A Novel Isothermal Assay of Borrelia burgdorferi by Recombinase Polymerase Amplification with Lateral Flow Detection
Abstract
:1. Introduction
2. Results
2.1. Establishment of Recombinase Polymerase Amplification with Lateral Flow (LF-RPA) Assay
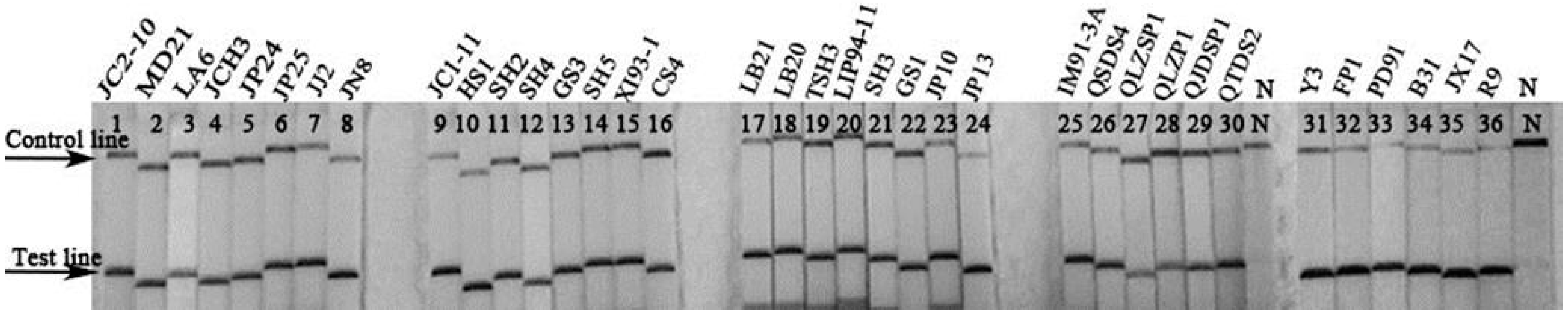
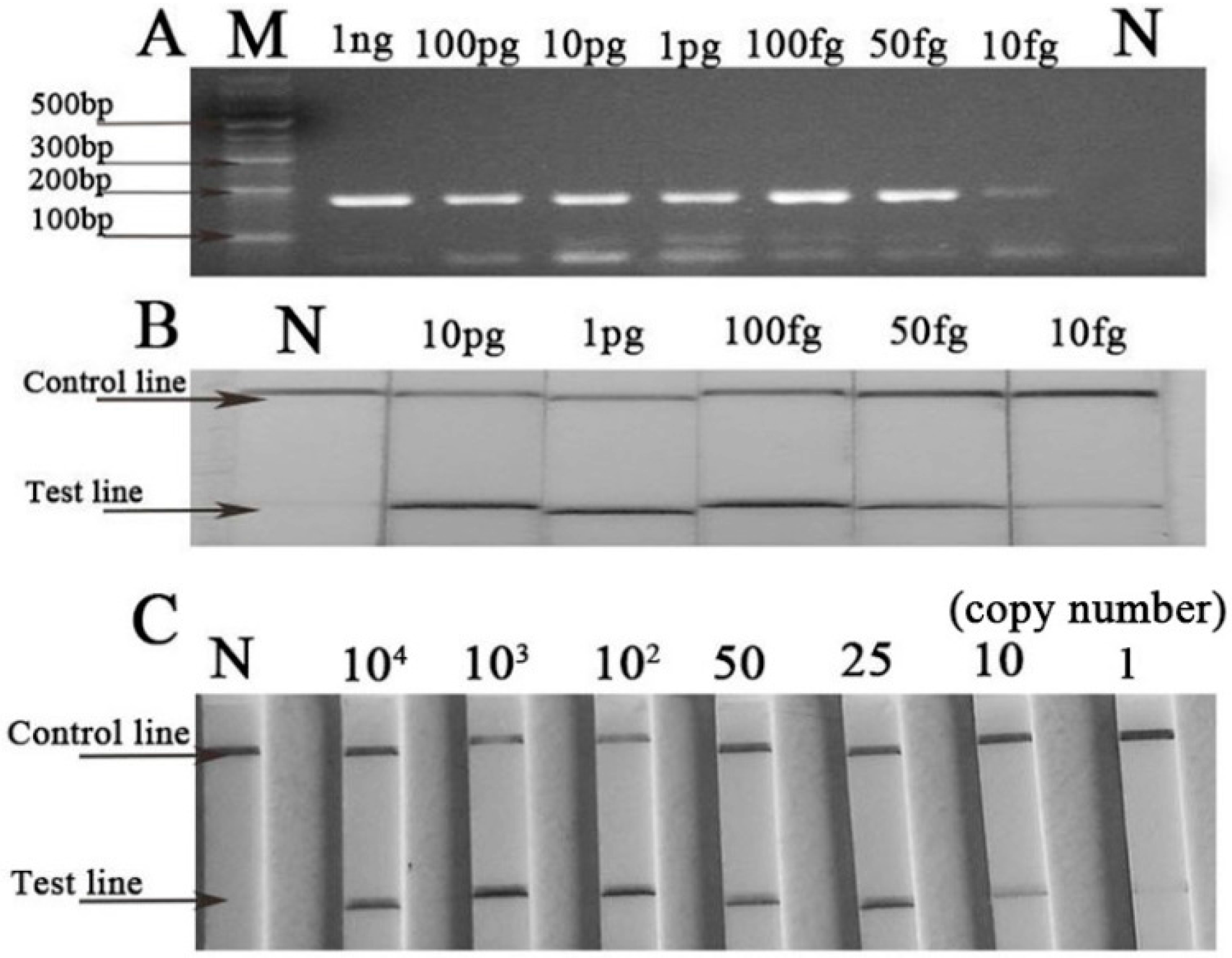
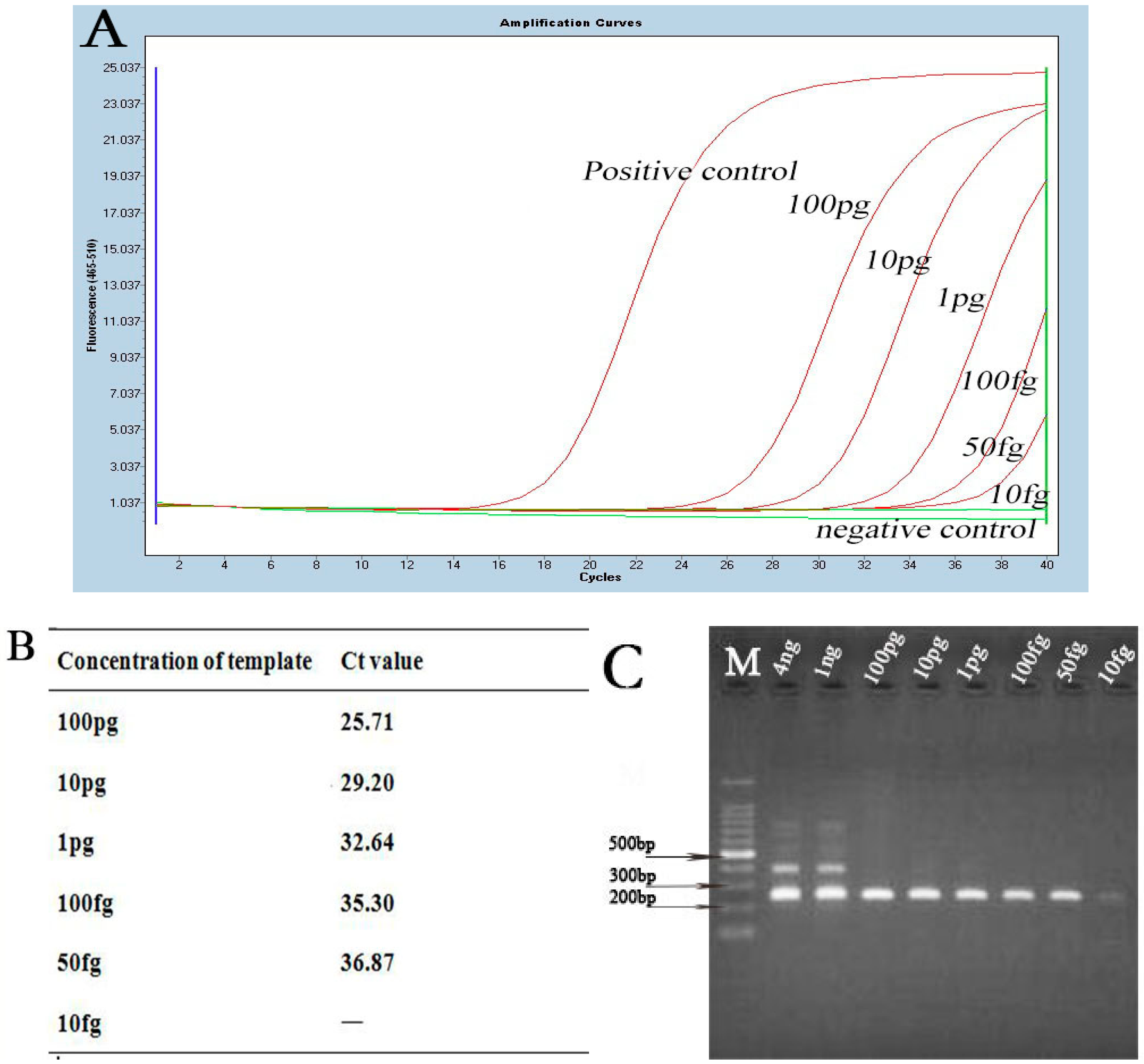
2.2. Sensitivity and Specificity of Basic Recombinase Polymerase Amplification (B-RPA) and LF-RPA Assay
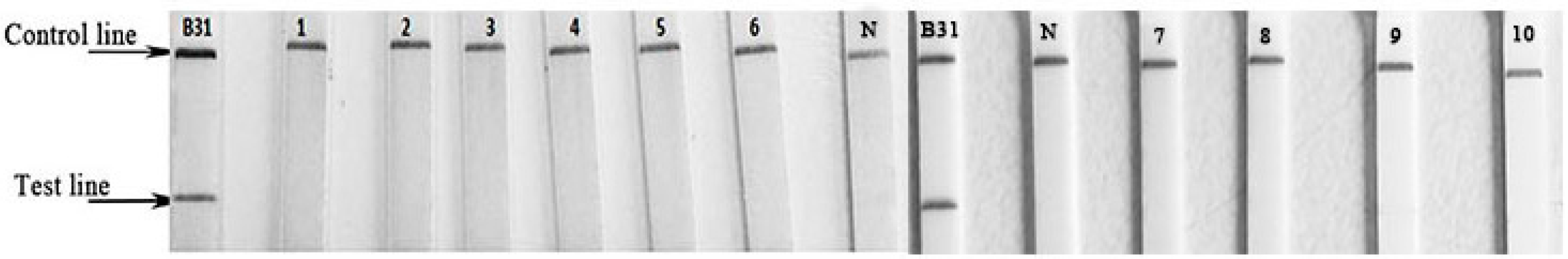
2.3. Evaluation of LF-RPA Assay for Clinical Samples
3. Discussion
4. Materials and Methods
4.1. Strains and DNA Extraction
4.2. Establishment of B-RPA and LF-RPA Assay
4.3. Sensitivity and Specificity of LF-RPA Assay
4.4. Evaluating the Efficiency of LF-RPA Assay in Clinical Diagnosis
4.5. Ethical Statement
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| LB | Lyme borreliosis |
| EM | erythema migrans |
| RPA | recombinase polymerase amplification |
| B-RPA | basic recombinase polymerase amplification |
| LF-RPA | recombinase polymerase amplification with lateral flow |
| LAMP | loop-mediated isothermal amplification |
| IFA | indirect immunofluorescence assay |
| EIA | enzyme immunoassay |
| ELISA | immunosorbent assay |
| WB | western blot |
References
- Marques, A.R. Laboratory diagnosis of lyme diseases: Advances and challenges. Infect. Dis. Clin. N. Am. 2015, 29, 295–307. [Google Scholar] [CrossRef] [PubMed]
