The Metabolomic Profile of Lymphoma Subtypes: A Pilot Study
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Population
4.2. Samples Preparation and GC-MS Analysis
4.3. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Soerjomataram, L.; Ervik, M.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 11 [Internet]; International Agency for Research on Cancer: Lyon, France, 2013; Available online: http://globocan.iarc.fr (accessed on 26 June 2019).
- Swerdlow, S.H.; Campo, E.; Harris, N.L.; Jaffe, E.S.; Pileri, S.A.; Stein, H.; Vardiman, J.W. World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th ed.; IARC Press: Lyon, France, 2008. [Google Scholar]
- Klupczyńska, A.; Dereziński, P.; Kokot, Z.J. Metabolomics in medical sciences–trends, challenges and perspectives. Acta Pol. Pharm. 2015, 72, 629–641. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.; Shah, S.H.; Corwin, E.J.; Fiehn, O.; Fitzgerald, R.K.; Gerszten, R.E.; Illig, T.; Rhee, E.P.; Srinivas, P.R.; Wang, T.J.; et al. Potential impact and study considerations of metabolomics in cardiovascular health and disease: A scientific statement from the American Heart Association. Circ. Cardiovasc. Genet. 2017, 10, e000032. [Google Scholar] [CrossRef] [PubMed]
- Spratlin, J.L.; Serkova, N.J.; Eckhardt, S.G. Clinical applications of metabolomics in oncology: A review. Clin Cancer Res. 2009, 15, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Allegra, A.; Innao, V.; Gerace, D.; Bianco, O.; Musolino, C. The metabolomic signature of hematologic malignancies. Leukemia Res. 2016, 49, 22–35. [Google Scholar] [CrossRef] [PubMed]
- Yoo, B.C.; Kong, S.Y.; Jang, S.G.; Kim, K.H.; Ahn, S.A.; Park, W.S.; Park, S.; Yun, T.; Eom, H.-S. Identification of hypoxanthine as a urine marker for non-Hodgkin lymphoma by low-mass-ion profiling (LC-MS). BMC Cancer 2010, 10, 55. [Google Scholar] [CrossRef] [PubMed]
- Medriano, C.A.D.; Na, J.; Lim, K.M.; Chung, J.H.; Park, Y.H. Liquid Chromatography Mass Spectrometry-Based Metabolite Pathway Analyses of Myeloma and Non-Hodgkin’s Lymphoma Patients. Cell J. 2017, 19 (Suppl. 1), 44–54. [Google Scholar] [CrossRef]
- Ducker, G.S.; Ghergurovich, J.M.; Mainolfi, N.; Suri, V.; Jeonga, S.K.; Hsin-Jung Li, S.; Friedman, A.; Manfredi, M.G.; Gitai, Z.; Kim, H.; et al. Human SHMT inhibitors reveal defective glycine import as a targetable metabolic vulnerability of diffuse large B-cell lymphoma. Proc. Natl. Acad. Sci. USA 2017, 114, 11404–11409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piszcz, J.; Lemancewicz, D.; Dudzik, D.; Ciborowski, M. Differences and similarities between LC-MS derived serum fingerprints of patients with B-cell malignancies. Electrophoresis 2013, 34, 2857–2864. [Google Scholar] [CrossRef]
