Kinect-Based Virtual Game for the Elderly that Detects Incorrect Body Postures in Real Time
Abstract
:1. Introduction
2. Background
3. Materials and Methods
3.1. Participants
3.2. Experimental Design
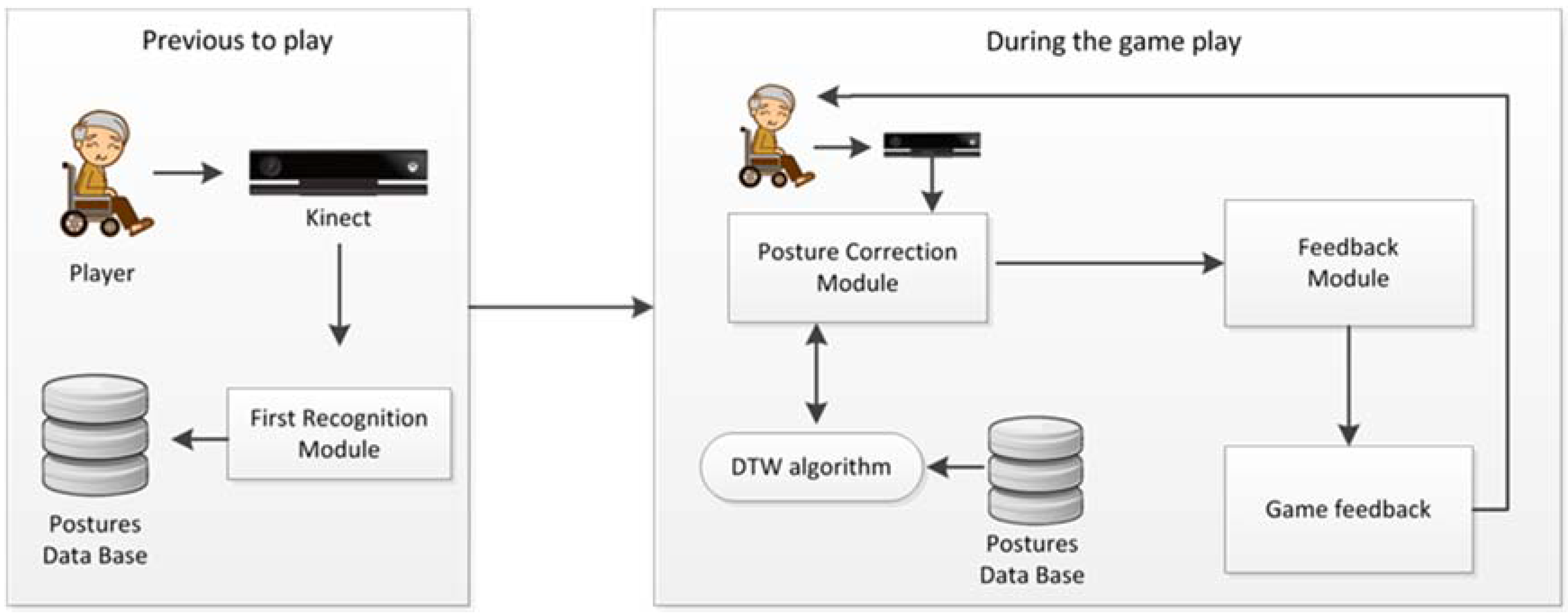
3.3. Corporal Posture Correction System
3.3.1. First Recognition Module
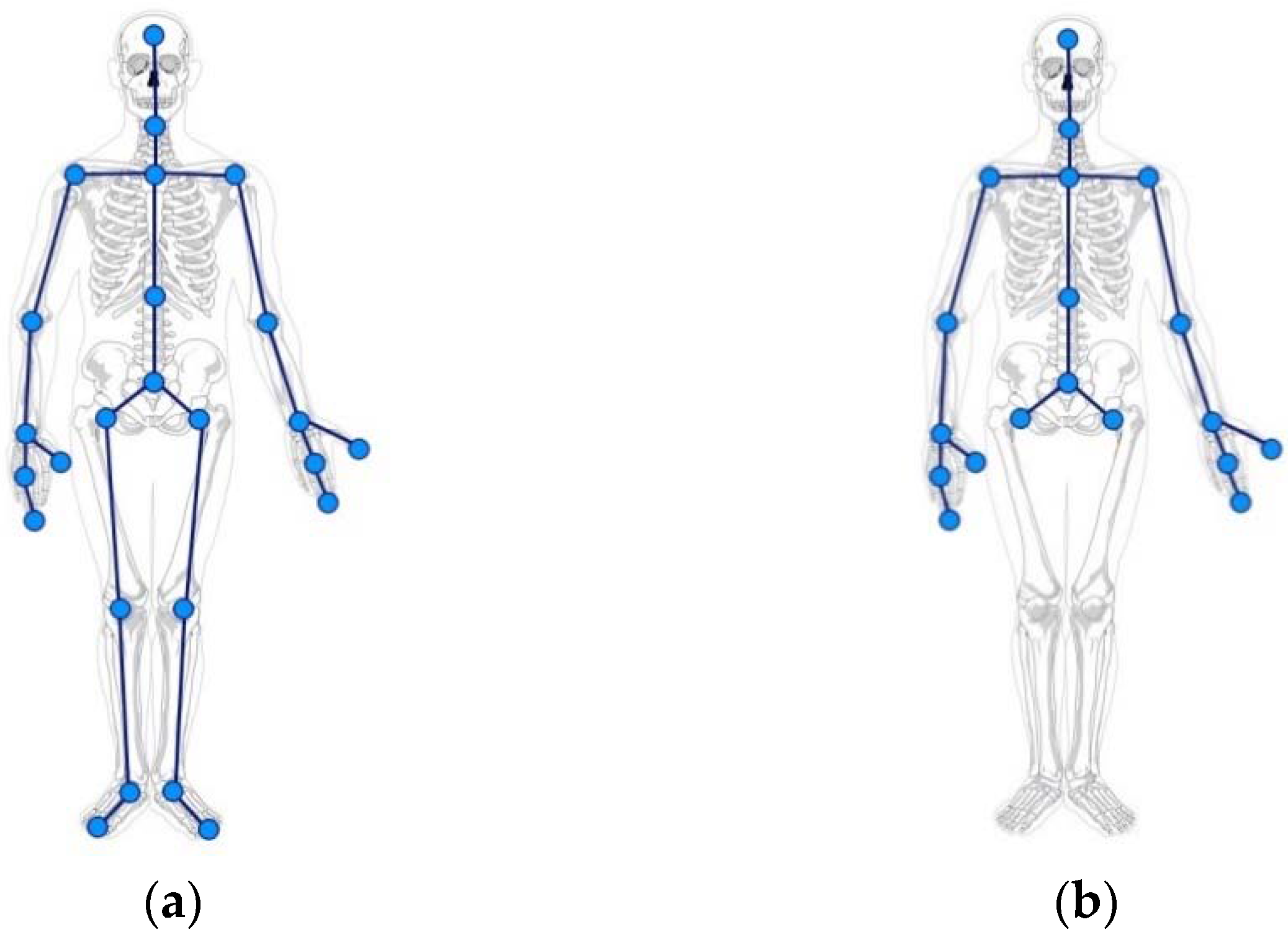
3.3.2. Posture Correction Module
DTW Algorithm
Node Data Normalization
3.3.3. Feedback module
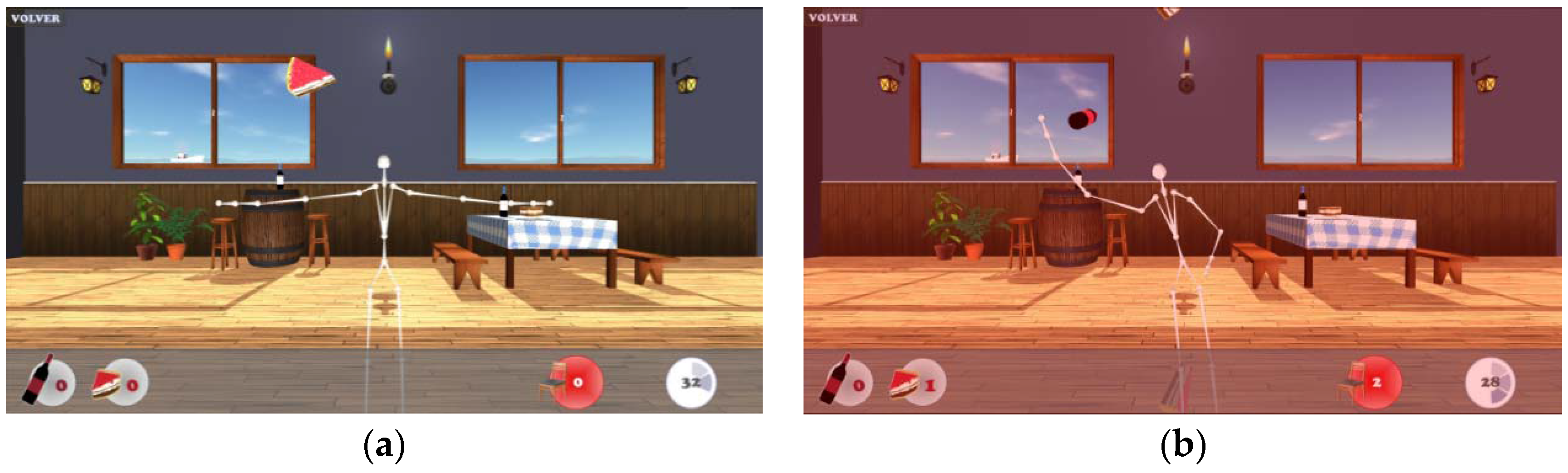
3.4. Game System Overview
- At the beginning of the game, users will be asked to enter their name, which will be referenced in the scores in order to store any related information during the gameplay. Also, the settings options can be configured.
- Then, the First Recognition Module explained above is run, and the user’s original posture is stored.
- The game starts with the first level and the user must collect all the objects appearing on the screen. Here, the Posture Correction Module is running and checks continuously whether the user posture deviates from the original one. If this action takes place, the game subtracts points from the total, obtaining more points if the object has been collected using correct posture.
