Patients’ Acceptance towards a Web-Based Personal Health Record System: An Empirical Study in Taiwan
Abstract
:1. Introduction
2. Literature Review and Hypotheses Development
2.1. Personal Health Records
2.1.1. Definitions and Functions of PHR
2.1.2. PHR for Infertility
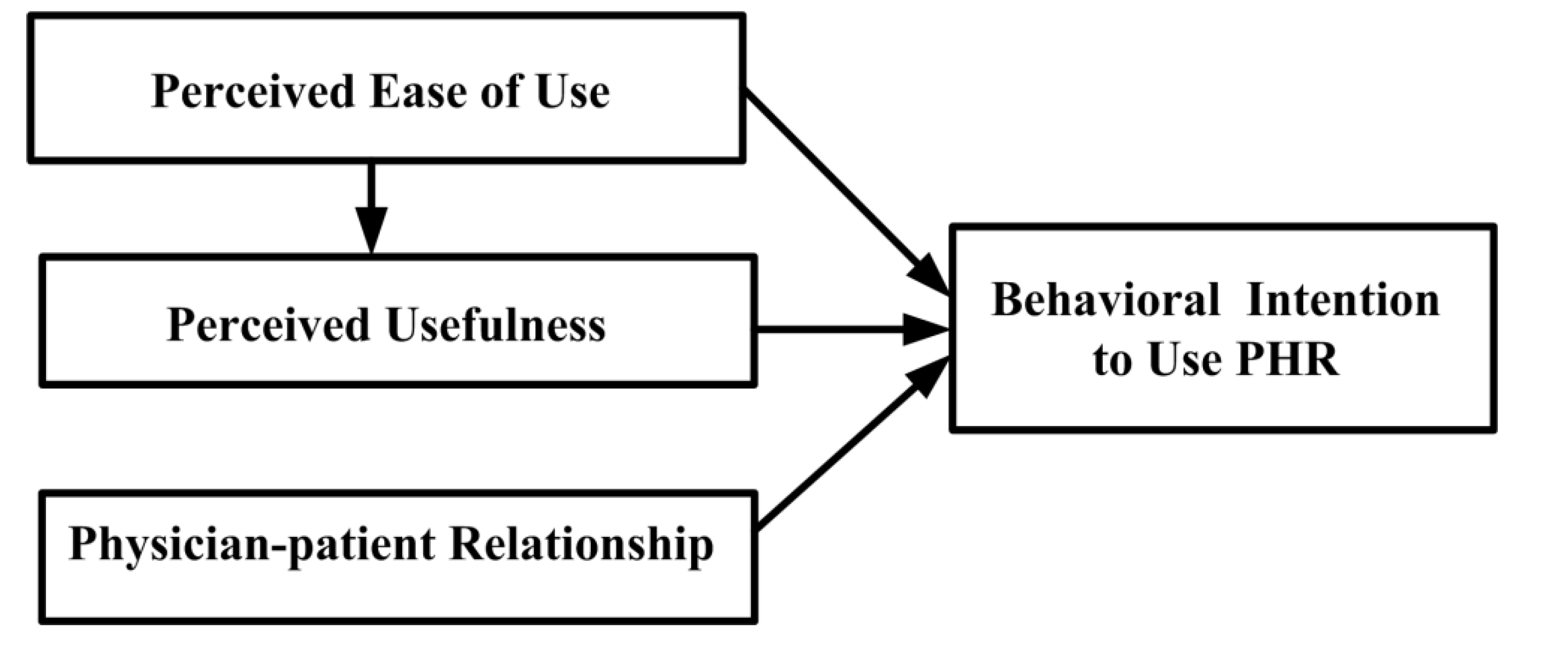
2.2. Technology Acceptance on PHR Adoption
- Hypothesis 1: A positive relationship exists between PEOU and PU in the PHR context.
- Hypothesis 2: A positive relationship exists between PEOU and BI in the PHR context.
- Hypothesis 3: A positive relationship exists between PU and BI in the PHR context.
2.3. Physician-Patient Relationship and Technology Acceptance
- Hypothesis 4: A positive relationship exists between PPR and BI in the PHR context.