- Zhou, J.; Yu, S.; Wang, Y.; Gu, X.; Wu, Q.; Xue, Y.; Shan, G.; Zhang, H.; Zhao, W.; Yan, C. Serum metabolite profiling of B-cell non-Hodgkin’s lymphoma using UPLC-QTOFMS and GC-TOFMS. Metabolomics 2013, 10, 677–687. [Google Scholar] [CrossRef]
- Pera, B.; Krumsiek, J.; Assouline, S.E.; Marullo, R.; Patel, J.; Phillip, J.M.; Romána, L.; Mannc, K.K.; Cerchiettia, L. Metabolomic profiling reveals cellular reprogramming of B-Cell lymphoma by a lysine deacetylase inhibitor through the choline pathway. EBioMedicine 2018, 28, 80–89. [Google Scholar] [CrossRef]
- Puchades-Carrasco, L.; Lecumberri, R.; Martinez-Lopez, J.; Lahuerta, J.J.; Mateos, M.V.; Prosper, F.; San-Miguel, J.F.; Pineda-Lucena, A. Multiple myeloma patients have a specific serum metabolomic profile that changes after achieving complete remission. Clin. Cancer Res. 2013, 19, 4770–4779. [Google Scholar] [CrossRef] [PubMed]
- Wojtowicz, W.; Chachaj, A.; Olczak, A.; Ząbek, A.; Piątkowska, E.; Rybka, J.; Butrym, A.; Biedroń, M.; Mazur, G.; Wróbel, T.; et al. Serum NMR metabolomics to differentiate haematologic malignancies. Oncotarget 2018, 9, 24414–24427. [Google Scholar] [CrossRef] [PubMed]
- Stenson, M.; Pedersen, A.; Hasselblom, S.; Nilsson-Ehle, H.; Goran Karlsson, B.; Pinto, R.; Andersson, P.O. Serum nuclear magnetic resonance-based metabolomics and outcome in diffuse large B-cell lymphoma patients—A pilot study. Leukemia Lymphoma 2016, 57, 1814–1822. [Google Scholar] [CrossRef] [PubMed]
- Schwarzfischer, P.; Reinders, J.; Dettmer, K.; Kleo, K.; Dimitrova, L.; Hummel, M.; Kube, D.; Szczepanowski, M.; Klapper, W.; Taruttis, F.; et al. Comprehensive Metaboproteomics of Burkitt’s and Diffuse Large B-Cell Lymphoma cell lines and primary tumor tissues reveals distinct differences in pyruvate content and metabolism. J. Proteome Res. 2017, 16, 1105–1120. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, H.; Kubota, M.; Shimizu, T.; Kasai, Y.; Sano, H.; Adachi, S.; Akiyama, Y.; Mikawa, H. Effect of high-dose methotrexate on plasma hypoxanthine and uridine levels in patients with acute leukemia or non-Hodgkin lymphoma in childhood. Leukemia 1992, 6, 1199–1202. [Google Scholar] [PubMed]
- Kim, K.; Yeo, S.G.; Yoo, B.C. Identification of hypoxanthine and phosphoenolpyruvic acid as serum markers of chemoradiotherapy response in locally advanced rectal cancer. Cancer Res. Treat. 2015, 47, 78–89. [Google Scholar] [CrossRef]
- Stillwell, W. Trans fatty acids. In An Introduction to Biological Membranes. Composition, Structure and Function, 2nd ed.; Elsevier Science: Amsterdam, NL, USA, 2016; p. 532. [Google Scholar]