- Stanek, G.; Fingerle, V.; Hunfeld, K.P.; Jaulhac, B.; Kaiser, R.; Krause, A.; Kristoferitsch, W.; O’Connell, S.; Ornstein, K.; Strle, F.; et al. Lyme borreliosis: Clinical case definitions for diagnosis and management in Europe. Clin. Microbiol. Infect. 2011, 17, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Stanek, G.; Strle, F. Lyme borreliosis. Lancet 2012, 379, 461–473. [Google Scholar] [CrossRef]
- Aguero-Rosenfeld, M.E.; Wang, G.; Schwartz, I.; Wormser, G.P. Diagnosis of Lyme borreliosis. Clin. Microbiol. Rev. 2005, 18, 484–509. [Google Scholar] [CrossRef] [PubMed]
- James, A.; Macdonald, J. Recombinase polymerase amplification: Emergence as a critical molecular technology for rapid, low-resource diagnostics. Expert Rev. Mol. Diagn. 2015, 15, 1475–1489. [Google Scholar] [CrossRef] [PubMed]
- Rosser, A.; Rollinson, D.; Forrest, M.; Webster, B.L. Isothermal Recombinase Polymerase Amplification (RPA) of Schistosoma haematobium DNA and oligochromatographic lateral flow detection. Parasites Vectors 2015, 8, 446. [Google Scholar] [CrossRef] [PubMed]
- Nair, G.; Rebolledo, M.; White, A.C.; Crannell, Z.; Richards-Kortum, R.R.; Pinilla, A.E.; Ramírez, J.D.; López, M.C.; Castellanos-Gonzalez, A. Detection of Entamoeba histolytica by Recombinase Polymerase Amplification. Am. J. Trop. Med. Hyg. 2015, 93, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Wahed, A.A.E.; Patel, P.; Faye, O.; Thaloengsok, S.; Heidenreich, D.; Matangkasombut, P.; Manopwisedjaroen, K.; Sakuntabhai, A.; Sall, A.A.; Hufert, F.T.; et al. Recombinase Polymerase Amplification assay for rapid diagnostics of dengue infection. PLoS ONE 2015, 10. [Google Scholar] [CrossRef]