3. Method
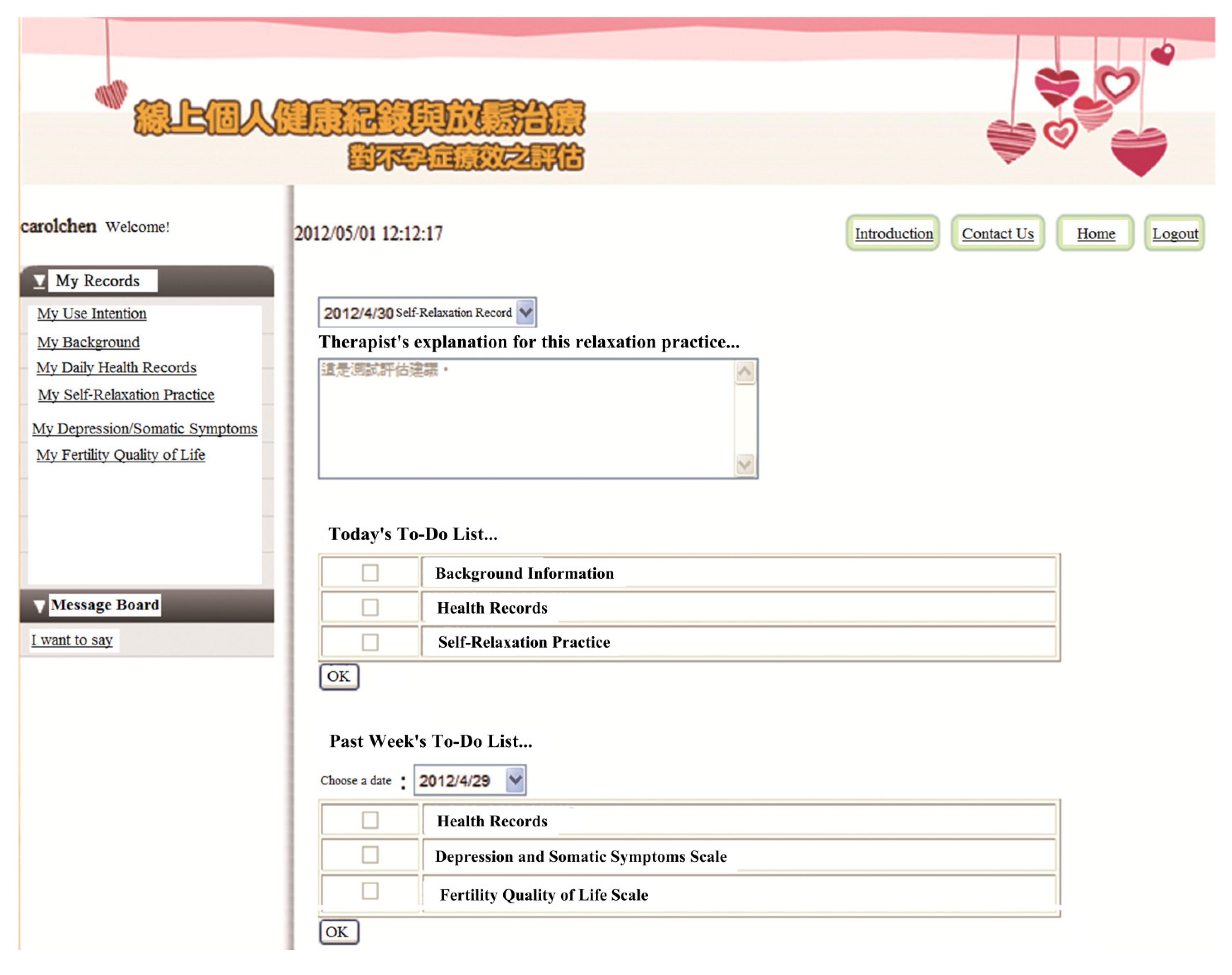
3.1. The Web-Based Infertile PHR System
- (1)
- Main menu: (1a) The upper right-hand corner of the website provides therapists’ suggestions based on the outcome of the patient’s last self-relaxation training; (1b) the middle of the right-hand side of the website presents items that should be personally recorded and evaluated during the current session; and (1c) the bottom right-hand corner presents the items that were not evaluated by the patient in the previous week and reminds users to complete the evaluation.
