. Available online: http://www.who.int/mediacentre/factsheets/fs349/en/ (accessed on 18 September 2013).
- Rehm, J.; Room, R.; Graham, K.; Monteiro, M.; Gmel, G.; Sempos, C.T. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: An overview. Addiction 2003, 98, 1209–1228. [Google Scholar] [CrossRef]
- World Health Organization. Screening and Brief Intervention. WHO Programmes and Projects: Geneva, Switzerland, 2003. Available online: http://www.who.int/substance_abuse/publications/en/SBIFactSheet.pdf (accessed on 18 September 2013).
- Bazargan, M.; Makar, M.; Bazargan-Hejazi, S.; Ani, C.; Wolf, K.E. Preventive, lifestyle, and personal health behaviors among physicians. Acad. Psychiatry 2009, 33, 289–295. [Google Scholar] [CrossRef]
- O’Cathail, M.; O’Callaghan, M. A profile of hospital consultants: The health practices of a cohort of medical professionals. Irish Med. J. 2013, 106, 134–136. [Google Scholar]
- Oreskovich, M.R.; Kaups, K.L.; Balch, C.M.; Hanks, J.B.; Satele, D.; Sloan, J.; Meredith, C.; Buhl, A.; Dyrbye, L.N.; Shanafelt, T.D. Prevalence of alcohol use disorders among American surgeons. Arch. Surg. 2012, 147, 168–174. [Google Scholar] [CrossRef]
- Schluter, P.J.; Turner, C.; Benefer, C. Long working hours and alcohol risk among Australian and New Zealand nurses and midwives: A cross-sectional study. Int. J. Nurs. Stud. 2012, 49, 701–709. [Google Scholar] [CrossRef]
- Unrath, M.; Zeeb, H.; Letzel, S.; Claus, M.; Escobar Pinzon, L.C. Identification of possible risk factors for alcohol use disorders among general practitioners in Rhineland-Palatinate, Germany. Swiss Med. Wkly. 2012, 142. [Google Scholar] [CrossRef]
- Voigt, K.; Twork, S.; Mittag, D.; Gobel, A.; Voigt, R.; Klewer, J.; Kugler, J.; Bornstein, S.R.; Bergmann, A. Consumption of alcohol, cigarettes and illegal substances among physicians and medical students in Brandenburg and Saxony (Germany). BMC Health Serv. Res. 2009, 9. [Google Scholar] [CrossRef]
- Kenna, G.A.; Wood, M.D. The prevalence of alcohol, cigarette and illicit drug use and problems among dentists. J. Am. Dent. Assoc. 2005, 136, 1023–1032. [Google Scholar]
- Aalto, M.; Hyvonen, S.; Seppa, K. Do primary care physicians’ own audit scores predict their use of brief alcohol intervention? A cross-sectional survey. Drug Alcohol Dependence 2006, 83, 169–173. [Google Scholar] [CrossRef]
- Rosta, J.; Aasland, O.G. Changes in alcohol drinking patterns and their consequences among Norwegian doctors from 2000 to 2010: A longitudinal study based on national samples. Alcohol Alcoholism. 2013, 48, 99–106. [Google Scholar] [CrossRef]
- Baldisseri, M.R. Impaired healthcare professional. Crit. Care Med. 2007, 35, S106–S116. [Google Scholar] [CrossRef]
- Frank, E.; Segura, C. Health practices of Canadian physicians. Can. Fam. Physician 2009, 55, 810–811. [Google Scholar]
- Sebo, P.; Gallacchi, M.B.; Goehring, C.; Kunzi, B.; Bovier, P.A. Use of tobacco and alcohol by Swiss primary care physicians: A cross-sectional survey. BMC Public Health 2007, 7. [Google Scholar] [CrossRef]
- Kenna, G.A.; Wood, M.D. Alcohol use by healthcare professionals. Drug Alcohol Depend. 2004, 75, 107–116. [Google Scholar] [CrossRef]
- Nash, L.M.; Daly, M.G.; Kelly, P.J.; van Ekert, E.H.; Walter, G.; Walton, M.; Willcock, S.M.; Tennant, C.C. Factors associated with psychiatric morbidity and hazardous alcohol use in Australian doctors. Med. J. Aust. 2010, 193, 161–166. [Google Scholar]
- Watson, H.; Whyte, R.; Schartau, E.; Jamieson, E. Survey of student nurses and midwives: Smoking and alcohol use. Br. J. Nurs. 2006, 15, 1212–1216. [Google Scholar]
