Comparative Solid-State Stability of Perindopril Active Substance vs. Pharmaceutical Formulation
Abstract
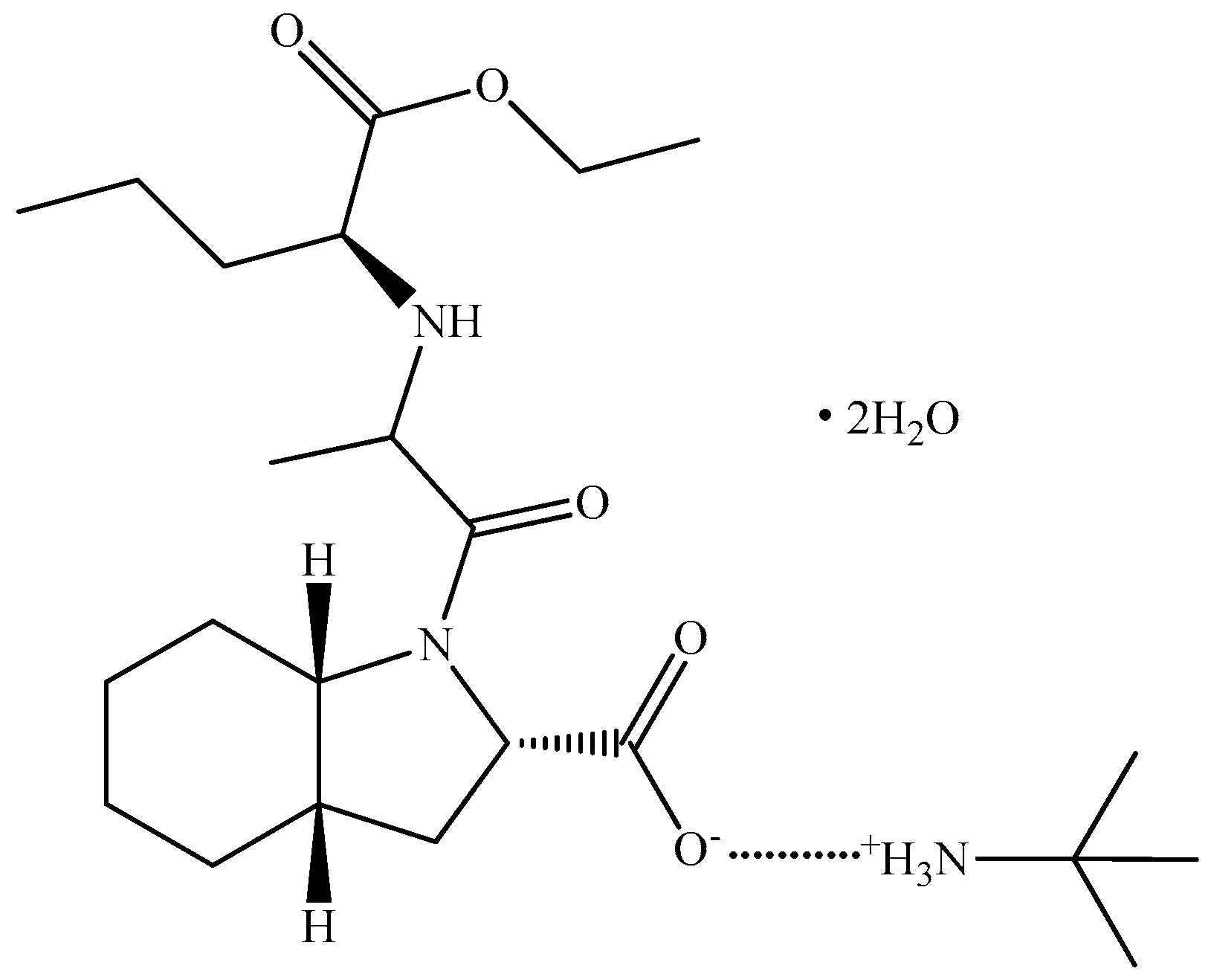
:1. Introduction
2. Results
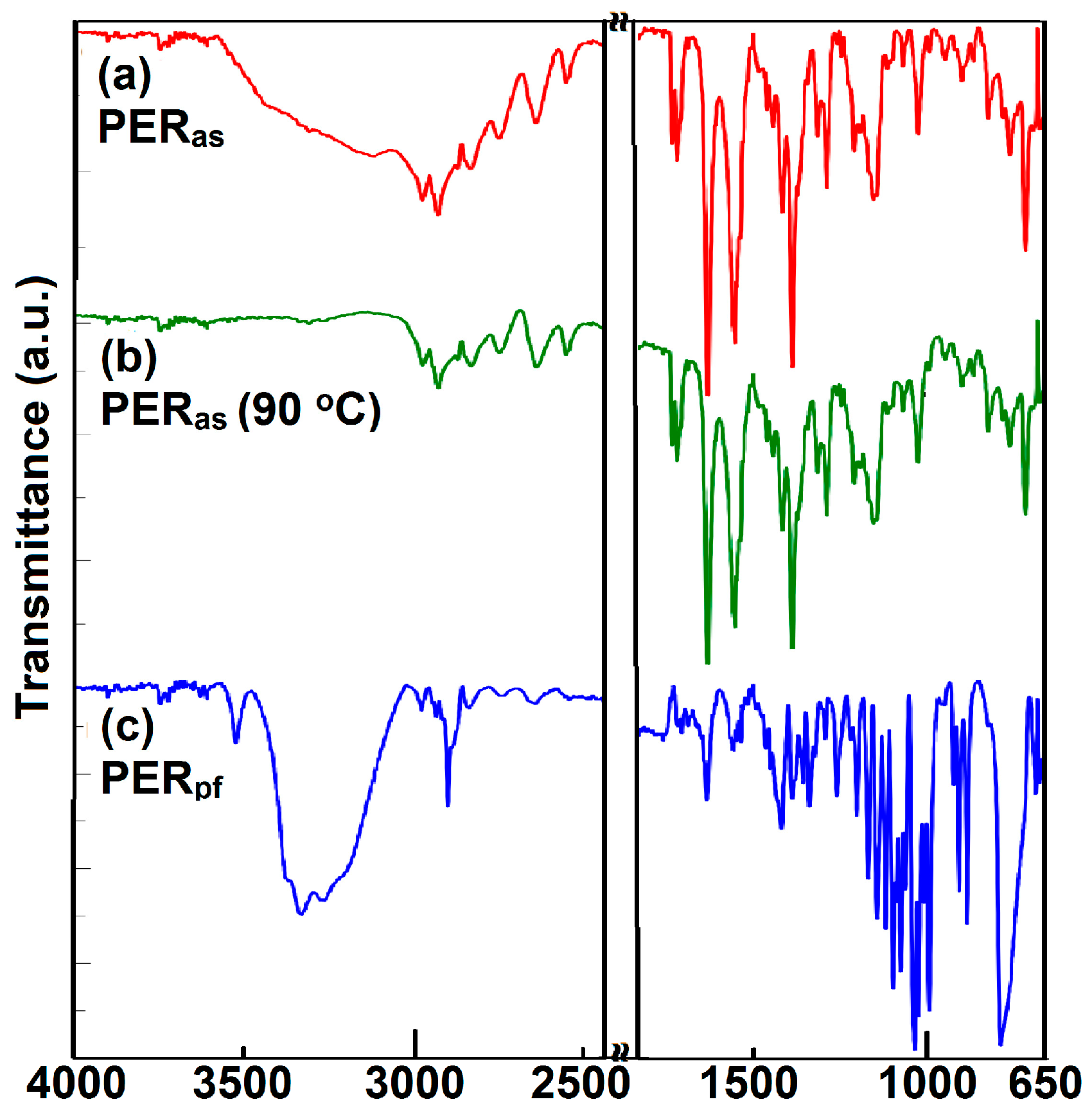
2.1. ATR-FTIR Investigations
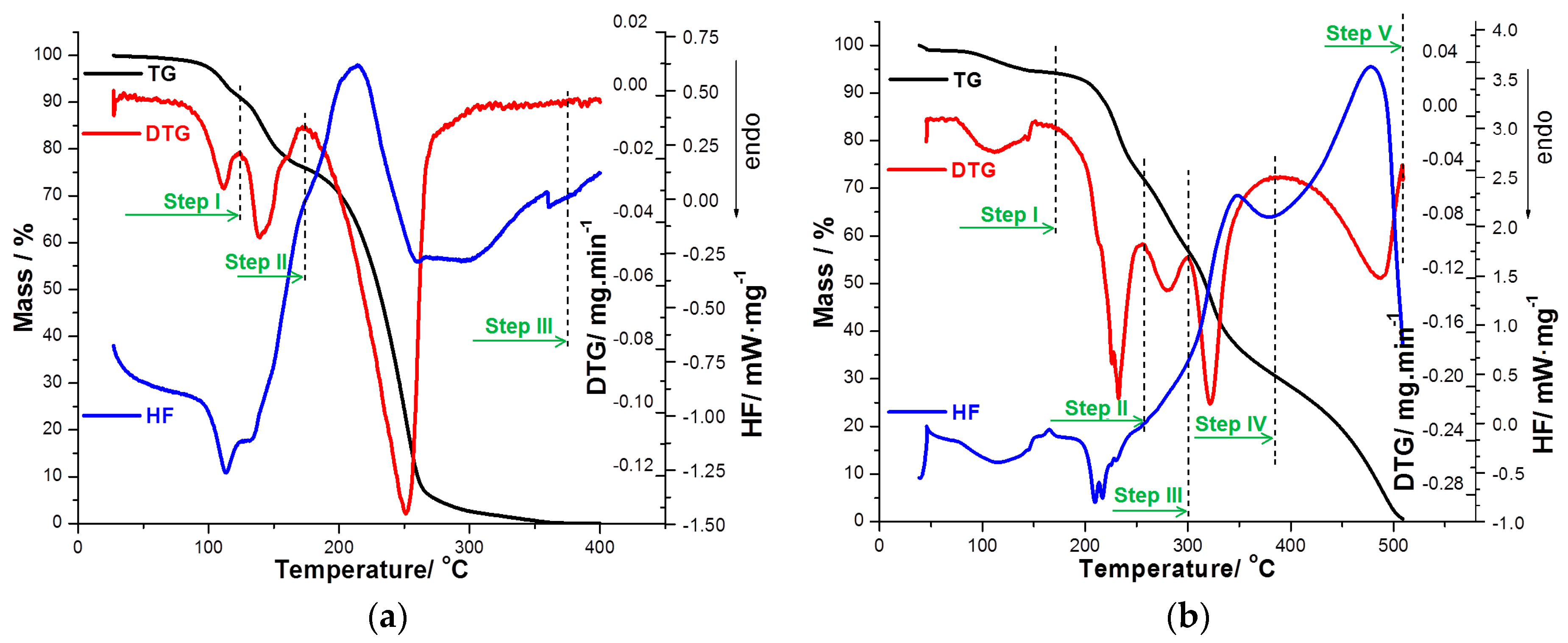
2.2. Thermal Stability Investigations
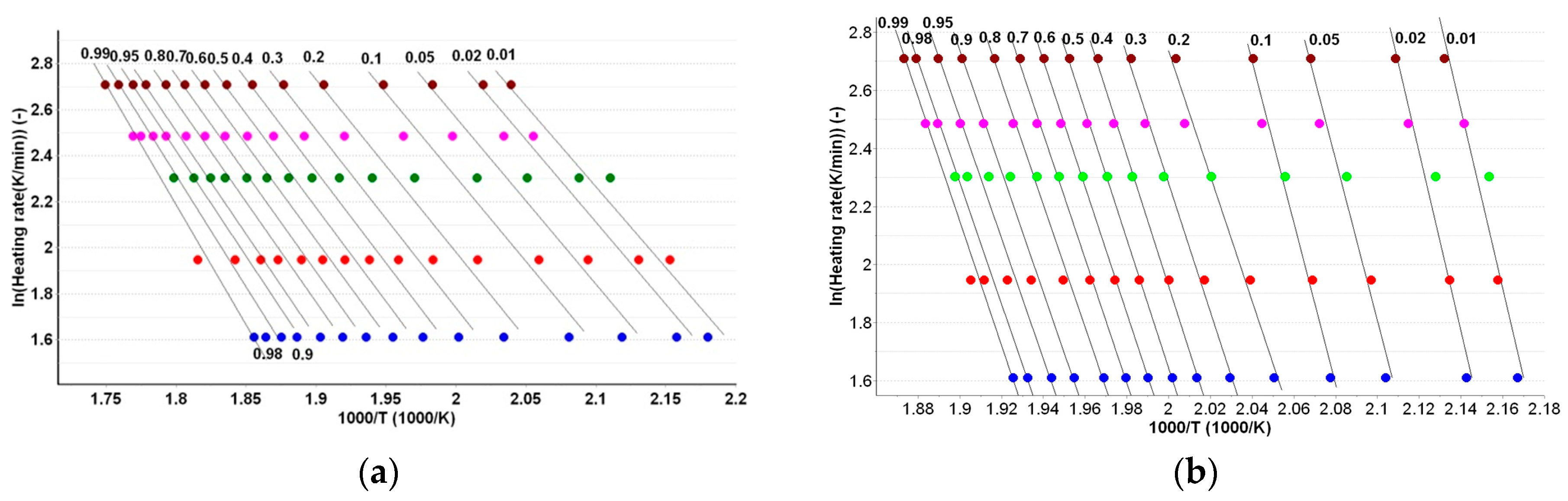
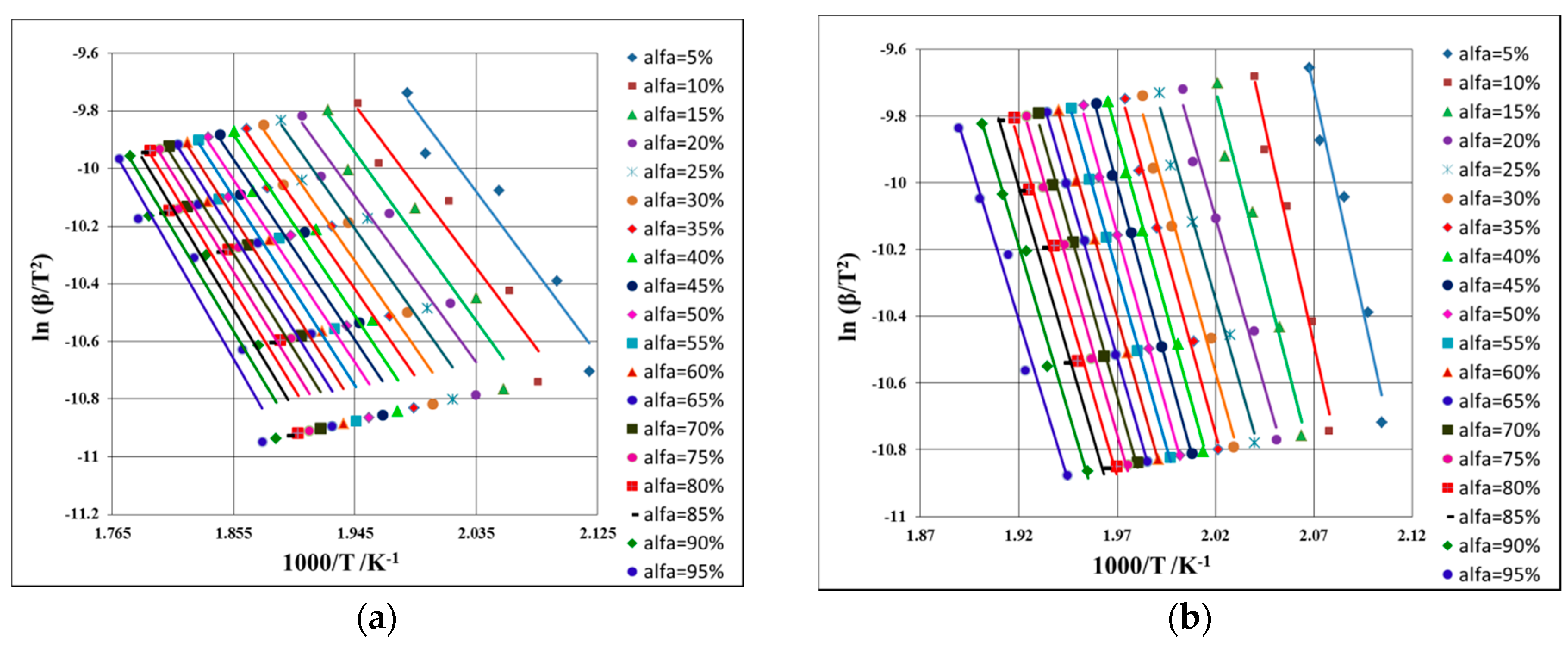
2.3. Kinetic Study
3. Discussion
3.1. ATR-FTIR Investigations
3.2. Thermal Stability Investigations
3.3. Kinetic Study
4. Materials and Methods
4.1. Samples and Preparation
4.2. Spectroscopic Investigations
4.3. Thermal Stability Investigations
4.4. Kinetic Study
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hanif, K.; Bid, K.H.; Konwar, R. Reinventing the ACE inhibitors: Some old and new implications of ACE inhibition. Hypertens. Res. 2010, 33, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Bohm, M.; Christiaens, T.; Cifkova, R.; de Backer, G.; Dominiczak, A.; et al. Task force for the management of arterial hypertension of the European society of hypertension and the European society of cardiology. 2013 ESH/ESC guidelines for the management of arterial hypertension. Eur. Heart J. 2013, 34, 2159–2219. [Google Scholar] [PubMed]
- Fox, K. Contribution of perindopril to cardiology: 20 years of success. Eur. Heart J. 2007, 9, E10–E19. [Google Scholar] [CrossRef]
- Tantu, M.; Belu, E.; Bobescu, E.; Armean, S.M.; Armean, P.; Constantin, M.M.; Dominaru, C.D. Role of angiotensin converting enzyme (ACE) inhibitors in hypertension and cardiovascular protection management. Farmacia 2014, 62, 451–459. [Google Scholar]
- Cockcroft, J.R. ACE inhibition in hypertension: Focus on perindopril. Am. J. Cardiovasc. Drugs 2007, 7, 3003–3017. [Google Scholar] [CrossRef]