- (2)
- Record history searching function: The search function, located in the upper left-hand corner of the web site enables patients to look up historical records and explanations and suggestions that have been previously provided by the relaxation training therapist.
- (3)
- Message board function: The bottom left-hand corner of the website provides a platform for patients and care teams (physicians and therapists) to ask questions, leave messages, and post notifications. The research team’s e-mail address and phone number are posted on the PHR Web site. Patients who participate in the program can contact the research team at any time via e-mail or telephone.
3.2. Research Model
3.3. Setting and Ethics Approval
- (1)
- Aged between 25 and 45 years.
- (2)
- Diagnosed with infertility by a physician.
- (3)
- Have not adopting nor were adopting children.
- (4)
- Have not received cognitive behavioral therapy of any form within the two months before the study.
- (5)
- Could access the Internet at home.
3.4. Instrument Development
3.5. Procedures
4. Data Analysis and Results
4.1. Descriptive Statistics
| Construct | Item | Loading | Mean | Std. Dev. | Cronbach’s α | CR | AVE | Communality | Redundancy |
|---|---|---|---|---|---|---|---|---|---|
| Perceived Ease of Use (PEOU) | PEOU1 | 0.72 | 4.21 | 0.64 | 0.84 | 0.91 | 0.77 | 0.77 | |
| PEOU2 | 0.93 | ||||||||
| PEOU3 | 0.95 | ||||||||
| Perceived Usefulness (PU) | PU1 | 0.90 | 3.72 | 0.55 | 0.92 | 0.94 | 0.76 | 0.76 | 0.12 |
| PU2 | 0.86 | ||||||||
| PU3 | 0.88 | ||||||||
| PU4 | 0.81 | ||||||||
| PU5 | 0.91 | ||||||||
| Physician-patient Relationship (PPR) | PPR1 | 0.79 | 4.06 | 0.74 | 0.94 | 0.95 | 0.80 | 0.80 | |
| PPR2 | 0.94 | ||||||||
| PPR3 | 0.93 | ||||||||
| PPR4 | 0.91 | ||||||||
| PPR5 | 0.90 | ||||||||
| Behavioral Intention (BI) | BI1 | 0.98 | 3.89 | 0.66 | 0.94 | 0.97 | 0.95 | 0.95 | 0.16 |
| BI2 | 0.97 |
4.2. Reliability, Validity and Model Fit
| PEOU | PPR | PU | BI | |
|---|---|---|---|---|
| Perceived Ease of Use (PEOU) | 0.88 | |||
| Physician-patient Relationship (PPR) | 0.36 | 0.89 | ||
| Perceived Usefulness (PU) | 0.39 | 0.43 | 0.87 | |
| Behavioral Intention (BI) | 0.50 | 0.56 | 0.67 | 0.98 |
4.3. Hypotheses Testing

5. Discussion and Suggestions
5.1. Behavioral Intention
5.2. Effect of PEOU on PU
5.3. Effect of PEOU on BI
5.4. Effect of PU on BI
5.5. Effect of PPR on BI
6. Conclusions
6.1. Summary of Findings and Contributions
6.2. Limitations and Future Directions
Acknowledgments
Conflicts of Interest
References
- Waegemann, C.P. The five levels of electronic health records. MD Comput. 1996, 13, 199–203. [Google Scholar]
- Institute of Medicine (IOM), The Computer-Based Patient Record: An Essential Technology for Health Care; National Academy Press: Washington, DC, USA, 1997.
- American Telemedicine Association (AHA). What is Telemedicine? Available online: http://www.americantelemed.org/learn/what-is-telemedicine (accessed on 2 September 2013).
- Tang, P.C.; Lansky, D. The missing link: Bridging the patient-provider health information gap. Health Aff. 2005, 24, 1290–1295. [Google Scholar]
- Connecting for Health: A Public-Private Collaborative; Markle Foundation: New York, NY, USA, 2003.