- Li, H.; Zhang, Q.; Song, J.; Wang, A.; Zou, Y.; Ding, L.; Wen, Y. Plasma trans-fatty acids levels and mortality: A cohort study based on 1999-2000 National Health and Nutrition Examination Survey (NHANES). Lipids Health Dis. 2017, 16, 176. [Google Scholar] [CrossRef] [PubMed]
- Charbonneau, B.; O’Connor, H.M.; Wang, A.H.; Liebow, M.; Thompson, C.A.; Fredericksen, Z.S.; Macon, W.R.; Slager, S.L.; Call, T.G.; Habermann, T.M.; et al. Trans Fatty Acid Intake Is Associated with Increased Risk and n3 Fatty Acid Intake with Reduced Risk of Non-Hodgkin Lymphoma. J. Nutr. 2013, 143, 672–681. [Google Scholar] [CrossRef]
- Buckley, D.; Duke, G.; Heuer, T.S.; O’Farrell, M.; Wagman, A.S.; McCulloch, W.; Kemble, G. Fatty acid synthase-Modern tumor cell biology insights into a classical oncology target. Pharmacol. Therapeut. 2017, 177, 23–31. [Google Scholar] [CrossRef]
- Röhrig, F.; Schulze, A. The multifaceted roles of fatty acid synthesis in cancer. Nat. Rev. Cancer 2016, 16, 732–749. [Google Scholar] [CrossRef]
- Wang, W.; Zhao, X.; Wang, H.; Liang, Y. Increased fatty acid synthase as a potential therapeutic target in multiple myeloma. J. Zhejiang Univ. Sci. B 2008, 9, 441–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tili, E.; Michaille, J.J.; Luo, Z.; Volinia, S.; Rassenti, L.Z.; Kipps, T.J.; Croce, C.M. The downregulation of miR-125b in chronic lymphocytic leukemias leads to metabolic adaptation of cells to a transformed state. Blood 2012. [Google Scholar] [CrossRef] [PubMed]
- Rozovski, U.; Hazan-Halevy, I.; Barzilay, M.; Keating, M.J.; Estrov, Z. Metabolism pathways in chronic lymphocytic leukemia. Leuk Lymphoma 2016, 57, 758–765. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Lan, Q.; Zhang, Y.; Bassig, B.A.; Holford, T.R.; Leaderer, B.; Boyle, P.; Zhu, Y.; Qin, Q.; Chanock, S.; et al. Role of one-carbon metabolizing pathway genes and gene-nutrient interaction in the risk of non-Hodgkin lymphoma. Cancer Causes Control 2013, 24, 1875–1884. [Google Scholar] [CrossRef] [PubMed]
- Cocco, P.; Zucca, M.; Sanna, S.; Satta, G.; Angelucci, E.; Gabbas, A.; Monne, M.; Campagna, M.; Scarpa, A.; Ennas, M.G. Interaction between dietary and lifestyle risk factors and N-acetyl transferase polymorphisms in B-cell lymphoma etiology. J. Environ. Anal. Toxicol. 2015, 5, 5. [Google Scholar] [CrossRef]
- Jung, K.; Reszka, R.; Kamlage, B.; Bethan, B.; Stephan, C.; Lein, M.; Kristiansenm, G. Tissue metabolite profiling identifies differentiating and prognostic biomarkers for prostate carcinoma. Int. J. Cancer 2013, 133, 2914–2924. [Google Scholar] [CrossRef]