- Louis, W.J.; Conway, E.L.; Krum, H.; Workman, B.; Drummer, O.H.; Lam, W.; Phillips, P.; Howes, L.G.; Jackson, B. Comparison of the pharmacokinetics and pharmacodynamics of perindopril, cilazapril and enalapril. Clin. Exp. Pharmacol. Physiol. Suppl. 1992, 19, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, R. Angiotensin-converting enzyme inhibition in cardiovascular disease evidence with perindopril. Expert Rev. Cardiovasc. Ther. 2005, 3, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Louis, W.J.; Workman, B.S.; Conway, E.L.; Worland, P.; Rowley, K.; Drummer, O.; McNeil, J.J.; Harris, G.; Jarrott, B. Single-dose and steady-state pharmacokinetics and pharmacodynamics of perindopril in hypertensive subjects. J. Cardiovasc. Pharmacol. 1992, 20, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Turlapaty, P.; Shen, Y.; Dong, V.; Batchelor, A.; Barlow, D.; Lagast, H. Clinical experience with perindopril in patients nonresponsive to previous antihypertensive therapy: A large US community trial. Am. J. Ther. 2004, 11, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Julius, S.; Cohn, J.N.; Neutel, J.; Weber, M.; Turlapaty, P.; Shen, Y.; Dong, V.; Batchelor, A.; Lagast, H. Antihypertensive utility of perindopril in a large, general practice-based clinical trial. J. Clin. Hypertens. 2004, 6, 10–17. [Google Scholar] [CrossRef]
- London, G.M.; Pannier, B.; Guerin, A.P.; Marchais, S.J.; Safar, M.E.; Cuche, J.L. Cardiac hypertrophy, aortic compliance, peripheral resistance, and wave reflection in end-stage renal disease. Comparative effects of ACE inhibition and calcium channel blockade. Circulation 1994, 90, 2786–2796. [Google Scholar] [CrossRef] [PubMed]
- Guerin, A.P.; Blacher, J.; Pannier, B.; Marchais, S.J.; Safar, M.E.; London, G.M. Impact of aortic stiffness attenuation on survival of patients in endstage renal failure. Circulation 2001, 103, 987–992. [Google Scholar] [CrossRef] [PubMed]