- Bozkurt, S.; Zayim, N.; Gulkesen, K.H.; Samur, M.K; Karaağaoglu, N.; Saka, O. Usability of a web-based personal nutrition management tool. Inform. Health Soc. Care 2011, 36, 190–205. [Google Scholar]
- Pirtle, B.; Chandra, A. An overview of consumer perceptions and acceptance as well as barriers and potential of electronic personal health records. Am. J. Health Sci. 2011, 2, 45–52. [Google Scholar]
- Wen, K.Y.; Gary, K.; Fang, Z.; Suzanne, M. Consumers’ perceptions about and use of the internet for personal health records and health information exchange: Analysis of the 2007 health information national trends survey. J. Med. Internet Res. 2010, 12. [Google Scholar] [CrossRef]
- Consumers and Health Information Technology: A National Survey; California HealthCare Foundation: Oakland, CA, USA, 2010.
- Jian, W.S.; Shabbir, S.A.; Sood, S.P.; Lee, P.; Hsu, M.H.; Ho, C.H.; Li, Y.C.; Wen, H.C. Factors influencing consumer adoption of USB-based Personal Health Records in Taiwan. BMC Health Serv. Res. 2012, 12. [Google Scholar] [CrossRef]
- Kaelber, D.C.; Jha, A.K.; Johnston, D.; Middleton, B.; Bates, D.W. A Research agenda for personal health records (PHRs). J. Am. Med. Inform. Assoc. 2008, 15, 729–736. [Google Scholar] [CrossRef]
- Steinwachs, D.M.; Roter, D.; Skinner, E.A.; Lehman, A.F.; Fahey, M.; Cullen, B.; Everett, A.S.; Gallucci, G. A web-based program to empower patients who have schizophrenia to discuss quality of care with mental health providers. Psychiatr. Serv. 2011, 62, 1296–1302. [Google Scholar] [CrossRef]
- Weissman, A.; Gotlieb, L.; Ward, S.; Greenblatt, E.; Casper, R.F. Use of the internet by infertile couples. Fertil. Steril. 2000, 73, 1179–1182. [Google Scholar] [CrossRef]
- Haagen, E.C.; Tuil, W.; Hendriks, J.; de Bruijn, R.P.; Braat, D.D.; Kremer, J.A. Current internet use and preferences of IVF and ICSI patients. Hum. Reprod. 2003, 18, 2073–2078. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- American Health Information Management Association (AHIMA). Defining the personal health record. J. AHIMA. 2005, 76, 24–25.
- Healthcare Information and Management Systems Society (HIMSS), HIMSS Personal Health Records—Definition and Position Statement; HIMSS: Chicago, IL, USA, 2007.
- Kim, M.I.; Johnson, K.B. Personal health records: Evaluation of functionality and utility. J. Am. Med. Inform. Assoc. 2002, 9, 171–180. [Google Scholar] [CrossRef]
- Chen, T.H.; Chang, S.P.; Tsai, C.F.; Juang, K.D. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Hum. Reprod. 2004, 19, 2313–2318. [Google Scholar] [CrossRef]
- Domar, A.D.; Broome, A.; Zuttermeister, P.C.; Seibel, M.; Friedman, R. The prevalence and predictability of depression in infertile women. Fertil. Steril. 1992, 58, 1158–1163. [Google Scholar]
- Eugster, A.; Vingerhoets, A.J. Psychological aspects of in vitro fertilization: A review. Soc. Sci. Med. 1999, 48, 575–589. [Google Scholar] [CrossRef]
- Wischmann, T. Psychosocial aspects of fertility disorders. Urologe 2005, 44, 185–194. [Google Scholar] [CrossRef]
- Lee, M.; Delaney, C.; Moorhead, S. Building a personal health record from a nursing perspective. Int. J. Med. Inform. 2007, 76, S308–S316. [Google Scholar] [CrossRef]
- Wright, A.; Sittig, D.F. Encryption characteristics of two usb-based personal health record devices. J. Am. Med. Inform. Assoc. 2007, 14, 397–399. [Google Scholar] [CrossRef]
- Sox, C.M.; Gribbons, W.M.; Loring, B.A.; Mandl, K.D.; Batista, R.; Porter, S.C. Patient-centered design of an information management module for a personally controlled health record. J. Med. Internet Res. 2010, 12. [Google Scholar] [CrossRef]
- Krist, A.H.; Peele, E.; Woolf, S.H.; Rothemich, S.F.; Loomis, J.F.; Longo, D.R.; Kuzel, A.J. Designing a patient-centered personal health record to promote preventive care. BMC Med. Inform. Decis. Mak. 2011, 11. [Google Scholar] [CrossRef]
- Kim, E.H.; Stolyar, A.; Lober, W.B.; Herbaugh, A.L.; Shinstrom, S.E.; Zierler, B.K.; Soh, C.B.; Kim, Y. Usage Patterns of a Personal Health Record by Elderly and Disabled Users. In Proceeding of the AMIA 2007 Symposium Proceedings, Chicago, IL, USA, 10–14 November 2007.