- Liljander, A.; Yu, M.; O’Brien, E.; Heller, M.; Nepper, J.F.; Weibel, D.B.; Gluecks, I.; Younan, M.; Frey, J.; Falquet, L.; et al. A field-applicable recombinase polymerase amplification assay for rapid detection of Mycoplasma capricolum subsp. capripneumoniae. J. Clin. Microbiol. 2015, 53, 2810–2815. [Google Scholar] [CrossRef] [PubMed]
- Kersting, S.; Rausch, V.; Bier, F.F.; von Nickisch-Rosenegk, M. Multiplex isothermal solid-phase recombinase polymerase amplification for the specific and fast DNA-based detection of three bacterial pathogens. Microchim. Acta 2014, 181, 1715–1723. [Google Scholar] [CrossRef] [PubMed]
- Chao, C.C.; Belinskaya, T.; Zhang, Z.; Ching, W.M. Development of Recombinase Polymerase Amplification assays for detection of Orientia tsutsugamushi or Rickettsia typhi. PLoS Negl. Trop. Dis. 2015, 9, e0003884. [Google Scholar] [CrossRef] [PubMed]
- Crannell, Z.A.; Castellanos-Gonzalez, A.; Irani, A.; Rohrman, B.; White, A.C.; Richards-Kortum, R. Nucleic acid test to diagnose cryptosporidiosis: Lab assessment in animal and patient specimens. Anal. Chem. 2014, 86, 2565–2571. [Google Scholar] [CrossRef] [PubMed]
- Hao, Q.; Hou, X.; Geng, Z.; Wan, K. Distribution of Borrelia burgdorferi sensu lato in China. J. Clin. Microbiol. 2011, 49, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.Y.; Jiang, B.G.; He, J.; Gao, Y.; Zhang, P.H.; Wu, X.M.; Zhang, W.Y.; Shi, H.; Gaowa, H.S.; Wang, J.B.; et al. Genetic diversity of Borrelia burgdorferi sensu lato isolates from Northeastern China. Vector Borne Zoonotic Dis. 2011, 11, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Kersting, S.; Rausch, V.; Bier, F.F.; von Nickisch-Rosenegk, M. Rapid detection of Plasmodium falciparum with isothermal recombinase polymerase amplification and lateral flow analysis. Malar. J. 2014, 13, 99. [Google Scholar] [CrossRef] [PubMed]