- Rosi, A.; Ricci-Vitiani, L.; Biffoni, M.; Grande, S.; Luciani, A.M.; Palma, A.; Runci, D.; Cappellari, M.; De Maria, R.; Guidoni, L.; et al. 1H NMR spectroscopy of glioblastoma stemlikecells identifies alpha-aminoadipate as a marker of tumor aggressiveness. NMR Biomed. 2015, 28, 317–326. [Google Scholar] [CrossRef]
- Nakamizo, S.; Sasayama, T.; Shinohara, M.; Irino, Y.; Nishiumi, S.; Nishihara, M. GC/MS-based metabolomic analysis of cerebrospinal fluid (CSF) from glioma patients. J. Neurooncol. 2013, 113, 65–74. [Google Scholar] [CrossRef] [Green Version]
- Goedert, J.J.; Sampson, J.N.; Moore, S.C.; Xiao, Q.; Xiong, X.; Hayes, R.B.; Ahn, J.; Shi, J.; Sinha, R. Fecal metabolomics: Assay performance and association with colorectal cancer. Carcinogenesis 2014, 35, 2089–2096. [Google Scholar] [CrossRef]
- Brown, D.G.; Rao, S.; Weir, T.L.; O’Malia, J.; Bazan, M.; Brown, R.J.; Ryan, E.P. Metabolomics and metabolic pathway networks from human colorectal cancers, adjacent mucosa, and stool. Cancer Metab. 2016, 4, 11. [Google Scholar] [CrossRef]
- Moon, H.J.; Jeya, M.; Kim, I.W.; Lee, J.K. Biotechnological production of erythritol and its applications. Appl. Microbiol. Biotechnol. 2010, 86, 1017–1025. [Google Scholar] [CrossRef] [PubMed]
- Hootman, K.C.; Trezzi, J.P.; Kraemer, L.; Burwell, L.S.; Dong, X.; Guertin, K.A.; Jaeger, C.; Stover, P.J.; Hiller, K.; Cassano, P.A. Erythritol is a pentose-phosphate pathway metabolite and associated with adiposity gain in young adults. Proc. Natl. Acad. Sci. USA 2017, 114, E4233–E4240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeng, J.; Yin, P.; Tan, Y.; Dong, L.; Hu, C.; Huang, Q.; Lu, X.; Wang, H.; Xu, G. Metabolomics Study of Hepatocellular Carcinoma: Discovery and Validation of Serum Potential Biomarkers by Using Capillary Electrophoresis−Mass Spectrometry. J. Proteome Res. 2014, 13, 3420–3431. [Google Scholar] [CrossRef] [PubMed]
- Gall, W.E.; Beebe, K.; Lawton, K.A.; Adam, K.P.; Mitchell, M.W.; Nakhle, P.J.; Ryals, A.J.; Milburn, M.V.; Nannipieri, M.; Camastra, S. α-Hydroxybutyrate is an early biomarker of insulin resistance and glucose intolerance in a nondiabetic population. PLoS ONE 2010, 5, e10883. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xu, Z.; Lu, X.; Yang, X.; Yin, P.; Kong, H.; Yu, Y.; Xu, G. Comprehensive two-dimensional gas chromatography/time-of-flight mass spectrometry for metabonomics: Biomarker discovery for diabetes mellitus. Anal. Chim. Acta 2009, 633, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Dunn, W.B.; Broadhurst, D.; Begley, P.; Zelena, E.; Francis-McIntyre, S.; Anderson, N.; Brown, M.; Knowles, J.D.; Halsall, A.; Haselden, J.N.; et al. Procedures for large-scale metabolic profiling of serum and plasma using gas chromatography and liquid chromatography coupled to mass spectrometry. Nat. Prot. 2011, 6, 1060–1083. [Google Scholar] [CrossRef] [PubMed]
