The Social Determinants of Infant Mortality and Birth Outcomes in Western Developed Nations: A Cross-Country Systematic Review
Abstract
:1. Introduction
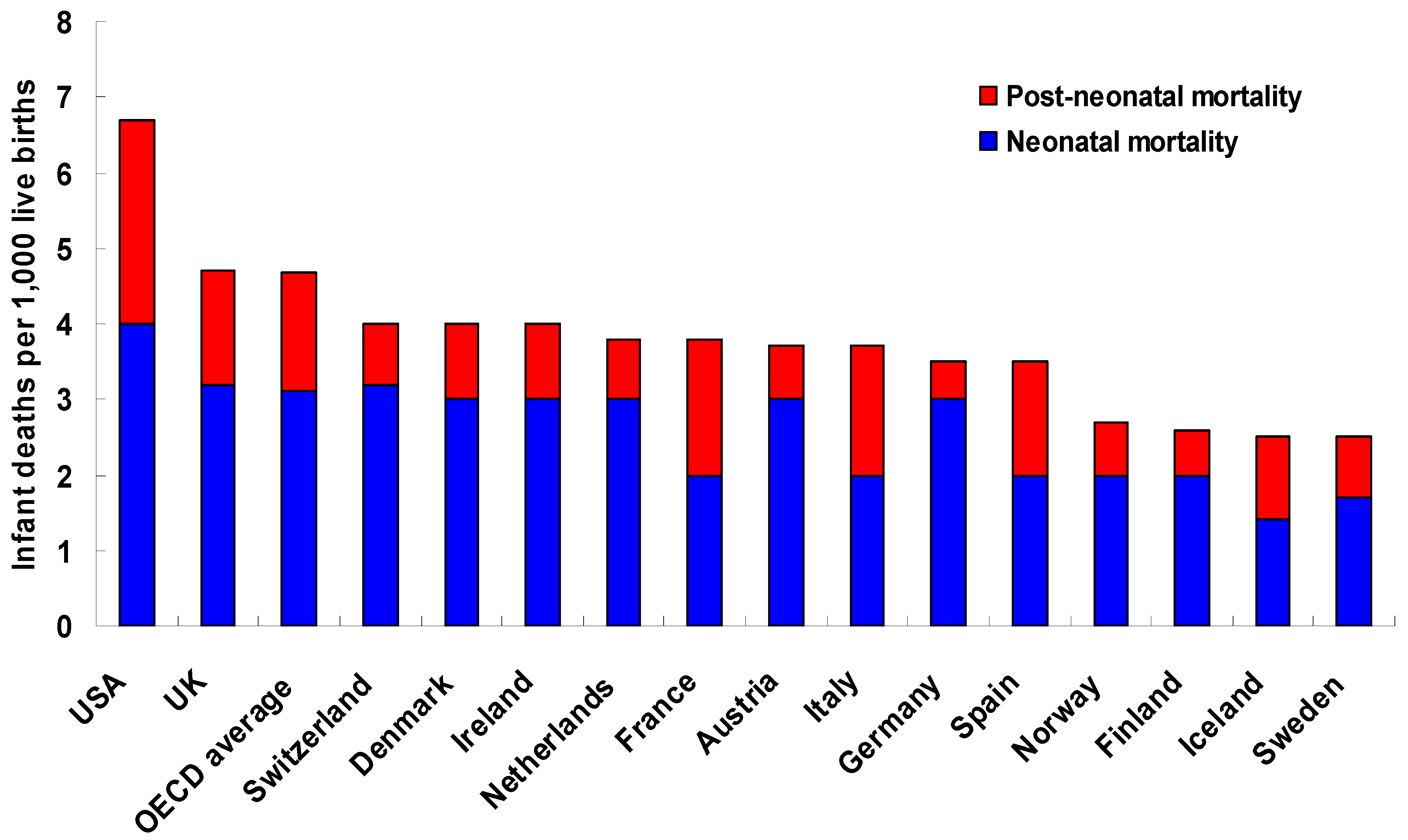
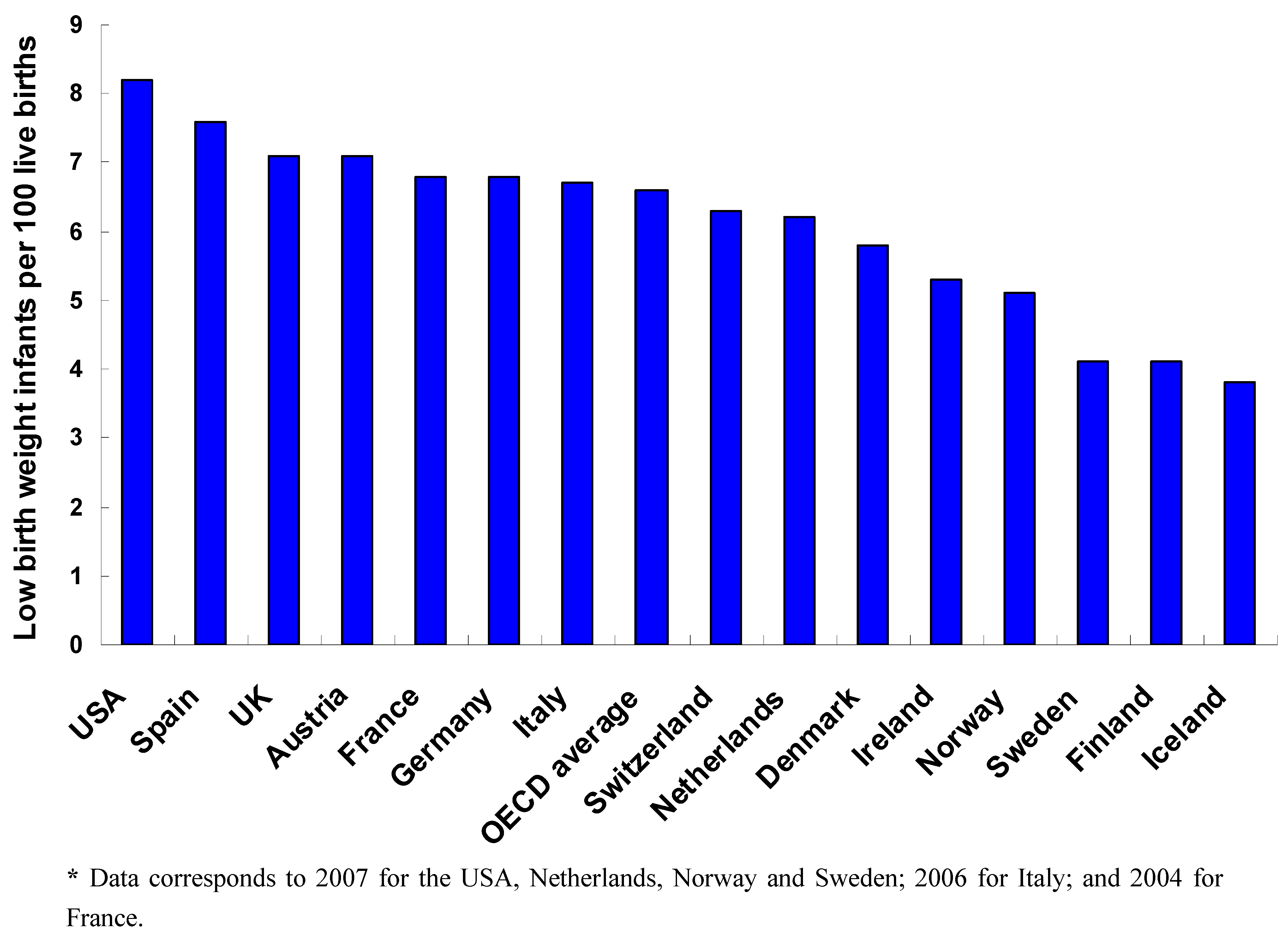
1.1. Between-Country Variations in IM/Birth Outcomes
1.2. Within-Country Variations in IM/Birth Outcomes
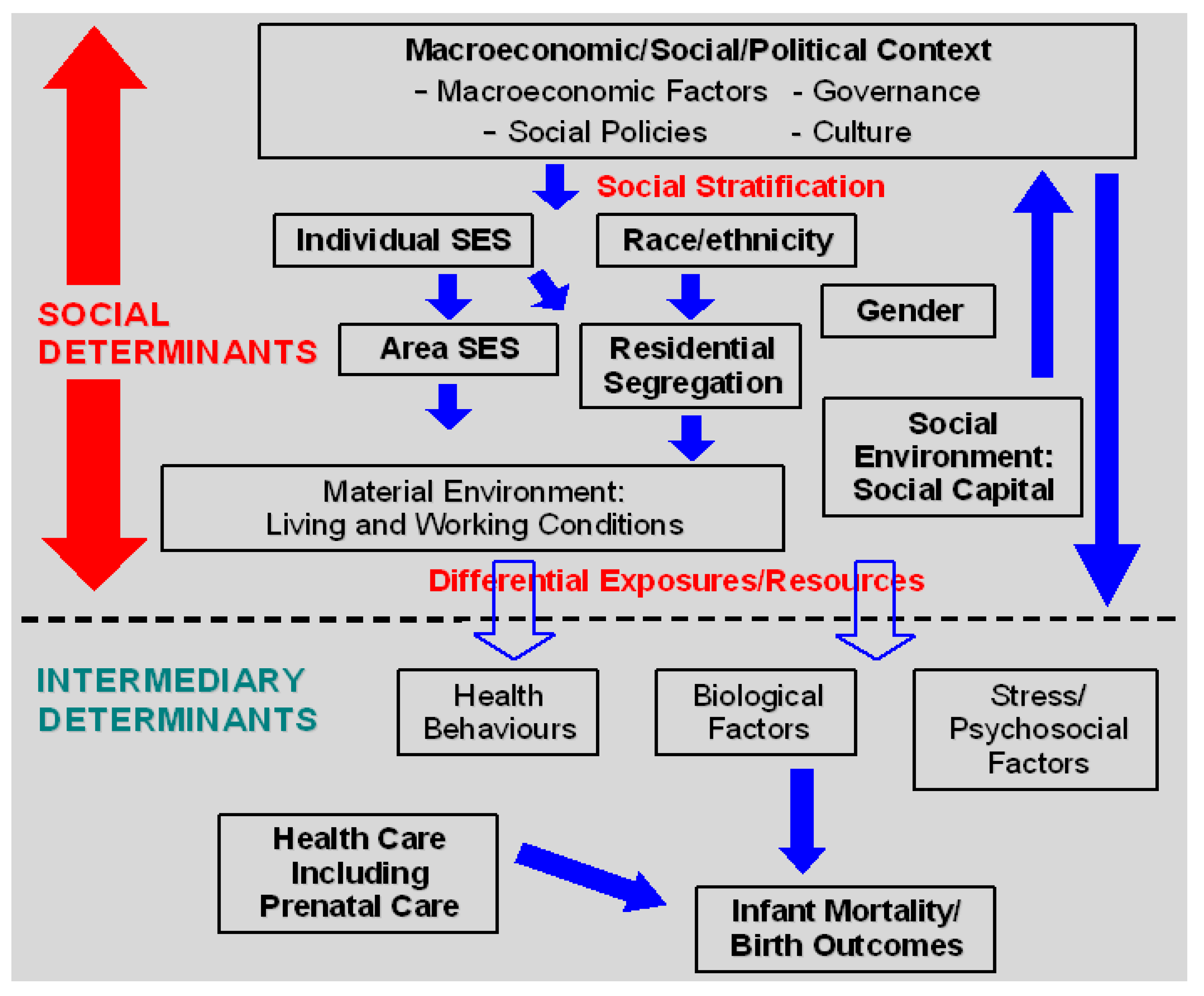
1.3. A Social Determinants of IM/Birth Outcomes Conceptual Framework
2. Methods
2.1. Systematic Literature Review
3. Results
3.2. Within-Country Evidence on Contextual Social Determinants
3.2.1. Neighbourhood SES/Material Conditions
3.2.2. Residential Segregation
3.2.3. Income Inequality
3.2.4. Social Cohesion/Social Capital
3.3. Within-Country Evidence on Individual Level Social Determinants
3.3.2. Individual SES
3.3.3. Health Behaviours
4. Discussion
5. Conclusions
Conflicts of Interest
Acknowledgements
References
- World Bank. World Development Indicators: Level & Trends in Child Mortality. Report 2010. Available online: http://data.worldbank.org/indicator/SH.DYN.MORT (accessed on 1 November 2012).