- Castellanos-Gonzalez, A.; Saldarriaga, O.A.; Tartaglino, L.; Gacek, R.; Temple, E.; Sparks, H.; Melby, P.C.; Travi, B.L. A novel molecular test to diagnose canine visceral leishmaniasis at the point of care. Am. J. Trop. Med. Hyg. 2015, 93, 970–975. [Google Scholar] [CrossRef] [PubMed]
- Dania, R.; Danièle, P.; Natacha, S.; Livey, I.; Matuschka, F.R.; Baranton, G. Delineation of Borrelia burgdorferi sensu lato species by multilocus sequence analysis and confirmation of the delineation of Borrelia spielmanii sp. nov. Int. J. Syst. Evol. Microbiol. 2006, 56, 873–881. [Google Scholar]
- Momert, S.; Gutzmer, R.; Kapp, A.; Werfel, T. Sensitive detection of Borrelia burgdorferi sensu lato DNA and differentiation of Borrelia species by LightCycler PCR. J. Clin. Microbiol. 2001, 39, 2663–2667. [Google Scholar] [CrossRef] [PubMed]
- Pietilä, J.; He, Q.; Oksi, J.; Viljanen, M.K. Rapid differentiation of Borrelia garinii from Borrelia afzelii and Borrelia burgdorferi sensu stricto by LightCycler fluorescence melting curve analysis of a PCR product of the recA gene. J. Clin. Microbiol. 2000, 38, 2756–2759. [Google Scholar]
- Magnarelli, L.A.; Anderson, J.F.; Johnson, R.C. Cross-reactivity in serological tests for Lyme disease and other spirochetal infections. J. Infect. Dis. 1987, 156, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhu, X.; Hou, X.; Geng, Z.; Chen, H.; Hao, Q. Test of 259 serums from patients with arthritis or neurological symptoms confirmed existence of Lyme disease in Hainan province, China. Int. J. Clin. Exp. Med. 2015, 8, 9531–9536. [Google Scholar] [PubMed]