- Chong, J.; Soufan, O.; Li, C.; Caraus, I.; Li, S.; Bourque, G.; Wishart, D.S.; Xia, J. MetaboAnalyst 4.0: Towards more transparent and integrative metabolomics analysis. Nucl. Acids Res. 2018, 46, W486–W494. [Google Scholar] [CrossRef]
- Eriksson, L.; Johansson, E.; Kettaneh-Wold, N.; Wold, S. Multi- and Megavariate Data Analysis; Umetrics AB: Umea, Sweden, 2001. [Google Scholar]
Sample Availability: Samples are not available from the authors. |

| N | Gender | Age | ||||
|---|---|---|---|---|---|---|
| M | F | M/F | Mean | sd | ||
| Controls | 96 | 50 | 46 | 1.09 | 57.0 | 12.87 |
| Diffuse Large B-cell Lymphoma | 13 | 6 | 7 | 0.86 | 62.2 | 10.46 |
| Follicular Lymphoma | 8 | 5 | 3 | 1.67 | 47.9 | 8.36 |
| Chronic Lymphocytic Leukaemia | 6 | 2 | 4 | 0.50 | 62.0 | 15.23 |
| Multiple Myeloma | 9 | 5 | 4 | 1.25 | 61.7 | 7.00 |
| Other B-cell Lymphoma | 14 | 10 | 4 | 2.50 | 59.7 | 7.92 |
| B-cell Lymphoma (total) | 50 | 28 | 22 | 1.27 | 59.1 | 10.52 |
| Hodgkin Lymphoma | 10 | 4 | 6 | 0.67 | 38.2 | 12.22 |
| T-cell Lymphoma | 2 | 2 | 0 | - | 59.5 | - |
| Unspecified Lymphoma subtype | 4 | 2 | 2 | 1.0 | 63.8 | 15.17 |
| All lymphomas | 66 | 36 | 30 | 1.20 | 57.3 | 13.22 |
| Metabolite | Diffuse Large B-Cell Lymphoma (DLBCL) | Follicular Lymphoma (FL) | Chronic Lymphocytic Leukemia (CLL) | Multiple Myeloma (MM) | Hodgkin Lymphoma (HL) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p-Value | FDR | Trend | p-Value | FDR | Trend | p-Value | FDR | Trend | p-Value | FDR | Trend | p-Value | FDR | Trend | |
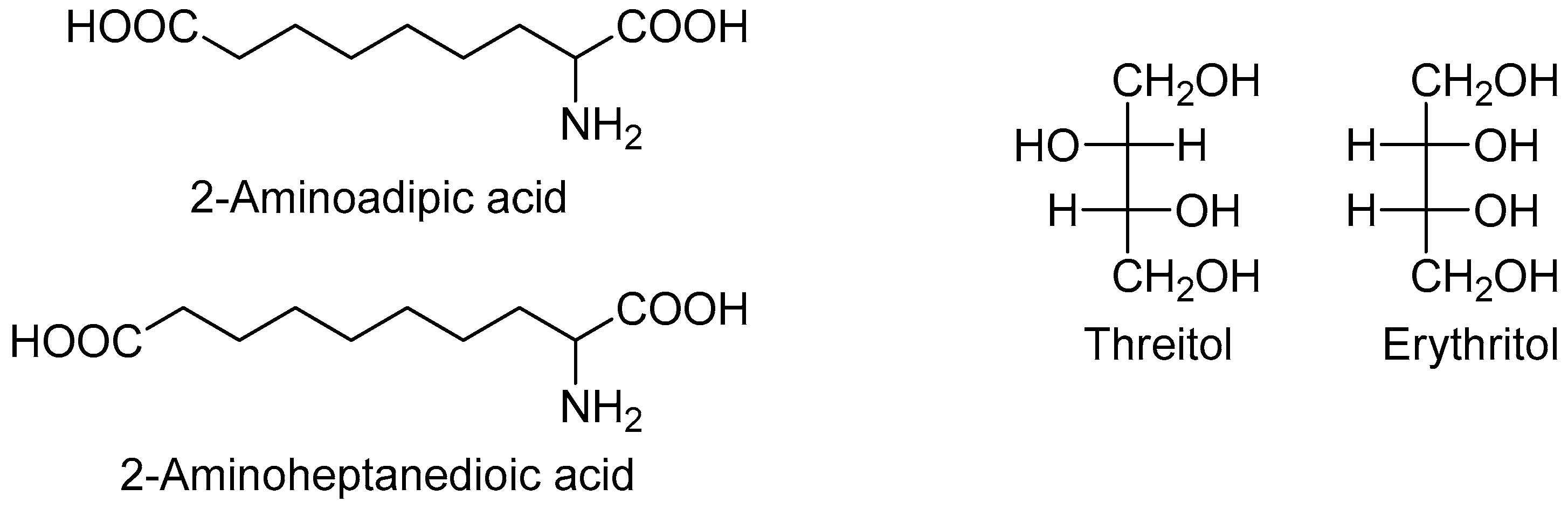
| 2-Aminoadipic acid | 0.0021 | 0.0279 | ↓ | 0.00048 | 0.0079 | ↓ | |||||||||
| 2-Aminoheptanedioic acid | 4.3 × 10−6 | 0.0004 | ↓ | ||||||||||||
| 3-Hydroxybutyric acid | 0.0017 | 0.0279 | ↑ | ||||||||||||
| 3-Phosphoglycerate | 0.00124 | 0.0401 | ↑ | ||||||||||||
| A148003 | 9.95 × 10−5 | 0.0042 | ↓ | ||||||||||||
| A203003 | 0.00024 | 0.0065 | ↑ | ||||||||||||
| Aspartic acid | 3.41 × 10−4 | 0.0096 | ↓ | ||||||||||||
| Carbonic acid | 0.00692 | 0.0405 | ↑ | ||||||||||||
| Erythritol | 0.0026 | 0.0279 | ↑ | 0.00503 | 0.0327 | ↑ | |||||||||
| Ethanolamine | 8.02 × 10−4 | 0.0233 | ↓ | ||||||||||||
| Fucose | 0.0045 | 0.0421 | ↑ | ||||||||||||
| Glucoheptonic acid 1,4-lactone | 0.0004 | 0.0079 | ↓ | ||||||||||||
| Glucose | 1.97 × 10−4 | 0.0088 | ↓ | 0.00374 | 0.0481 | ↓ | |||||||||
| Glutamic acid | 0.00363 | 0.0271 | ↑ | ||||||||||||