- Chau, J.P.; Chung, L.C.; Wong, R.Y.; Loo, K.M.; Lo, S.H.; So, T.T.; Lau, M.S.; Yeung, T.H.; Leung, B.S.; Tong, M.L.; et al. An evaluation of a web-based diabetes education program designed to enhance self-management among patients living with diabetes. Comput. Inform. Nurs. 2012, 30, 672–679. [Google Scholar] [CrossRef]
- Logue, M.D.; Effken, J.A. Modeling factors that influence personal health records adoption. Comput. Inform. Nurs. 2012, 30, 354–362. [Google Scholar]
- Davis, F.D.; Venkatesh, V. A critical assessment of potential measurement biases in the technology acceptance model: Three experiments. Int. J. Hum.-Comput. Stud. 1996, 45, 19–45. [Google Scholar] [CrossRef]
- Lee, Y.; Kozar, K.A.; Larsen, K.R.T. The technology acceptance model: Past, present, and future. Commun. Assoc. Inf. Syst. 2003, 12, 752–780. [Google Scholar]
- Pare, G.; Sicotte, C.; Jacques, H. The Effects of creating psychological ownership on physicians’ acceptance of clinical information systems. J. Am. Med. Inform. Assoc. 2006, 13, 197–205. [Google Scholar] [CrossRef]
- Aggelidis, V.P.; Chatzoglou, P.D. Using a modified technology acceptance model in hospitals. Int. J. Med. Inform. 2009, 78, 115–126. [Google Scholar] [CrossRef]
- Kowitlawakul, Y. The technology acceptance model: Predicting nurses’ intention to use telemedicine technology (eICU). Comput. Inform. Nurs. 2011, 29, 411–418. [Google Scholar] [CrossRef]
- Rahimpour, M.; Lovell, N.H.; Celler, B.G.; McCormick, J. Patients’ perceptions of a home telecare system. Int. J. Med. Inform. 2008, 77, 486–498. [Google Scholar] [CrossRef]
- Or, C.; Karsh, B.T.; Severtson, D.J.; Burke, L.J.; Brown, R.L.; Brennan, P.F. Factors affecting home care patients’ acceptance of a web-based interactive self-management technology. J. Am. Med. Inform. Assoc. 2011, 18, 51–59. [Google Scholar] [CrossRef]
- Lim, S.H.; Kim, D. The role of trust in the use of health infomediaries among university students. Inform. Health Soc. Care 2012, 37, 92–105. [Google Scholar] [CrossRef]
- Teutsch, C. Patient-doctor communication. Med. Clin. North. Am. 2003, 87, 1115–1145. [Google Scholar] [CrossRef]
- Roter, D.L.; Hall, J.A. Doctors Talking With Patients/Patients Talking with Doctors: Improving Communication in Medical Visits; Auburn House: Westport, CT, USA, 1992. [Google Scholar]
- The Medical Interview: Clinical Care, Education, and Research; Lipkin, M.; Putnam, S.M.; Lazare, A. (Eds.) Springer-Verlag: New York, NY, USA, 1995.