- Baldwin, J.N.; Bartek, J.K.; Scott, D.M.; Davis-Hall, R.E.; DeSimone, E.M., 2nd. Survey of alcohol and other drug use attitudes and behaviors in nursing students. Subst. Abuse 2009, 30, 230–238. [Google Scholar] [CrossRef]
- Blake, H.; Malik, S.; Mo, P.K.; Pisano, C. “Do as say, but not as I do”: Are next generation nurses role models for health? Perspect. Public Health 2011, 131, 231–239. [Google Scholar] [CrossRef]
- World Health Organization. Health Professions Networks. WHO Programmes and Projects: Geneva, Switzerland, 2013. Available online: http://www.who.int/hrh/professionals/en/ (accessed on 18 September 2013).
- Crothers, C.E.; Dorrian, J. Determinants of nurses’ attitudes toward the care of patients with alcohol problems. ISRN Nurs. 2011, 2011. [Google Scholar] [CrossRef]
- Gilchrist, G.; Moskalewicz, J.; Slezakova, S.; Okruhlica, L.; Torrens, M.; Vajd, R.; Baldacchino, A. Staff regard towards working with substance users: A European multi-centre study. Addiction 2011, 106, 1114–1125. [Google Scholar] [CrossRef]
- Geirsson, M.; Bendtsen, P.; Spak, F. Attitudes of Swedish general practitioners and nurses to working with lifestyle change, with special reference to alcohol consumption. Alcohol Alcoholism 2005, 40, 388–393. [Google Scholar] [CrossRef]
- Murray, M.M.; Li, T.-K. Expanding the role of the generalist nurse in the prevention and treatment of alcohol use disorders. J. Addict. Nurs. 2007, 18, 163–165. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Emont, S.; Miller, D.C. Assessing delivery of the five “As” for patient-centered counseling. Health Promot. Int. 2006, 21, 245–255. [Google Scholar]
- Dosh, S.A.; Holtrop, J.S.; Torres, T.; Arnold, A.K.; Baumann, J.; White, L.L. Changing organizational constructs into functional tools: An assessment of the 5 A’s in primary care practices. Ann. Fam. Med. 2005, 3, S50–S52. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—ii. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Riboldi, L.; Bordini, L.; Ferrario, M.M. Fitness for work in health care workers: State of the art and possible operational recommendations for its formulation and management in relationship to alcohol and drug addiction. Med. Lav. 2012, 103, 203–211. [Google Scholar]
- Pipe, A.; Sorensen, M.; Reid, R. Physician smoking status, attitudes toward smoking, and cessation advice to patients: An international survey. Patient Educ. Couns. 2009, 74, 118–123. [Google Scholar] [CrossRef]
- Fie, S.; Norman, I.J.; While, A.E. The relationship between physicians’ and nurses’ personal physical activity habits and their health-promotion practice: A systematic review. Health Educ. J. 2013, 72, 102–119. [Google Scholar] [CrossRef]
- Zhu, D.; Norman, I.J.; While, A.E. The relationship between health professionals’ weight status and attitudes towards weight management: A systematic review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2011, 12, 324–337. [Google Scholar] [CrossRef]
- Zhu, D.Q.; Norman, I.J.; While, A.E. The relationship between doctors’ and nurses’ own weight status and their weight management practices: A systematic review. Obes. Rev.: Off. J. Int. Assoc. Study Obes. 2011, 12, 459–469. [Google Scholar] [CrossRef]
- Kishore, V.; Lynch, S.; Pichon, J.; Theall, K.; Johnson, S.; Roberson, E.; Hinton, S. Knowledge, attitudes and practice relating to hazardous alcohol use across the continuum of care in a community healthcare centre. Drugs-Educ. Prev. Policy 2011, 18, 60–68. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Altman, D.G.; Egger, M.; Gotzsche, P.C.; Pocock, S.J.; Vandenbroucke, J.P.; von Elm, E. Strobe Checklist for Cross-Sectional Studies; ISPM: University of Bern: Bern, Switzerland, 2007. Available online: http://www.strobe-statement.org (accessed on 3 September 2013).
