Salts of Therapeutic Agents: Chemical, Physicochemical, and Biological Considerations
Abstract
:1. Introduction
2. Drug Chemistry Considerations
2.1. API Functional Groups
2.2. pKa of the Drug
2.3. Lipophilicity
2.4. Hygroscopicity
2.5. Water of Hydration
2.6. Polymorphism
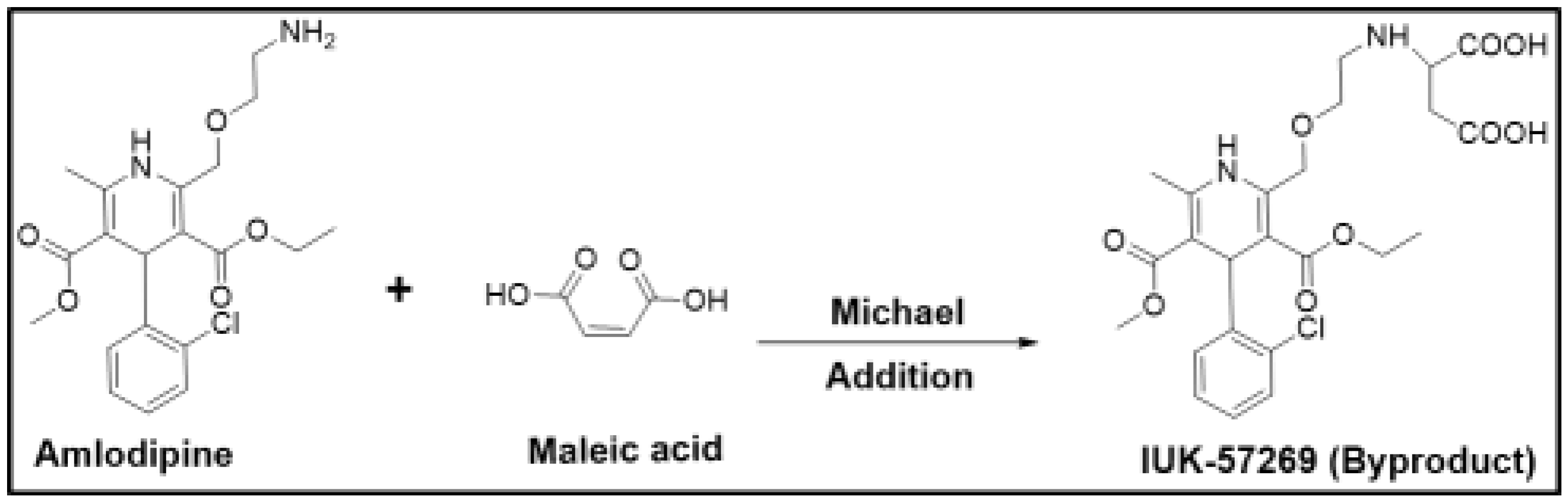
2.7. Chemical Stability
2.8. Solubility and Dissolution Rate
3. Pharmaceutical Considerations
3.1. Dosage Form Desired
3.1.1. A Liquids (Suspensions)
3.1.2. B Solutions
3.1.3. Creams/Ointments/Gels
3.1.4. Aerosols
3.2. Ease of Synthesis and Scale-Up
3.2.1. Flowability
3.2.2. Corrosiveness of Counterions
3.2.3. Compatibility with Excipients
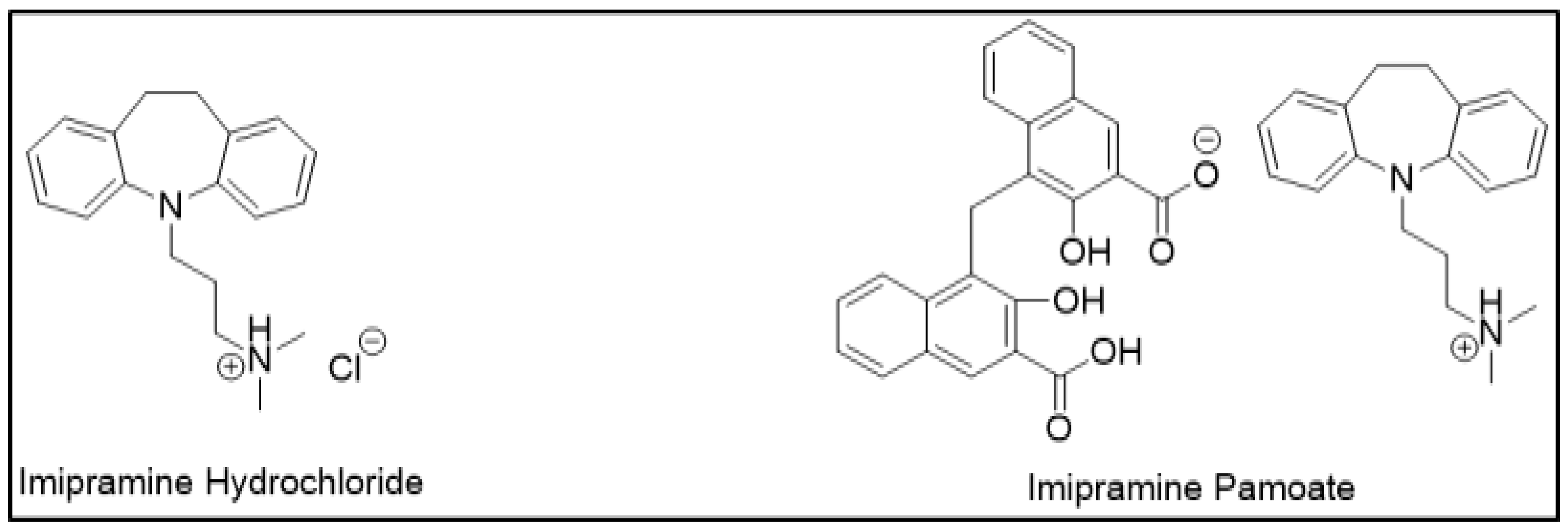
3.3. Route of Administration
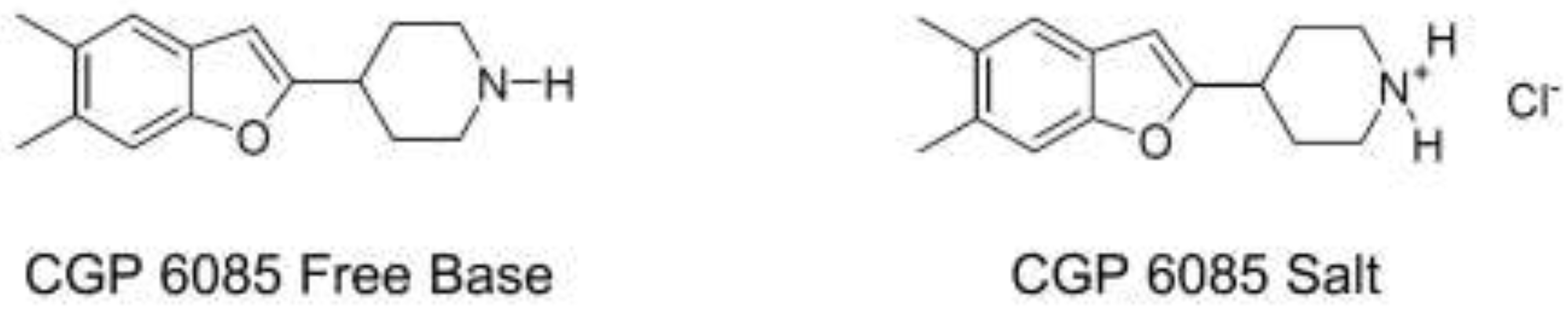
3.4. Controlled Release Dosage Forms
4. Pharmacokinetics (PK), Pharmacodynamics (PD), and Safety Considerations
4.1. Toxicological Consideration
4.2. Distribution and Clearance
4.3. Onset and Termination of Therapeutic Effects
4.4. Counteracting Side Effects
4.5. Drug Interactions
5. Economic Considerations
Intellectual Property (IP) Considerations
6. Screening, Preparation, and Characterization of Salts
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| API | Active Pharmaceutical Ingredient |
| FDA | Food and Drug Administration |
| GRAS | Generally Regarded as Safe |
| IR | Immediate Release |
| PPI | Proton Pump Inhibitors |
References
- Paulekuhn, G.S.; Dressman, J.B.; Saal, C. Trends in active pharmaceutical ingredient salt selection based on analysis of the orange book database. J. Med. Chem. 2007, 50, 6665–6672. [Google Scholar] [CrossRef] [PubMed]
- Prohotsky, D.L.; Zhao, F. A survey of top 200 drugs—Inconsistent practice of drug strength expression for drugs containing salt forms. J. Pharm. Sci. 2012, 101, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Rubino, J.T. Solubilities and solid state properties of the sodium salts of drugs. J. Pharm. Sci. 1989, 78, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.; Rubino, J. Solubility, melting point and salting-out relationships in a group of secondary amine hydrochloride salts. Int. J. Pharm. 1996, 130, 179–185. [Google Scholar] [CrossRef]