| Glycine | 0.0011 | 0.0231 | ↑ | ||||||||||||
| Hippuric acid | 7.28 × 10−5 | 0.0032 | ↓ | ||||||||||||
| Hypoxanthine | 1.03 × 10−5 | 0.0004 | ↑ | 0.00134 | 0.0401 | ↑ | |||||||||
| Iminodiacetic acid | 0.00338 | 0.0271 | ↓ | ||||||||||||
| Inositol | 0.00811 | 0.0443 | ↑ | ||||||||||||
| Lactic acid | 3.26 × 10−5 | 0.0029 | ↑ | 0.00257 | 0.0481 | ↑ | |||||||||
| Linoleic acid | 0.00372 | 0.0481 | ↑ | ||||||||||||
| Mannose | 0.0027 | 0.0279 | ↑ | 0.00104 | 0.0122 | ↑ | |||||||||
| Ornithine | 0.0093 | 0.0476 | ↑ | ||||||||||||
| Palmitic acid | 0.00286 | 0.0481 | ↑ | ||||||||||||
| Phosphate | 8.7 × 10−4 | 0.0401 | ↑ | ||||||||||||
| Proline+CO2 | 0.006 | 0.0455 | ↓ | ||||||||||||
| Quinic acid | 2.91 × 10−5 | 0.0025 | ↓ | ||||||||||||
| Tryptophan | 0.00074 | 0.0102 | ↑ | ||||||||||||
| Unknown 1314 | 8.30 × 10−6 | 0.0004 | ↓ | ||||||||||||
| Unknown 1342 | 0.00519 | 0.0327 | ↑ | ||||||||||||
| Unknown 2028 | 0.00344 | 0.0271 | ↓ | ||||||||||||
| Uric acid | 0.01032 | 0.0498 | ↑ | ||||||||||||
| Comparison | Number of Components | Accuracy | R2 | Q2 |
|---|---|---|---|---|
| DLBCL/C | 2 | 0.945 | 0.845 | 0.600 |
| FL/C | 5 | 0.857 | 0.973 | 0.131 |
| CLL/C | 2 | 1.00 | 0.911 | 0.734 |
| MM/C | 4 | 0.933 | 0.949 | 0.613 |
| HL/C | 4 | 0.935 | 0.950 | 0.679 |
| Metabolite | Class e | HMDB ID | CAS | DLBCL | CLL | MM | HL |
|---|---|---|---|---|---|---|---|
| 2-Aminoadipic acid a | AA | HMDB0000510 | 7620-28-2 | ↓ | ↓ | ||
| 2-Aminoheptanedioic acid a | AA | HMDB0034252 | 3721-85-5 | ↓ | ↓ | ↓ | |
| 2-Hydroxybutyric acid c | HA | HMDB0000008 | 600-15-7 | ↑ | ↑ | ||
| 3-Aminoisobutyric acid c | AA | HMDB0003911 | 144-90-1 | ↓ | ↑ | ||
| 3-Hydroxybutyric acid c | HA | HMDB0000357 | 300-85-6 | ↑ | |||
| 3-Phosphoglyceric acid b | HA | HMDB0000807 | 820-11-1 | ↑ | |||
| 4-Hydroxyproline c | AA | HMDB0000725 | 51-35-4 | ↑ | ↑ | ||
| A148003 b | - | - | - | ↓ | ↓ | ||
| A203003 b | - | - | - | ↑ | |||
| Aspartic acid c | AA | HMDB0000191 | 56-84-8 | ↓ | |||
| Cis-Aconitic acid c | A | HMDB0000072 | 585-84-2 | ↓ | ↓ | ||
| Cysteine c | AA | HMDB0000574 | 52-90-4 | ↓ | ↑ | ||
| Elaidic acid c | FA | HMDB0000573 | 112-79-8 | ↑ | ↑ | ↑ | ↑ |
| Erythritol c | PO | HMDB0002994 | 149-32-6 | ↑ | ↑ | ||
| Erythronic acid b | HA | HMDB0000613 | 13752-84-6 | ↑ | |||
| Ethanolamine c | Am | HMDB0000149 | 141-43-5 | ↓ | |||
| Fructose c | S | HMDB0000660 | 53188-23-1 | ↓ | |||
| Fucose c | S | HMDB0000174 | 2438-80-4 | ↑ | |||
| Glucoheptonic acid b | HA | - | 87-74-1 | ↓ | ↓ | ||
| Gluconic acid c | HA | HMDB0000625 | 526-95-4 | ↑ | ↑ | ↓ | |
| Glutamic acid c | AA | HMDB0000148 | 56-86-0 | ↑ | ↑ | ↑ | |
