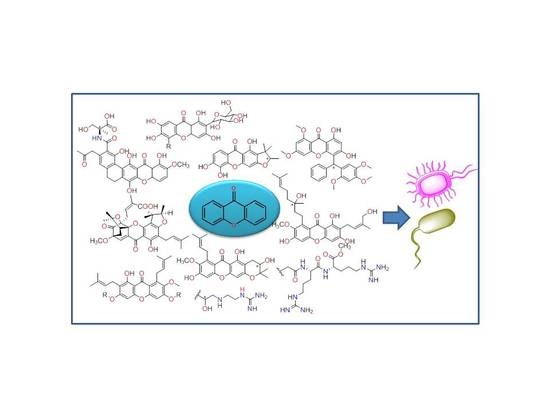
Chiral Derivatives of Xanthones with Antimicrobial Activity
Abstract
1. Introduction
2. Natural Chiral Derivatives of Xanthones
2.1. Natural CDXs with Furan Groups
2.2. Natural CDXs with Pyran Groups
2.3. Natural CDXs with Hydroxy Side Chains
2.4. Natural Caged Xanthones
2.5. Other Natural CDXs
3. Synthetic CDXs
3.1. Muchimangins Analogues
3.2. Mangiferin Analogues
3.3. Amino Acid Xanthone Derivatives
3.4. α-Mangostin Analogues
3.5. Xanthone Derivatives with 2-Hydro-3-Amino and Piperazine Groups
3.6. Derivatives of Caged Xanthones
3.7. Xanthone Derivatives of C-2-Substituted
4. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Morehead, M.S.; Scarbrough, C. Emergence of global antibiotic resistance. Prim. Care 2018, 45, 467–484. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention, Antibiotic Use in the United States: Progress and Opportunities. Available online: https://www.cdc.gov/antibiotic-use/stewardship-report/pdf/stewardship-report.pdf (accessed on 20 December 2018).
- Morgan, D.; Okeke, I.; Laxminarayan, R.; Perencevich, E.; Weisenberg, S. Non-prescription antimicrobial use worldwide: A systematic review. Lancet Infect Dis. 2011, 11, 692–701. [Google Scholar] [CrossRef]
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial resistance: A global multifaceted phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Liu, S.; Koh, J.J.; Zou, H.; Lakshminarayanan, R.; Bai, Y.; Pervushin, K.; Zhou, L.; Verma, C.; Beuerman, R.W. A novel fragment based strategy for membrane active antimicrobials against MRSA. BBA 2015, 1848, 1023–1031. [Google Scholar] [CrossRef] [PubMed]
- Gomes, A.; Brandão, P.; Fernandes, C.; Sousa, M.; Pinto, M. Drug-like properties and ADME of xanthone derivatives: The antechamber of clinical trials. Curr. Med. Chem. 2016, 23, 3654–3686. [Google Scholar] [CrossRef]
- Pinto, M.; Sousa, M.; Nascimento, M. Xanthone derivatives: New insights in biological activities. Curr. Med. Chem. 2005, 12, 2517–2538. [Google Scholar] [CrossRef]
- Shagufta; Ahmad, I. Recent insight into the biological activities of synthetic xanthone derivatives. Eur. J. Med. Chem. 2016, 116, 267–280. [Google Scholar] [CrossRef]
- Luo, C.T.; Mao, S.S.; Liu, F.L.; Yang, M.X.; Chen, H.; Kurihara, H.; Li, Y. Antioxidant xanthones from Swertia mussotii, a high altitude plant. Fitoterapia 2013, 91, 140–147. [Google Scholar] [CrossRef]
- Jung, H.; Su, B.; Keller, W.; Mehta, R.; Kinghorn, A. Antioxidant Xanthones from the Pericarp of Garcinia mangostana (Mangosteen). J. Agric. Food Chem. 2006, 54, 2077–2082. [Google Scholar] [CrossRef]
- Francik, R.; Szkaradek, N.; Zelaszczk, D.; Marona, H. Antioxidant activity of xanthones derivatives. Acta Pol. Pharm. 2016, 73, 1505–1509. [Google Scholar]
- Cheng, Y.W.; Kang, J.J. Mechanism of vasorelaxation of thoracic aorta caused by xanthone. Eur. J. Pharmacol. 1997, 336, 23–28. [Google Scholar] [CrossRef]
- Ali, M.; Latif, A.; Zaman, K.; Arfan, M.; Maitland, D.; Ahmad, H.; Ahmad, M. Anti-ulcer xanthones from the roots of Hypericum oblongifolium Wall. Fitoterapia 2014, 95, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Yang, L.; Wang, C. Anti-inflammatory activity of mangostins from Garcinia mangostana. Food Chem. Toxicol. 2008, 46, 688–693. [Google Scholar] [CrossRef] [PubMed]
- Pfister, J.R.; Ferraresi, R.W.; Harrison, I.T.; Rooks, W.H.; Roszkowski, A.P.; Horn, A.V.; Fried, H. Xanthone-2-carboxylic acids, a new series of antiallergic substances. J. Med. Chem. 1972, 15, 1032–1035. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Huang, L.; Chen, X.H.; Zhu, X.F.; Qian, X.J.; Feng, G.K.; Lan, W.J.; Li, H.J. Cytotoxic prenylated xanthones from the pericarps of Garcinia mangostana. Molecules 2014, 19, 1820–1827. [Google Scholar] [CrossRef] [PubMed]
- Reutrakul, V.; Anantachoke, N.; Pohmakotr, M.; Jaipetch, T.; Sophasan, S.; Yoosook, C.; Kasisit, J.; Napaswat, C.; Santisuk, T.; Tuchinda, P. Cytotoxic and anti-HIV-1 caged xanthones from the resin and fruits of Garcinia hanburyi. Planta Med. 2007, 73, 33–40. [Google Scholar] [CrossRef]
- Marona, H.; Szkaradek, N.; Karczewska, E.; Trojanowska, D.; Budak, A.; Bober, P.; Przepiorka, W.; Cegla, M.; Szneler, E. Antifungal and antibacterial activity of the newly synthesized 2-xanthone derivatives. Arch. Pharm. Chem. Life Sci. 2009, 342, 9–18. [Google Scholar] [CrossRef]
- Yasunaka, K.; Abe, F.; Nagayama, A.; Okabe, H.; Lozada-Perez, L.; Lopez-Villafranco, E.; Muniz, E.E.; Aguilar, A.; Reyes-Chilpa, R. Antibacterial activity of crude extracts from mexican medicinal plants and purified coumarins and xanthones. J. Ethnopharmacol. 2005, 97, 293–299. [Google Scholar] [CrossRef]
- Nguemeving, J.; Azebaze, A.; Kuete, V.; Eric Carly, N.; Beng, V.; Meyer, M.; Blond, A.; Bodo, B.; Nkengfack, A. Laurentixanthones A and B, antimicrobial xanthones from Vismia laurentii. Phytochemistry 2006, 67, 1341–1346. [Google Scholar] [CrossRef]
- Fukai, T.; Yonekawa, M.; Hou, A.J.; Nomura, T.; Sun, H.D.; Uno, J. Antifungal agents from the roots of Cudrania cochinchinensis against Candida, Cryptococcus, and Aspergillus Species. J. Nat. Prod. 2003, 66, 1118–1120. [Google Scholar] [CrossRef]
- Groweiss, A.; Cardellina, J.H.; Boyd, M.R. HIV-Inhibitory prenylated xanthones and flavones from Maclura tinctoria. J. Nat. Prod. 2000, 63, 1537–1539. [Google Scholar] [CrossRef] [PubMed]
- Rajtar, G.; Zolkowska, D.; Kleinrok, Z.; Marona, H. Antiplatelets activity of some xanthone derivatives. Acta Pol. Pharm. 1999, 56, 319–324. [Google Scholar] [PubMed]
- Marona, H.; Librowski, T.; Cegła, M.; Erdoğan, C.; Sahin, N. Antiarrhythmic and antihypertensive activity of some xanthone derivatives. Acta Pol. Pharm. 2008, 65, 383–390. [Google Scholar]