- Organization for Economic Co-operation and Development (OECD), OECD Family Database; OECD: Paris, France, 2011.
- MacDorman, M.F.; Mathews, T.J. NCHS data brief: Recent trends in infant mortality in the United States. Natl. Center Health Stat. 2008, 9, 1–8. [Google Scholar]
- MacDorman, M.F.; Hoyert, D.L.; Martin, J.; Munson, M.L.; Hamilton, B.E. Fetal and perinatal mortality, United States, 2003. Natl. Vital Stat. Reports 2007, 55, 1–20. [Google Scholar]
- Neonatal and Perinatal Mortality: Country, Regional, and Global Estimates; World Health Organization: Geneva, Switzerland, 2006.
- Mathews, T.J.; MacDorman, M.F. Infant mortality statistics from the 2006 period linked birth/infant death data set. Natl. Vital Stat. Reports 2010, 58, 1–32. [Google Scholar]
- Beck, S.; Wojdyla, D.; Say, L.; Betran, A.P.; Merialdi, M.; Requejo, J.H.; Rubens, C.; Menon, R.; van Look, P.F.A. The worldwide incidence of preterm birth: A systematic review of maternal mortality and morbidity. Bull. WHO 2010, 88, 31–38. [Google Scholar]
- Lawn, J.E.; Gravett, M.G.; Nunes, T.M.; Rubens, C.E.; Cynthia, S.; GAPPS Review Group. Global report on preterm birth and stillbirth (1 of 7): Definitions, description of the burden and opportunities to improve data. BMC Pregnancy Childbirth 2010, 10 (Suppl. 1), S1. [Google Scholar] [CrossRef]
- UNICEF, Low Birth Weight: Country, Regional, and Global Estimates; United Nations Children’s Fund and World Health Organization: New York, NY, USA, 2004.
- Hamilton, B.E.; Martin, J.A.; Ventura, S.J. Births: Preliminary data for 2009. Natl. Vital Stat. Reports 2010, 59, 1–19. [Google Scholar]
- OECD. Health at a Glance: Europe 2010. Available online: http://dx.doi.org/10.1787/health_glance-2010-en (accessed on 1 November 2012).
- Conley, D.; Springer, K.W. Welfare state and infant mortality. Am. J. Sci. 2001, 107, 768–807. [Google Scholar]
- Odd, D.E.; Gunnell, D.; Lewis, G.; Rasmussen, F. Long-term impact of poor birth condition on social and economic outcomes in early adulthood. Pediatrics 2011, 127, e1498–e1504. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Infant mortality and low birth weight among Black and White infants—United States, 1980–2000. MMWR 2002, 51, 589–592.
- Blumenshine, P.; Egerter, S.; Barclay, C.J.; Cubbin, C.; Braveman, P.A. Socioeconomic disparities in adverse birth outcomes: A systematic review. Am. J. Prev. Med. 2010, 39, 263–272. [Google Scholar] [CrossRef]
- Shah, N.R.; Bracken, M.B. A systematic review and meta-analysis of prospective studies on the association between maternal cigarette smoking and preterm delivery. Am. J. Obstetr. Gyn. 2010, 182, 465–472. [Google Scholar]
- Littleton, H.L.; Bye, K.; Buck, K.; Amacker, A. Psychosocial stress during pregnancy and perinatal outcomes: A meta-analytic review. J. Psychosom. Obstetr. Gyn. 2010, 31, 219–228. [Google Scholar] [CrossRef]
- Gray, R.; Headley, J.; Oakley, L.; Kurinczuk, J.J.; Brocklehurst, P.; Hollowell, J. Inequalities in Infant Mortality Project Briefing Paper 3. Towards an Understanding of Variations in Infant Mortality Rates between Different Ethnic Groups; National Perinatal Epidemiology Unit: Oxford, UK, 2009. [Google Scholar]
- Patel, R.; Steer, P.; Doyle, P.; Little, M.P.; Elliott, P. Does gestation vary by ethnic group? A London-based study of over 122,000 pregnancies with spontaneous onset of labour. Int. J. Epi. 2003, 33, 107–113. [Google Scholar]
- Field, D.; Draper, E.S.; Fenton, A.; Papiernik, E.; Zeitlin, J.; Blondel, B.; Cuttini, M.; Maier, R.F.; Weber, T.; Carrapato, M.; et al. Rates of very preterm birth in Europe and neonatal mortality rates. Arch. Dis. Child. Fetal Neonatal. Ed. 2009, 94, F253–F256. [Google Scholar] [CrossRef]
- Zeitlin, J.; Bucourt, M.; Rivera, L.; Topuz, B.; Papiernik, E. Preterm birth and maternal country of birth in a French district with a multiethnic population. Br. J. Obstetr. Gyn. 2004, 111, 849–855. [Google Scholar] [CrossRef]
- Zeitlin, J.; Combier, E.; De Caunes, F.; Papiernik, E. Socio-demographic risk factors for perinatal mortality: A study of perinatal mortality in the French district of Seine-Saint-Denis. Acta Obstetr. Gyn. Scand. 1998, 77, 826–835. [Google Scholar] [CrossRef]
- David, M.; Pachaly, J.; Vetter, K. Perinatal outcome in Berlin (Germany) among immigrants from Turkey. Arch. Gyn. Obstetr. 2006, 274, 271–278. [Google Scholar] [CrossRef]
- Fantini, M.P.; Stivanello, E.; Dallolio, L.; Loghi, M.; Savoia, E. Persistent geographical disparities in infant mortality rates in Italy (1999–2001): Comparison with France, England, Germany, and Portugal. Eur J Public Health 2005, 16, 429–432. [Google Scholar]
- Jørgensen, T.; Mortensen, L.H.; Anderson, A.M. Social inequality in fetal and perinatal mortality in the Nordic countries. Scand. J. Public Health 2008, 36, 635–649. [Google Scholar] [CrossRef]
- Commission on Social Determinants of Health, Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008.
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health. Discussion Paper for the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Muntaner, C.; Chung, H.; Benach, J.; Ng, E. Hierarchical cluster analysis of labour market regulations and population health: A taxonomy of low- and middle-income countries. BMC Public Health 2012, 12, 286. [Google Scholar] [CrossRef]
- Chung, H.; Muntaner, C. Political and welfare state determinants of infant and child health indicators: An analysis of wealthy countries. Soc. Sci. Med. 2006, 63, 829–842. [Google Scholar] [CrossRef]
- Bezo, B.; Maggi, S.; Roberts, W.L. The rights and freedoms gradient of health: Evidence from a cross-national study. Front. Psychol. 2012, 3, 441. [Google Scholar] [CrossRef]
- Dubay, L.; Joyce, T.; Kaestner, R.; Kenney, G.M. Changes in prenatal care timing and low birth weight by race and socioeconomic status: Implications for the Medicaid expansions for pregnant women. Health Serv. Res. 2001, 36, 373–398. [Google Scholar]
- Haas, J.S.; Udvarhelyi, I.S.; Morris, C.N.; Epstein, A.M. The effect of providing health coverage to poor uninsured pregnant women in Massachusetts. JAMA 1993, 269, 87–91. [Google Scholar] [CrossRef]
- Hueston, W.J.; Gilbert, G.E.; Davis, L.; Sturgill, V. Delayed prenatal care and the risk of low birth weight delivery. J. Community Health 2003, 28, 199–208. [Google Scholar] [CrossRef]
- Phillippi, J.C. Women’s perceptions of access to prenatal care in the United States: A literature review. J. Midwifery Womens Health 2009, 54, 219–225. [Google Scholar] [CrossRef]
- Robert Wood Johnson Foundation Commission to Build a Healthier America, Beyond Health Care: New Directions to a Healthier America; Robert Wood Johnson Foundation: Princeton, NJ, USA, 2009.