| Glycerol-3-Phosphate c | PO | HMDB0000126 | 57-03-4 | ↑ | ↑ | ||
| Glycine c | AA | HMDB0000123 | 56-40-6 | ↑ | ↑ | ||
| Glycolic acid c | HA | HMDB0000115 | 79-14-1 | ↑ | ↑ | ||
| Hippuric acid c | A | HMDB0000714 | 495-69-2 | ↑ | ↓ | ↓ | |
| Hypoxanthine c | P | HMDB0000157 | 68-94-0 | ↑ | ↑ | ↑ | ↑ |
| Iminodiacetic acid c | A | HMDB0011753 | 142-73-4 | ↓ | |||
| Inositol-like d | PO | - | - | ↑ | ↑ | ||
| Inositol phosphate a | PO | HMDB0002985 | 15421-51-9 | ↑ | |||
| Lactic acid c | HA | HMDB0000190 | 79-33-4 | ↑ | |||
| Linoleic acid c | FA | HMDB0000673 | 60-33-3 | ↑ | |||
| Mannitol c | PO | HMDB0000765 | 69-65-8 | ↑ | ↑ | ||
| Monosaccharide 1886 | S | - | - | ↓ | ↑ | ||
| Myristic acid c | FA | HMDB0000806 | 544-63-8 | ↑ | ↑ | ||
| Oleic acid c | FA | HMDB0000207 | 112-80-1 | ↑ | ↑ | ↑ | |
| Ornithine c | AA | HMDB0000214 | 3184-13-2 | ↑ | |||
| Palmitic acid c | FA | HMDB0000220 | 57-10-3 | ↑ | |||
| Palmitoleic acid c | FA | HMDB0003229 | 373-49-9 | ↑ | ↑ | ↑ | |
| Phosphate c | I | HMDB0001429 | 14265-44-2 | ↓ | ↑ | ||
| Proline+CO2 b | AA | - | - | ↓ | |||
| Pyroglutamic acid c | AA | HMDB0000267 | 98-79-3 | ↑ | |||
| Pyrophosphate a | I | HMDB0000250 | 14000-31-8 | ↓ | |||
| Quinic acid b | HA | HMDB0003072 | 77-95-2 | ↓ | ↓ | ||
| Serine c | AA | HMDB0000187 | 56-45-1 | ↑ | |||
| Serotonin a | Am | HMDB0000259 | 50-67-9 | ↓ | |||
| Stearic acid c | FA | HMDB0000827 | 57-11-4 | ↑ | ↑ | ||
| Succinic acid c | A | HMDB0000254 | 110-15-6 | ↑ | ↑ | ||
| Sucrose c | S | HMDB0000258 | 57-50-1 | ↓ | |||
| Threitol c | PO | HMDB0004136 | 2418-52-2 | ↑ | ↑ | ↓ | |
| Tryptophan c | AA | HMDB0000929 | 73-22-3 | ↓ | ↑ | ||
| Unknown 1314 | - | - | - | ↓ | |||
| Unknown 1910 | - | - | - | ↑ | ↑ | ↑ | |
| Unknown 2028 | - | - | - | ↓ | ↓ | ||
| Uric acid c | P | HMDB0000289 | 69-93-2 | ↓ | ↑ | ↑ | ↓ |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barberini, L.; Noto, A.; Fattuoni, C.; Satta, G.; Zucca, M.; Cabras, M.G.; Mura, E.; Cocco, P. The Metabolomic Profile of Lymphoma Subtypes: A Pilot Study. Molecules 2019, 24, 2367. https://doi.org/10.3390/molecules24132367
Barberini L, Noto A, Fattuoni C, Satta G, Zucca M, Cabras MG, Mura E, Cocco P. The Metabolomic Profile of Lymphoma Subtypes: A Pilot Study. Molecules. 2019; 24(13):2367. https://doi.org/10.3390/molecules24132367
Chicago/Turabian StyleBarberini, Luigi, Antonio Noto, Claudia Fattuoni, Giannina Satta, Mariagrazia Zucca, Maria Giuseppina Cabras, Ester Mura, and Pierluigi Cocco. 2019. "The Metabolomic Profile of Lymphoma Subtypes: A Pilot Study" Molecules 24, no. 13: 2367. https://doi.org/10.3390/molecules24132367





