Validation of a New Scintillating Fiber Dosimeter for Radiation Dose Quality Control in Computed Tomography
Abstract
:1. Introduction
2. Materials and Methods
2.1. Computed Tomography Equipment
2.2. Irradiation Parameters
2.3. Reference Dose Indexes
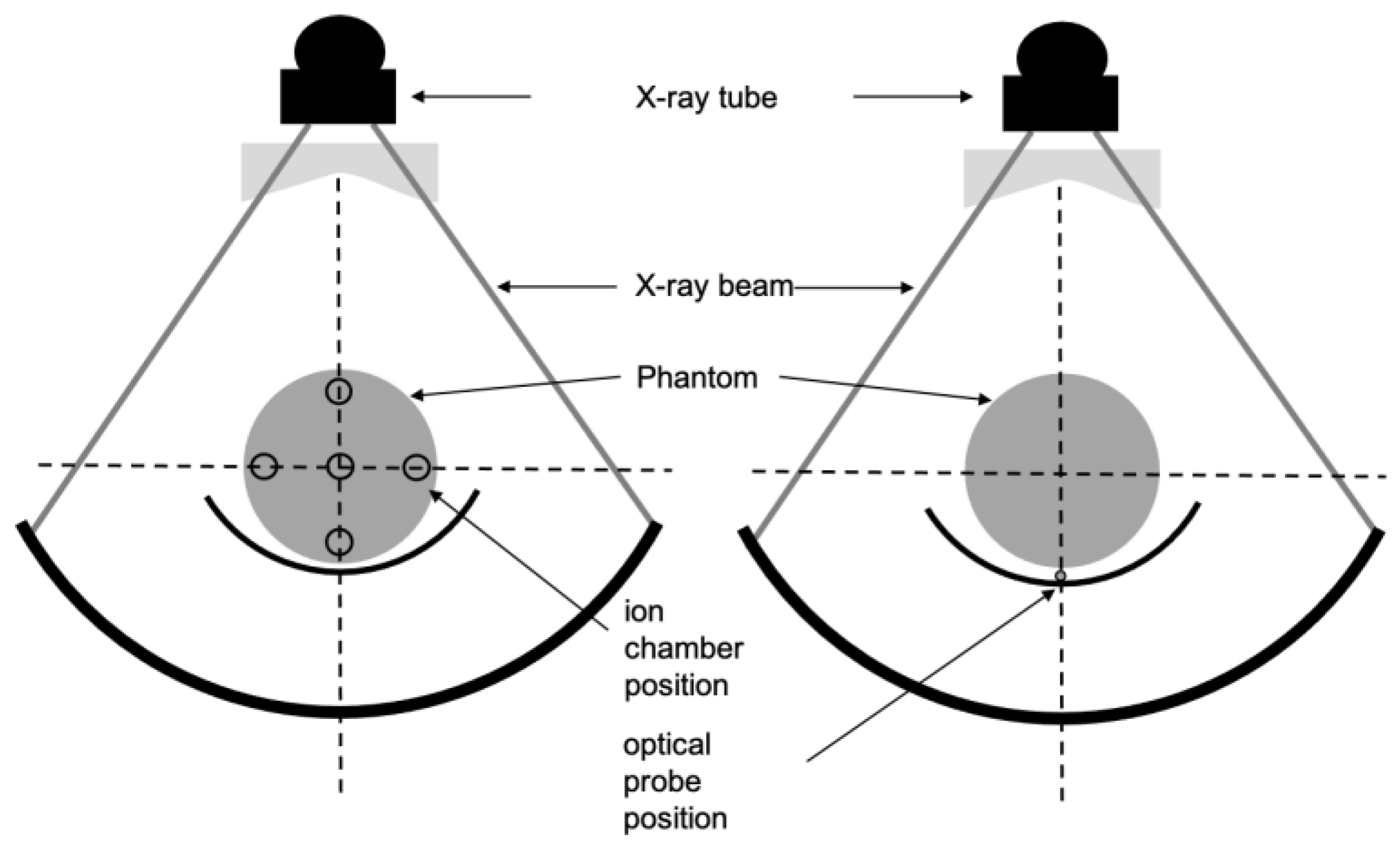
2.3.1. Reference Materials
2.3.2. Reference Measurements
- CT scan Compliance
- Beam Width < 40 mm
- Beam Width > 40 mm
2.4. IVIscan Dose Indexes
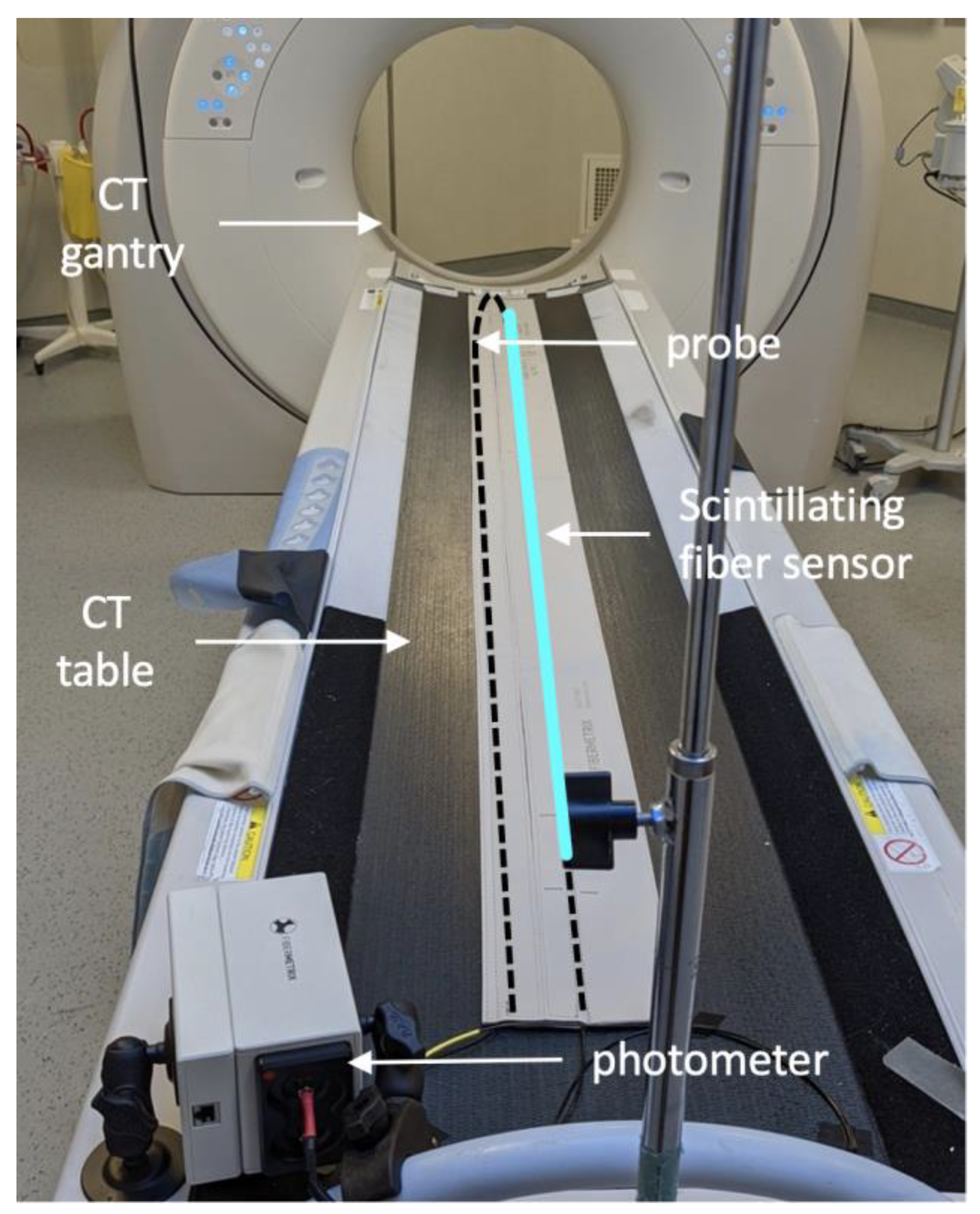
2.4.1. IVIscan Scintillating Fiber Detector
2.4.2. IVIscan Measurement Method