- PROGRESS Collaborative Group. Randomised trial of a perindoprilbased blood-pressure-lowering regimen among 6105 individuals with previous stroke or transient ischaemic attack. Lancet 2001, 358, 1033–1041. [Google Scholar]
- Fox, K.M. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: Randomised, double-blind, placebo-controlled, multicentre trial (the EUROPA study). Lancet 2003, 362, 782–788. [Google Scholar] [PubMed]
- Ceconi, C.; Fox, K.M.; Remme, W.J.; Simoons, M.L.; Bertrand, M.; Parrinello, G.; Kluft, C.; Blann, A.; Cokkinos, D.; Ferrari, R. EUROPA Investigators; PERTINENT Investigators and the Statistical Committee. ACE inhibition with perindopril and endothelial function. Results of a substudy of the EUROPA study: PERTINENT. Cardiovasc. Res. 2007, 73, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Buda, V.; Andor, M.; Cristescu, C.; Voicu, M.; Suciu, L.; Suciu, M.; Tomescu, M. Blockers of the RAA system: Perindopril and candesartan and their implication on endothelial dysfunction. Med. Evol. 2014, 3, 509–517. [Google Scholar]
- Buda, V.; Tomescu, M.; Cristescu, C. The relationship between the bradykinins, RAAS and ACE inhibitors: An overview. Med. Evol. 2014, 2, 301–309. [Google Scholar]
- Buda, V.; Andor, M.; Cristescu, C.; Voicu, M.; Suciu, L.; Muntean, C.; Cretu, O.; Baibata, D.E.; Gheorghiu, C.M.; Tomescu, M.C. The influence of perindopril on PTX3 plasma levels in hypertensive patients with endothelial dysfunction. Farmacia 2016, 64, 382–389. [Google Scholar]
- Patel, A.; ADVANCE Collaborative Group; MacMahon, S.; Chalmers, J.; Neal, B.; Woodward, M.; Billot, L.; Harrap, S.; Poulter, N.; Marre, M.; et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): A randomised controlled trial. Lancet 2007, 370, 829–840. [Google Scholar] [PubMed]
- Amenta, F.; Mignini, F.; Rabbia, F.; Tomassoni, D.; Veglio, F. Protective effect of antihypertensive treatment on cognitive function in essential hypertension: Analysis of published clinical data. J. Neurol. Sci. 2002, 203–204, 147–151. [Google Scholar] [CrossRef]