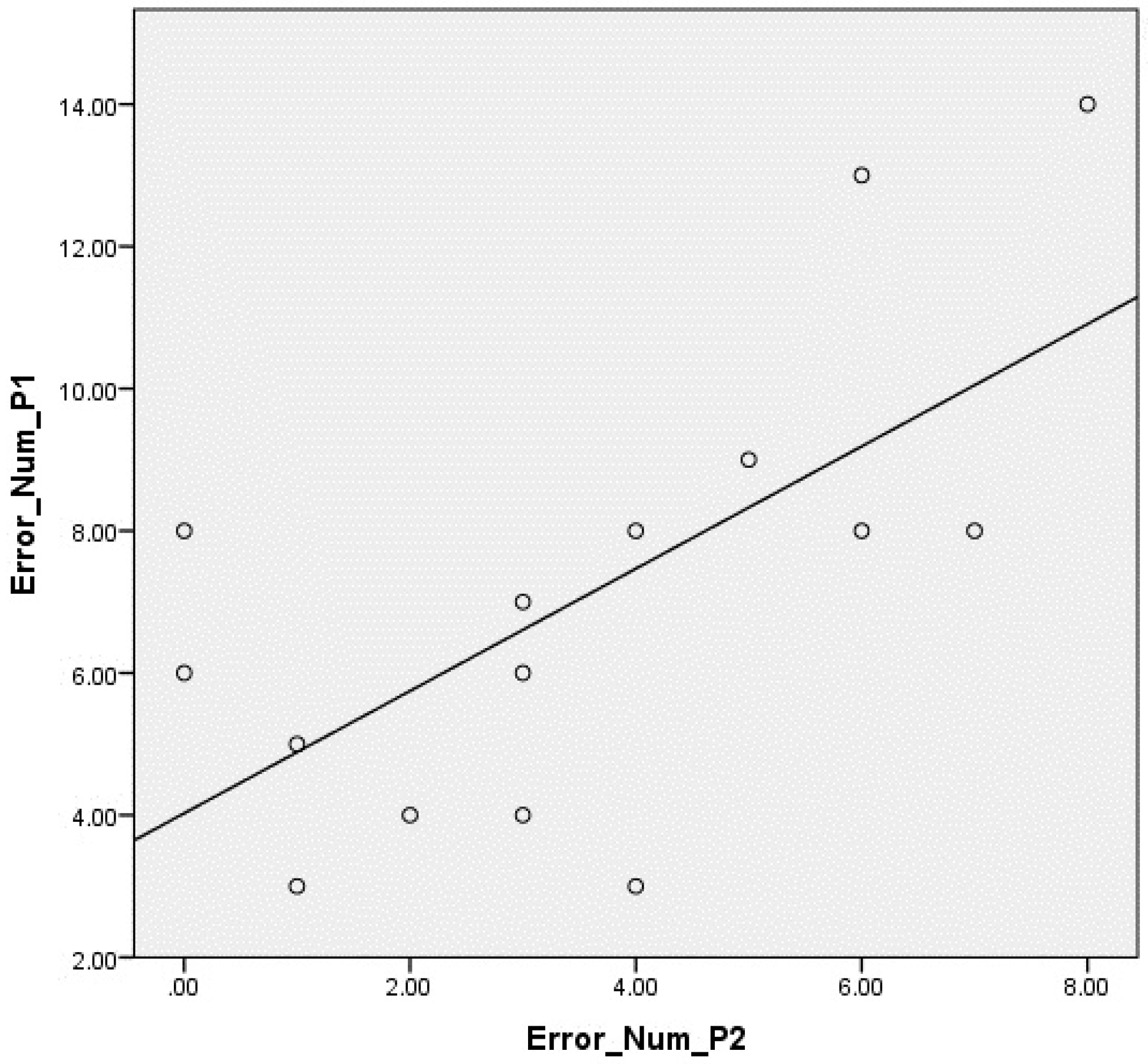
4. Results
Game Usability Scale Questionnaire
5. Conclusions and Further Research
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kamitani, K.; Michikawa, T.; Iwasawa, S.; Eto, N.; Tanaka, T.; Takebayashi, T.; Nishiwaki, Y. Spinal posture in the sagittal plane is associated with future dependence in activities of daily living: A community-based cohort study of older adults in Japan. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, J.D.; Côté, P.; Carroll, L.J.; Kristman, V. Incidence and course of low back pain episodes in the general population. Spine 2005, 30, 2817–2823. [Google Scholar] [CrossRef] [PubMed]
- Thiese, M.S.; Hegmann, K.T.; Wood, E.M.; Garg, A.; Moore, J.S.; Kapellusch, J.; Foster, J.; Ott, U. Prevalence of low back pain by anatomic location and intensity in an occupational population. BMC Musculoskelet. Disord. 2014, 15. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.M.S.; Casarotto, R.A.; João, S.M.A. Effects of educational sessions on school backpack use among elementary school students. Braz. J. Phys. Ther. 2008, 12, 447–453. [Google Scholar] [CrossRef]