2.5. Statistical Analysis
2.5.1. Repeatability
2.5.2. Energy Dependence
3. Results
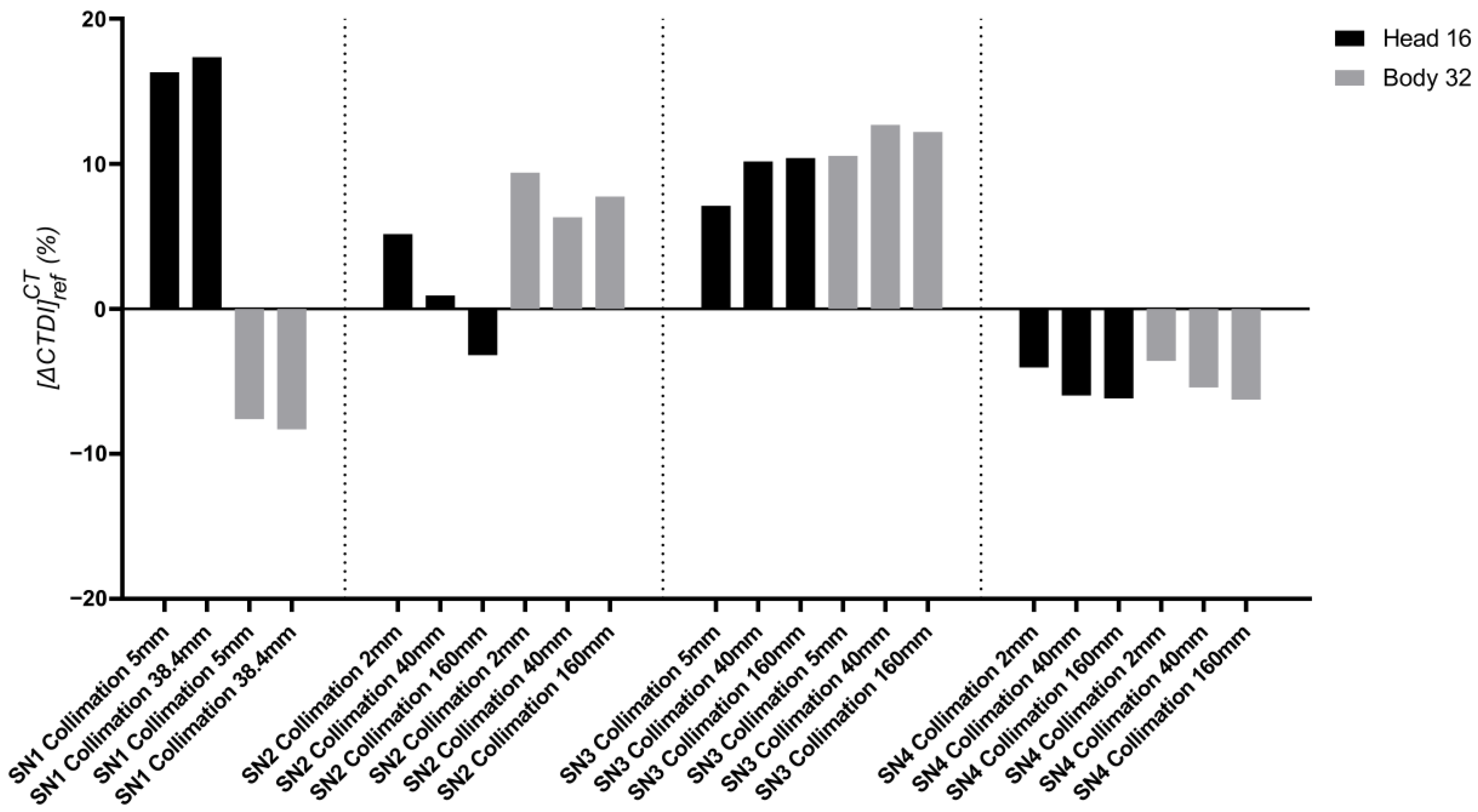
3.1. CT Scan Compliance
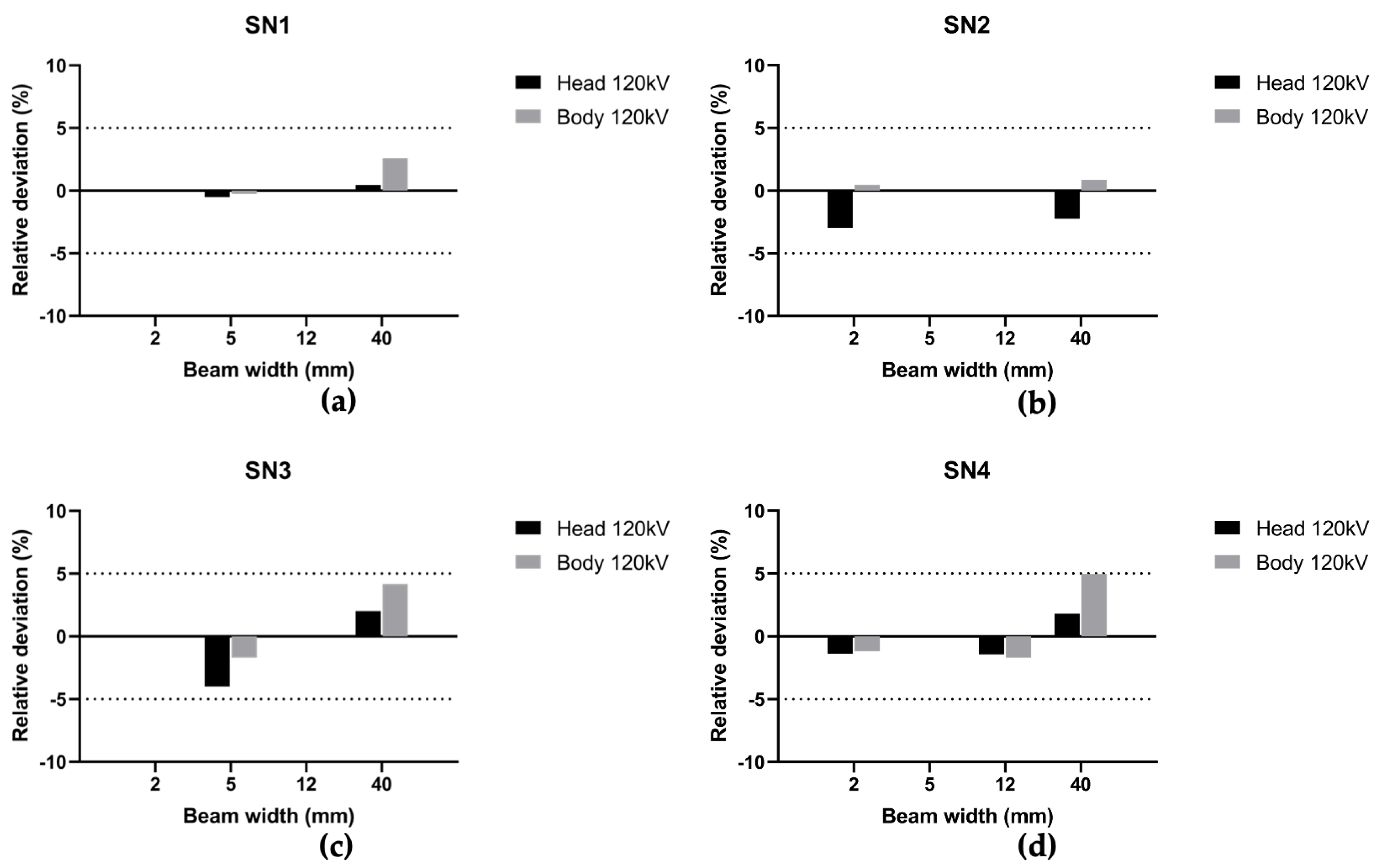
3.2. IVIscan Validation
3.2.1. Repeatability
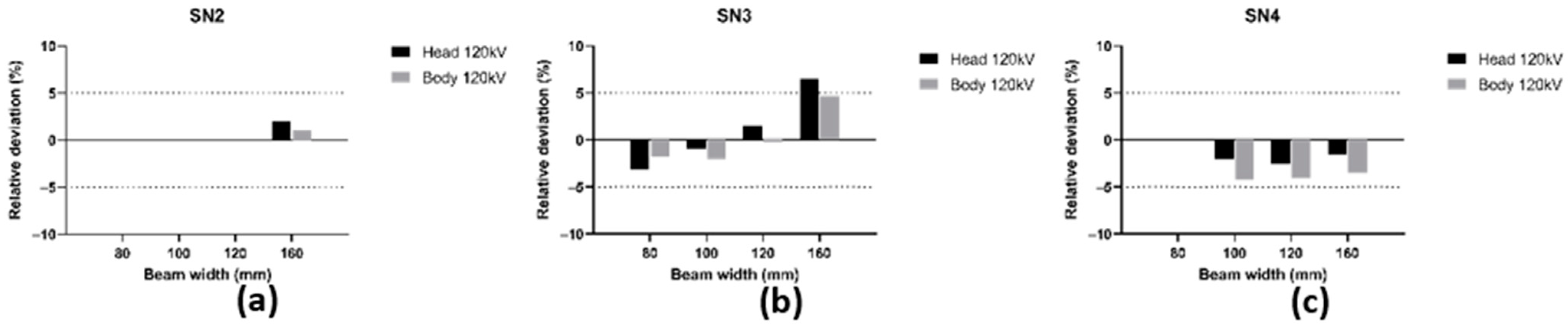
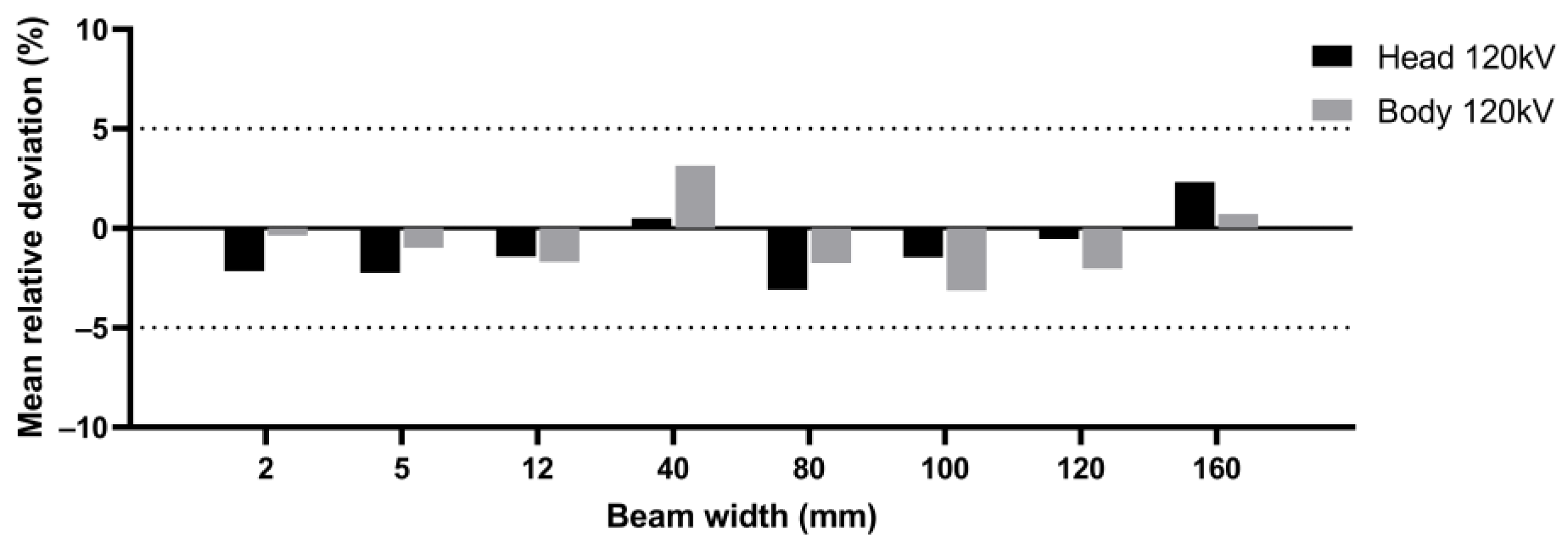
3.2.2. Deviation between and
3.2.3. Energy Dependence
4. Discussion and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shope, T.B.; Gagne, R.M.; Johnson, G.C. A Method for Describing the Doses Delivered by Transmission X-ray Computed Tomography. Med. Phys. 1981, 8, 488–495. [Google Scholar] [CrossRef]