- Jastrzebska-Wiesek, M.; Czarnecki, R.; Marona, H. The anticonvulsant, local anesthetic and hemodynamic properties of some chiral aminobutanol derivatives of xanthone. Acta Pol. Pharm. 2008, 65, 591–600. [Google Scholar] [PubMed]
- Gnerra, C.; Thulla, U.; Gaillard, P.; Carrupta, P.A.; Testa, B.; Fernandes, E.; Silva, F.; Pinto, M.; Pinto, M.M.M.; Wolfender, J.L.; et al. Natural and synthetic xanthones as monoamine oxidase inhibitors: Biological assay and 3D-QSAR. Helv. Chim. Acta 2001, 84, 552–570. [Google Scholar] [CrossRef]
- Iikubo, K.; Ishikawa, Y.; Ando, N.; Umezawab, K.; Nishiyama, S. The first direct synthesis of alfa-mangostin, a potent inhibitor of the acidic sphingomyelinase. Tetrahedron Lett. 2002, 43, 291–293. [Google Scholar] [CrossRef]
- Szkaradek, N.; Rapacz, A.; Pytka, K.; Filipek, B.; Żelaszczyk, D.; Szafrański, P.; Słoczyńska, K.; Marona, H. Cardiovascular activity of the chiral xanthone derivatives. Bioorg. Med. Chem. 2015, 23, 6714–6724. [Google Scholar] [CrossRef]
- Fernandes, C.; Oliveira, L.; Tiritan, M.E.; Leitao, L.; Pozzi, A.; Noronha-Matos, J.B.; Correia-de-Sa, P.; Pinto, M.M. Synthesis of new chiral xanthone derivatives acting as nerve conduction blockers in the rat sciatic nerve. Eur. J. Med. Chem. 2012, 55, 1–11. [Google Scholar] [CrossRef]
- Hassan, N.; Taher, M.; Susanti, D. Phytochemical constituents and pharmacological properties of Garcinia xanthochymus- a review. Biomed. Pharmacother. 2018, 106, 1378–1389. [Google Scholar] [CrossRef]
- Ruan, J.; Zheng, C.; Liu, Y.; Qu, L.; Yu, H.; Han, L.; Zhang, Y.; Wang, T. Chemical and biological research on herbal medicines rich in xanthones. Molecules 2017, 22, 1698. [Google Scholar] [CrossRef]
- Cruz, M.; Cidade, H.; Pinto, M. Dual/multitargeted xanthone derivatives for Alzheimer’s disease: Where do we stand? Future Med. Chem. 2017, 9, 1611–1630. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.H.; Ma, L.; Wei, Z.P.; Han, F.; Gao, J. Advances in isolation and synthesis of xanthone derivatives. CHM 2012, 4, 87–102. [Google Scholar]
- Masters, K.S.; Brase, S. Xanthones from fungi, lichens, and bacteria: The natural products and their synthesis. Chem. Rev. 2012, 112, 3717–3776. [Google Scholar] [CrossRef]
- Pinto, M.; Castanheiro, R.; Kijjoa, A. Xanthones from marine-derived microorganisms: Isolation, structure elucidation and biological activities. In Encyclopedia of Analytical Chemistry; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2014; pp. 1–21. [Google Scholar] [CrossRef]
- Azevedo, C.; Afonso, C.; Pinto, M. Routes to xanthones: An update on the synthetic approaches. Curr. Org. Chem. 2012, 16, 1–50. [Google Scholar] [CrossRef]
- Hostettmann, K.; Borloz, A.; Urbain, A.; Marston, A. Natural product inhibitors of acetylcholinesterase. Curr. Org. Chem. 2006, 10, 825–847. [Google Scholar] [CrossRef]
- Hussain, H.; Al-Sadi, A.; Schulz, B.; Steinert, M.; Khan, A.; Green, I.; Ahmed, I. A fruitful decade for fungal polyketides from 2007 to 2016: Antimicrobial activity, chemotaxonomy and chemodiversity. Futur. Med. Chem. 2017, 9, 1631–1648. [Google Scholar] [CrossRef]
- Epifano, F.; Fiorito, S.; Genovese, S. Phytochemistry and pharmacognosy of the genus Psorospermum. Phytochemistry Rev. 2013, 12, 673–684. [Google Scholar] [CrossRef]
- Abou-Shoer, M.; Boettner, F.; Chang, C.; Cassady, J. Antitumour and cytotoxic xanthones of Psorospermum Febrifugum. Phytochemistry 1998, 27, 2795–2800. [Google Scholar] [CrossRef]
- Komguem, J.; Meli, A.; Manfouo, R.; Lontsi, D.; Ngounou, F.; Kuete, V.; Kamdem, H.; Tane, P.; Ngadjui, B.; Sondengam, B.; et al. Xanthones from Garcinia smeathmannii (Oliver) and their antimicrobial activity. Phytochemistry 2005, 66, 1713–1717. [Google Scholar] [CrossRef]
- El-Seedi, H.R.; El-Barbary, M.A.; El-Ghorab, D.M.; Bohlin, L.; Borg-Karlson, A.K.; Göransson, U.; Verpoorte, R. Recent insights into the biosynthesis and biological activities of natural xanthones. Curr. Med. Chem. 2010, 17, 854–901. [Google Scholar] [CrossRef]
- Kaomongkolgit, R.; Jamdez, K.; Chaisomboon, N. Antifungal activity of alpha-mangostin against Candida albicans. J. Oral Sci. 2009, 51, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Guzman-Beltran, S.; Rubio-Badillo, M.A.; Juarez, E.; Hernandez-Sanchez, F.; Torres, M. Nordihydroguaiaretic acid (NDGA) and alpha-mangostin inhibit the growth of Mycobacterium tuberculosis by inducing autophagy. Int. Immunopharmacol. 2016, 31, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Sudta, P.; Jiarawapi, P.; Suksamrarn, A.; Hongmanee, P.; Suksamrarn, S. Potent activity against Multidrug-Resistant Mycobacterium tuberculosis of α-Mangostin analogs. Chem. Pharm. Bull. 2013, 61, 194–203. [Google Scholar] [CrossRef]
- Suksamrarn, S.; Suwannapoch, N.; Phakhodee, W.; Thanuhiranlert, J.; Ratananukul, P.; Chimnoi, N.; Suksamrarn, A. Antimycobacterial activity of prenylated xanthones from the fruits of Garcinia mangostana. Chem. Pharm. Bull. 2003, 51, 857–859. [Google Scholar] [CrossRef] [PubMed]
- Zanatta, N.; Alves, S.H.; Coelho, H.S.; Borchhardt, D.M.; Machado, P.; Flores, K.M.; da Silva, F.M.; Spader, T.B.; Santurio, J.M.; Bonacorso, H.G.; et al. Synthesis, antimicrobial activity, and QSAR studies of furan-3-carboxamides. Bioorg. Med. Chem. 2007, 15, 1947–1958. [Google Scholar] [CrossRef] [PubMed]
- Nilar; Harrison, L.J. Xanthones from the heartwood of Garcinia mangostana. Phytochemistry 2002, 60, 541–548. [Google Scholar] [CrossRef]
- Fukai, T.; Oku, Y.; Hou, A.J.; Yonekawa, M.; Terada, S. Antimicrobial activity of hydrophobic xanthones from Cudrania cochinchinensis against Bacillus subtilis and Methicillin-Resistant Staphylococcus aureus. Chem. Biodivers. 2004, 1, 1385–1390. [Google Scholar] [CrossRef]