- Gumieniczek, A.; Maczka, P.; Komsta, L.; Pietras, R. Dissolution profiles of perindopril and indapamide in their fixed-dose formulations by a new HPLC method and different mathematical approaches. Acta Pharm. 2015, 65, 235–252. [Google Scholar] [CrossRef] [PubMed]
- Dorniani, D.; Hussein, M.Z.B.; Kura, A.U.; Fakurazi, S.; Shaari, A.H.; Ahmad, Z. Sustained release of prindopril erbumine from its chitosan-coated magnetic nanoparticles for biomedical applications. Int. J. Mol. Sci. 2013, 14, 23639–23653. [Google Scholar] [CrossRef] [PubMed]
- Bouabdallah, S.; Trabelsi, H.; Ben Dhia, M.T.; Ben Hamida, N. Kinetic Study on the Isomerization of Perindopril by HPLC. Chromatographia 2012, 75, 1247–1255. [Google Scholar] [CrossRef]
- Simoncic, Z.; Rokar, R.; Gartner, A.; Kogej, K.; Kmetec, V. The use of microcalorimetry and HPLC for the determination of degradation kinetics and thermodynamic parameters of Perindopril Erbumine in aqueous solutions. Int. J. Pharm. 2008, 356, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Rahman, N.; Anwar, N.; Kashif, M. Optimized and validated initial-rate method for the determination of perindopril erbumine in tablets. Chem. Pharm. Bull. 2006, 54, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Macedo, R.O.; do Nascimento, T.G.; Aragao, C.F.S.; Gomes, A.P.B. Application of thermal analysis in the characterization of anti-hypertensive drugs. J. Therm. Anal. Calorim. 2000, 59, 657–661. [Google Scholar] [CrossRef]
- Ambrozini, B.; Cervini, P.; Cavalheiro, E.T.G. Thermal behavior of the β-blocker propranolol. J. Therm. Anal. Calorim. 2016, 123, 1013–1017. [Google Scholar] [CrossRef]
- Silva, A.C.M.; Galico, D.A.; Guerra, R.B.; Perpetuo, G.L.; Legendre, A.O.; Rinaldo, D.; Bannach, G. Thermal stability and thermal decomposition of the antihypertensive drug amlodipine besylate. J. Therm. Anal. Calorim. 2015, 120, 889–892. [Google Scholar] [CrossRef]