- Dixon, R.L.; Anderson, J.A.; Bakalyar, D.M.; Boedeker, K.; Boone, J.M.; Cody, D.D.; Fahrig, R.; Jaffray, D.A.; Kyprianou, I.S.; Mc Collough, C.H.; et al. Comprehensive Methodology for the Evaluation of Radiation Dose in X-ray Computed Tomography; Report TG n°111; AAPM: Alexandria, VA, USA, 2010; Available online: https://www.aapm.org/pubs/reports/RPT_111.pdf (accessed on 4 January 2023).
- Dixon, R.L.A. New Look at CT Dose Measurement: Beyond CTDI. Med. Phys. 2003, 30, 1272–1280. [Google Scholar] [CrossRef] [PubMed]
- Perisinakis, K.; Damilakis, J.; Tzedakis, A.; Papadakis, A.; Theocharopoulos, N.; Gourtsoyiannis, N. Determination of the Weighted CT Dose Index in Modern Multi-Detector CT Scanners. Phys. Med. Biol. 2007, 52, 6485–6495. [Google Scholar] [CrossRef] [PubMed]
- Boone, J.M. The Trouble with CTDI100: The Trouble with CTDI100. Med. Phys. 2007, 34, 1364–1371. [Google Scholar] [CrossRef]
- Damilakis, J. CT Dosimetry: What Has Been Achieved and What Remains to Be Done. Investig. Radiol. 2021, 56, 62–68. [Google Scholar] [CrossRef]