- Fukai, T.; Oku, Y.; Hou, A.J.; Yonekawa, M.; Terada, S. Antimicrobial activity of isoprenoid-substituted xanthones from Cudrania cochinchinensis against Vancomycin-resistant Enterococci. Phytomedicine 2005, 12, 510–513. [Google Scholar] [CrossRef]
- Boonsri, S.; Karalai, C.; Ponglimanont, C.; Kanjana-opas, A.; Chantrapromma, K. Antibacterial and cytotoxic xanthones from the roots of Cratoxylum formosum. Phytochemistry 2006, 67, 723–727. [Google Scholar] [CrossRef]
- Wang, Y.H.; Hou, A.J.; Zhu, G.F.; Chen, D.F.; Sun, H.D. Cytotoxic and antifungal isoprenylated xanthones and flavonoids from Cudrania fruticosa. Plant Med. 2005, 71, 273–274. [Google Scholar] [CrossRef]
- Siridechakorn, I.; Phakhodee, W.; Ritthiwigrom, T.; Promgool, T.; Deachathai, S.; Cheenpracha, S.; Prawat, U.; Laphookhieo, S. Antibacterial dihydrobenzopyran and xanthone derivatives from Garcinia cowa stem barks. Fitoterapia 2012, 83, 1430–1434. [Google Scholar] [CrossRef]
- Gurunanjappa, P.; Ningappa, M.; Kariyappa, A. Synthesis of pyrazole fused pyran analogues: Antimicrobial, antioxidant and molecular docking studies. Chem. Data Collect. 2016, 5–6, 1–11. [Google Scholar] [CrossRef]
- Dharmaratne, H.; Wijesinghe, W.; Thevanasem, V. Antimicrobial activity of xanthones from Calophyllum species, against methicillin-resistant Staphylococcus aureus (MRSA). J. Ethnopharmacol. 1999, 66, 339–342. [Google Scholar] [CrossRef]
- Namdaung, U.; Aroonrerk, N.; Suksamrarn, S.; Danwitsetkanjana, K.; Saenboonrueng, J.; Arjchomphu, W.; Suksamrarn, A. Bioactive constituents of the root bark of Artocarpus rigidus subsp. rigidus. Chem. Pharm. Bull. 2006, 54, 1433–1436. [Google Scholar] [CrossRef]
- Makmur, L.; Syamsurizal, S.; Tukiran, T.; Achmad, S.A.; Aimi, N.; Hakim, E.H.; Kitajima, M.; Takayama, H. Artoindonesianin C, a New Xanthone Derivative from Artocarpus teysmanii. J. Nat. Prod. 2000, 63, 243–244. [Google Scholar] [CrossRef] [PubMed]
- Genovese, S.; Fiorito, S.; Taddeo, V.A.; Epifano, F. Recent developments in the pharmacology of prenylated xanthones. Drug Discov. Today 2016, 21, 1814–1819. [Google Scholar] [CrossRef] [PubMed]
- Auranwiwat, C.; Laphookhieo, S.; Rattanajak, R.; Kamchonwongpaisan, S.; Pyne, S.G.; Ritthiwigrom, T. Antimalarial polyoxygenated and prenylated xanthones from the leaves and branches of Garcinia mckeaniana. Tetrahedron 2016, 72, 6837–6842. [Google Scholar] [CrossRef]
- Tantapakul, C.; Phakhodee, W.; Ritthiwigrom, T.; Cheenpracha, S.; Prawat, U.; Deachathai, S.; Laphookhieo, S. Rearranged benzophenones and prenylated xanthones from Garcinia propinqua Twigs. J. Nat. Prod. 2012, 75, 1660–1664. [Google Scholar] [CrossRef]
- Nontakham, A.; Upamai, W.; Suksamrarn, S.; Charoenram, N.; Taweechotipatr, M. Anti-Helicobacter pylori xanthones of Garcinia fusca. Arch. Pharm. Res. 2013, 37, 972–977. [Google Scholar] [CrossRef] [PubMed]
- Oger, J.M.; Morel, C.; Helesbeux, J.J.; Litaudon, M.; Séraphin, D.; Dartiguelongue, C.; Larcher, G.; Richomme, P.; Duval, O. First 2-hydroxy-3-methylbut-3-enyl substituted xanthones isolated from plants: Structure elucidation, synthesis and antifungal activity. Nat. Prod. Res. 2003, 17, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Suksamrarn, S.; Suwannapoch, N.; Ratananukul, P.; Aroonlerk, N.; Suksamrarn, A. Xanthones from the green fruit hulls of Garcinia mangostana. J. Nat. Prod. 2002, 65, 761–763. [Google Scholar] [CrossRef] [PubMed]
- Chaiyakunvat, P.; Anantachoke, N.; Reutrakul, V.; Jiarpinitnun, C. Caged xanthones: Potent inhibitors of global predominant MRSA USA300. Bioorg. Med. Chem. Lett. 2016, 26, 2980–2983. [Google Scholar] [CrossRef] [PubMed]
- Rukachaisirikul, V.; Phainuphong, P.; Sukpondma, Y.; Phongpaichit, S.; Taylor, W.C. Antibacterial caged-tetraprenylated xanthones from the stem bark of Garcinia scortechinii. Plant Med. 2005, 71, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Sukpondma, Y.; Rukachaisirikul, V.; Phongpaichit, S. Antibacterial caged-tetraprenylated xanthones from the fruits of Garcinia hanburyi. Chem. Pharm. Bull. 2005, 53, 850–852. [Google Scholar] [CrossRef] [PubMed]
- Banik, K.; Harsha, C.; Bordoloi, D.; Lalduhsaki Sailo, B.; Sethi, G.; Leong, H.C.; Arfuso, F.; Mishra, S.; Wang, L.; Kumar, A.P.; et al. Therapeutic potential of gambogic acid, a caged xanthone, to target cancer. Cancer Lett. 2018, 416, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Azebaze, A.; Meyer, M.; Valentin, A.; Nguemfo, E.; Fomum, Z.; Nkengfack, A. Prenylated xanthone derivatives with antiplasmodial activity from allanblackia monticola staner l.c. Chem. Pharm. Bull. 2006, 54, 111–113. [Google Scholar] [CrossRef]
- Asano, J.; Chiba, K.; Tada, M.; Yoshii, T. Cytotoxic xanthones from Garcinia Hanburyl. Phytochemistry 1996, 41, 815–820. [Google Scholar] [CrossRef]
- Ren, Y.; Matthew, S.; Lantvit, D.D.; Ninh, T.N.; Chai, H.; Fuchs, J.R.; Soejarto, D.D.; de Blanco, E.J.; Swanson, S.M.; Kinghorn, A.D. Cytotoxic and NF-kappaB inhibitory constituents of the stems of Cratoxylum cochinchinense and their semisynthetic analogues. J. Nat. Prod. 2011, 74, 1117–1125. [Google Scholar] [CrossRef]
- Ren, Y.; Lantvit, D.D.; de Carcache Blanco, E.J.; Kardono, L.B.; Riswan, S.; Chai, H.; Cottrell, C.E.; Farnsworth, N.R.; Swanson, S.M.; Ding, Y.; et al. Proteasome-inhibitory and cytotoxic constituents of Garcinia lateriflora: Absolute configuration of caged xanthones. Tetrahedron 2010, 66, 5311–5320. [Google Scholar] [CrossRef]