- Vidal, J.; Borràs, P.A.; Ponseti, F.J.; Cantallops, J.; Ortega, F.B.; Palou, P. Effects of a postural education program on school backpack habits related to low back pain in children. Eur. Spine J. 2013, 22, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Sandvik, L.; Erikssen, J.; Thaulow, E.; Erikssen, G.; Mundal, R.; Rodahl, K. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N. Engl. J. Med. 1993, 328, 533–537. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Kronmal, R.A.; Newman, A.B.; Bild, D.E.; Mittelmark, M.B.; Polak, J.F.; Robbins, J.A.; Gardin, J.M. Risk factors for 5-year mortality in older adults. JAMA 1998, 279, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Rockhill, B.; Willett, W.C.; Manson, J.E.; Leitzmann, M.F.; Stampfer, M.J.; Hunter, D.J.; Colditz, G.A. Physical activity and mortality: A prospective study among women. Am. J. Public Health 2001, 91, 578–583. [Google Scholar] [PubMed]
- Woodard, C.; Berry, M. Enhancing adherence to prescribed exercise: Structured behavioral interventions in clinical exercise programs. J. Cardiopulm. Rehabil. 2001, 21, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Allaire, J.C.; McLaughlin, A.C.; Trujillo, A.; Whitlock, L.A.; LaPorte, L.; Gandy, M. Successful aging through digital games: Socioemotional differences between older adult gamers and non-gamers. Comput. Hum. Behav. 2013, 29, 1302–1306. [Google Scholar] [CrossRef]
- Kharrazi, H.; Shirong, A.; Gharghabi, F.; Coleman, W. A scoping review of health game research: Past, present, and future. Games Health J. 2012, 1, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Lin, J.; Crouse, J. Is playing exergames really exercising? A meta-analysis of energy expenditure in active video games. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Webster, D.; Celik, O. Systematic review of Kinect applications in elderly care and stroke rehabilitation. J. NeuroEng. Rehabil. 2014, 11. [Google Scholar] [CrossRef] [PubMed]
- Gerling, K.M.; Masuch, M. When Gaming is not suitable for everyone: Playtesting wii games with frail elderly. In Proceedings of the 1st Workshop on Game Accessibility: Xtreme Interaction Design (FDG 2011), Bordeaux, France, 28 June 2011.