- Schulz, K.F.; Altman, D.G.; Moher, D. Consort 2010 statement: Updated guidelines for reporting parallel group randomised trials. Br. Med. J. 2010, 340. [Google Scholar] [CrossRef]
- Enhancing the Quality and Transparency of Health Research; The Equator Network: Oxford, UK, 2013. Available online: http://www.equator-network.org/ (accessed on 3 September 2013).
- Tsai, Y.F.; Tsai, M.C.; Lin, Y.P.; Weng, C.E.; Chou, Y.L.; Chen, C.Y. An alcohol training program improves chinese nurses’ knowledge, self-efficacy, and practice: A randomized controlled trial. Alcohol: Clin. Exp. Res. 2011, 35, 976–983. [Google Scholar] [CrossRef]
- Van Beurden, I.; Anderson, P.; Akkermans, R.P.; Grol, R.P.; Wensing, M.; Laurant, M.G. Involvement of general practitioners in managing alcohol problems: A randomized controlled trial of a tailored improvement programme. Addiction 2012, 107, 1601–1611. [Google Scholar] [CrossRef]
- Vadlamudi, R.; Adams, S.; Hogan, B. Nurses’ attitudes, beliefs and confidence levels regarding care for those who abuse alcohol: Impact of educational intervention. Nurse Educ. Pract. 2008, 8, 290–298. [Google Scholar] [CrossRef]
- Aalto, M.; Seppa, K. Primary health care physicians’ definitions on when to advise a patient about weekly and binge drinking. Addict. Behav. 2007, 32, 1321–1330. [Google Scholar] [CrossRef]
- Amaral-Sabadini, M.B.; Saitz, R.; Souza-Formigoni, M.L. Do attitudes about unhealthy alcohol and other drug (AOD) use impact primary care professionals’ readiness to implement AOD-related preventive care? Drug Alcohol Rev. 2010, 29, 655–661. [Google Scholar] [CrossRef]
- Chun, T.H.; Spirito, A.; Rakowski, W.; D’Onofrio, G.; Woolard, R.H. Beliefs and practices of pediatric emergency physicians and nurses regarding counseling alcohol-using adolescents: Can counseling practice be predicted? Pediatr. Emerg. Care 2011, 27, 812–825. [Google Scholar] [CrossRef]
- Demmert, A.; Grothues, J.M.; Rumpf, H.J. Attitudes towards brief interventions to reduce smoking and problem drinking behaviour in gynaecological practice. Public Health 2011, 125, 182–186. [Google Scholar] [CrossRef]
- Fitzgerald, N.; Watson, H.; McCaig, D.; Stewart, D. Developing and evaluating training for community pharmacists to deliver interventions on alcohol issues. Pharm. World Sci. 2009, 31, 149–153. [Google Scholar] [CrossRef]
- Freeman, T.; Roche, A.M.; Williamson, P.; Pidd, K. Hazardous alcohol use interventions with emergency patients: Self-reported practices of nurses, and predictors of behaviour. Emerg. Med. Australas. 2011, 23, 479–489. [Google Scholar] [CrossRef]
- Geirsson, M.; Hensing, G.; Spak, F. Does gender matter? A vignette study of general practitioners’ management skills in handling patients with alcohol-related problems. Alcohol Alcoholism 2009, 44, 620–625. [Google Scholar] [CrossRef]
- Gross, S.R.; Marshall, E.J.; Wolff, K. Substance misuse among health care workers: National survey of occupational physicians. Occup. Med. 2012, 62, 254–260. [Google Scholar] [CrossRef]
- Holmqvist, M.; Bendtsen, P.; Spak, F.; Rommelsjo, A.; Geirsson, M.; Nilsen, P. Asking patients about their drinking.A national survey among primary health care physicians and nurses in Sweden. Addict. Behav. 2008, 33, 301–314. [Google Scholar] [CrossRef]