- Tao, S.J.; Guan, S.H.; Wang, W.; Lu, Z.Q.; Chen, G.T.; Sha, N.; Yue, Q.X.; Liu, X.; Guo, D.A. Cytotoxic polyprenylated xanthones from the resin of Garcinia hanburyi. J. Nat. Prod. 2009, 72, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Han, Q.; Yang, L.; Liu, Y.; Wang, Y.; Qiao, C.; Song, J.; Xu, L.; Yang, D.; Chen, S.; Xu, H. Gambogic acid and epigambogic acid, C-2 epimers with novel anticancer effects from Garcinia hanburyi. Planta Med. 2006, 72, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Han, Q.; Wang, Y.L.; Yang, L.; Tso, T.F.; Qiao, C.F.; Song, J.Z.; Xu, L.J.; Chen, S.L.; Yang, D.J.; Xu, H.X. Cytotoxic polyprenylated xanthones from the resin of Garcinia hanburyi. Chem. Pharm. Bull. 2006, 54, 265–267. [Google Scholar] [CrossRef] [PubMed]
- Rukachaisirikul, V.; Kaewnok, W.; Koysomboon, S.; Phongpaichit, S.; Taylor, W.C. Caged-tetraprenylated xanthones from Garcinia scortechinii. Tetrahedron 2000, 56, 8539–8543. [Google Scholar] [CrossRef]
- Rukachaisirikul, V.; Painuphong, P.; Sukpondma, Y.; Koysomboon, S.; Sawangchote, P.; Taylor, W. Caged-triprenylated and -tetraprenylated xanthones from the latex of Garcinia scortechinii. J. Nat. Prod. 2003, 66, 933–938. [Google Scholar] [CrossRef]
- Ren, Y.; Yuan, C.; Chai, H.B.; Ding, Y.; Li, X.C.; Ferreira, D.; Kinghorn, A.D. Absolute configuration of (−)-gambogic acid, an antitumor agent. J. Nat. Prod. 2011, 74, 460–463. [Google Scholar] [CrossRef] [PubMed]
- Coqueiro, A.; Choi, Y.; Verpoorte, R.; Gupta, K.; Mieri, M.; Hamburger, M.; Young, M.; Stapleton, P.; Gibbons, S.; Bolzani, V. Antistaphylococcal prenylated acylphoroglucinol and xanthones from Kielmeyera variabilis. J. Nat. Prod. 2016, 79, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Tiwari, R.; Sinha, S.; Danta, C.; Prasad, S. Antimicrobial evaluation of mangiferin and its synthesized analogues. Asian Pac. J. Trop. Biomed. 2012, 2, S884–S887. [Google Scholar] [CrossRef]
- Singh, S.; Sinha, S.; Prasad, S.; Kumar, R.; Bithu, B.; Kumar, S.; Singh, P. Synthesis and evaluation of novel analogues of mangiferin as potent antipyretic. Asian Pac. J. Trop. Biomed. 2011, 4, 866–869. [Google Scholar] [CrossRef]
- Zheng, M.; Lu, Z. Antiviral effect of mangiferin and isomangiferin on herpes simplex virus. Chin. Med. J. 1990, 103, 160–165. [Google Scholar] [PubMed]
- Zhu, X.; Song, J.; Huang, Z.; Wu, Y.; Yu, M. Antiviral activity of mangiferin against herpes simplex virus type 2 in vitro. Acta Pharm. Sin. 1993, 14, 452–454. [Google Scholar]
- Siler, B.; Zivkovic, S.; Banjanac, T.; Cvetkovic, J.; Zivkovic, J.; Ciric, A.; Sokovic, M.; Misic, D. Centauries as underestimated food additives: Antioxidant and antimicrobial potential. Food Chem. 2014, 147, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Moon, K.; Chung, B.; Shin, Y.; Rheingold, A.; Moore, C.; Park, S.; Park, S.; Lee, S.; Oh, K.; Shin, J.; et al. Pentacyclic antibiotics from a tidal mud flat-derived actinomycete. J. Nat. Prod. 2015, 78, 524–529. [Google Scholar] [CrossRef] [PubMed]
- Eltamany, E.; Abdelmohsen, U.; Ibrahim, A.; Hassanean, H.; Hentschel, U.; Ahmed, S.A. New antibacterial xanthone from the marine sponge-derived Micrococcus sp. EG45. Bioorg. Med. Chem. Lett. 2014, 24, 4939–4942. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Liao, Y.; Huang, X.; Tang, C.; Cai, P. A novel xanthone dimer derivative with antibacterial activity isolated from the bark of Garcinia mangostana. Nat. Prod. Res. 2018, 32, 1769–1774. [Google Scholar] [CrossRef]
- Zou, H.; Koh, J.J.; Li, J.; Qiu, S.; Aung, T.T.; Lin, H.; Lakshminarayanan, R.; Dai, X.; Tang, C.; Lim, F.H.; et al. Design and synthesis of amphiphilic xanthone-based, membrane-targeting antimicrobials with improved membrane selectivity. J. Med. Chem. 2013, 56, 2359–2373. [Google Scholar] [CrossRef]
- Proenca, C.; Albuquerque, H.M.; Ribeiro, D.; Freitas, M.; Santos, C.M.; Silva, A.M.; Fernandes, E. Novel chromone and xanthone derivatives: Synthesis and ROS/RNS scavenging activities. Eur. J. Med. Chem. 2016, 115, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Tiritan, M.E.; Ribeiro, A.R.; Fernandes, C.; Pinto, M.M.M. Chiral Pharmaceuticals; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2016; pp. 1–28. [Google Scholar]
- Chanllener, C.A. Chiral Drugs; Ashgate: Farnham, UK, 2001. [Google Scholar]
- Fernandes, C.; Masawang, K.; Tiritan, M.E.; Sousa, E.; de Lima, V.; Afonso, C.; Bousbaa, H.; Sudprasert, W.; Pedro, M.; Pinto, M. New chiral derivatives of xanthones: Synthesis and investigation of enantioselectivity as inhibitors of growth of human tumor cell lines. Bioorg. Med. Chem. 2014, 22, 1049–1062. [Google Scholar] [CrossRef]
- Fernandes, C.; Tiritan, M.; Cass, Q.; Kairys, V.; Fernandes, M.; Pinto, M. Enantioseparation and chiral recognition mechanism of new chiral derivatives of xanthones on macrocyclic antibiotic stationary phases. J. Chromatogr. Sep. Tech. 2012, 1241, 60–68. [Google Scholar] [CrossRef]
- Kodama, T.; Ito, T.; Dibwe, D.F.; Woo, S.Y.; Morita, H. Syntheses of benzophenone-xanthone hybrid polyketides and their antibacterial activities. Bioorg. Med. Chem. Lett. 2017, 27, 2397–2400. [Google Scholar] [CrossRef]
- Dibwe, D.; Awale, S.; Kadota, S.; Tezuka, Y. Muchimangins A–D: Novel diphenylmethyl-substituted xanthones from Securidaca longepedunculata. Tetrahedron Lett. 2012, 53, 6186–6190. [Google Scholar] [CrossRef]
- Dahiya, R.; Kumar, A.; Yadav, R. Synthesis and biological activity of peptide derivatives of iodoquinazolinones/nitroimidazoles. Molecules 2008, 13, 958–976. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Leng, J.; Rakesh, K.P.; Darshini, N.; Shubhavathi, T.; Vivek, H.K.; Mallesha, N.; Qin, H.-L. Synthesis and molecular docking studies of xanthone attached amino acids as potential antimicrobial and anti-inflammatory agents. Medchemcomm 2017, 8, 1706–1719. [Google Scholar] [CrossRef]
- Koh, J.J.; Zou, H.; Mukherjee, D.; Lin, S.; Lim, F.; Tan, J.K.; Tan, D.; Stocker, B.L.; Timmer, M.; Corkran, H.M.; et al. Amphiphilic xanthones as a potent chemical entity of anti-mycobacterial agents with membrane-targeting properties. Eur. J. Med. Chem. 2016, 123, 684–703. [Google Scholar] [CrossRef]