- Andre, V.; Cunha-Silva, L.; Duarte, M.T.; Santos, P.P. First crystal structures of the antihypertensive drug perindopril erbumine: A novel hydrated form and polymorphs α and β. Cryst. Growth Des. 2011, 11, 3703–3706. [Google Scholar] [CrossRef]
- Budrugeac, P.; Segal, E. Applicability of the Kissinger equation in thermal analysis. J. Therm. Anal. Calorim. 2007, 88, 703–707. [Google Scholar] [CrossRef]
- Ledeti, I.; Vlase, G.; Ciucanu, I.; Olariu, T.; Fulias, A.; Suta, L.M.; Belu, I. Analysis of solid binary systems containing simvastatin. Rev. Chim.-Buchar. 2015, 66, 240–243. [Google Scholar]
- Fulias, A.; Vlase, G.; Vlase, T.; Suta, L.M.; Soica, C.; Ledeti, I. Screening and characterization of cocrystal formation between carbamazepine and succinic acid. J. Therm. Anal. Calorim. 2015, 121, 1081–1086. [Google Scholar] [CrossRef]
- Ivan, C.; Suta, L.M.; Olariu, T.; Ledeti, I.; Vlase, G.; Vlase, T.; Olariu, S.; Matusz, P.; Fulias, A. Preliminary kinetic study for heterogenous degradation of cholesterol-containing human biliary stones. Rev. Chim.-Buchar. 2015, 66, 1253–1255. [Google Scholar]
- Fulias, A.; Soica, C.; Ledeti, I.; Vlase, T.; Vlase, G.; Suta, L.M.; Belu, I. Characterization of pharmaceutical acetylsalicylic acid—theophylline cocrystal obtained by slurry method under microwave irradiation. Rev. Chim.-Buchar. 2014, 65, 1281–1284. [Google Scholar]
- Ilici, M.; Bercean, V.; Venter, M.; Ledeti, I.; Olariu, T.; Suta, L.M.; Fulias, A. Investigations on the thermal-induced degradation of transitional coordination complexes containing (3H-2-thioxo-1,3,4-thiadiazol-5-yl)thioacetate moiety. Rev. Chim.-Buchar. 2014, 65, 1142–1145. [Google Scholar]
- Ledeti, I.; Vlase, G.; Vlase, T.; Suta, L.M.; Todea, A.; Fulias, A. Selection of solid-state excipients for simvastatin dosage forms through thermal and nonthermal techniques. J. Therm. Anal. Calorim. 2015, 121, 1093–1102. [Google Scholar] [CrossRef]