- Liao, Y.; Yang, Y.; Wu, Y.; Wang, R. Virtual reality-based wii fit training in improving muscle strength, sensory integration ability, and walking abilities in patients with parkinson’s disease: A randomized control trial. Int. J. Gerontol. 2015, 9, 190–195. [Google Scholar] [CrossRef]
- Chang, C.Y.; Lange, B.; Zhang, M.; Koenig, S.; Requejo, P.; Somboon, N.; Sawchuk, A.A.; Rizzo, A.A. Towards pervasive physical rehabilitation using Microsoft Kinect. In Proceedings of the 6th International Conference on Pervasive Computing Technologies for Healthcare (Pervasive Health 2012), San Diego, CA, USA, 21–24 May 2012; pp. 159–162.
- Clark, R.A.; Pua, Y.H.; Fortin, K.; Ritchie, C.; Webster, K.E.; Denehy, L.; Bryant, A.L. Validity of the Microsoft Kinect for assessment of postural control. Gait Posture 2012, 36, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Obdrzalek, S.; Kurillo, G.; Ofli, F.; Bajcsy, R.; Seto, E.; Jimison, H.; Pavel, M. Accuracy and robustness of Kinect pose estimation in the context of coaching of elderly population. In Proceedings of the 2012 Annual International IEEE Conference, Engineering in Medicine and Biology Society (EMBC), San Diego, CA, USA, 28 August–1 September 2012; pp. 1188–1193.
- Fernandez-Baena, A.; Susin, A.; Lligadas, X. Biomechanical validation of upper-body and lower-body joint movements of Kinect motion capture data for rehabilitation treatments. In Proceedings of the 2012 Fourth International Conference on Intelligent Networking and Collaborative Systems, Bucharest, Romania, 19–21 September 2012; pp. 656–661.
- González-Ortega, D.; Díaz-Pernas, F.J.; Martínez-Zarzuela, M.; Antón-Rodríguez, M. A Kinect-based system for cognitive rehabilitation exercises monitoring. Comput. Methods Programs Biomed. 2014, 113, 620–631. [Google Scholar] [CrossRef] [PubMed]
- Pagliari, D.; Pinto, L. Calibration of kinect for xbox one and comparison between the two generations of Microsoft sensors. Sensors 2015, 15, 27569–27589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holden, M.K. Virtual environments for motor rehabilitation: Review. Cyberpsychol. Behav. 2005, 8, 187–211. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.J.; Han, W.Y.; Tsai, Y.C. A Kinect-based upper limb rehabilitation system to assist people with cerebral palsy. Res. Dev. Disabil. 2013, 34, 3654–3659. [Google Scholar] [CrossRef] [PubMed]
- Pastor, I.; Hayes, H.A.; Bamberg, S.J. A feasibility study of an upper limb rehabilitation system using Kinect and computer games. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), San Diego, CA, USA, 28 August–1 September 2012.