- Lin, S.; Koh, J.J.; Aung, T.T.; Lim, F.; Li, J.; Zou, H.; Wang, L.; Lakshminarayanan, R.; Verma, C.; Wang, Y.; et al. Symmetrically substituted xanthone amphiphiles combat gram-positive bacterial resistance with enhanced membrane selectivity. J. Med. Chem. 2017, 60, 1362–1378. [Google Scholar] [CrossRef] [PubMed]
- Koh, J.J.; Lin, S.; Aung, T.T.; Lim, F.; Zou, H.; Bai, Y.; Li, J.; Lin, H.; Pang, L.M.; Koh, W.L.; et al. Amino acid modified xanthone derivatives: Novel, highly promising membrane-active antimicrobials for multidrug-resistant Gram-positive bacterial infections. J. Med. Chem. 2015, 58, 739–752. [Google Scholar] [CrossRef]
- Koh, J.J.; Lin, S.; Bai, Y.; Sin, W.; Aung, T.T.; Li, J.; Chandra, V.; Pervushin, K.; Beuerman, R.; Liu, S. Antimicrobial activity profiles of amphiphilic xanthone derivatives are a function of their molecular oligomerization. BBA 2018, 860, 2281–2298. [Google Scholar] [CrossRef]
- Abd-El-Aziz, A.; Abdelghani, A.; El-Sadany, S.; Overy, D.; Kerr, R. Antimicrobial and anticancer activities of organoiron melamine dendrimers capped with piperazine moieties. Eur. Polym. J. 2016, 82, 307–323. [Google Scholar] [CrossRef]
- Szkaradek, N.; Rapacz, A.; Pytka, K.; Filipek, B.; Siwek, A.; Cegla, M.; Marona, H. Synthesis and preliminary evaluation of pharmacological properties of some piperazine derivatives of xanthone. Bioorg. Med. Chem. 2013, 21, 514–522. [Google Scholar] [CrossRef]
- Másson, M.; Holappa, J.; Hjálmarsdóttir, M.; Rúnarsson, Ö.; Nevalainen, T.; Järvinen, T. Antimicrobial activity of piperazine derivatives of chitosan. Carbohydr. Polym. 2008, 74, 566–571. [Google Scholar] [CrossRef]
- Ahmed, A.; Molvi, K.; Nazim, S.; Baig, I.; Memon, T.; Rahil, M. The importance of six membered saturated nitrogen containing ring in psychological disorders. J. Chem. Pharm. Res. 2012, 4, 872–880. [Google Scholar]
- Akkoc, M.; Yuksel, M.; Durmaz, I.; Atalay, R. Design, synthesis, and biological evaluation of indole-based 1,4-disubstituted piperazines as cytotoxic agents. Turk. J. Chem. 2012, 36, 515–525. [Google Scholar]
- Ibezim, E.; Duchowicz, P.; Ortiz, E.; Castro, E. QSAR on aryl-piperazine derivatives with activity on malaria. Chemom. Intell. Lab. Syst. 2012, 110, 81–88. [Google Scholar] [CrossRef]
- Jain, V.; Jain, B.; Sharma, U.; Saha, D. Synthesis, characterization and antimicrobial screening of some 4-substitued-1-(4-substitued phenyl) piperazine derivatives. Int. J. Curr. Pharm. Res. 2011, 3, 66–70. [Google Scholar]
- Shaquiquzzaman, M.; Verma, G.; Marella, A.; Akhter, M.; Akhtar, W.; Khan, M.F.; Tasneem, S.; Alam, M.M. Piperazine scaffold: A remarkable tool in generation of diverse pharmacological agents. Eur. J. Med. Chem. 2015, 102, 487–529. [Google Scholar] [CrossRef] [PubMed]
- Chimenti, F.; Bizzarri, B.; Bolasco, A.; Secci, D.; Chimenti, P.; Granese, A.; Carradori, S.; Rivanera, D.; Zicari, A.; Scaltrito, M.M.; et al. Synthesis, selective anti-Helicobacter pylori activity, and cytotoxicity of novel N-substituted-2-oxo-2H-1-benzopyran-3-carboxamides. Bioorg. Med. Chem. Lett. 2010, 20, 4922–4926. [Google Scholar] [CrossRef] [PubMed]
- Klesiewicz, K.; Karczewska, E.; Budak, A.; Marona, H.; Szkaradek, N. Anti-Helicobacter pylori activity of some newly synthesized derivatives of xanthone. J. Antibiot. 2016, 69, 825–834. [Google Scholar] [CrossRef]
- Szkaradek, N.; Stachura, K.; Waszkielewicz, A.; Cegla, M.; Szneler, E.; Marona, H. Synthesis and antimycobacterial assay of some xanthone derivatives. Acta Pol. Pharm. 2008, 65, 21–28. [Google Scholar] [PubMed]

| No. | Name/Structure | Antimicrobial Activity (MIC) |
|---|---|---|
| 1N | Mangostanin | Mycobacterium tuberculosis H37Ra (25 µM) |
| 2N | Toxyloxanthone-C | Candida albicans (25 µM); Candida glabrata (8 µM); Aspergillus fumigatus (8 µM); Aspergilus nidulans (8 µM); Cryptococcus neoformans (8 µM); Bacillus substilis PCI-219 (3.13 µM); MSSA JMC-2874 (6.25 µM); MRSA (6.25 µM); Micrococcus Luteus (12.5 µM) |
| 3N | Gerontoxanthone-G | B. subtilis PCI-219 (12.5 µM); MSSA JMC-2874 (12.5 µM); MRSA (12.5 µM); M. luteus (12.5 µM) |
| 4N | Gerontoxanthone-A | B. subtilis PCI-219 (<25 µM); MSSA JMC-2874 (<25 µM); MRSA (<25 µM); M. luteus (<25 µM); Enterococcus faecalis (VSE) (>25 µg/mL); E. faecalis (VanA) (>25 µg/mL); E. faecalis (VanB) (>25 µg/mL); Enterococcus gallinarum (VanC) (>25 µg/mL) |
| 5N | Formoxanthone-C | B. Substilis (4.6 µM); S. aureus (2.3 µM); Streptococcus faecalis (18.7 µM); Salmonella Typhi (4.6 µM) |
| No. | Name/Structure | Antimicrobial Activity (MIC) |
|---|---|---|
| 6N | Mangostanol | M. tuberculosis H37Ra (200 µg/mL) |
| 7N | Tovophyllin-B | M. tuberculosis H37Ra (25 µM) |
| 8N | Calozeyloxanthone | 17 MRSA strains and 25 MSSA strains (range 4.1–8.1 µg/mL) |
| 9N | Smeathxanthone B | Escherichia coli (625 µg/mL), Klebsiella pneumoniae (625 µg/mL), Proteus vulgaris (312.5 µg/mL), S. typhi (625 µg/mL), S. faecalis (625 µg/mL), C. albicans (312.5 µg/mL), C. krusei (312.25 µg/mL) |
| 10N | Artoindonesianin-C | M. tuberculosis H37Ra (12.5 µM) |
| 11N | Cowagarcinone-D | MRSA-SK1 (128 µg/mL); S. aureus (inactive); E. coli (128 µg/mL); Salmonella typhimurium (128 µg/mL) |
| No. | Name/Structure | Antimicrobial Activity (MIC) |
|---|---|---|
| 12N | Fuscaxanthone I | Helicobacter pylori ATCC 43504 (30.5 µM); H. pylori DMST 20165 (15.2 µM); H. pylori HP40 (122.0 µM) |
| 13N | Caledol | A. fumigatus (32 µM); C. albicans (inactive) |
| 14N | Dicaledol | A. fumigatus (1 µM); C. albicans (inactive) |
| 15N | Mangostenol | M. tuberculosis H37Ra (100 µM) |
| No. | Name/Structure | a | Antimicrobial Activity (MIC) |
|---|---|---|---|
| 16N | Scortechinone A | +18° (0.028) | S. aureus (128 µg/mL); S aureus SK1 (128 µg/mL); MRSA (128 µg/mL) |