- Rodgers, G.B. Income inequality as determinants of mortality: An international cross section analysis. Pop. Studies 1979, 33, 343–351. [Google Scholar]
- Ensor, T.; Cooper, S.; Davidson, L.; Fitzmaurice, A.; Graham, W.J. The impact of economic recession on maternal and infant mortality: Lessons from history. BMC Public Health 2010, 10, 727. [Google Scholar] [CrossRef] [Green Version]
- Wennemo, I. Infant-mortality, public policy, and inequality—A comparison of 18 industrialized countries 1950–85. Soc. Health Illness 1993, 15, 429–446. [Google Scholar] [CrossRef]
- Macinko, J.; Shi, L.; Starfield, B. Wage inequality, health care, and infant mortality in 19 industrialized countries. Soc. Sci. Med. 2004, 58, 279–292. [Google Scholar] [CrossRef]
- Muntaner, C.; Lynch, J.W.; Hillemeier, M.; Lee, J.H.; David, R.; Benach, J.; Borrell, C. Economic inequality, working class power, social capital, and cause-specific mortality in wealthy countries. Int. J. Health Services 2002, 32, 629–656. [Google Scholar] [CrossRef]
- Lynch, J.W.; Smith, G.D.; Hillemeier, M.; Shaw, M.; Raghunathan, T.; Kaplan, G.A. Income inequality, the psychosocial environment, and health: Comparisons of wealthy nations. Lancet 2001, 358, 194–200. [Google Scholar] [CrossRef]
- Ruhm, C.J. Parental leave and child health. J. Health Econ. 2000, 19, 931–960. [Google Scholar] [CrossRef]
- Hales, S.; Howden-Chapman, P.; Salmond, C.; Woodward, A.; Mackenbach, J. National infant mortality rates in relation to gross national product and distribution of income. Lancet 1999, 354, 2047. [Google Scholar] [CrossRef]
- McIsaac, S.; Wilkinson, R.G. Income distribution and cause-specific mortality. Eur. J. Public HealIth 1997, 7, 45–53. [Google Scholar] [CrossRef]
- Waldmann, R.J. Income-distribution and infant-mortality. Quart. J. Econ. 1992, 107, 1283–1302. [Google Scholar] [CrossRef]
- Pampel, F.C.; Pillai, V.K. Patterns and determinants of infant mortality in developed nations, 1950–1975. Demography 1986, 23, 525–542. [Google Scholar] [CrossRef]
- Leigh, A.; Jencks, C. Inequality and mortality: Long-run evidence from a panel of countries. J. Health Econ. 2007, 26, 1–24. [Google Scholar] [CrossRef]
- Kennelly, B.; O’Shea, E.; Garvey, E. Social capital, life expectancy and mortality: A cross-national examination. Soc. Sci. Med. 2003, 56, 2367–2377. [Google Scholar] [CrossRef]
- Wildman, J.; Gravelle, H.; Sutton, M. Health and income inequality: Attempting to avoid the aggregation problem. Applied Econ. 2003, 35, 999–1004. [Google Scholar] [CrossRef]
- Mellor, J.M.; Milyo, J. Reexamining the evidence of an ecological association between income inequality and health. J. Health Politics Policy Law 2001, 26, 487–522. [Google Scholar] [CrossRef]
- Judge, K.; Muligan, J.A.; Benzeval, M. Income inequality and population health. Soc. Sci. Med. 1998, 46, 567–579. [Google Scholar] [CrossRef]
- Heymann, J.; Raub, A.; Earle, A. Creating and using new data sources to analyze the relationship between social policy and global health: The case of maternal leave. Public Health Rep. 2011, 126 (Suppl. 3), 127–134. [Google Scholar]
- Bradley, E.H.; Elkins, B.R.; Herrin, J.; Elbel, B. Health and social services expenditures: Associations with health outcomes. BMJ Qual. Saf. 2011, 20, 826–831. [Google Scholar] [CrossRef]
- Filmer, D.; Pritchett, L. The impact of public spending on health: Does money matter? Soc. Sci. Med. 1999, 49, 1309–1323. [Google Scholar] [CrossRef]
- Janevic, T.; Stein, C.R.; Savitz, D.A.; Kaufman, J.S.; Mason, S.M.; Herring, A.H. Neighbourhood deprivation and adverse birth outcomes among diverse ethnic groups. Ann. Epidemiol. 2010, 20, 445–451. [Google Scholar] [CrossRef]
- Holzman, C.; Eyster, J.; Kleyn, M.; Messer, L.C.; Kaufman, J.S.; Laraia, B.A.; O’Campo, P.; Burke, J.G.; Culhane, J.; Elo, I.T. Maternal weathering and risk of preterm delivery. Am. J. Public Health 2009, 99, 1864–1871. [Google Scholar] [CrossRef]
- O’Campo, P.; Burke, J.G.; Culhane, J.; Elo, I.T.; Eyster, J.; Holzman, C.; Messer, L.C.; Kaufman, J.S.; Laraia, B.A. Neighbourhood deprivation and preterm birth among non-Hispanic Black and White women in eight geographic areas in the United States. Am. J. Epidemiol. 2008, 15, 155–163. [Google Scholar]
- Williams, B.L.; Pennock-Roman, M.; Suen, H.K.; Magsumbol, M.S.; Ozdenerol, E. Assessing the impact of the local environment on birth outcomes: A case for HLM. J. Expo. Sci. Environ. Epidemiol. 2007, 17, 445–457. [Google Scholar] [CrossRef]
- Currie, J.; Moretti, E. Biology as destiny? Short- and long-run determinants of intergenerational transmission of birth weight. J. Labor Econ. 2007, 25, 231–263. [Google Scholar] [CrossRef]
- Masi, C.M.; Hawkley, L.C.; Piotrowski, Z.H.; Pickett, K.E. Neighbourhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Soc. Sci. Med. 2007, 65, 2440–2457. [Google Scholar] [CrossRef]
- Farley, T.A.; Mason, K.; Rice, J.; Habel, J.D.; Scribner, R.; Cohen, D.A. The relationship between the neighbourhood environment and adverse birth outcomes. Paediatr. Perinat. Epidemiol. 2006, 20, 188–200. [Google Scholar] [CrossRef]
- Grady, S.C. Racial disparities in low birth weight and the contribution of residential segregation: A multilevel analysis. Soc. Sci. Med. 2006, 63, 3013–3029. [Google Scholar] [CrossRef]
- Messer, L.C.; Kaufman, J.S.; Dole, N.; Savitz, D.A.; Laraia, B.A. Neighbourhood crime, deprivation, and preterm birth. Ann. Epidemiol. 2006, 16, 455–462. [Google Scholar] [CrossRef]
- Subramanian, S.V.; Chen, J.T.; Rehkopf, D.H.; Waterman, P.D.; Krieger, N. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: A multilevel analysis of Massachusetts births, 1989–1991. Am. J. Epidemiol. 2006, 164, 823–834. [Google Scholar] [CrossRef]
- Krieger, N.; Chen, J.T.; Waterman, P.D.; Rehkopf, D.H.; Subramanian, S.V. Painting a truer picture of U.S. socioeconomic and racial/ethnic health inequalities: The Public Health Disparities Geocoding Project. Am. J. Public Health 2005, 95, 312–323. [Google Scholar] [CrossRef]
- Reagan, P.B.; Salsberry, P.J. Race and ethnic differences in determinants of preterm birth in the USA: Broadening the social context. Soc. Sci. Med. 2005, 60, 2217–2228. [Google Scholar] [CrossRef]
- Buka, S.L.; Brennan, R.T.; Rich-Edwards, J.W.; Raudenbush, S.W.; Earls, F. Neighbourhood support and the birth weight of urban infants. Am. J. Epidemiol. 2003, 157, 1–8. [Google Scholar] [CrossRef]
- Krieger, N.; Chen, J.T.; Waterman, P.D.; Soobader, M.J.; Subramanian, S.V.; Carson, R. Choosing area-based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (U.S.). J. Epidemiol. Community Health 2003, 57, 186–199. [Google Scholar] [CrossRef]
- Rich-Edwards, J.W.; Buka, S.L.; Brennan, R.T.; Earls, F. Diverging associations of maternal age with low birth weight for Black and White mothers. Int. J. Epidemiol. 2003, 32, 83–90. [Google Scholar] [CrossRef]
- Kaufman, J.S.; Dole, N.; Savitz, D.A.; Herring, A.H. Modeling community-level effects on preterm birth. Ann. Epidemiol. 2003, 13, 377–384. [Google Scholar] [CrossRef]
- Pickett, K.E.; Ahern, J.E.; Selvin, S.; Abrams, B. Neighbourhood socioeconomic status, maternal race and preterm delivery: A case-control study. Ann. Epidemiol. 2002, 12, 410–418. [Google Scholar] [CrossRef]
- Wegner, E.L.; Loos, G.P.; Onaka, A.T.; Crowell, D.; Li, Y.; Zheng, H. Changes in the association of low birth weight with socioeconomic status in Hawaii: 1970–1990. Soc. Biol. 2001, 48, 196–211. [Google Scholar]
- Rauh, V.A.; Andrews, H.F.; Garfinkel, R.S. The contribution of maternal age to racial disparities in birth weight: A multilevel perspective. Am. J. Public Health 2001, 91, 1815–1824. [Google Scholar] [CrossRef]
- Fang, J.; Madhavan, S.; Alderman, M.H. Low birth weight: Race and maternal nativity—Impact of community income. Pediatr. 1999, 103, E5:1–E5:6. [Google Scholar] [CrossRef]
- Silva, A.; Whitman, S.; Margellos, H.; Ansell, D. Evaluating Chicago’s success in reaching the Healthy People 2000 goal of reducing health disparities. Public Health Rep. 2001, 116, 484–494. [Google Scholar] [CrossRef]
- Sundquist, J.; Sundquist, K.; Johansson, S.E.; Li, X.; Winkleby, M. Mothers, places and small for gestational age births: A cohort study. Arch. Dis. Childhood 2011, 96, 380–385. [Google Scholar] [CrossRef]
- Agyemang, C.; Vrijkotte, T.G.M.; Droomers, M.; van der Wal, M.F.; Bonsel, G.J.; Stronks, K. The effect of neighbourhood income and deprivation on pregnancy outcomes in Amsterdam, The Netherlands. J. Epidemiol. Community Health 2009, 63, 755–760. [Google Scholar] [CrossRef]
- Sellström, E.; Arnoldsson, G.; Bremberg, S.; Hjern, A. Are there differences in birth weight between neighbourhoods in a Nordic welfare state? BMC Public Health 2007, 7, 267. [Google Scholar] [CrossRef]
- Dibben, C.; Sigala, M.; Macfarlane, A. Area deprivation, individual factors and low birth weight in England: Is there evidence of an “area effect”? J Epidemiol Community Health 2006, 60, 1053–1059. [Google Scholar] [CrossRef]
- Janghorbani, M.; Stenhouse, E.; Millward, A.; Jones, R.B. Neighbourhood deprivation and preterm birth in Plymouth, UK. J. Matern. Fetal Neonatal. Med. 2006, 19, 85–91. [Google Scholar] [CrossRef]