- Chu, C.Y.; Jiang, B.G.; Liu, W.; Zhao, Q.M.; Wu, X.M.; Zhang, P.H.; Zhan, L.; Yang, H.; Cao, W.C. Presence of pathogenic Borrelia burgdorferi sensu lato in ticks and rodents in Zhejiang, south-east China. J. Med. Microbiol. 2008, 57, 980–985. [Google Scholar] [CrossRef] [PubMed]
- Postic, D.; Assous, M.V.; Grimont, P.A.; Baranton, G. Diversity of Borrelia burgdorferi sensu lato evidenced by restriction fragment length polymorphism of rrf (5S)-rrl (23S) intergenic spacer amplicons. Int. J. Syst. Bacteriol. 1994, 44, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.J.; Gazumyan, A.; Schwartz, A.I. rRNA gene organization in the Lyme disease spirochete, Borrelia burgdorferi. J. Bacteriol. 1992, 174, 3757–3765. [Google Scholar] [PubMed]
- Ge, Z.; Hou, X.; Zhang, L.; Hao, Q. Evaluation of a new real-time PCR assay for detection of Borrelia burgdorferi in rodents. Chin. J. Zoonoses 2015, 31, 812–816. [Google Scholar]
| Numbers of Samples | Western Blot | Real-Time qPCR (Ct Value ) | Nested-PCR | LF-RPA |
|---|---|---|---|---|
| 1 | +(IgM) | 35.4 | + | + |
| 2 | +(IgM) | 32.11 | + | + |
| 3 | +(IgG, IgM) | 34.21 | − | + |
| 4 | +(IgM) | − | + | + |
| 5 | +(IgG, IgM) | 37.17 | + | + |
| 6 | +(IgG, IgM) | − | + | + |
| 7 | +(IgM) | − | + | + |
| 8 | +(IgM) | − | − | + |
| 9 | +(IgG) | − | − | − |
| 10 | +(IgG) | − | − | − |
| 11 | +(IgM) | 35.42 | − | + |
| 12 | +(IgG, IgM) | 32.32 | + | + |
| 13 | − | 34.63 | + | + |
| 14 | +(IgM) | 33.36 | − | + |
| 15 | +(IgM) | 37.14 | − | + |
| 16 | − | 32.96 | + | + |
| 17 | +(IgM) | 36.91 | − | + |
| 18 | +(IgM) | 37.40 | + | + |