- Chowhan, Z.T. Ph-solubility profiles or organic carboxylic acids and their salts. J. Pharm. Sci. 1978, 67, 1257–1260. [Google Scholar] [CrossRef] [PubMed]
- Forbes, R.T.; York, P.; Davidson, J.R. Dissolution kinetics and solubilities of p-aminosalicylic acid and its salts. Int. J. Pharm. 1995, 126, 199–208. [Google Scholar] [CrossRef]
- Gould, P.L. Salt selection for basic drugs. Int. J. Pharm. 1986, 33, 201–217. [Google Scholar] [CrossRef]
- Pandit, N.K.; Strykowski, J.M.; Shtohryn, L. The effect of salts on the distribution and solubility of an acidic drug. Int. J. Pharm. 1989, 50, 7–13. [Google Scholar] [CrossRef]
- Wiedmann, T.S.; Naqwi, A. Pharmaceutical salts: Theory, use in solid dosage forms and in situ preparation in an aerosol. Asian J. Pharm. Sci. 2016, 11, 722–734. [Google Scholar] [CrossRef] [Green Version]
- Gross, T.D.; Schaab, K.; Ouellette, M.; Zook, S.; Reddy, J.P.; Shurtleff, A.; Sacaan, A.I.; Alebic-Kolbah, T.; Bozigian, H. An approach to early-phase salt selection: Application to NBI-75043. Org. Process Res. Dev. 2007, 11, 365–377. [Google Scholar] [CrossRef]
- Cruz-Cabeza, A.J. Acid-base crystalline complexes and the pka rule. CrystEngComm 2012, 14, 6362–6365. [Google Scholar] [CrossRef]
- Stahl, P.H.; Skinner, F.S. Pharmaceutical aspects of the api salt form. In Pharmaceutical Salts: Properties, Selection, and Use, 2nd ed.; Stahl, P.H., Wermuth, C.G., Eds.; WILEY-VCH: Weinheim, Germany, 2011; pp. 85–124. [Google Scholar]
- Serajuddin, A.T.; Jarowski, C.I. Influence of ph on release of phenytoin sodium from slow-release dosage forms. J. Pharm. Sci. 1993, 82, 306–310. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Dahan, A.; Gupta, D.; Varghese, S.; Amidon, G.L. Quasi-equilibrium analysis of the ion-pair mediated membrane transport of low-permeability drugs. J. Control. Release 2009, 137, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Dahan, A.; Gupta, D.; Varghese, S.; Amidon, G.L. Enabling the intestinal absorption of highly polar antiviral agents: Ion-pair facilitated membrane permeation of zanamivir heptyl ester and guanidino oseltamivir. Mol. Pharm. 2010, 7, 1223–1234. [Google Scholar] [CrossRef] [PubMed]
- Walkling, W.D.; Reynolds, B.E.; Fegely, B.J.; Janicki, C.A. Xilobam: Effect of salt form on pharmaceutical properties. Drug Dev. Ind. Pharm. 1983, 9, 809–819. [Google Scholar] [CrossRef]