- Lambert, J.W.; Phillips, E.D.; Villanueva-Meyer, J.E.; Nardo, L.; Facchetti, L.; Gould, R.G. Axial or Helical? Considerations for Wide Collimation CT Scanners Capable of Volumetric Imaging in Both Modes. Med. Phys. 2017, 44, 5718–5725. [Google Scholar] [CrossRef] [PubMed]
- Bujila, R.; Kull, L.; Danielsson, M.; Andersson, J. Applying Three Different Methods of Measuring CTDIfree Air to the Extended CTDI Formalism for Wide-Beam Scanners (IEC 60601–2–44): A Comparative Study. J. Appl. Clin. Med. Phys. 2018, 19, 281–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dixon, R.L.; Ballard, A.C. Experimental Validation of a Versatile System of CT Dosimetry Using a Conventional Ion Chamber: Beyond CTDI100: A Versatile CT Dosimetry System. Med. Phys. 2007, 34, 3399–3413. [Google Scholar] [CrossRef] [PubMed]
- International Atomic Energy Agency. Status of Computed Tomography Dosimetry for Wide Cone Beam Scanners; Human Health Reports n°5; IAEA: Vienna, Austria, 2011; Available online: https://www-pub.iaea.org/mtcd/publications/pdf/pub1528_web.pdf (accessed on 4 January 2023).