- Lasbeur, L.; Kaminski, M.; Ancel, P.-Y.; Mazaubrun, C.D.; Zeitlin, J.; Epipage Paris-Petite, C. Analysis of social inequalities in perinatal health using census data: The risk of very preterm birth in the Paris region. Population 2006, 61, 485–502. [Google Scholar] [CrossRef]
- Smith, G.C.; Shah, I.; White, I.R.; Pell, J.P.; Crossley, J.A.; Dobbie, R. Maternal and biochemical predictors of spontaneous preterm birth among nulliparous women: A systematic analysis in relation to the degree of prematurity. Int. J. Epidemiol. 2006, 35, 1169–1177. [Google Scholar] [CrossRef]
- Bundred, P.; Manning, D.; Brewster, B.; Buchan, I. Social trends in singleton births and birth weight in Wirral residents, 1990–2001. Arch. Dis. Child. Fetal Neonatal. Ed. 2003, 88, F421–F425. [Google Scholar] [CrossRef]
- Aveyard, P.; Cheng, K.K.; Manaseki, S.; Gardosi, J. The risk of preterm delivery in women from different ethnic groups. BJOG 2002, 109, 894–849. [Google Scholar] [CrossRef]
- Bonellie, S.R. Effect of maternal age, smoking and deprivation on birth weight. Pediatr. Perinat. Epidemiol. 2001, 15, 19–26. [Google Scholar] [CrossRef]
- Spencer, N.; Bambang, S.; Logan, S.; Gill, L. Socioeconomic status and birth weight: Comparison of an area-based measure with the Registrar General’s social class. J. Epidemiol. Community Health 1999, 53, 495–498. [Google Scholar] [CrossRef]
- Spencer, N.J.; Logan, S.; Gill, L. Trends and social patterning of birth weight in Sheffield, 1985–94. Arch. Dis. Child. Fetal Neonatal. Ed. 1999, 81, F138–F140. [Google Scholar] [CrossRef]
- Smith, L.K.; Draper, E.S.; Manktelow, B.N.; Dorling, J.S.; Field, D.J. Socioeconomic inequalities in very preterm birth rates. Arch. Dis. Child. Fetal Neonatal. Ed. 2007, 92, F11–F14. [Google Scholar] [CrossRef]
- Messer, L.C.; Vinikoor, L.C.; Laraia, B.A.; Kaufman, J.S.; Eyster, J.; Holzman, C.; Culhane, J.; Elo, I.; Burke, J.G.; O’Campo, P. Socioeconomic domains and associations with preterm birth. Soc. Sci. Med. 2008, 67, 1247–1257. [Google Scholar] [CrossRef]
- Collins, J.W., Jr.; Simon, D.M.; Jackson, T.A.; Drolet, A. Advancing maternal age and infant birth weight among urban African Americans: The effect of neighbourhood poverty. Ethn. Dis. 2006, 16, 180–186. [Google Scholar]
- Ahern, J.; Pickett, K.E.; Selvin, S.; Abrams, B. Preterm birth among African American and White women: A multilevel analysis of socioeconomic characteristics and cigarette smoking. J. Epidemiol. Community Health 2003, 57, 606–611. [Google Scholar] [CrossRef]
- English, P.B.; Kharrazi, M.; Davies, S.; Scalf, R.; Waller, L.; Neutra, R. Changes in the spatial pattern of low birth weight in a southern California county: The role of individual and neighbourhood level factors. Soc. Sci. Med. 2003, 56, 2073–2088. [Google Scholar] [CrossRef]
- Pearl, M.; Braveman, P.; Abrams, B. The relationship of neighbourhood socioeconomic characteristics to birth weight among 5 ethnic groups in California. Am. J. Public Health 2001, 91, 1808–1814. [Google Scholar]
- Howell, E.M.; Pettit, K.L.; Kingsley, G.T. Trends in maternal and infant health in poor urban neighbourhoods: Good news from the 1990s, but challenges remain. Public Health Rep. 2005, 120, 409–417. [Google Scholar]
- Taylor-Robinson, D.; Agarwal, U.; Diggle, P.J.; Platt, M.J.; Yoxall, B.; Alfirevic, Z. Quantifying the impact of deprivation on preterm births: A retrospective cohort study. PLoS One 2011, 6, e23163. [Google Scholar] [CrossRef]
- Zeitlin, J.; Combier, E.; Levaillant, M.; Lasbeur, L.; Pilkington, H.; Charreire, H.; Rivera, L. Neighbourhood socio-economic characteristics and the risk of preterm birth for migrant and non-migrant women: A study in a French district. Paed. Perinatal Epidemiol. 2011, 25, 347–356. [Google Scholar] [CrossRef]
- Hillemeier, M.M.; Weisman, C.S.; Chase, G.A.; Dyer, A.M. Individual and community predictors of preterm birth and low birth weight along the rural-urban continuum in central Pennsylvania. J. Rural Health 2007, 23, 42–48. [Google Scholar]
- Morenoff, J.D. Neighbourhood mechanisms and the spatial dynamics of birth weight. Am. J. Sociol. 2003, 108, 976–1017. [Google Scholar] [CrossRef]
- Young, R.L.; Weinberg, J.; Vieira, V.; Aschengrau, A.; Webster, T.F. A multilevel non-hierarchical study of birth weight and socioeconomic status. Int. J. Health Geographics 2012, 9, 36. [Google Scholar] [CrossRef]
- Jaffee, K.D.; Perloff, J.D. An ecological analysis of racial differences in low birth weight: Implications for maternal and child health social work. Health Soc. Work 2003, 28, 9–22. [Google Scholar] [CrossRef]
- Calling, S.; Li, X.; Sundquist, J.; Sundquist, K. Socioeconomic inequalities and infant mortality of 46,470 preterm infants born in Sweden between 1992 and 2006. Paed. Perinatal. Epidemiol. 2011, 25, 357–365. [Google Scholar] [CrossRef]
- Clausen, T.; Oyen, N.; Henriksen, T. Pregnancy complications by overweight and residential area. A prospective study of an urban Norwegian cohort. Acta Obstet. Gynecol. Scand. 2006, 85, 526–533. [Google Scholar] [CrossRef]
- Delpisheh, A.; Kelly, Y.; Rizwan, S.; Brabin, B.J. Socio-economic status, smoking during pregnancy and birth outcomes: An analysis of cross-sectional community studies in Liverpool (1993–2001). J. Child Health Care 2006, 10, 140–148. [Google Scholar] [CrossRef]
- Debbink, M.P.; Bader, M.D. Racial residential segregation and low birth weight in Michigan’s metropolitan areas. Am. J. Public Health 2011, 101, 1714–1720. [Google Scholar]
- Kramer, M.R.; Cooper, H.L.; Drews-Botsch, C.D.; Waller, L.A.; Hogue, C.R. Metropolitan isolation segregation and Black-White disparities in very preterm birth: A test of mediating pathways and variance explained. Soc. Sci. Med. 2010, 71, 2108–2116. [Google Scholar] [CrossRef]
- Walton, E. Residential segregation and birth weight among racial and ethnic minorities in the United States. J. Health Soc. Behav. 2009, 50, 427–442. [Google Scholar] [CrossRef]
- Bell, J.F.; Zimmerman, F.J.; Almgren, G.R.; Mayer, J.D.; Huebner, C.E. Birth outcomes among urban African-American women: A multilevel analysis of the role of racial residential segregation. Soc. Sci. Med. 2006, 63, 3030–3045. [Google Scholar] [CrossRef]
- McFarland, M.; Smith, C.A. Segregation, race, and infant well-being. Pop. Res. Policy Rev. 2011, 30, 467–493. [Google Scholar] [CrossRef]
- Lobmayer, P.; Wilkinson, R.G. Inequality, residential segregation by income, and mortality in US cities. J. Epidemiol. Community Health 2002, 56, 183–187. [Google Scholar] [CrossRef]
- Guest, A.M.; Almgren, G.; Hussey, J.M. The ecology of race and socioeconomic distress: Infant and working-age mortality in Chicago. Demography 1998, 35, 23–34. [Google Scholar] [CrossRef]
- Polednak, A. Trends in urban Black infant mortality by degree of residential segregation. Am. J. Public Health 1996, 86, 723–726. [Google Scholar] [CrossRef]
- Bird, S.T.; Bauman, K.E. The relationship between structural and health services variables and state-level infant mortality in the United States. Am. J. Public Health 1995, 85, 26–29. [Google Scholar] [CrossRef]
- Laveist, T.A. Segregation, poverty, and empowerment: Health consequences for African Americans. Milbank Q. 1993, 71, 41–64. [Google Scholar] [CrossRef]
- Polednak, A.P. Poverty, residential segregation, and Black/White mortality ratios in urban areas. J. Health Care Poor Underserved 1993, 4, 363–373. [Google Scholar] [CrossRef]
- Polednak, A.P. Black-White differences in infant mortality in 38 standard metropolitan statistical areas. Am. J. Public Health 1991, 81, 1480–1482. [Google Scholar] [CrossRef]
- LaVeist, T.A. Simulating the effects of poverty on the race disparity in post-neonatal mortality. J. Public Health Policy 1990, 11, 463–473. [Google Scholar] [CrossRef]
- LaVeist, T.A. Linking residential segregation to the infant mortality race disparity in U.S. cities. Sociol. Soc. Res. 1989, 73, 90–94. [Google Scholar]
- Yankauer, A.; Allaway, N.C. The relation of indices of fetal and infant loss to residential segregation: A follow-up report. Am. Soc. Rev. 1958, 23, 573–578. [Google Scholar] [CrossRef]
- Yankauer, A., Jr. The relationship of fetal and infant mortality to residential segregation: An inquiry into social epidemiology. Am. Soc. Rev. 1950, 15, 644–648. [Google Scholar] [CrossRef]
- Vinikoor, L.C.; Kaufman, J.S.; Maclehose, R.F.; Laraia, B.A. Effects of racial density and income incongruity on pregnancy outcomes in less segregated communities. Soc. Sci. Med. 2008, 66, 255–259. [Google Scholar] [CrossRef]
- Pickett, K.E.; Collins, J.W.; Masi, C.M.; Wilkinson, R.G. Ethnic density effects on maternal and infant health in the Millenium Cohort Study. Soc. Sci. Med. 2009, 69, 1476–1483. [Google Scholar] [CrossRef]
- Hearst, M.O.; Oakes, J.M.; Johnson, P.J. The effect of racial segregation on Black infant mortality. Am. J. Epidemiol. 2008, 168, 1247–1254. [Google Scholar] [CrossRef]
- Nkansah-Amankra, S.; Dhawain, A.; Hussey, J.R.; Luchok, K.J. Maternal social support and neighbourhood income inequality as predictors of low birth weight and preterm birth outcome disparities: Analysis of South Carolina Pregnancy Risk Assessment and Monitoring System survey, 2000–2003. Mat. Child Health J. 2010, 14, 774–785. [Google Scholar] [CrossRef]