- Scott, A. Economics of General Practice. In Handbook of Health Economics; Culyer, A.J., Newhouse, J.P., Eds.; Elsevier Science: New York, NY, USA, 2000; Volume 1B. [Google Scholar]
- Winkelman, W.J.; Leonard, K.J.; Rossos, P.G. Patient-perceived usefulness of online electronic medical records: Employing grounded theory in the development of information and communication technologies for use by patients living with chronic illness. J. Am. Med. Inform. Assoc. 2005, 12, 306–314. [Google Scholar] [CrossRef]
- Ventres, W.; Kooienga, S.; Vuckovic, N.; Marlin, R.; Nygren, P.; Stewart, V. Physicians, patients, and the electronic health record: An ethnographic analysis. Ann. Fam. Med. 2006, 4, 124–131. [Google Scholar] [CrossRef]
- Werner, P.; Karnieli, E. A model of the willingness to use telemedicine for routine and specialized care. J. Telemed. Telecare 2003, 9, 264–272. [Google Scholar] [CrossRef]
- Werner, P. Willingness to use telemedicine for psychiatric care. Telemed. e-Health 2004, 10, 286–293. [Google Scholar] [CrossRef]
- Öst, L.G. Applied relaxation: description of a coping technique and review of controlled studies. Behav. Res. Ther. 1987, 25, 397–409. [Google Scholar] [CrossRef]
- Hung, C.I.; Weng, L.J.; Su, Y.J.; Liu, C.Y. Depression and somatic symptoms scale: A new scale with both depression and somatic symptoms emphasized. Psychiatry Clin. Neurosci. 2006, 60, 700–708. [Google Scholar] [CrossRef]
- The Fertility Quality of Life Questionnaire, 2009. Available online: http://www.fertiqol.org (accessed on 20 September 2012).
- Department of Health, UK. The GP Patient Survey Questionnaire (July–September 2011). Available online: http://www.gp-patient.co.uk/download/Questionnaires/Y6Q1%20GP%20Patient%20Survey%20questionnaire.pdf (accessed on 20 September 2012).
- Chin, W.W. How to Write up and Report PLS Analyses. In Handbook of Partial Least Squares Concepts, Methods and Applications, 1st ed.; Vinzi, V.E., Chin, W.W., Henseler, J., Wang, H., Eds.; Springer: Heidelberg, Berlin, Germany, 2010. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- O’Leary-Kelly, S.W.; Vokurka, R.J. The empirical assessment of construct validity. J. Oper. Manag. 1998, 16, 387–405. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sinkovics, R.R. The use of partial least squares path modeling in international marketing. Adv. Int. Mark. 2009, 20, 277–319. [Google Scholar]
- Wetzels, M.; Schroder, G.O.; Oppen, V.C. Using PLS path modeling for assessing hierarchical construct models: Guidelines and empirical illustration. MIS Quart. 2009, 33, 177–195. [Google Scholar]
- Van Bon, A.C.; Kohinor, M.J.; Hoekstra, J.B.; von Basum, G.; de Vries, J.H. Patients’ perception and future acceptance of an artificial pancreas. J. Diabetes Sci. Technol. 2010, 4, 596–602. [Google Scholar]
- Ziefle, M.; Wilkowska, W. Technology Acceptability for Medical Assistance. In Proceedings of the 4th International Conference on Pervasive Computing Technologies for Healthcare, Munchen, Germany, 22–25 March 2010.