- Fulias, A.; Vlase, G.; Ledeti, I.; Suta, L.M. Ketoprofen-cysteine equimolar salt. Synthesis, thermal analysis, PXRD and FTIR spectroscopy investigation. J. Therm. Anal. Calorim. 2015, 121, 1087–1091. [Google Scholar] [CrossRef]
- Ledeti, I.; Vlase, G.; Vlase, T.; Ciucanu, I.; Olariu, T.; Todea, A.; Fulias, A.; Suta, L.M. Instrumental analysis of potential lovastatin—Excipient interactions in preformulation studies. Rev. Chim.-Bucharest. 2015, 66, 879–882. [Google Scholar]
- Ledeti, I.; Vlase, G.; Vlase, T.; Fulias, A. Kinetic analysis of solid-state degradation of pure pravastatin versus pharmaceutical formulation. J. Therm. Anal. Calorim. 2015, 121, 1103–1110. [Google Scholar] [CrossRef]
- Ledeti, I.; Vlase, G.; Vlase, T.; Fulias, A.; Suta, L.M. Comparative thermal stability of two similar-structure hypolipidemic agents Simvastatin and Lovastatin-kinetic study. J. Therm. Anal. Calorim. 2016, 125, 769–775. [Google Scholar] [CrossRef]
- Ledeti, I.; Ledeti, A.; Vlase, G.; Vlase, T.; Matusz, P.; Bercean, V.; Suta, L.M.; Piciu, D. Thermal stability of synthetic thyroid hormone l-thyroxine and l-thyroxine sodium salt hydrate both pure and in pharmaceutical formulations. J. Pharm. Biomed. 2016, 125, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Ledeti, I.; Alexa, A.; Bercean, V.; Vlase, G.; Vlase, T.; Suta, L.M.; Fulias, A. Synthesis and degradation of schiff bases containing heterocyclic pharmacophore. Int. J. Mol. Sci. 2015, 16, 1711–1727. [Google Scholar] [CrossRef] [PubMed]
- Friedman, H.L. New methods for evaluating kinetic parameters from thermal analysis data. J. Polym. Sci. 1969, 7, 41–46. [Google Scholar] [CrossRef]
- Ozawa, T. A new method of analyzing thermogravimetric data. Bull. Chem. Soc. Jpn. 1965, 38, 1881–1886. [Google Scholar] [CrossRef]