- Olson, M.E.; Diekema, D.; Elliott, B.A.; Renier, C.M. Impact of income and income inequality on infant health outcomes in the United States. Pediatrics 2010, 126, 1165–1173. [Google Scholar]
- Sohler, N.L.; Arno, P.S. Income inequality and infant mortality in New York City. J. Urban Health 2003, 80, 650–657. [Google Scholar] [CrossRef]
- Ross, N.A.; Wolfson, M.C.; Dunn, J.R.; Berthelot, J.-M.; Kaplan, G.A.; Lynch, J.W. Relation between income inequality and mortality in Canada and in the United States: Cross sectional assessment using census data and vital statistics. Br. Med. J. 2000, 320, 898–902. [Google Scholar]
- Shi, L.; Starfield, B.; Kennedy, B.; Kawachi, I. Income inequality, primary care, and health indicators. J. Family Practice 1999, 48, 275–284. [Google Scholar]
- Kennedy, B.P.; Kawachi, I.; Prothrow-Stith, D. Income distribution and mortality: Cross sectional ecological study of the Robin Hood index in the United States. Br. Med. J. 1996, 20, 1004–1007. [Google Scholar]
- Kaplan, G.A.; Pamuk, E.R.; Lynch, J.W.; Cohen, R.D.; Balfour, J.L. Inequality in income and mortality in the United States: Analysis of mortality and potential pathways. Br. Med. J. 1996, 312, 999–1003. [Google Scholar]
- Materia, E.; Cacciani, L.; Bugarini, G.; Cesaroni, G.; Davoli, M.; Mirale, M.P.; Vergine, L.; Baglio, G.; Simeone, G.; Perucci, C.A. Income inequality and mortality in Italy. Eur. J. Public Health 2005, 15, 411–417. [Google Scholar] [CrossRef]
- Finch, B.K. Early origins of the gradient: The relationship between socioeconomic status and infant mortality in the United States. Demography 2003, 40, 675–699. [Google Scholar] [CrossRef]
- Deaton, A.; Lubotsky, D. Mortality, inequality and race in American cities and states. Soc. Sci. Med. 2003, 56, 1139–1153. [Google Scholar] [CrossRef]
- Kawachi, I.; Kennedy, B.P.; Lochner, K.; Prothrow-Stith, D. Social capital, income inequality, and mortality. Am. J. Public Health 1997, 87, 1491–1498. [Google Scholar] [CrossRef]
- Nabukera, S.K.; Wingate, M.S.; Owen, J.; Salihu, H.M.; Swaminathan, S.; Alexander, G.R.; Kirby, R.S. Racial disparities in perinatal outcomes and pregnancy spacing among women delaying initiation of childbearing. Matern. Child Health J. 2009, 13, 81–89. [Google Scholar]
- Shen, T.T.; DeFranco, E.A.; Stamilio, D.M.; Chang, J.J.; Muglia, L.J. A population based study of race-specific risk for preterm premature rupture of membranes. Am. J. Obstet. Gynecol. 2008, 199, 373:e1–373:e7. [Google Scholar]
- Ehrenthal, D.B.; Jurkovitz, C.; Hoffman, M.; Kroelinger, C.; Weintraub, W. A population study of the contribution of medical comorbidity to the risk of prematurity in Blacks. Am. J. Obstet. Gynecol. 2007, 197, 409:e1–409:e6. [Google Scholar]
- Kistka, Z.A.; Palomar, L.; Lee, K.A.; Boslaugh, S.E.; Wangler, M.F.; Cole, F.S.; DeBaun, M.R.; Muglia, L.J. Racial disparity in the frequency of recurrence of preterm birth. Am. J. Obstet. Gynecol. 2007, 196, 131:e1–131:e6. [Google Scholar]
- Buescher, P.A.; Mittal, M. Racial disparities in birth outcomes increase with maternal age: Recent data from North Carolina. North Carolina Med. J. 2006, 67, 16–20. [Google Scholar]
- Dominguez, T.P.; Schetter, C.D.; Mancuso, R.; Rini, C.M.; Hobel, C. Stress in African American pregnancies: Testing the roles of various stress concepts in prediction of birth outcomes. Ann. Behav. Med. 2005, 29, 12–21. [Google Scholar] [CrossRef]
- Dole, N.; Savitz, D.A.; Siega-Riz, A.M.; Hertz-Picciotto, I.; McMahon, M.J.; Buekens, P. Psychosocial factors and preterm birth among African American and White women in central North Carolina. Am. J. PublicHealth. 2004, 94, 1358–1365. [Google Scholar]
- Rosenberg, L.; Palmer, J.R.; Wise, L.A.; Horton, N.J.; Corwin, M.J. Perceptions of racial discrimination and the risk of preterm birth. Epidemiology 2002, 13, 646–652. [Google Scholar] [CrossRef]
- Berg, C.J.; Wilcox, L.S.; d’Almada, P.J. The prevalence of socioeconomic and behavioural characteristics and their impact on very low birth weight in Black and White infants in Georgia. Matern. Child Health J. 2001, 5, 75–84. [Google Scholar] [CrossRef]
- Adams, M.M.; Elam-Evans, L.D.; Wilson, H.G.; Gilbertz, D.A. Rates of and factors associated with recurrence of preterm delivery. J. Am. Med. Assoc. 2000, 283, 1591–1596. [Google Scholar] [CrossRef]
- Foster, H.W.; Wu, L.; Bracken, M.B.; Semenya, K.; Thomas, J.; Thomas, J. Intergenerational effects of high socioeconomic status on low birth weight and preterm birth in African Americans. J. Natl. Med. Assoc. 2000, 92, 213–221. [Google Scholar]
- Alexander, G.R.; Kogan, M.D.; Himes, J.H.; Mor, J.M.; Goldenberg, R. Racial differences in birth weight for gestational age and infant mortality in extremely low-risk US populations. Paed. Perinat. Epidemiol. 1999, 13, 205–217. [Google Scholar] [CrossRef]
- David, R.; Collins, J. Differing birth weight among infants of U.S.-born Blacks, African-born Blacks, and U.S.-born Whites. N. Engl. J. Med. 1997, 337, 1209–1214. [Google Scholar] [CrossRef]
- Singh, G.K.; Yu, S.M. Adverse pregnancy outcomes: Differences between US- and foreign-born women in major US racial and ethnic groups. Am. J. Public Health. 1996, 86, 837–843. [Google Scholar] [CrossRef]
- Schoendorf, K.C.; Hogue, C.J.; Kleinman, J.C.; Rowley, D. Mortality among infants of Black as compared with White college educated parents. N. Engl. J. Med. 1992, 326, 1522–1526. [Google Scholar] [CrossRef]
- Abrams, B.; Newman, V. Small-for-gestational age birth: Maternal predictors and comparison with risk factors of spontaneous delivery in the same cohort. Am. J. Obstet. Gynecol. 1991, 164, 785–790. [Google Scholar] [CrossRef]
- Kleinman, J.C.; Kessel, S.S. Racial differences in low birth weight: Trends and risk factors. N. Engl. J. Med. 1987, 317, 749–753. [Google Scholar] [CrossRef]
- Shiono, P.; Klebanoff, M. Ethnic differences in preterm and very preterm delivery. Am. J. Public Health. 1986, 76, 1317–1321. [Google Scholar] [CrossRef]
- Reeske, A.; Kutschmann, M.; Razum, O.; Spallek, J. Stillbirth differences according to regions of origin: An analysis of the German perinatal database, 2004–2007. BMC Pregn. Childbirth 2011, 11, 63. [Google Scholar] [CrossRef]
- Kelly, Y.; Panico, L.; Bartley, M.; Marmot, M.; Nazroo, J.; Sacker, A. Why does birth weight vary among ethnic groups in the UL? Findings from the Millennium Cohort Study. J. Public Health 2008, 31, 131–137. [Google Scholar] [CrossRef]
- Essén, B.; Hanson, B.S.; Östergren, P.O.; Lindquist, P.G.; Gudmundsson, S. Increased perinatal mortality among sub-Saharan immigrants in a city-population in Sweden. Acta Obstetr. Gyn. Scand. 2000, 79, 737–743. [Google Scholar]
- Vangen, S.; Stoltenberg, C.; Elise, R.; Sundby, J.; Stray-Pedersen, B. Perinatal complications among ethnic Somalis in Norway. Acta Obstetr. Gyn. Scand. 2002, 81, 317–322. [Google Scholar] [CrossRef]
- Collins, J.W., Jr.; David, R.J.; Handler, A.; Wall, S.; Andes, S. Very low birth weight in African American infants: The role of maternal exposure to interpersonal racial discrimination. Am. J. Public Health. 2004, 94, 2132–2138. [Google Scholar] [CrossRef]
- Mustillo, S.; Krieger, N.; Gunderson, E.P.; Sidney, S.; McCreath, H.; Kiefe, C.I. Self-reported experiences of racial discrimination and Black-White differences in preterm and low birth weight deliveries: the CARDIA Study. Am. J. Public Health 2004, 94, 2125–2131. [Google Scholar] [CrossRef]
- Collins, J.W., Jr.; David, R.J.; Symons, R.; Handler, A.; Wall, S.N.; Dwyer, L. Low-income African-American mothers’ perception of exposure to racial discrimination and infant birth weight. Epidemiology 2000, 11, 337–339. [Google Scholar] [CrossRef]
- Goldenberg, R.L.; Iams, J.D.; Mercer, B.M.; Meis, P.J.; Moawad, A.H.; Copper, R.L.; Das, A.; Thom, E.; Johnson, F.; McNellis, D. The preterm prediction study: The value of new vs. standard risk factors in predicting early and all spontaneous preterm births. NICHD MFMU Network. Am. J. Public Health. 1998, 88, 233–238. [Google Scholar] [CrossRef]
- Dailey, D.E. Social stressors and strengths as predictors of infant birth weight in low-income African American women. Nurs. Res. 2009, 58, 340–347. [Google Scholar] [CrossRef]
- Korte, J.E. Psychosocial Stress and Its Relationship to Weight for Gestational Age and Gestational Age at Delivery. Ph.D. Thesis, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, May 1999. [Google Scholar]
- Shiono, P.H.; Rauh, V.A.; Park, M.; Lederman, S.A.; Zuskar, D. Ethnic differences in birth weight: The role of lifestyle and other factors. Am. J. Public Health. 1997, 87, 787–793. [Google Scholar] [CrossRef]
- Murrell, N.L. Stress, self-esteem, and racism: Relationships with low birth weight and preterm delivery in African American women. J. Natl. Black Nurses Assoc. 1996, 8, 45–53. [Google Scholar]
- Acevedo-Garcia, D.; Soobader, M.J.; Berkman, L.F. Low birth weight among U.S. Hispanic/Latino subgroups: The effect of maternal foreign-born status and education. Soc. Sci. Med. 2007, 65, 2503–2516. [Google Scholar] [CrossRef]
- Astone, N.M.; Misra, D.; Lynch, C. The effect of maternal socio-economic status throughout the lifespan on infant birth weight. Pediatr. Perinat. Epidemiol. 2007, 21, 310–318. [Google Scholar] [CrossRef]