- Hargreaves, J.S. Will electronic personal health records benefit providers and patients in rural America? Telemed. e-Health 2010, 16, 167–176. [Google Scholar] [CrossRef]
- Klein, R. Internet-based patient–physician electronic communication applications: Patient acceptance and trust. e-Service J. 2007, 5, 27–51. [Google Scholar] [CrossRef]
- Lim, S.; Xue, L.; Yen, C.C.; Chang, L.; Chan, H.C.; Tai, B.C.; Duh, B.L.; Choolani, M. A study on Singaporean women’s acceptance of using mobile phones to seek health information. Int. J. Med. Inform. 2011, 80, e189–e202. [Google Scholar] [CrossRef]
- Ta, W.H.; Ooi, K.B.; Sim, J.J.; Phusavat, K. Determinants of mobile learning adoption: An empirical analysis. J. Comput. Inf. Syst. 2012, 52, 82–91. [Google Scholar]
- Gefen, D.; Karahanna, E.; Straub, D.W. Trust and TAM in online shopping: An integrated model. MIS Quart. 2003, 27, 51–90. [Google Scholar]
- Ong, C.S.; Lai, J.Y.; Wang, Y.S. Factors affecting engineers’ acceptance of asynchronous e-learning systems in high-tech companies. Inf. Manag. 2004, 41, 795–804. [Google Scholar] [CrossRef]
- Teo, T.; van Schaik, P. Understanding technology acceptance in pre-service teachers: A structural-equation modeling approach. Asia-Pac. Educ. Res. 2009, 18, 47–66. [Google Scholar]
- Pikkarainen, T.; Pikkarainen, K.; Karjaluoto, H.; Pahnila, S. Consumer acceptance of online banking: An extension of the technology acceptance model. Internet Res. 2004, 14, 224–235. [Google Scholar] [CrossRef]
- Wu, J.H.; Wang, S.C. What drives mobile commerce? An empirical evaluation of the revised technology acceptance model. Inf. Manag. 2006, 42, 719–729. [Google Scholar]
- Barker, D.J.; van Schaik, P.; Simpson, D.S.; Corbett, W.A. Evaluating a spoken dialogue system for recording clinical observations during an endoscopic examination. Inform. Health Soc. Care 2003, 28, 85–97. [Google Scholar] [CrossRef]
- Liang, H.; Xue, Y.; Chase, S.K. Online health information seeking by people with physical disabilities due to neurological conditions. Int. J. Med. Inform. 2011, 78, 115–126. [Google Scholar]
- Shaw, B.R.; Han, J.Y.; Hawkins, R.P.; James, S.; McTavish, F.; Gustafson, D.H. Doctor–patient relationship as motivation and outcome: Examining uses of an interactive cancer communication system. Int. J. Med. Inform. 2007, 76, 274–282. [Google Scholar] [CrossRef]
- Tieman, J. Survey: Hospital dabble in internet. Mod. Healthc. 2000, 52, 52,54. [Google Scholar]
- Ball, M.J.; Lillis, J. E-health: Transforming the physician/patient relationship. Int. J. Med. Inform. 2001, 61, 1–10. [Google Scholar] [CrossRef]
- Anderson, J.G.; Rainey, M.R.; Eysenbach, G. The impact of CyberHealthcare on the Physician–patient relationship. J. Med. Syst. 2003, 27, 67–84. [Google Scholar] [CrossRef]
- Omary, Z.; Lupiana, D.; Mtenzi, F.; Wu, B. Analysis of the challenges affecting e-healthcare adoption in developing countries: A case of Tanzania. Int. J. Inf. Stud. 2010, 2, 38–50. [Google Scholar]
- Fang, D.; Fang, C.L.; Tsai, B.K.; Lan, L.C.; Hsu, W.S. Relationships among trust in messages, risk perception, and risk reduction preferences based upon avian influenza in Taiwan. Int. J. Environ. Res. Public Health 2012, 9, 2742–2757. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Liu, C.-F.; Tsai, Y.-C.; Jang, F.-L. Patients’ Acceptance towards a Web-Based Personal Health Record System: An Empirical Study in Taiwan. Int. J. Environ. Res. Public Health 2013, 10, 5191-5208. https://doi.org/10.3390/ijerph10105191
Liu C-F, Tsai Y-C, Jang F-L. Patients’ Acceptance towards a Web-Based Personal Health Record System: An Empirical Study in Taiwan. International Journal of Environmental Research and Public Health. 2013; 10(10):5191-5208. https://doi.org/10.3390/ijerph10105191
Chicago/Turabian StyleLiu, Chung-Feng, Yung-Chieh Tsai, and Fong-Lin Jang. 2013. "Patients’ Acceptance towards a Web-Based Personal Health Record System: An Empirical Study in Taiwan" International Journal of Environmental Research and Public Health 10, no. 10: 5191-5208. https://doi.org/10.3390/ijerph10105191
APA StyleLiu, C.-F., Tsai, Y.-C., & Jang, F.-L. (2013). Patients’ Acceptance towards a Web-Based Personal Health Record System: An Empirical Study in Taiwan. International Journal of Environmental Research and Public Health, 10(10), 5191-5208. https://doi.org/10.3390/ijerph10105191