| 17N | Scortechinone B | −105° (0.095) | S. aureus (8 µg/mL); S aureus SK1 (2 µg/mL); MRSA (2 µg/mL) |
| 18N | Scortechinone C | −107° (0.014) | S. aureus (32 µg/mL); S aureus SK1 (32 µg/mL); MRSA (32 µg/mL) |
| 19N | Scortechinone D | +222° (0.018) | S. aureus (>256 µg/mL); S aureus SK1 (>256 µg/mL) |
| 20N | Scortechinone E | −240° (0.025) | S. aureus (>256 µg/mL); S aureus SK1 (>256 µg/mL) |
| 21N | Scortechinone F | −333° (0.015) | S. aureus (16 µg/mL); S aureus SK1 (4 µg/mL) |
| 22N | Scortechinone G | −95° (0.021) | S. aureus (>64 µg/mL); S aureus SK1 (>64 µg/mL) |
| 23N | Scortechinone H | −120° (0.025) | S. aureus (>64 µg/mL); S aureus SK1 (4 µg/mL) |
| 24N | Scortechinone I | +43° (0.023) | S. aureus (8 µg/mL); S aureus SK1 (8 µg/mL) |
| 25N | Scortechinone J | −200° (0.015) | S. aureus (32 µg/mL); S aureus SK1 (8 µg/mL) |
| 26N | Scortechinone K | +48° (0.021) | S. aureus (128 µg/mL); S aureus SK1 (128 µg/mL) |
| 27N | Scortechinone L | −176° (0.017) | S. aureus (>64 µg/mL); S aureus SK1 (>64 µg/mL) |
| 28N | Scortechinone M | −353° (0.017) | S. aureus (32 µg/mL); S aureus SK1 (32 µg/mL) |
| 29N | Scortechinone N | −263° (0.019) | S. aureus (32 µg/mL); S aureus SK1 (32 µg/mL) |
| 30N | Scortechinone O | +77° (0.013) | S. aureus (>128 µg/mL); S aureus SK1 (>128 µg/mL) |
| 31N | Scortechinone P | +83° (0.012) | S. aureus (32 µg/mL); S aureus SK1 (16 µg/mL) |
| 32N | 2-isoprenylforbesione | MRSA USA300 SF8300 (7.20 mm b; >400 µM); MSSA ATCC 25923 (7.56 mm b; 400 µM) | |
| 33N | Deoxygamboginin | MRSA USA300 SF8300 (6 mm b); MSSA ATCC 25923 (6 mm b) | |
| 34N | Hanburin | MRSA USA300 SF8300 (6 mm b); MSSA ATCC 25923 (6 mm b) | |
| 35N | Forbesione | MRSA USA300 SF8300 (7.97 mm b; >400 µM); MSSA ATCC 25923 (7.86 mm b, 200 µM) | |
| 36N | Dihydroisomorellin | MRSA USA300 SF8300 (6 mm b); MSSA ATCC 25923 (6 mm b) |
| No. | Name/Structure | a | Antimicrobial Activity (MIC or Zone of Growth) |
|---|---|---|---|
| 37N | Hanburinone | −62° (0.09) | MRSA (200 µM) |
| 38N | Isomoreollin B | −44° (0.11) | MRSA (200 µM) |
| 39N | Morellin | −600° (0.04) | MRSA (200 µM) |
| 40N | Moreollic acid | −39° (0.22) | MRSA (25 µM) |
| 41N | Morellic acid | −541° (0.19) | MRSA (25 µM); MRSA USA300 SF8300 (19.52 mmb; 12.5 µM); MSSA ATCC 25923 (19.23 mm b; 12.5 µM) |
| 42N | Deoxymorellin | MRSA USA300 SF8300 (6 mm b); MSSA ATCC 25923 (6 mm b) | |
| 43N | Isomorellinol | MRSA USA300 SF8300 (8.57 mm b); MSSA ATCC 25923 (7.75 mm b) | |
| 44N | Gambogic acid | (0.17) = −714.1° | MRSA USA300 SF8300 (17.29 mm b; 25 µM); MSSA ATCC 25923 (16.59 mm b; 12.5 µM) |
| No. | Name/Structure | Antimicrobial Activity (MIC or Zone of Growth) |
|---|---|---|
| 45N | Kielcorin = −70.0° (0.01) a | S. aureus-1199B (>512 mg/L); MRSA XU212 (>512 mg/L); S. aureus ATCC 25923 (>512 mg/L); MRSA RN4220 (>512 mg/L); EMRSA-15 (>512 mg/L); EMRSA-16 (>512 mg/L) |
| 46N | Mangiferin | Bacillus pumilus (18 mm b); B. cereus (15 mm b); Salmonella enterica serotype Virchow (22 mm b); Pseudomonas aeruginosa (0 mm b); Aspergillus flavus (0 mm b; 12 mm c); Thermoascus aurantiacus (0 mm b; 18 mm c); B. cereus (40 µg/mL); Mariniluteicoccus flavus (40 µg/mL); Listeria monocytogenes (40 µg/mL); E. coli (40 µg/mL); Enterobacter cloacae (40 µg/mL); P. aeruginosa (40 µg/mL); S. typhimurium (40 µg/mL); Penicillium funiculosum (40 µg/mL); Penicillium ochrochloron (40 µg/mL); Trichoderma viride (40 µg/mL); A. fumigatos (20 µg/mL); A. niger (40 µg/mL); A. flavus (40 µg/mL); A. versicolor (20 µg/mL); C. albicans (40 µg/mL) |
| 47N | Buanmycin = +72.0° (0.5) a | S. aureus (10.5 µM); B. subtilis (0.7 µM); Kocuria rhizophila (10.5 µM) |
| 48N | Microluside-A | E. faecalis JH212 (10 µM); S. aureus NCTC 8325 (13 µM) |
| 49N | Garmoxanthone | 2strains of MRSA (3.9 µg/mL); 2 strains of Vibrio vulnificus (15.6 µg/mL); Vibrio rotiferianus (15.6 µg/mL); Vibrio campbellii (31.2 µg/mL) |
| No. | Structure | a | Antimicrobial Activity (MIC) |
|---|---|---|---|
| 1S |  | ± | S. aureus (10.0 µM); B. subtilis (50.0 µM) |
| +2.5 (0.02) | S. aureus (10.0 µM); B. subtilis (50.0 µM) | ||
| −28.0 (0.02) | S. aureus (12.5 µM); B. subtilis (100.0 µM) | ||
| 2S |  | ± | S. aureus (10.0 µM); B. subtilis (12.5 µM) |
| + | S. aureus (10.0 µM); B. subtilis (10.0 µM) | ||
| - | S. aureus (10.0µM); B. subtilis (12.5 µM) | ||
| 3S |  | ± | S. aureus (25.0 µM); B. subtilis (>100.0 µM) |
| + | S. aureus (10.0 µM); B. subtilis (>100.0 µM) | ||
| - | S. aureus (50.0 µM); B. subtilis (>100.0 µM) | ||
| 4S |  | ± | S. aureus (>100 µM); B. subtilis (>100.0 µM) |
| 5S |  | ± | S. aureus (>100 µM); B. subtilis (>100.0 µM) |

| No. | R | Antimicrobial Activity (Inhibitory Growth Zones) |
|---|---|---|
| 45N | H (Mangiferin) | B. pumilus (18 mm); B. cereus (15 mm); S. virchow (22 mm); P. aeruginosa (0 mm); A. flavus (0 mm; 12 mm *); T. aurantiacus (0 mm; 18 mm *) |
| 6S |  | B. pumilus (16 mm); B. cereus (12 mm); S. virchow (19 mm); P. aeruginosa (0 mm; 10 mm *); A. flavus (0 mm; 11 mm *); T. aurantiacus (0 mm; 14 mm *) |
| 7S |  | B. pumilus (15 mm); B. cereus (12 mm); S. virchow (20 mm); P. aeruginosa (0 mm; 8 mm *); A. flavus (0 mm; 11 mm *); T. aurantiacus (0 mm; 13 mm *) |
| 8S |  | B. pumilus (17 mm); B. cereus (15 mm); S. virchow (20 mm); P. aeruginosa (0 mm; 10 mm *); A. flavus (0 mm; 14 mm *); T. aurantiacus (0 mm; 15 mm *) |
| 9S |  | B. pumilus (18 mm); B. cereus (14 mm); S. virchow (20 mm); P. aeruginosa (0 mm; 9 mm *); A. flavus (0 mm; 11 mm *); T. aurantiacus (0 mm; 16 mm *) |
| 10S |  | B. pumilus (17 mm); B. cereus (14 mm); S. virchow (19 mm); P. aeruginosa (0 mm; 9 mm *); A. flavus (0 mm; 12 mm *); T. aurantiacus (0 mm; 14 mm *) |
| 11S |  | B. pumilus (18 mm); B. cereus (13 mm); S. virchow (18 mm); P. aeruginosa (0 mm; 10 mm *); A. flavus (0 mm; 11 mm *); T. aurantiacus (0 mm; 15 mm *) |