- El Reda, D.K.; Grigorescu, V.; Posner, S.F.; Davis-Harrier, A. Lower rates of preterm birth in women of Arab ancestry: An epidemiologic paradox—Michigan, 1993–2002. Matern. Child Health J. 2007, 11, 622–627. [Google Scholar] [CrossRef]
- Colen, C.G.; Geronimus, A.T.; Bound, J.; James, S.A. Maternal upward socioeconomic mobility and Black-White disparities in infant birth weight. Am. J. Public Health. 2006, 96, 2032–2039. [Google Scholar] [CrossRef]
- Goldman, N.; Kimbro, R.T.; Turra, C.M.; Pebley, A.R. Socioeconomic gradients in health for White and Mexican-origin populations. Am. J. Public Health. 2006, 96, 2186–2193. [Google Scholar] [CrossRef]
- Madan, A.; Palaniappan, L.; Urizar, G.; Wang, Y.; Fortmann, S.P.; Gould, J.B. Sociocultural factors that affect pregnancy outcomes in two dissimilar immigrant groups in the U.S. J. Pediatr. 2006, 148, 341–346. [Google Scholar] [CrossRef]
- Messer, L.C.; Laraia, B.A.; Kaufman, J.S.; Eyster, J.; Holzman, C.; Culhane, J.; Elo, I.; Burke, J.G.; O’Campo, P. The development of a standardized neighbourhood deprivation index. J. Urban Health 2006, 83, 1041–1062. [Google Scholar] [CrossRef]
- Acevedo-Garcia, D.; Soobader, M.J.; Berkman, L.F. The differential effect of foreign-born status on low birth weight by race/ethnicity and education. Pediatrics 2005, 115, e20–e30. [Google Scholar]
- Ponce, N.A.; Hoggatt, K.J.; Wilhelm, M.; Ritz, B. Preterm birth: The interaction of traffic-related air pollution with economic hardship in Los Angeles neighbourhoods. Am. J. Epidemiol. 2005, 162, 140–148. [Google Scholar] [CrossRef]
- Nicolaidis, C.; Ko, C.W.; Saha, S.; Koepsell, T.D. Racial discrepancies in the association between paternal vs. maternal educational level and risk of low birth weight in Washington State. BMC Pregnancy Childbirth 2004, 4, 10. [Google Scholar] [CrossRef] [Green Version]
- Savitz, D.A.; Kaufman, J.S.; Dole, N.; Siega-Riz, A.M.; Thorp, J.M., Jr; Kaczor, D.T. Poverty, education, race, and pregnancy outcome. Ethn. Dis. 2004, 14, 322–329. [Google Scholar]
- Steward, D.K.; Moser, D.K. Intrauterine growth retardation in full-term newborn infants with birth weights greater than 2,500 g. Res. Nurs. Health 2004, 27, 403–412. [Google Scholar] [CrossRef]
- Gould, J.B.; Madan, A.; Qin, C.; Chavez, G. Perinatal outcomes in two dissimilar immigrant populations in the U.S.: A dual epidemiologic paradox. Pediatrics 2003, 111, e676–e682. [Google Scholar] [CrossRef]
- Abrevaya, J. The effects of demographics and maternal behaviour on the distribution of birth outcomes. Empirical Econ. 2001, 26, 247–257. [Google Scholar] [CrossRef]
- Rolett, A.; Kiely, J.L. Maternal sociodemographic characteristics as risk factors for preterm birth in twins versus singletons. Paediatr. Perinat. Epidemiol. 2000, 14, 211–218. [Google Scholar] [CrossRef]
- Shmueli, A.; Cullen, M.R. Birth weight, maternal age, and education: New observations from Connecticut and Virginia. Yale J. Biol. Med. 1999, 72, 245–258. [Google Scholar]
- Gorman, B.K. Racial and ethnic variation in low birth weight in the U.S.: Individual and contextual determinants. Health Place 1999, 5, 195–207. [Google Scholar] [CrossRef]
- du Prel, X.; Kramer, U.; Behrendt, H.; Ring, J.; Oppermann, H.; Schikowski, T.; Ranft, U. Preschool children’s health and its association with parental education and individual living conditions in East and West Germany. BMC Public Health 2006, 6, 312. [Google Scholar] [CrossRef]
- Gisselmann, M.D. The influence of maternal childhood and adulthood social class on the health of the infant. Soc. Sci. Med. 2006, 63, 1023–1033. [Google Scholar]
- Reime, B.; Ratner, P.A.; Tomaselli-Reime, S.N.; Kelly, A.; Schuecking, B.A.; Wenzlaff, P. The role of mediating factors in the association between social deprivation and low birth weight in Germany. Soc. Sci. Med. 2006, 62, 1731–1744. [Google Scholar] [CrossRef]
- Fairley, L. Changing patterns of inequality in birth weight and its determinants: A population-based study, Scotland 1980–2000. Paediatr. Perinat. Epidemiol. 2005, 19, 342–351. [Google Scholar]
- Thompson, J.M.; Irgens, L.M.; Rasmussen, S.; Daltveit, A.K. Secular trends in socio-economic status and the implications for preterm birth. Paediatr. Perinat. Epidemiol. 2006, 20, 182–187. [Google Scholar] [CrossRef]
- Spencer, N.J. Accounting for the social disparity in birth weight: Results from an intergenerational cohort. J. Epidemiol. Community Health 2004, 58, 418–419. [Google Scholar]
- Gissler, M.; Merilainen, J.; Vuori, E.; Hemminki, E. Register based monitoring shows decreasing socioeconomic differences in Finnish perinatal health. J. Epidemiol. Community Health 2003, 57, 433–439. [Google Scholar] [CrossRef]
- Ronda, E.; Regidor, E. Higher birth weight and lower prevalence of low birth weight in children of agricultural workers than in those of workers in other occupations. J. Occup. Environ. Med. 2003, 45, 34–40. [Google Scholar] [CrossRef]
- Moser, K.; Li, L.; Power, C. Social inequalities in low birth weight in England and Wales: Trends and implications for future population health. J. Epidemiol. Community Health. 2003, 57, 687–691. [Google Scholar] [CrossRef]
- Raum, E.; Arabin, B.; Schlaud, M.; Walter, U.; Schwartz, F.W. The impact of maternal education on intrauterine growth: A comparison of former West and East Germany. Int. J. Epidemiol. 2001, 30, 81–87. [Google Scholar] [CrossRef]
- Ancel, P.Y.; Saurel-Cubizolles, M.J.; Di Renzo, G.C.; Papiernik, E.; Breart, G. Very and moderate preterm births: Are the risk factors different? Br. J. Obstet. Gynaecol. 1999, 106, 1162–1170. [Google Scholar] [CrossRef]
- Basso, O.; Olsen, J.; Christensen, K. Study of environmental, social, and paternal factors in preterm delivery using sibs and half sibs: A population-based study in Denmark. J. Epidemiol. Community Health 1999, 53, 20–23. [Google Scholar] [CrossRef]
- Blumenshine, P.M.; Egerter, S.A.; Libet, M.L.; Braveman, P.A. Father’s education: An Independent Marker of Risk for Preterm Birth. Matern. Child Health J. 2011, 15, 60–67. [Google Scholar]
- Reagan, P.B.; Salsberry, P.J.; Olsen, R.J. Does the measure of economic disadvantage matter? Exploring the effect of individual and relative deprivation on intrauterine growth restriction. Soc. Sci. Med. 2007, 64, 2016–2129. [Google Scholar] [CrossRef]
- Finch, B.K. Socioeconomic gradients and low birth weight: Empirical and policy considerations. Health Serv. Res. 2003, 38, 1819–1841. [Google Scholar] [CrossRef]
- Braveman, P.; Cubbin, C.; Marchi, K.; Egerter, S.; Chavez, G. Measuring socioeconomic status/position in studies of racial/ethnic disparities: Maternal and infant health. Public Health Rep. 2001, 116, 449–463. [Google Scholar]
- Conley, D.; Bennett, N.G. Is biology destiny? Birth weight and life chances. Am. Sociol. Rev. 2000, 65, 458–467. [Google Scholar] [CrossRef]
- Parker, J.D.; Schoendorf, K.C.; Kiely, J.L. Associations between measures of socioeconomic status and low birth weight, small for gestational age, and premature delivery in the United States. Ann. Epidemiol. 1994, 4, 271–278. [Google Scholar]
- Nobile, C.G.; Raffaele, G.; Altomare, C.; Pavia, M. Influence of maternal and social factors as predictors of low birth weight in Italy. BMC Public Health. 2007, 7, 192. [Google Scholar] [CrossRef]
- Voigt, M.; Heineck, G.; Hesse, V. The relationship between maternal characteristics, birth weight and preterm delivery: Evidence from Germany at the end of the 20th century. Econ. Hum. Biol. 2004, 2, 265–280. [Google Scholar] [CrossRef]
- Grimmer, I.; Buhrer, C.; Dudenhausen, J.W.; Stroux, A.; Reiher, H.; Halle, H.; Obladen, M. Preconceptional factors associated with very low birth weight delivery in East and West Berlin: A case-control study. BMC Public Health 2002, 2, 10. [Google Scholar] [CrossRef] [Green Version]
- Lekea-Karanika, V.; Tzoumaka-Bakoula, C.; Matsaniotis, N.S. Sociodemographic determinants of low birth weight in Greece: A population study. Paediatr. Perinat. Epidemiol. 1999, 13, 65–77. [Google Scholar]
- Misra, D.P.; O’Campo, P.; Strobino, D. Testing a sociomedical model for preterm delivery. Paediatr. Perinat. Epidemiol. 2001, 15, 110–122. [Google Scholar]
- Longo, D.R.; Kruse, R.L.; LeFevre, M.L.; Schramm, W.F.; Stockbauer, J.W.; Howell, V. An investigation of social and class differences in very-low birth weight outcomes: A continuing public health concern. J. Health Care Finance 1999, 25, 75–89. [Google Scholar]
- Villalbi, J.R.; Salvador, J.; Cano-Serral, G.; Rodriguez-Sanz, M.C.; Borrell, C. Maternal smoking, social class and outcomes of pregnancy. Paediatr. Perinat. Epidemiol. 2007, 21, 441–447. [Google Scholar]
- Dejin-Karlsson, E.; Ostergren, P.O. Country of origin, social support and the risk of small for gestational age birth. Scand. J. Public Health. 2004, 32, 442–449. [Google Scholar]
- Skórzyńska, H.; Rudnicka-Drozak, E. Social and medical factors of risk of premature births and prematurity. Annales Universitatis Mariae Curie-Sklodowska 1999, 54, 345–350. [Google Scholar]
- Vagero, D.; Koupilova, I.; Leon, D.A.; Lithell, U.B. Social determinants of birth weight, ponderal index and gestational age in Sweden in the 1920s and the 1980s. Acta Paediatr. 1999, 88, 445–453. [Google Scholar]