- Holmqvist, M.; Hermansson, U.; Nilsen, P. Towards increased alcohol intervention activity in Swedish occupational health services. Int. J. Occup. Med. Environ. Health 2008, 21, 179–187. [Google Scholar]
- Indig, D.; Copeland, J.; Conigrave, K.M.; Rotenko, I. Attitudes and beliefs of emergency department staff regarding alcohol-related presentations. Int. Emerg. Nurs. 2009, 17, 23–30. [Google Scholar] [CrossRef]
- Kesmodel, U.S.; Kesmodel, P.S. Alcohol in pregnancy: Attitudes, knowledge, and information practice among midwives in Denmark 2000 to 2009. Alcohol: Clin. Exp. Res. 2011, 35, 2226–2230. [Google Scholar] [CrossRef]
- Koopman, F.A.; Parry, C.D.; Myers, B.; Reagon, G. Addressing alcohol problems in primary care settings: A study of general medical practitioners in Cape Town, South Africa. Scand. J. | Public Health 2008, 36, 298–302. [Google Scholar]
- Lynagh, M.; Sanson-Fisher, R.; Shakeshaft, A. Alcohol-related harm: Perceptions of ambulance officers and health promotion actions they do and would do. Health Promot. J. Aust. 2010, 21, 19–25. [Google Scholar]
- McCaig, D.; Fitzgerald, N.; Stewart, D. Provision of advice on alcohol use in community pharmacy: A cross-sectional survey of pharmacists’ practice, knowledge, views and confidence. Int. J. Pharm. Pract. 2011, 19, 171–178. [Google Scholar] [CrossRef]
- Nilsen, P.; Holmqvist, M.; Hermansson, U. Alcohol prevention in Swedish occupational health care. Occup. Med. 2011, 61, 472–479. [Google Scholar] [CrossRef]
- Nygaard, P.; Paschall, M.J.; Aasland, O.G.; Lund, K.E. Use and barriers to use of screening and brief interventions for alcohol problems among Norwegian general practitioners. Alcohol Alcoholism 2010, 45, 207–212. [Google Scholar] [CrossRef]
- Payne, J.M.; France, K.E.; Henley, N.; D’Antoine, H.A.; Bartu, A.E.; Mutch, R.C.; Elliott, E.J.; Bower, C. Paediatricians’ knowledge, attitudes and practice following provision of educational resources about prevention of prenatal alcohol exposure and fetal alcohol spectrum disorder. J. Paediatr. Child Health 2011, 47, 704–710. [Google Scholar] [CrossRef]
- Raistrick, D.; Russell, D.; Tober, G. A survey of substance use by health care professionals and their attitudes to substance misuse patients (NHS staff survey). J. Subst. Use 2008, 13, 57–69. [Google Scholar]
- Seppanen, K.K.; Aalto, M.; Seppa, K. Institutionalization of brief alcohol intervention in primary health care-the Finnish case. Alcohol: Clin. Exp. Res. 2012, 36, 1456–1461. [Google Scholar] [CrossRef]
- Shepherd, S.; Bonnetti, D.; Clarkson, J.E.; Ogden, G.R.; Young, L. Current practices and intention to provide alcohol-related health advice in primary dental care. British Dental Journal 2011, 211. [Google Scholar] [CrossRef]
- Vederhus, J.K.; Kristensen, O.; Laudet, A.; Clausen, T. Attitudes towards 12-step groups and referral practices in a 12-step naive treatment culture; a survey of addiction professionals in norway. BMC Health Services Research 2009, 9. [Google Scholar] [CrossRef]
- Wilson, G.B.; Lock, C.A.; Heather, N.; Cassidy, P.; Christie, M.M.; Kaner, E.F. Intervention against excessive alcohol consumption in primary health care: A survey of GPs’ attitudes and practices in England 10 years on. Alcohol Alcoholism 2011, 46, 570–577. [Google Scholar] [CrossRef]