- International Atomic Energy Agency. Quality Assurance Program for Computed Tomography: Diagnostic and Therapy Applications; Human Health Series n°19; IAEA: Vienna, Austria, 2012; Available online: https://www-pub.iaea.org/mtcd/publications/pdf/pub1557_web.pdf (accessed on 4 January 2023).
- American College of Radiology. Computed Tomography Quality Control Manual; ACR: Reston, VA, USA, 2017; Available online: https://www.acr.org/-/media/ACR/Files/Clinical-Resources/QC-Manuals/CT_QCManual.pdf (accessed on 4 January 2023).
- Gillet, P.; Munier, M.; Arbor, N.; Carbillet, F.; El Bitar, Z. Evaluation of an Optical Scintillating Fiber Detector for CT Dosimetry. Radiat. Meas. 2018, 119, 125–131. [Google Scholar] [CrossRef]
- Gillet, P. Validation d’un Dosimètre Patient Temps Réel Basé Sur Fibre Optique Pour La Tomodensitométrie X à l’aide de Simulation Monte Carlo. Ph.D. Thesis, Université de Strasbourg, Strasbourg, France, 2018. [Google Scholar]
- Devic, C.; Plagnard, J.; Munier, M. Characterization of an Innovative Detector Based on Scintillating Fiber for Personalized Computed Tomography Dosimetry. Sensors 2021, 22, 90. [Google Scholar] [CrossRef] [PubMed]
- Veronese, I.; Chiodini, N.; Cialdi, S.; d’Ippolito, E.; Fasoli, M.; Gallo, S.; La Torre, S.; Mones, E.; Vedda, A.; Loi, G. Real-time dosimetry with Yb-doped silica optical fibres. Phys. Med. Biol. 2017, 62, 4218. [Google Scholar] [CrossRef] [PubMed]
- Zubair, H.T.; Oresegun, A.; Mizanur Rahman, A.K.M.; Ung, N.M.; Mat Sharif, K.A.; Zulkifi, M.I.; Muhd Yassin, S.Z.; Maah, M.J.; Yusoff, Z.; Abdul-Rashid, H.A.; et al. Real-time radiation dosimetry using P-doped silica optical fiber. Measurement 2019, 146, 119–124. [Google Scholar] [CrossRef]
- Horner, M.R.; Stepusin, E.J.; Hyer, D.; Hintenlang, D.E. Characterizing energy dependence and count rate performance of a dual scintillator fiber-optic detector for computed tomography: Performance of a Dual Scintillator Fiber-Optic Detector. Med. Phys. 2015, 42, 1268–1279. [Google Scholar] [CrossRef] [PubMed]
- Thrower, S.; Prajapati, S.; Holmes, S.; Schüler, E.; Beddar, S. Characterization of the plastic scintillator detector system Exradin W2 in a high dose rate flattening-filter-free Photon Beam. Sensors 2022, 22, 6785. [Google Scholar] [CrossRef] [PubMed]
- Galavis, P.E.; Hu, L.; Holmes, S.; Das, I.J. Characterization of the plastic scintillation detector Exradin W2 for small field dosimetry. Med. Phys. 2019, 46, 2468–2476. [Google Scholar] [CrossRef] [PubMed]
- Underwood, T.S.A.; Rowland, B.C.; Ferrand, R.; Vieillevigne, L. Application of the Exradin W1 scintillator to determine Ediode 60,017 and microdiamond 60,019 correction factors for relative dosimetry within small MV and FFF fields. Phys. Med. Biol. 2015, 60, 6669–6683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Popotte, C.; Devic, C.; Munier, M.; Moreno, R.; Rousseau, H.; Perlongo, S.; Pilleul, F.; Paul, D. Multicentric comparative study of dose indexes using an “in vivo” optical fiber detection system. Phys. Med. Int. J. Med. Phys. 2021, 92, S127–S128. [Google Scholar] [CrossRef]