- Lobel, M.; Cannella, L.; Graham, J.E.; DeVincent, C.; Schneider, J.; Meyer, B.A. Pregnancy-specific stress, prenatal health behaviours, and birth outcomes. Health Psychol. 2008, 27, 604–615. [Google Scholar]
- Orr, S.T.; James, S.A.; Miller, C.A.; Barakat, B.; Daikoku, M.; Pupkin, M.; Engstrom, K.; Huggins, G. Psychosocial stressors and low birth weight in an urban population. Am. J. Prev. Med. 1996, 12, 459–466. [Google Scholar]
- Doucette, J.T.; Bracken, M.B. Possible role of asthma in the risk of preterm labor and delivery. Epidemiology 1993, 4, 143–150. [Google Scholar]
- Shiono, P.H.; Klebanoff, M.A.; Rhoads, G.G. Smoking and drinking during pregnancy. Their effects on preterm birth. JAMA 1986, 255, 82–84. [Google Scholar]
- van den Berg, B.J.; Oechsli, F.W. Prematurity. In Perinatal Epidemiology; Bracken, M.B., Ed.; Oxford University Press: New York, NY, USA, 1984. [Google Scholar]
- Frazier, T.M.; Davis, G.H.; Goldstein, H.; Goldberg, I.D. Cigarette smoking and prematurity: A prospective study. Am. J. Obstet. Gynecol. 1961, 81, 988–996. [Google Scholar]
- Wisborg, K.; Henriksen, T.B.; Hedegaard, M.; Secher, N.J. Smoking during pregnancy and preterm birth. Br. J. Obstet. Gynaecol. 1996, 103, 800–805. [Google Scholar]
- Henriksen, T.B.; Wilcox, A.J.; Hedegaard, M.; Secher, N.J. Bias in studies of preterm and postterm delivery due to ultrasound assessment of gestational age. Epidemiology 1995, 6, 533–537. [Google Scholar]
- Ahlborg, G., Jr.; Bodin, L. Tobacco smoke exposure and pregnancy outcome among working women: A prospective study at prenatal care centers in Orebro County, Sweden. Am. J. Epidemiol. 1991, 133, 338–347. [Google Scholar]
- Stein, A.; Campbell, E.A.; Day, A.; McPherson, K.; Cooper, P.J. Social adversity, low birth weight, and preterm delivery. BMJ 1987, 295, 291–293. [Google Scholar] [CrossRef]
- Obel, E.B. Pregnancy complications following legally induced abortion: an analysis of the population with special reference to prematurity. Dan. Med. Bull. 1979, 26, 192–199. [Google Scholar]
- Russell, C.S.; Taylor, R.; Law, C.E. Smoking in pregnancy, maternal blood pressure, pregnancy outcome, baby weight and growth, and other related factors: A prospective study. Br. J. Prev. Soc. Med. 1968, 22, 119–126. [Google Scholar]
- Siega-Riz, A.M.; Adair, L.S.; Hobel, C.J. Maternal underweight status and inadequate rate of weight gain during the third trimester of pregnancy increases the risk of preterm delivery. J. Nutr. 1996, 126, 146–153. [Google Scholar]
- Wen, S.W.; Goldenberg, R.L.; Cutter, G.R.; Hoffman, H.J.; Cliver, S.P. Intrauterine growth retardation and preterm delivery: Prenatal risk factors in an indigent population. Am. J. Obstet. Gynecol. 1990, 162, 213–218. [Google Scholar]
- Naeye, R.L. Factors that predispose to premature rupture of the fetal membranes. Obstet. Gynecol. 1982, 60, 93–98. [Google Scholar]
- Rush, D.; Kass, E.H. Maternal smoking: A reassessment of the association with perinatal mortality. Am. J. Epidemiol. 1972, 96, 183–196. [Google Scholar]
- Yerushalmy, J. Mother’s cigarette smoking and survival of the infant. Am. J. Obstet. Gynecol. 1964, 88, 505–518. [Google Scholar]
- Nordentoft, M.; Lou, H.C.; Hansen, D.; Nim, J.; Pryds, O.; Rubin, P.; Hemmingsen, R. Intrauterine growth retardation and premature delivery: The influence of maternal smoking and psychosocial factors. Am. J. Public Health 1996, 86, 347–354. [Google Scholar]
- Peacock, J.L.; Bland, J.M.; Anderson, H.R. Preterm delivery: Effects of socioeconomic factors, psychological stress, smoking, alcohol, and caffeine. BMJ 1995, 311, 531–535. [Google Scholar] [CrossRef]
- Donovan, J.W. Randomised controlled trial of anti-smoking advice in pregnancy. Br. J. Prev. Soc. Med. 1977, 31, 6–12. [Google Scholar]
- Glynn, L.M.; Dunkel-Schetter, C.; Hobel, C.J.; Sandman, C.A. Pattern of perceived stress and anxiety in pregnancy predicts preterm birth. Health Psychol. 2008, 27, 43–51. [Google Scholar]
- Stinson, J.C.; Lee, K.A. Premature labor and birth: Influence of rank and perception of fatigue in active duty military women. Mil. Med. 2003, 168, 385–389. [Google Scholar]
- Orr, S.T.; James, S.A.; Blackmore Prince, C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am. J. Epidemiol. 2002, 156, 797–802. [Google Scholar]
- Wadhwa, P.D.; Sandman, C.A.; Porto, M.; Dunkel-Schetter, C.; Garite, T.J. The association between prenatal stress and infant birth weight and gestational age at birth: A prospective investigation. Am. J. Obstet. Gynecol. 1993, 169, 858–865. [Google Scholar]
- Reeb, K.G.; Graham, A.V.; Zyzanski, S.J.; Kitson, G.C. Predicting low birth weight and complicated labor in urban Black women: A biopsychosocial perspective. Soc. Sci. Med. 1987, 25, 1321–1327. [Google Scholar]
- Wisner, K.L.; Sit, D.K.; Hanusa, B.H.; Moses-Kolko, E.L.; Bogen, D.L.; Hunker, D.F.; Perel, J.M.; Jones-Ivy, S.; Bodnar, L.M.; Singer, L.T. Major depression and antidepressant treatment: Impact on pregnancy and neonatal outcomes. Am. J. Psychiatry 2009, 166, 557–566. [Google Scholar]
- Neggers, Y.; Goldenberg, R.; Cliver, S.; Hauth, J. The relationship between psychosocial profile, health practices, and pregnancy outcomes. Acta. Obstet. Gynecol. Scand. 2006, 85, 277–285. [Google Scholar] [CrossRef]
- Jesse, D.E.; Seaver, W.; Wallace, D.C. Maternal psychosocial risks predict preterm birth in a group of women from Appalachia. Midwifery 2003, 19, 191–202. [Google Scholar]
- Zimmer-Gembeck, M.J.; Helfand, M. Low birth weight in a public prenatal care program behavioural and psychosocial risk factors and psychosocial intervention. Soc. Sci. Med. 1996, 43, 187–197. [Google Scholar]
- Steer, R.A.; Scholl, T.O.; Hediger, M.L.; Fischer, R.L. Self-reported depression and negative pregnancy outcomes. J. Clin. Epidemiol. 1992, 45, 1093–1099. [Google Scholar]
- Class, Q.A.; Lichtenstein, P.; Långström, N.; D’Onofrio, B.M. Timing of prenatal maternal exposure to severe life events and adverse pregnancy outcomes: A population study of 2.6 million pregnancies. Psychosomatic Med. 2011, 73, 234–241. [Google Scholar] [CrossRef]
- Martini, J.; Knappe, S.; Beesdo-Baum, K.; Lieb, R.; Wittchen, H.U. Anxiety disorders before birth and self-perceived distress during pregnancy: Associations with maternal depression and obstetric, neonatal and early childhood outcomes. Early Hum. Dev. 2010, 86, 305–310. [Google Scholar]
- Khashan, A.S.; McNamee, R.; Abel, K.M.; Mortensen, P.B.; Kenny, L.C.; Pedersen, M.G.; Webb, R.T.; Baker, P.N. Rates of preterm birth following antenatal maternal exposure to severe life events: A population-based cohort study. Hum Reprod. 2009, 24, 429–437. [Google Scholar] [CrossRef]
- Hedegaard, M.; Henriksen, T.B.; Secher, N.J.; Hatch, M.C.; Sabroe, S. Do stressful life events affect duration of gestation and risk of preterm delivery? Epidemiology 1996, 7, 339–345. [Google Scholar] [CrossRef]
- Dayan, J.; Creveuil, C.; Marks, M.N.; Conroy, S.; Herlicoviez, M.; Dreyfus, M.; Tordjman, S. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: A prospective cohort study among women with early and regular care. Psychosom. Med. 2006, 68, 938–946. [Google Scholar] [CrossRef]
- Dayan, J.; Creveuil, C.; Herlicoviez, M.; Herbel, C.; Baranger, E. Antenatal depression, a risk factor for prenatal delivery. Presse Med. 1999, 28, 1698. [Google Scholar]
- Hedegaard, M.; Henriksen, T.B.; Sabroe, S.; Secher, N.J. Psychological distress in pregnancy and preterm delivery. BMJ 1993, 307, 234–239. [Google Scholar]
- Kramer, M.S.; Lydon, J.; Seguin, L.; Goulet, L.; Kahn, S.R.; McNamara, H.; Genest, J.; Dassa, C.; Chen, M.F.; Sharma, S.; et al. Stress pathways to spontaneous preterm birth: The role of stressors, psychological distress, and stress hormones. Am. J. Epidemiol. 2009, 169, 1319–1326. [Google Scholar] [CrossRef]
- Strange, L.B. Sleep patterns of women at risk for the development of preterm labor. Diss. Abstr. Int. 2004, 65, 665B. [Google Scholar]
- James, T.D. The effects of chronic stress on the duration of pregnancy. Diss. Abstr. Int. 2000, 61, 2472B. [Google Scholar]
- Diego, M.A.; Field, T.; Hernandez-Reif, M.; Schanberg, S.; Kuhn, C.; Gonzalez-Quintero, V.H. Prenatal depression restricts fetal growth. Early Hum. Dev. 2009, 85, 65–70. [Google Scholar]
- Gavin, A.R.; Holzman, C.; Siefert, K.; Tian, Y. Maternal depressive symptoms, depression, and psychiatric medication use in relation to risk of preterm delivery. Womens Health Issues 2009, 19, 325–334. [Google Scholar] [CrossRef]
- Li, D.; Liu, L.; Odouli, R. Presence of depressive symptoms during early pregnancy and the risk of preterm delivery: A prospective cohort study. Hum. Reprod. 2009, 24, 146–153. [Google Scholar]
- Suri, R.; Altshuler, L.; Hellemann, G.; Burt, V.K.; Aquino, A.; Mintz, J. Effects of antenatal depression and antidepressant treatment on gestational age at birth and risk of preterm birth. Am. J. Psychiatry 2007, 164, 1206–1213. [Google Scholar]
- Haas, J.S.; Fuentes-Afflick, E.; Stewart, A.L.; Jackson, R.A.; Dean, M.L.; Brawarsky, P.; Escobar, G.J. Prepregnancy health status and the risk of preterm delivery. Arch. Pediatr. Adolesc. Med. 2005, 159, 58–63. [Google Scholar]