| 19 | +(IgM) | 34.13 | + | + |
| 20 | − | 35.30 | − | + |
| Assays | Primers |
|---|---|
| Basic RPA reaction | F: 5′-ATTGTATTAGATGAAGCTCTTGGCATTGGTGGA-3′ |
| R: 5′-AATAGGATCGAGATCAAGTTCTGCTTCAATA-3′ | |
| Lateral flow RPA reaction | LF-F: 5′-ATTGTATTAGATGAAGCTCTTGGCATTGGTGGA-3′ |
| LF-R: 5′-biotin-TTGCATAAATAGGATCGAGATCAAGTTCTGC-3′ | |
| LF-P: 5′-(FAM)-ACTTTGATCCTTCAAGCGATTGCTGARGT-(dSpacer)-CAAAAAGAAGGAGGCAT-C3Spacer-3′ |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, W.; Liu, H.-X.; Zhang, L.; Hou, X.-X.; Wan, K.-L.; Hao, Q. A Novel Isothermal Assay of Borrelia burgdorferi by Recombinase Polymerase Amplification with Lateral Flow Detection. Int. J. Mol. Sci. 2016, 17, 1250. https://doi.org/10.3390/ijms17081250
Liu W, Liu H-X, Zhang L, Hou X-X, Wan K-L, Hao Q. A Novel Isothermal Assay of Borrelia burgdorferi by Recombinase Polymerase Amplification with Lateral Flow Detection. International Journal of Molecular Sciences. 2016; 17(8):1250. https://doi.org/10.3390/ijms17081250
Chicago/Turabian StyleLiu, Wei, Hui-Xin Liu, Lin Zhang, Xue-Xia Hou, Kang-Lin Wan, and Qin Hao. 2016. "A Novel Isothermal Assay of Borrelia burgdorferi by Recombinase Polymerase Amplification with Lateral Flow Detection" International Journal of Molecular Sciences 17, no. 8: 1250. https://doi.org/10.3390/ijms17081250
APA StyleLiu, W., Liu, H.-X., Zhang, L., Hou, X.-X., Wan, K.-L., & Hao, Q. (2016). A Novel Isothermal Assay of Borrelia burgdorferi by Recombinase Polymerase Amplification with Lateral Flow Detection. International Journal of Molecular Sciences, 17(8), 1250. https://doi.org/10.3390/ijms17081250