- McConville, K.V. Virtual rehabilitation and training for postural balance and neuromuscular control. In Virtual Reality in Psychological, Medical and Pedagogical Applications; Eichenberg, C., Ed.; InTech: Rijeka, Croatia, 2012. [Google Scholar]
- Carmichael, A.; Rice, M.; MacMillan, F.; Kirk, A. Investigating a DTV-based physical activity application to facilitate wellbeing in older adults. In Proceedings of the 24th BCS Interaction Specialist Group Conference, Dundee, UK, 6–10 September 2010.
- Rice, M.; Tan, W.P.; Ong, J.; Yau, L.J.; Wan, M.; Ng, J. The dynamics of younger and older adult's paired behavior when playing an interactive silhouette game. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Paris, France, 27 April–2 May 2013; pp. 1081–1090.
- Smeddinck, J.D.; Herrlich, M.; Malaka, R. Exergames for physiotherapy and rehabilitation: A medium-term situated study of motivational aspects and impact on functional reach. In Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems, Seoul, Korea, 18–23 April 2015; pp. 4143–4146.
- Tang, R.; Yang, X.D.; Bateman, S.; Jorge, J.; Tang, A. Physio@ Home: Exploring visual guidance and feedback techniques for physiotherapy exercises. In Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems, Seoul, Korea, 18–23 April 2015; pp. 4123–4132.
- Suárez, H.; Suárez, A.; Lavinsky, L. Postural adaptation in elderly patients with instability and risk of falling after balance training using a virtual-reality system. Int. Tinnitus J. 2006, 12, 41–44. [Google Scholar] [PubMed]
- Posture Minder. Available online: http://www.postureminder.co.uk/ (accessed on 11 January 2016).
- Kopaničáková, A.; Virčíková, M. Gesture Recognition Using DTW and Its Application Potential in Human-Centered Robotics. Available online: http://neuron.tuke.sk/maria.vircik/phd/files/documents/publications/Gesture%20Recognition%20using%20DTW%20and%20its%20Application%20Potential%20in%20Human-Centered%20Robotics.pdf (accessed on 13 May 2016).
- Jangyodsuk, P.; Conly, C.; Athitsos, V. Sign language recognition using dynamic time warping and hand shape distance based on histogram of oriented gradient features. In Proceedings of the 7th International Conference on PErvasive Technologies Related to Assistive Environments, Rhodes, Greece, 27–30 May 2014.
- Hyeon-Kyu, L.; Kim, J.H. An HMM-based threshold model approach for gesture recognition. IEEE Trans. Pattern Anal. Mach. Intell. 1999, 21, 961–973. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, C.; Wu, X.; Xu, S.; Li, H. Kinect based dynamic hand gesture recognition algorithm research. In Proceedings of the 4th International Conference on Intelligent Human-Machine Systems and Cybernetics (IHMSC), Nanchang, China, 26–27 August 2012; pp. 274–279.
- Fels, S.S.; Hinton, G.E. Glove-TalkII-a neural-network interface which maps gestures to parallel formant speech synthesizer controls. IEEE Trans. Neural Netw. 1998, 9, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Feng, H.; Lun, R.; Espy, D.D.; Reinthal, M. A Kinect-based rehabilitation exercise monitoring and guidance system. In Proceedings of the 5th IEEE International Conference on Software Engineering and Service Science (ICSESS), Beijing, China, 27–29 June 2014; pp. 762–765.
- Zhao, W.; Lun, R.; Espy, D.D.; Reinthal, M. Rule based realtime motion assessment for rehabilitation exercises. In Proceedings of the IEEE Symposium on Computational Intelligence in Healthcare and E-Health (CICARE), Orlando, FL, USA, 9–12 December 2014; pp. 133–140.
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Minimental State”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Li, Z.X.; Zhang, F.M.; Li, K.W. DTW based pattern matching method for multivariate time series. Pattern Recognit. Artif. Intell. 2011, 24, 425–430. [Google Scholar]
- Sáenz-de-Urturi, Z.; García Zapirain, B.; Méndez Zorrilla, A. Elderly user experience to improve a Kinect-based game playability. Behav. Inf. Technol. 2015, 34, 1040–1051. [Google Scholar] [CrossRef]
- Gerling, K.; Livingston, I.; Nacke, L.; Mandryk, R. Full-body motion-based game interaction for older adults. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Austin, TX, USA, 5–10 May 2012; pp. 1873–1882.