- Sarveiya, V.; Templeton, J.F.; Benson, H.A. Ion-pairs of ibuprofen: Increased membrane diffusion. J. Pharm. Pharmacol. 2004, 56, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Visalakshi, N.A.; Mariappan, T.T.; Bhutani, H.; Singh, S. Behavior of moisture gain and equilibrium moisture contents (EMC) of various drug substances and correlation with compendial information on hygroscopicity and loss on drying. Pharm. Dev. Technol. 2005, 10, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Carstensen, J.T. Effect of moisture on the stability of solid dosage forms. Drug Dev. Ind. Pharm. 1988, 14, 1927–1969. [Google Scholar] [CrossRef]
- Suzuki, T.; Araki, T.; Kitaoka, H.; Terada, K. Characterization of non-stoichiometric hydration and the dehydration behavior of sitafloxacin hydrate. Chem. Pharm. Bull. 2012, 60, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chow, P.S.; Tan, R.B.H.; Black, S.N. Effect of water activity on the transformation between hydrate and anhydrate of carbamazepine. Org. Process Res. Dev. 2008, 12, 264–270. [Google Scholar] [CrossRef]
- Etter, M.C.; Urbanczyk-Lipkowska, Z.; Zia-Ebrahimi, M.; Panunto, T.W. Hydrogen bond-directed cocrystallization and molecular recognition properties of diarylureas. J. Am. Chem. Soc. 1990, 112, 8415–8426. [Google Scholar] [CrossRef]
- Khankari, R.K.; Grant, D.J.W. Pharmaceutical hydrates. Thermochim. Acta 1995, 248, 61–79. [Google Scholar] [CrossRef]
- Singhal, D.; Curatolo, W. Drug polymorphism and dosage form design: A practical perspective. Adv. Drug Deliv. Rev. 2004, 56, 335–347. [Google Scholar] [CrossRef] [PubMed]
- Macek, T.J. The physical and chemical problems inherent in the formulation of dosage forms for new pharmaceuticals I. Am. J. Pharm. Sci. Support. Public Health 1965, 137, 217–238. [Google Scholar] [PubMed]
- Bučar, D.-K.; Lancaster, R.W.; Bernstein, J. Disappearing polymorphs revisited. Angew. Chem. (Int.Ed.Eng.) 2015, 54, 6972–6993. [Google Scholar] [CrossRef] [PubMed]
- Bauer, J.; Spanton, S.; Henry, R.; Quick, J.; Dziki, W.; Porter, W.; Morris, J. Ritonavir: An extraordinary example of conformational polymorphism. Pharm. Res. 2001, 18, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Chemburkar, S.R.; Bauer, J.; Deming, K.; Spiwek, H.; Patel, K.; Morris, J.; Henry, R.; Spanton, S.; Dziki, W.; Porter, W.; et al. Dealing with the impact of ritonavir polymorphs on the late stages of bulk drug process development. Org. Process Res. Dev. 2000, 4, 413–417. [Google Scholar] [CrossRef]