| No. | Structure/R | Antimicrobial Activity (Inhibitory Growth Zones/MIC) |
|---|---|---|
| 12S |  | S. aureus (6 mm-25 µg/mL); B. substilis (8 mm-25 µg/mL); E. coli (17 mm-25 µg/mL); K. pneumonia (6 mm-25 µg/mL) |
| 13S |  | S. aureus (10 mm-25µg/mL); B. substilis (7 mm-25 µg/mL); E. coli (8 mm-25 µg/mL); K. pneumonia (5 mm-25 µg/mL) |
| 14S |  | S. aureus (7 mm-25 µg/mL); B. substilis (11 mm-25 µg/mL); E. coli (4 mm-25 µg/mL); K. pneumonia (8 mm-25 µg/mL) |
| 15S |  | S. aureus (4 mm-25 µg/mL); B. substilis (7 mm-25 µg/mL); E. coli (8 mm-25 µg/mL); K. pneumonia (7 mm-25 µg/mL) |
| 16S |  | S. aureus (18 mm-25 µg/mL); B. substilis (17 mm-25 µg/mL); E. coli (16 mm-25 µg/mL); K. pneumonia (20 mm-25 µg/mL) |
| 17S |  | S. aureus (20 mm-25 µg/mL); B. substilis (20 mm-25 µg/mL); E. coli (20 mm-25 µg/mL); K. pneumonia (18 mm-25 µg/mL) |
| 18S |  | S. aureus (22 mm-25 µg/mL); B. substilis (23 mm-25 µg/mL); E. coli (24 mm-25 µg/mL); K. pneumonia (22 mm-25 µg/mL) |
| 19S |  | S. aureus (20 mm-25 µg/mL); B. substilis (20mm-25 µg/mL); E. coli (18 mm-25 µg/mL); K. pneumonia (18 mm-25 µg/mL) |
| 20S |  | S. aureus (15 mm-25 µg/mL); B. substilis (13 mm-25 µg/mL); E. coli (16 mm-25 µg/mL); K. pneumonia (16 mm-25 µg/mL) |
| 21S |  | S. aureus (17mm-25 µg/mL); B. substilis (15mm-25 µg/mL); E. coli (17 mm-25 µg/mL); K. pneumonia (13 mm-25 µg/mL) |
| 22S |  | S. aureus (9 mm-25 µg/mL); B. substilis (11 mm-25 µg/mL); E. coli (15 mm-25 µg/mL); K. pneumonia (8 mm-25 µg/mL) |
| 23S |  | S. aureus (14 mm-25 µg/mL); B. substilis (10 mm-25 µg/mL); E. coli (11 mm-25 µg/mL); K. pneumonia (16 mm-25 µg/mL) |
| 24S |  | S. aureus (9 mm-25 µg/mL); B. substilis (13 mm-25 µg/mL); E. coli (8 mm-25 µg/mL); K. pneumonia (10 mm-25 µg/mL) |
| 25S |  | S. aureus (7 mm-25 µg/mL); B. substilis (11 mm-25 µg/mL); E. coli (10 mm-25 µg/mL); K. pneumonia (8 mm-25 µg/mL) |
| 26S |  | S. aureus (22 mm - 25 µg/mL); B. substilis (22 mm - 25 µg/mL); E. coli (20 mm - 25 µg/mL); K. pneumonia (23 mm - 25 µg/mL) |
| 27S |  | S. aureus (23 mm-25 µg/mL); B. substilis (23 mm-25 µg/mL); E. coli (21 mm-25 µg/mL); K. pneumonia (21 mm-25 µg/mL) |
| 28S |  | S. aureus (24 mm-25 µg/mL); B. substilis (26 mm-25 µg/mL); E. coli (26 mm-25 µg/mL); K. pneumonia (23 mm-25 µg/mL) |
| 29S |  | S. aureus (20 mm-25 µg/mL); B. substilis (19 mm-25 µg/mL); E. coli (19 mm-25 µg/mL); K. pneumonia (15 mm-25 µg/mL) |
| 30S |  | S. aureus (17 mm-25 µg/mL); B. substilis (15 mm-25 µg/mL); E. coli (17 mm-25 µg/mL); K. pneumonia (17 mm-25 µg/mL) |
| 31S |  | S. aureus (20 mm-25 µg/mL); B. substilis (18 mm-25 µg/mL); E. coli (20 mm-25 µg.mL); K. pneumonia (18 mm-25 µg.mL) |

| No. | Structure/R | Antimicrobial Activity (MIC) |
|---|---|---|
| 32S |  | S. aureaus (6 µg/mL); MRSA DM21455 (12 µg/mL); MRSA DM09809R (6 µg/mL); B. cereus ATCC 11778 (12 µg/mL) |
| 33S |  | S. aureaus (>50 µg/mL); MRSA DM21455 (>50 µg/mL); MRSA DM09809R (>50 µg/mL); B. cereus ATCC 11778 (>50 µg/mL); Mycobacetrium smegmatis (>24.9 µg/mL); M. bovis (>24.9 µg/mL) |
| 34S |  | S. aureaus DM4001 (2 µg/mL); MRSA DM21455 (3 µg/mL); MRSA DM09809R (3 µg/mL); B. cereus ATCC 11778 (2 µg/mL); M. smegmatis (>25.1 µg/mL); M. bovis (>25.1 µg/mL); MSSA (7 strains) (2–4 µg/mL); VISA (4 µg/mL); MRSA (10 strains) (2-4 µg/mL); EMRSA (3 strains) (2–4 µg/mL); teicoplanin-RI (2 µg/mL); MDR (2 µg/mL); Staphylococcus epidermidis (2 strains) (2 µg/mL); VSE (3 strains) (2–4 µg/mL); VRE (5 strains) (2–4 µg/mL); Streptococcus (4 strains) (4–8 µg/mL); Corynebacterium jeikeium and L. monocytogenes (4–8 µg/mL) |
| 35S |  | S. aureaus (6 µg/mL); MRSA DM21455 (6 µg/mL); MRSA DM09809R (12 µg/mL). B. cereus ATCC 11778 (12 µg/mL) |
| 36S |  | S. aureaus DM4001 (6 µg/mL); MRSA DM21455 (1 µg/mL); MRSA DM09809R (6 µg/mL); B. cereus ATCC 11778 (6 µg/mL); M. smegmatis (>26.1 µg/mL); M. bovis (>11.1 µg/mL) |
| 37S |  | S. aureaus (12 µg/mL); MRSA DM21455 (12 µg/mL); MRSA DM09809R (12 µg/mL). B. cereus ATCC 11778 (12 µg/mL) |
| 38S |  | S. aureaus (0.5 µg/mL); MRSA DM21455 (2 µg/mL); MRSA DM09809R (3 µg/mL); B. cereus ATCC 11778 (3 µg/mL); MSSA (7 strains) 2–4; VISA 2; MRSA (10 strains) (2 µM); EMRSA (3 strains) (2 µM); teicoplanin-RI (2 µg/mL); MDR (2 µM); S. epidermidis (2 strains) (2 µM); VSE (3 strains) (2–4 µM); VRE (5 strains) (1–2 µM); Streptococcus (4 strains) (2–8 µM); C. jeikeium and L. monocytogenes (2–4 µM) |
| 39S |  | M. smegmatis (>19.3 µg/mL); M. bovis (>19.3 µg/mL) |
| 40S |  | M. smegmatis (>21.8 µg/mL); M. bovis (>21.8 µg/mL) |
| 41S |  | M. smegmatis (>24.5 µg/mL); M. bovis (>24.5 µg/mL) |
| 42S |  | M. smegmatis (>21.8 µg/mL); M. bovis (>4.6 µg/mL) |
| 43S |  | M. smegmatis (>4.3 µg/mL); M. bovis (>4.3 µg/mL) |
| 44S |  | M. smegmatis (>19.9 µg/mL); M. bovis (>22.9 µg/mL) |

| No. | Structure | Inhibitory Growth Zones [mm] a | |||
|---|---|---|---|---|---|
| Other Strains | Clarithromycin Resistant H. Pylori Strains | Metronidazole Resistant H. Pylori Strains | Double Resistant H. Pylori Strains | ||
| 45S | R1=R3=H; R2=Me | S. aureaus ATCC 25923-13; MRSA 14.002-23; E. coli ATCC 25922-8 | ATCC 700684-36 HP 132/194-40 HP 115/168-40 | ATCC 43504-42 HP 125/180-40 HP 139/202-44 HP 143/207-44 | HP 126/181-40 HP 106/154-39 |
| 46S | R1=R3=H; R2=Me | S. aureaus ATCC 25923-11; MRSA 14.002-18 | ATCC 700684-32 HP 132/194-34 HP 115/168-26 | ATCC 43504-35 HP 125/180-36 HP 139/202-46 HP 143/207-29 | HP 126/181-40 HP 106/154-33 |
| 47S | R1=R3=H; R2=Me | S. aureaus ATCC 25923-15; MRSA 14.002-23; E. coli ATCC 25922-10 | ATCC 700684-34 HP 132/194-42 HP 115/168-46 | ATCC 43504-54 HP 125/180-46 HP 139/202-52 HP 143/207-58 | HP 126/181-50 HP 106/154-47 |