- Brooke, J. SUS: A quick and dirty usability scale. In Usability Evaluation in Industry; Jordan, P.W.B., Weerdmeester, A., Thomas, M.I.L., Eds.; Taylor & Francis: London, UK, 1996; pp. 189–194. [Google Scholar]
- Nacke, L.; Schild, J.; Niesenhaus, J. Gameplay experience testing with playability and usability surveys—An experimental pilot study. In Proceedings of the Fun and Games 2010 Workshop, NHTV Expertise Series 10 Workshop Paper: Playability and Player Experience, Leuven, Belgium, 15–17 September 2010; pp. 31–45.
- Tullis, T.; Albert, B. Measuring the User Experience: Collecting, Analyzing, and Presenting Usability Metrics. Burlington; Morgan Kaufmann: Burlington, MA, USA, 2008. [Google Scholar]
| No. Part. | Age | Sex | Disability | MMSE Level | MMSE Score |
|---|---|---|---|---|---|
| 1 | 84 | M | Muscular Dystrophy | Mild | 22 |
| 2 | 77 | M | Macular degeneration | Normal | 26 |
| 3 | 69 | M | Macular degeneration | Normal | 27 |
| 4 | 85 | M | None | Mild | 20 |
| 5 | 74 | M | None | Normal | 24 |
| 6 | 82 | F | None | Normal | 25 |
| 7 | 89 | F | Presbyopia | Mild | 21 |
| 8 | 96 | F | None | Normal | 26 |
| 9 | 73 | F | Muscular Dystrophy | Normal | 27 |
| 10 | 87 | F | Parkinson | Moderate | 19 |
| 11 | 84 | F | None | Normal | 25 |
| 12 | 94 | F | Presbyopia | Mild | 20 |
| 13 | 87 | F | Muscular Dystrophy | Normal | 24 |
| 14 | 85 | F | None | Normal | 27 |
| 15 | 88 | F | None | Normal | 24 |
| No. Part. | Incorrect Postures Mean | Mean of Incorrect Postures Detected | Mean of Incorrect Postures Not Detected |
|---|---|---|---|
| 1 | 4 | 4 | 0 |
| 2 | 9.5 | 9.5 | 0 |
| 3 | 5 | 5 | 0 |
| 4 | 12 | 11 | 1 |
| 5 | 7 | 7 | 0 |
| 6 | 2 | 2 | 0 |
| 7 | 6 | 6 | 0 |
| 8 | 8 | 7 | 1 |
| 9 | 4.5 | 4.5 | 0 |
| 10 | 3.5 | 3.5 | 0 |
| 11 | 3 | 3 | 0 |
| 12 | 9 | 7.5 | 1.5 |
| 13 | 4 | 3.5 | 0.5 |
| 14 | 3 | 3 | 0 |
| 15 | 3 | 3 | 0 |
| Total | 83.5 | 79.5 (95.20%) | 4 (4.79%) |
| Num_Object1_P2 and Num_Object1_P1 | Num_Object2_P2 and Num_Object2_P1 | Num_Errores_P2 and Num_Errores_P1 | Tilt_P2 and Tilt_P1 |
|---|---|---|---|
| Z = −2.370 | Z = −2.422 | Z = −3.307 | Z = −1.000 |
| p = 0.018 | p = 0.015 | p = 0.001 | p = 0.317 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saenz-de-Urturi, Z.; Garcia-Zapirain Soto, B. Kinect-Based Virtual Game for the Elderly that Detects Incorrect Body Postures in Real Time. Sensors 2016, 16, 704. https://doi.org/10.3390/s16050704
Saenz-de-Urturi Z, Garcia-Zapirain Soto B. Kinect-Based Virtual Game for the Elderly that Detects Incorrect Body Postures in Real Time. Sensors. 2016; 16(5):704. https://doi.org/10.3390/s16050704
Chicago/Turabian StyleSaenz-de-Urturi, Zelai, and Begonya Garcia-Zapirain Soto. 2016. "Kinect-Based Virtual Game for the Elderly that Detects Incorrect Body Postures in Real Time" Sensors 16, no. 5: 704. https://doi.org/10.3390/s16050704