- Popotte, C.; Devic, C.; Guillochon, N.; Munier, M.; Paul, D. Evaluation of the IVIscan Detector for Dosimetric Quality Control and Dose Measurements for Cone Beam Computed Tomography in Radiotherapy. Phys. Med. Eur. J. Med. Phys. 2022, 104, S32. [Google Scholar] [CrossRef]
- American Association of Physicists in Medicine. Performance Evaluation of Computed Tomography Systems; Report Task Group 233; AAPM: Alexandria, VA, USA, 2019; Available online: https://www.aapm.org/pubs/reports/RPT_233.pdf (accessed on 4 January 2023).
- Agence Nationale de Sécurité du Médicament et des Produits de Santé. Annexe de la Décision du 22/11/2007 Fixant les Modalités du Contrôle de Qualité des Scanographes Modifiée par la Décision du 11/03/2011; ANSM: Saint Denis, France, 2019. Available online: https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000023850697 (accessed on 4 January 2023).
- Fibermetrix. IVIscan. Available online: https://fibermetrix.com/wp-content/uploads/2022/10/Fiche_produit_IVI_ENG.pdf (accessed on 4 January 2023).
- Munier, M.; Sohier, T.; Torche, F.; Carbillet, F. Dispositif de Détermination D’une Dose Déposée et Procédé Associé. FR Patent 3053799 (B1), 30 August 2019. [Google Scholar]
- Munier, M.; Carbillet, F.; Prudhomme, P.-B.; Guillochon, N. Procédé de Traitement des Données Relatives à un Examen Radiologique D’un Patient. FR Patent 3110708 (B1), 22 April 2022. [Google Scholar]



| Beam width (mm) | 5 | 38.5 | ||||||
| Tube voltage (kV) | 70 | 100 | 120 | 140 | 70 | 100 | 120 | 140 |
| Mean (mGy) | 3.78 | 12.77 | 21.52 | 32.19 | 4.31 | 14.43 | 24.11 | 35.70 |
| RSD (%) | 0.21% | 0.07% | 0.10% | 0.16% | 0.05% | 0.11% | 0.10% | 0.02% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guillochon, N.; Balde, M.; Popotte, C.; Pondard, S.; Desport, C.; Kien, N.; Carbillet, F.; Moreno, R.; Munier, M. Validation of a New Scintillating Fiber Dosimeter for Radiation Dose Quality Control in Computed Tomography. Sensors 2023, 23, 2614. https://doi.org/10.3390/s23052614
Guillochon N, Balde M, Popotte C, Pondard S, Desport C, Kien N, Carbillet F, Moreno R, Munier M. Validation of a New Scintillating Fiber Dosimeter for Radiation Dose Quality Control in Computed Tomography. Sensors. 2023; 23(5):2614. https://doi.org/10.3390/s23052614
Chicago/Turabian StyleGuillochon, Nicolas, Mamoutou Balde, Christian Popotte, Selena Pondard, Corentin Desport, Nicolas Kien, Fanny Carbillet, Ramiro Moreno, and Mélodie Munier. 2023. "Validation of a New Scintillating Fiber Dosimeter for Radiation Dose Quality Control in Computed Tomography" Sensors 23, no. 5: 2614. https://doi.org/10.3390/s23052614