| 48S | R1=R2=R3=H | ATCC 700684-28 HP 132/194-30 HP 115/168-30 | ATCC 43504-21 HP 125/180-28 HP 139/202-38 HP 143/207-36 | HP 126/181-28 HP 106/154-26 | |
| 49S | R1=R2=R4=H | S. aureaus ATCC 25923-12; MRSA 14.002-15; E. coli ATCC 2592-9 | ATCC 700684-35 HP 132/194-42 HP 115/168-38 | ATCC 43504-41 HP 125/180-36 HP 139/202-48 HP 143/207-42 | HP 126/181-48 HP 106/154-39 |
| 50S | R1=R2=R4=H | ATCC 700684-24 HP 132/194-22 HP 115/168-17 | ATCC 43504-11 HP 125/180-17 HP 139/202-26 HP 143/207-22 | HP 126/181-23 HP 106/154-16 | |
| 51S | R1=R2=R4=H | S. aureaus ATCC 25923-12; MRSA 14.002-11 | ATCC 700684-34 HP 132/194-32 HP 115/168-31 | ATCC 43504-36 HP 125/180-40 HP 139/202-40 HP 143/207-32 | HP 126/181-34 HP 106/154-31 |
| 52S | R1=R2=R4=H | ATCC 700684-20 HP 132/194-16 HP 115/168-25 | ATCC 43504-19 HP 125/180-20 HP 139/202-20 HP 143/207-22 | HP 126/181-20 HP 106/154-21 | |
| 53S | R1=R2=R4=H | ATCC 700684-27 HP 132/194-29 HP 115/168-34 | ATCC 43504-28 HP 125/180-32 HP 139/202-38 HP 143/207-32 | HP 126/181-38 HP 106/154-31 | |
| 54S | R1=R2=R4=H | ATCC 700684-25 HP 132/194-30 HP 115/168-33 | ATCC 43504-23 HP 125/180-35 HP 139/202-32 HP 143/207-36 | HP 126/181-36 HP 106/154-34 | |
| 55S | R1=R2=R4=H | S. aureaus ATCC 25923-9; MRSA 14.002-11 | ATCC 700684-38 HP 132/194-48 HP 115/168-44 | ATCC 43504-39 HP 125/180-50 HP 139/202-54 HP 143/207-50 | HP 126/181-56 HP 106/154-45 |
| 56S | R1=Cl; R2=R4=H | S. aureaus ATCC 25923-10; MRSA 14.002-16 | ATCC 700684-34 HP 132/194-40 HP 115/168-40 | ATCC 43504-37 HP 125/180-40 HP 139/202-40 HP 143/207-48 | HP 126/181-45 HP 106/154-40 |
| 57S | R1=Cl; R2=R4=H | S. aureaus ATCC 25923-12; MRSA 14.002-13 | ATCC 700684-26 HP 132/194-22 HP 115/168-25 | ATCC 43504-25 HP 125/180-32 HP 139/202-28 HP 143/207-23 | HP 126/181-25 HP 106/154 -21 |
| 58S | R1=Cl; R2=R4=H | S. aureaus ATCC 25923-16; MRSA 14.002-16; E. coli ATCC 25922-9 | ATCC 700684-35 HP 132/194-44 HP 115/168-46 | ATCC 43504-50 HP 125/180-42 HP 139/202-40 HP 143/207-50 | HP 126/181-26 HP 106/154-30 |
| 59S | R1=Cl; R2=R4=H | S. aureaus ATCC 25923-17; MRSA 14.002-15; E. coli ATCC 25922-9 | ATCC 700684-34 HP 132/194-36 HP 115/168-38 | ATCC 43504-28 HP 125/180-32 HP 139/202-32 HP 143/207-33 | HP 126/181-41 HP 106/154-35 |
| 60S | R1=Cl; R2=R4=H | S.aureaus ATCC 25923-12; MRSA 14.002-15 | ATCC 700684-23 HP 132/194-19 HP 115/168-24 | ATCC 43504-15 HP 125/180-18 HP 139/202-31 HP 143/207-26 | HP 126/181-20 HP 106/154-19 |
| 61S | R1=Cl; R2=R4=H | S. aureaus ATCC 259-16; MRSA 14.002-16 | ATCC 700684-30 HP 132/194-32 HP 115/168-28 | ATCC 43504-24 HP 125/180-28 HP 139/202-36 HP 143/207-40 | HP 126/181-26 HP 106/154-26 |
| 62S | R1=Cl; R2=R4=H | ATCC 700684-22 HP 132/194-24 HP 115/168-27 | ATCC 43504-24 HP 125/180-27 HP 139/202-26 HP 143/207-24 | HP 126/181-25 HP 106/154-24 | |
| 63S | R1=Cl; R2=R4=H | S. aureaus ATCC 25923-9; MRSA 14.002-9 | ATCC 700684-19 HP 132/194-22 HP 115/168-25 | ATCC 43504-22 HP 125/180-29 HP 139/202-30 HP 143/207-25 | HP 126/181-27 HP 106/154-25 |
| No. | Structure | Antimicrobial Activity (MIC or Inhibitory Growth Zones *) |
|---|---|---|
| 64S |  | MRSA USA300 SF8300 (22.24 mm; 25 µM); MSSA ATCC 25923 (19.99 mm; 12.5 µM) |
| 65S |  | MRSA USA300 SF8300 (16.27 mm; 25 µM); MSSA ATCC 25923 (17.07 mm; 12.5 µM) |
| 66S |  | MRSA USA300 SF8300 (6.27 mm); MSSA ATCC 25923 (6.53 mm) |
| 67S |  | MRSA USA300 SF8300 (6 mm); MSSA ATCC 25923 (6 mm) |
| 68S |  | MRSA USA300 SF8300 (9.53 mm); MSSA ATCC 25923 (7.09 mm) |
| 69S |  | MRSA USA300 SF8300 (18.34 mm; 25 µM); MSSA ATCC 25923 (16.52 mm; 25 µM) |
| 70S |  | MRSA USA300 SF8300 (6.28 mm); MSSA ATCC 25923 (6.09 mm) |
| 71S |  | MRSA USA300 SF8300 (19.35 mm; 25 µM); MSSA ATCC 25923 (15.91 mm; 25 µM) |
| 72S |  | MRSA USA300 SF8300 (15.91 mm; 100 µM); MSSA ATCC 25923 (13.08 mm; 50 µM) |
| 73S |  | MRSA USA300 SF8300 (8.21 mm); MSSA ATCC 25923 (6.89 mm) |
| 74S |  | MRSA USA300 SF8300 (9.09 mm); MSSA ATCC 25923 (7.50 mm) |
| 75S |  | MRSA USA300 SF8300 (6 mm; 25 µM); MSSA ATCC 25923 (6 mm; 12.5 µM) |

| No. | Structure | Antimicrobial Activity (Inhibitory Growth Zones or MIC) |
|---|---|---|
| 76S | R1=H | aC. lusitaniae (8 mm); T. mentagrophytes (18 mm); S. aureus (9 mm); E.faecalis (9 mm) |
| 77S | R1=Cl | aT. mentagrophytes (12 mm) |
| 78S | R1=H | M. tuberculosis H37Rv (>2.5% with 35% inhibition) |
| 79S | R1=H | M. tuberculosis H37Rv (>2.5% with 32% inhibition) |
| 80S | R1=H | M. tuberculosis H37Rv (>2.5% with 35% inhibition) |
| 81S | R1=H | M. tuberculosis H37Rv (>2.5% with 34% inhibition) |
| 82S | R1=H | M. tuberculosis H37Rv (>2.5% with 63% inhibition) |
| 83S | R1=H | M. tuberculosis H37Rv (>2.5% with 3% inhibition) |
| 84S | R1=H | M. tuberculosis H37Rv (>2.5% with 25% inhibition) |
| 85S | R1=H | M. tuberculosis H37Rv (>2.5% with 14% inhibition) |
| 86S | R1=H | M. tuberculosis H37Rv (<2.5% with 94% inhibition) |
| 87S | R1=H | M. tuberculosis H37Rv (>2.5% with 24% inhibition) |
| 88S | R1=H | M. tuberculosis H37Rv (>2.5% with 59% inhibition) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araújo, J.; Fernandes, C.; Pinto, M.; Tiritan, M.E. Chiral Derivatives of Xanthones with Antimicrobial Activity. Molecules 2019, 24, 314. https://doi.org/10.3390/molecules24020314
Araújo J, Fernandes C, Pinto M, Tiritan ME. Chiral Derivatives of Xanthones with Antimicrobial Activity. Molecules. 2019; 24(2):314. https://doi.org/10.3390/molecules24020314
Chicago/Turabian StyleAraújo, Joana, Carla Fernandes, Madalena Pinto, and Maria Elizabeth Tiritan. 2019. "Chiral Derivatives of Xanthones with Antimicrobial Activity" Molecules 24, no. 2: 314. https://doi.org/10.3390/molecules24020314
APA StyleAraújo, J., Fernandes, C., Pinto, M., & Tiritan, M. E. (2019). Chiral Derivatives of Xanthones with Antimicrobial Activity. Molecules, 24(2), 314. https://doi.org/10.3390/molecules24020314