- Flynn, J.H.; Wall, L.A. A quick direct method for determination of activation energy from thermogravimetric data. J. Polym. Sci. B 1966, 4, 323–328. [Google Scholar] [CrossRef]
- Kissinger, H.E. Reaction kinetics in differential thermal analysis. Anal. Chem. 1957, 29, 1702–1706. [Google Scholar] [CrossRef]
- Akahira, T.; Sunose, T. Joint convention of four electrical institutes. Researvh Report (Chiba Institute Technology). Sci. Technol. 1971, 16, 22–31. [Google Scholar]
- Rucman, R.; Zupet, P. New Hydrated Crystalline Forms of Perindopril Erbumine, Process for the Preparation thereof and Pharmaceutical Formulations Containing These Compounds. EP Patent App. EP20,050,468,015, 5 April 2006. [Google Scholar]
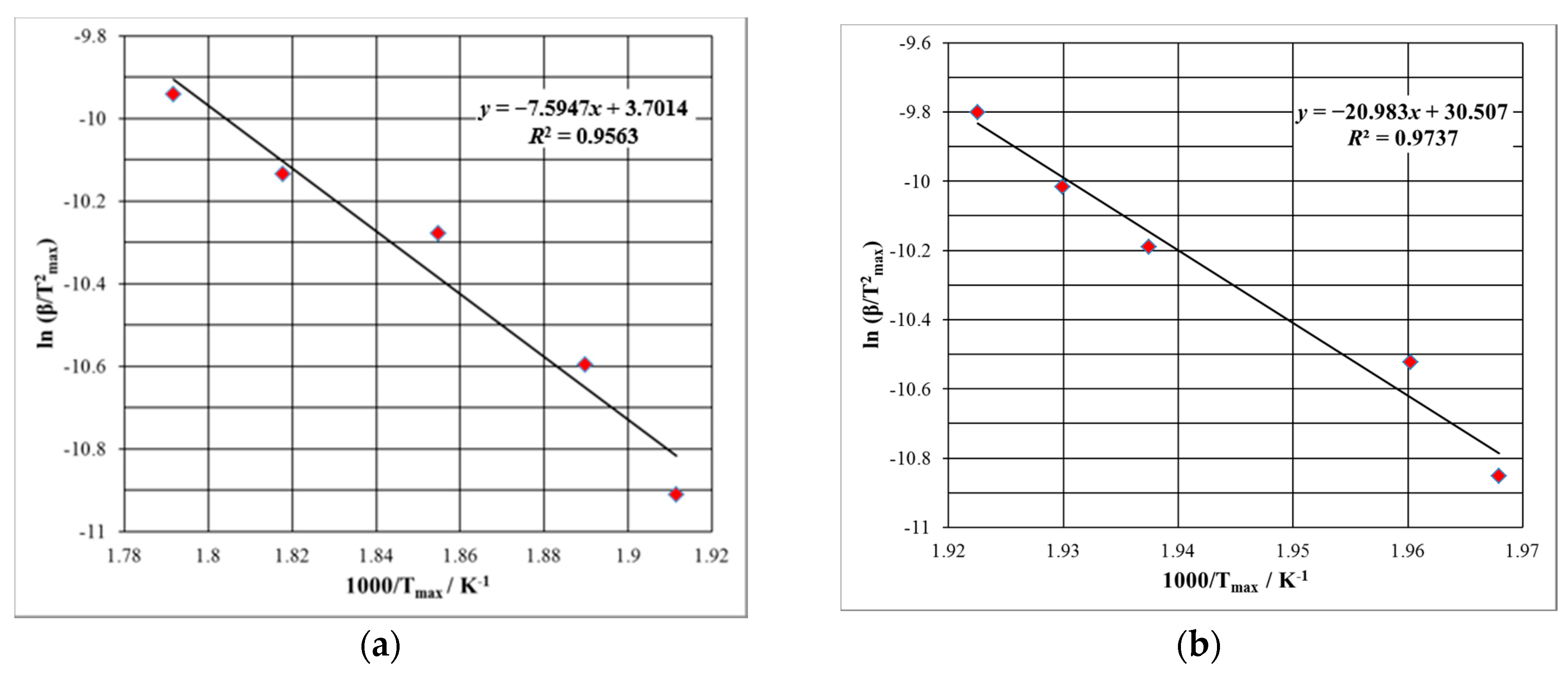
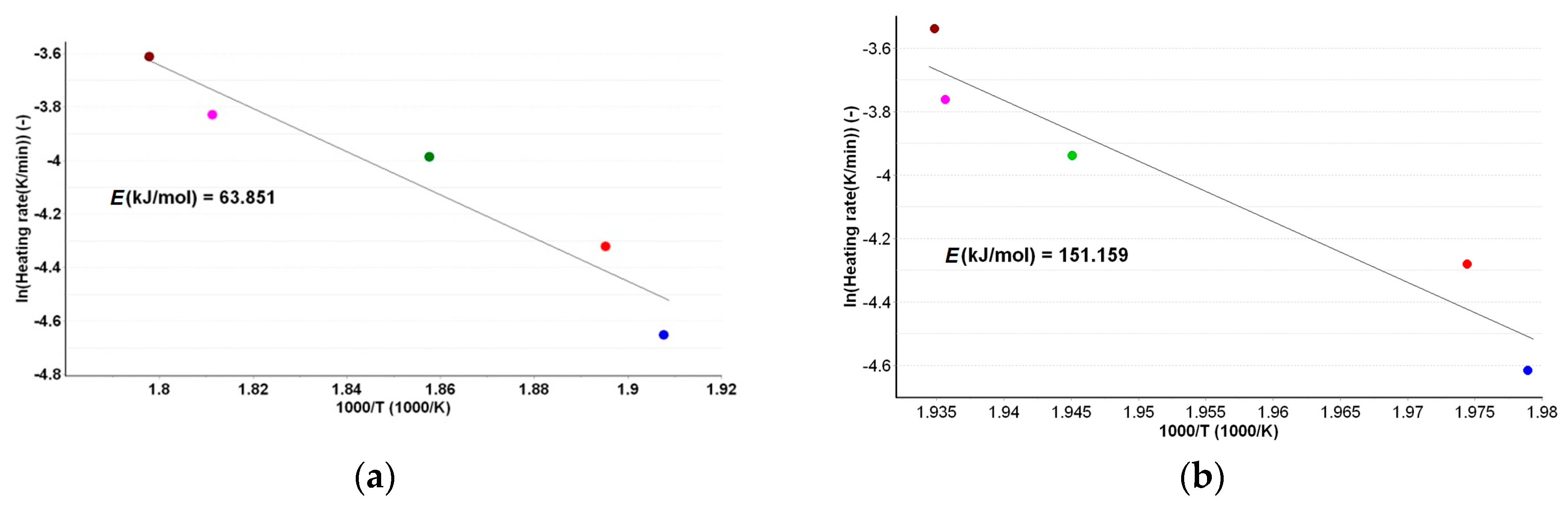


| Sample | Ea (kJ·mol−1) | |
|---|---|---|
| Kissinger | ASTM E698 | |
| PERas | 63.1 | 63.9 |
| PERpf | 174.5 | 151.2 |
| Conversion Degree α | Ea (kJ·mol−1) vs. α for PERas | Ea (kJ·mol−1) vs. α for PERpf | ||||
|---|---|---|---|---|---|---|
| Fr | KAS | FWO | Fr | KAS | FWO | |
| 0.05 | 59.6 | 54.1 | 59.2 | 190.6 | 178.2 | 179.3 |
| 0.10 | 60.2 | 54.8 | 60.1 | 194.1 | 176.5 | 177.2 |
| 0.15 | 60.9 | 55.6 | 60.9 | 194.0 | 167.2 | 168.9 |
| 0.20 | 61.2 | 56.0 | 61.4 | 193.9 | 169.5 | 169.7 |
| 0.25 | 62.9 | 56.3 | 61.7 | 186.7 | 169.0 | 171.4 |
| 0.30 | 65.6 | 56.8 | 62.2 | 186.8 | 174.2 | 174.4 |
| 0.35 | 67.0 | 57.5 | 62.9 | 188.2 | 176.0 | 176.5 |
| 0.40 | 67.8 | 57.7 | 63.1 | 176.7 | 176.2 | 177.6 |
| 0.45 | 69.0 | 58.4 | 63.8 | 162.2 | 175.1 | 176.6 |
| 0.50 | 69.9 | 59.1 | 64.5 | 159.5 | 174.0 | 174.4 |
| 0.55 | 71.3 | 59.9 | 65.3 | 167.8 | 173.1 | 173.2 |
| 0.60 | 71.9 | 60.5 | 65.9 | 163.3 | 170.3 | 172.3 |
| 0.65 | 72.6 | 61.3 | 66.7 | 162.9 | 169.9 | 171.4 |
| 0.70 | 74. 1 | 61.9 | 67.3 | 153.4 | 168.5 | 169.8 |
| 0.75 | 74.8 | 62.6 | 68.0 | 153.1 | 166.1 | 167.8 |
| 0.80 | 76.0 | 63.4 | 68.8 | 165.0 | 166.6 | 166.7 |