- Cartwright, A.K.J. The attitudes of helping agents towards the alcoholic client: The influence of experience, support, training, and self-esteem. Br. J. Addict. 1980, 75, 413–431. [Google Scholar]
- Anderson, P.; Clement, S. The AAPPQ revisited: The measurement of general practitioners’ attitudes to alcohol problems. Br. J. Addict. 1987, 82, 753–759. [Google Scholar]
- Cammann, C.; Fichman, M.; Jenkins, G.J.; Klesh, J. Assessing the Attitudes and Perceptions of Organizational Members. In Assessing Organizational Change: A Guide to Methods, Measures, and Practices; Seashore, S., Lawler, E.I., Mirvis, P., Cammann, C., Eds.; Wiley: New York, NY, USA, 1983; pp. 71–138. [Google Scholar]
- Karasek, R.; Brisson, C.; Kawakami, N.; Houtman, I.; Bongers, P.; Amick, B. The job content questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. J. Occup. Health Psychol. 1998, 3, 322–355. [Google Scholar]
- Drummond, D.C. The relationship between alcohol dependence and alcohol-related problems in a clinical population. Br. J. Addict. 1990, 85, 357–366. [Google Scholar] [CrossRef]
- Sheridan, J.; Wheeler, A.; Chen, L.J.H.; Huang, A.C.Y.; Leung, I.N.Y.; Tien, K.Y.C. Screening and brief interventions for alcohol: Attitudes, knowledge and experience of community pharmacists in Auckland, New Zealand. Drug Alcohol Rev. 2008, 27, 380–387. [Google Scholar]
- Kaner, E.F.S.; Heather, N.; Mcavoy, B.R.; Lock, C.A.; Gilvarry, E. Intervention for excessive alcohol consumption in primary health care: Attitudes and practices of English general practitioners. Alcohol Alcoholism 1999, 34, 559–566. [Google Scholar]
- Tsai, Y.F.; Tsai, M.C.; Lin, Y.P.; Weng, C.E.; Chen, C.Y.; Chen, M.C. Facilitators and barriers to intervening for problem alcohol use. J. Adv. Nurs. 2010, 66, 1459–1468. [Google Scholar] [CrossRef]
- Vargas, D.; Luis, M.A. Alcohol, alcoholism and alcohol addicts: Conceptions and attitudes of nurses from district basic health centers. Rev. Lat. Am. Enfermagem 2008, 16, 543–550. [Google Scholar]
- Das, A.K.; Corrado, O.J.; Kyerematen, E.; Smithson, J.A.J.; West, R.M. Do doctors understand alcohol units? Clin. Med. 2009, 9, 525–527. [Google Scholar]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Bakhshi, S.; While, A.E. Health Professionals’ Alcohol-Related Professional Practices and the Relationship between Their Personal Alcohol Attitudes and Behavior and Professional Practices: A Systematic Review. Int. J. Environ. Res. Public Health 2014, 11, 218-248. https://doi.org/10.3390/ijerph110100218
Bakhshi S, While AE. Health Professionals’ Alcohol-Related Professional Practices and the Relationship between Their Personal Alcohol Attitudes and Behavior and Professional Practices: A Systematic Review. International Journal of Environmental Research and Public Health. 2014; 11(1):218-248. https://doi.org/10.3390/ijerph110100218
Chicago/Turabian StyleBakhshi, Savita, and Alison E. While. 2014. "Health Professionals’ Alcohol-Related Professional Practices and the Relationship between Their Personal Alcohol Attitudes and Behavior and Professional Practices: A Systematic Review" International Journal of Environmental Research and Public Health 11, no. 1: 218-248. https://doi.org/10.3390/ijerph110100218