- Dole, N.; Savitz, D.A.; Hertz-Picciotto, I.; Siega-Riz, A.M.; McMahon, M.J.; Buekens, P. Maternal stress and preterm birth. Am. J. Epidemiol. 2003, 157, 14–24. [Google Scholar]
- Hoffman, S.; Hatch, M.C. Depressive symptomatology during pregnancy: Evidence for an association with decreased fetal growth in pregnancies of lower social class women. Health Psychol. 2000, 19, 535–543. [Google Scholar]
- Copper, R.L.; Goldenberg, R.L.; Das, A.; Elder, N.; Swain, M.; Norman, G.; Ramsey, R.; Cotroneo, P.; Collins, B.A.; Johnson, F.; et al. The preterm prediction study: Maternal stress is associated with spontaneous preterm birth at less than thirty-five weeks’ gestation. Am. J. Obstet. Gynecol. 1996, 175, 1286–1292. [Google Scholar] [CrossRef]
- Perkin, M.R.; Bland, J.M.; Peacock, J.L.; Anderson, H.R. The effect of anxiety and depression during pregnancy on obstetric complications. Br. J. Obstet. Gynaecol. 1993, 100, 629–634. [Google Scholar]
- Krabbendam, L.; Smits, L.; de Bie, R.; Bastiaanssen, J.; Stelma, F.; van Os, J. The impact of maternal stress on pregnancy outcome in a well-educated Caucasian population. Paediatr. Perinat. Epidemiol. 2005, 19, 421–425. [Google Scholar]
- Henriksen, T.B.; Hedegaard, M.; Secher, N.J. The relation between psychosocial job strain, and preterm delivery and low birth weight for gestational age. Int. J. Epidemiol. 1994, 23, 764–774. [Google Scholar]
- Elsenbruch, S.; Benson, S.; Rücke, M.; Rose, M.; Dudenhausen, J.; Pincus-Knackstedt, M.K.; Klapp, B.F.; Arck, P.C. Social support during pregnancy: Effects on maternal depressive symptoms, smoking and pregnancy outcome. Hum. Reprod. 2007, 22, 869–877. [Google Scholar]
- Berle, J.O.; Mykletun, A.; Daltveit, A.K.; Rasmussen, S.; Holsten, F.; Dahl, A.A. Neonatal outcomes in offspring of women with anxiety and depression during pregnancy: A linkage study from The Nord-Trøndelag Health Study (HUNT) and Medical Birth Registry of Norway. Arch. Women’s Ment. Health 2005, 8, 181–189. [Google Scholar] [CrossRef]
- Andersson, L.; Sundström-Poromaa, I.; Wulff, M.; Aström, M.; Bixo, M. Neonatal outcome following maternal antenatal depression and anxiety: A population based study. Am. J. Epidemiol. 2004, 159, 872–881. [Google Scholar]
- Rossin, M. The effects of maternity leave on children’s birth and infant health outcomes in the United States. J. Health Econ. 2011, 30, 221–239. [Google Scholar]
- Papiernik, E.; Goffinet, F. Prevention of preterm births, the French experience. Clin. Obstetr. Gyn. 2004, 47, 755–767. [Google Scholar]
- Lu, M.C.; Kotelchuck, M.; Hogan, V.; Jones, L.; Wright, K.; Halfon, N. Closing the Black-White gap in birth outcomes: A lifecourse approach. Ethn. Dis. 2010, 20, 62–76. [Google Scholar]
- Kim, D.; Baum, C.F.; Ganz, M.; Subramanian, S.V.; Kawachi, I. The contextual effects of social capital on health: A cross-national instrumental variable analysis. Soc. Sci. Med. 2011, 73, 1689–1697. [Google Scholar]
- Kramer, M.R.; Hogue, C.R. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiol. Rev. 2009, 31, 84–98. [Google Scholar]
- Goldenberg, R.L.; Culhane, J.F.; Iams, J.D.; Romero, R. Epidemiology and causes of preterm birth. Lancet 2008, 371, 75–84. [Google Scholar]
- Lu, M.C.; Halfon, N. Racial and ethnic disparities in birth outcomes: A life-course perspective. Mat. Child Health J. 2003, 7, 13–30. [Google Scholar]
- Collins, J.W.; David, R.J. Racial disparity in low birth weight and infant mortality. Clin. Perinatol. 2009, 36, 63–73. [Google Scholar]
- Giurgescu, C.; McFarlin, B.L.; Lomax, J.; Craddock, C.; Albrecht, A. Racial discrimination and the Black-White gap in adverse birth outcomes: A review. J. Midwifery Womens Health 2011, 56, 362–370. [Google Scholar]
- Gissler, M.; Alexander, S.; Macfarlane, A.; Small, R.; Stray-Pedersen, B.; Zeitlin, J.; Zimbeck, M.; Gagnon, A. Stillbirths and infant deaths among migrants in industrialized countries. Acta Obstetr. Gyn. 2009, 88, 134–148. [Google Scholar]
- Arntzen, A.; Nybo Anderson, A.M. Social determinants for infant mortality in the Nordic countries, 1980–2001. Scand. J. Public Health 2004, 32, 381–389. [Google Scholar]
- Arntzen, A.; Mortensen, L.; Schnor, O.; Cnattingius, S.; Gissler, M.; Nybo Anderson, A. Neonatal and post-neonatal mortality by maternal education—A population-based study of trends in the Nordic countries, 1981–2000. Eur. J. Public Health 2007, 18, 245–251. [Google Scholar]
- Forssas, E.; Gissler, M.; Sihvonen, M.; Hemminki, E. Maternal predictors of perinatal mortality: The role of birth weight. Int. J. Epidemiol. 1999, 28, 475–478. [Google Scholar]
- Barger, M.K. Maternal nutrition and perinatal outcomes. J. Midwifery Womens Health 2010, 55, 502–511. [Google Scholar]
- Catov, J.M.; Bodnar, L.M.; Ness, R.B.; Markovic, N.; Roberts, J.M. Association of periconceptional multivitamin use and risk of preterm or small-for-gestational-age births. Amer. J. Epidemiol. 2007, 166, 296–303. [Google Scholar]
- Dunlop, A.L.; Kramer, M.R.; Hogue, C.J.; Menon, R.; Ramakrishan, U. Racial disparities in preterm birth: An overview of the potential role of nutrient deficiencies. Acta Obstetr. Gyn. 2011, 90, 1332–1341. [Google Scholar]
- Tennant, P.W.G.; Rankin, J.; Bell, R. Maternal body mass index and the risk of fetal and infant death: A cohort study from the North of England. Hum. Reprod. 2011, 26, 1501–1511. [Google Scholar]
- Knight, M.; Kurinczuk, J.J.; Spark, P.; Brocklehurst, P.; UK Obstetric Surveillance System. Extreme obesity in pregnancy in the United Kingdom. Obstetr. Gyn. 2010, 115, 989–997. [Google Scholar]
- Maconochie, N.; Doyle, P.; Prior, S.; Simmons, R. Risk factors for first trimester miscarriage—Results from a UK-population-based case-control study. Br. J. Obstetr. Gyn. 2006, 114, 170–186. [Google Scholar]
- Grote, N.K.; Bridge, J.A.; Gavin, A.R.; Melville, J.L.; Iyengar, S.; Katon, W.J. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch. General Psychiatr. 2010, 67, 1012–1024. [Google Scholar]
- Giscombé, C.L.; Lobel, M. Explaining disproportionately high rates of adverse birth outcomes among African Americans: The impact of stress, racism, and related factors in pregnancy. Psychol. Bull. 2005, 131, 662–683. [Google Scholar] [CrossRef]
- Alder, J.; Fink, N.; Bitzer, J.; Hösli, I.; Holzgreve, W. Depression and anxiety during pregnancy: A risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J. Matern. Fetal Neonatal. Med. 2007, 20, 189–209. [Google Scholar]
- Preston, S.H. The changing relation between mortality and level of economic development. Popul. Stud. 1975, 29, 231–248. [Google Scholar]
- Ward, A.C. The role of causal criteria in causal inferences: Bradford Hill’s “aspects of association”. Epidemiol. Perspect. Innov. 2009, 6, 2. [Google Scholar] [CrossRef]
- Luo, Z.; Gardiner, J.C.; Bradley, C.J. Applying propensity score methods in medical research: Pitfalls and prospects. Med. Care Res. Rev. 2010, 67, 528–554. [Google Scholar]
- Suarez, D.; Borràs, R.; Basagaña, X. Differences between marginal structural models and conventional models in their exposure effect estimates: A systematic review. Epidemiology 2011, 22, 586–588. [Google Scholar]
- Warnecke, R.B.; Oh, A.; Breen, N.; Gehlert, S.; Paskett, E.; Tucker, K.L.; Lurie, N.; Rebbeck, T.; Goodwin, J.; Flack, J.; et al. Approaching health disparities from a population perspective: The National Institutes of Health Centers for Population Health and Health Disparities. Am. J. Public Health 2008, 98, 1608–1615. [Google Scholar] [CrossRef]
- Committee on the Review and Assessment of the NIH’s Strategic Research Plan and Budget to Reduce and Ultimately Eliminate Health Disparities, Examiningthe Health Disparities Research Plan of the National Institutesof Health: Unfinished Business; National Academy Press: Washington, DC, USA, 2006.
- Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 1985, 14, 32–38. [Google Scholar]
- Bailar, J.C. The promise and problems of meta-analysis. N. Engl. J. Med. 1997, 337, 559–561. [Google Scholar]
- Adelaide Statement on Health in All Policies: Moving towards a Shared Governance for Health and Well-Being. In Health in All Policies International Meeting, Adelaide, 13–15 April 2010; World Health Organization: Geneva, Switzerland, 2010.
- Nair, M.; Webster, P.; Ariana, P. Impact of non-health policies on infant mortality through the social determinants pathway. Bull. WHO 2011, 89, 778. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Kim, D.; Saada, A. The Social Determinants of Infant Mortality and Birth Outcomes in Western Developed Nations: A Cross-Country Systematic Review. Int. J. Environ. Res. Public Health 2013, 10, 2296-2335. https://doi.org/10.3390/ijerph10062296
Kim D, Saada A. The Social Determinants of Infant Mortality and Birth Outcomes in Western Developed Nations: A Cross-Country Systematic Review. International Journal of Environmental Research and Public Health. 2013; 10(6):2296-2335. https://doi.org/10.3390/ijerph10062296
Chicago/Turabian StyleKim, Daniel, and Adrianna Saada. 2013. "The Social Determinants of Infant Mortality and Birth Outcomes in Western Developed Nations: A Cross-Country Systematic Review" International Journal of Environmental Research and Public Health 10, no. 6: 2296-2335. https://doi.org/10.3390/ijerph10062296