| 0.85 | 77.9 | 64.2 | 69.6 | 162.7 | 164.7 | 166.2 |
| 0.90 | 79.3 | 65.2 | 70.6 | 155.9 | 164.9 | 164.7 |
| 0.95 | 79.8 | 65.7 | 71.1 | 164.9 | 159.6 | 163.6 |
| (kJ·mol−1) | 69.3 ± 6.5 | 59.5 ± 3.5 | 64.9 ± 3.5 | 172.7 ± 14.7 | 170.5 ± 4.9 | 171.7 ± 4.5 |
| Samples | Step | Temperature Range/°C | DTGmax/°C | Normalized HF | Δm/% | |
|---|---|---|---|---|---|---|
| Tonset/°C | Tpeak/°C | |||||
| PERas | I | 40.0–121.8 | 110.9 | 83.2 | 113.2 | 8.10 |
| II | 121.8–166.9 | 137.4 | 151.2 | 132.3 | 15.54 | |
| III | 166.9–374.9 | 249.6 | 171.5 | 213.1 | 76.36 | |
| PERpf | I | 40.0–171.2 | 108.9 | 70.0 | 110.5 | 5.81 |
| II | 171.2–253.5 | 222.6; 232.3 | 165.8 | 204.7; 216.1 | 21.30 | |
| III | 253.5–298.9 | 277.8 | - | - | 15.60 | |
| IV | 298.9–381.7 | 320.0 | 310.3 | 342.8 | 26.20 | |
| V | 381.7–500.0 | 485.6 | 380.1 | 479.2 | 31.09 | |
© 2017 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buda, V.; Andor, M.; Ledeti, A.; Ledeti, I.; Vlase, G.; Vlase, T.; Cristescu, C.; Voicu, M.; Suciu, L.; Tomescu, M.C. Comparative Solid-State Stability of Perindopril Active Substance vs. Pharmaceutical Formulation. Int. J. Mol. Sci. 2017, 18, 164. https://doi.org/10.3390/ijms18010164
Buda V, Andor M, Ledeti A, Ledeti I, Vlase G, Vlase T, Cristescu C, Voicu M, Suciu L, Tomescu MC. Comparative Solid-State Stability of Perindopril Active Substance vs. Pharmaceutical Formulation. International Journal of Molecular Sciences. 2017; 18(1):164. https://doi.org/10.3390/ijms18010164
Chicago/Turabian StyleBuda, Valentina, Minodora Andor, Adriana Ledeti, Ionut Ledeti, Gabriela Vlase, Titus Vlase, Carmen Cristescu, Mirela Voicu, Liana Suciu, and Mirela Cleopatra Tomescu. 2017. "Comparative Solid-State Stability of Perindopril Active Substance vs. Pharmaceutical Formulation" International Journal of Molecular Sciences 18, no. 1: 164. https://doi.org/10.3390/ijms18010164