- Narang, A.S.; Desai, D.; Badawy, S. Impact of excipient interactions on solid dosage form stability. Pharm. Res. 2012, 29, 2660–2683. [Google Scholar] [CrossRef] [PubMed]
- Chakole, D.D. Stabilized Pharmaceutical Formulations Containing Amlodipine Maleate. U.S. Patent WO2003032954 A1, 24 April 2003. [Google Scholar]
- Elder, D.P.; Delaney, E.; Teasdale, A.; Eyley, S.; Reif, V.D.; Jacq, K.; Facchine, K.L.; Oestrich, R.S.; Sandra, P.; David, F. The utility of sulfonate salts in drug development. J. Pharm. Sci. 2010, 99, 2948–2961. [Google Scholar] [CrossRef] [PubMed]
- Bastin, R.J.; Bowker, M.J.; Slater, B.J. Salt selection and optimisation procedures for pharmaceutical new chemical entities. Org. Process Res. Dev. 2000, 4, 427–435. [Google Scholar] [CrossRef]
- Carmichael, R.R.; Mahoney, C.D.; Jeffrey, L.P. Solubility and stability of phenytoin sodium when mixed with intravenous solutions. Am. J. Hosp. Pharm. 1980, 37, 95–98. [Google Scholar] [PubMed]
- Marwah, H.; Garg, T.; Goyal, A.K.; Rath, G. Permeation enhancer strategies in transdermal drug delivery. Drug Deliv. 2016, 23, 564–578. [Google Scholar] [CrossRef] [PubMed]
- Fini, A.; Fazio, G.; Gonzalez-Rodriguez, M.; Cavallari, C.; Passerini, N.; Rodriguez, L. Formation of ion-pairs in aqueous solutions of diclofenac salts. Int. J. Pharm. 1999, 187, 163–173. [Google Scholar] [CrossRef]
- David, T.M.; Ivan, M. Integration of active pharmaceutical ingredient solid form selection and particle engineering into drug product design. J. Pharm. Pharmacol. 2015, 67, 782–802. [Google Scholar] [Green Version]
- Ahmed, H.; Shimpi, M.R.; Velaga, S.P. Relationship between mechanical properties and crystal structure in cocrystals and salt of paracetamol. Drug Dev. Ind. Pharm. 2017, 43, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, G.A.; Aburub, A.; Woods, T.A. Physical stability of salts of weak bases in the solid-state. J. Pharm. Sci. 2011, 100, 1607–1617. [Google Scholar] [CrossRef] [PubMed]
- Makary, P. Principles of salt formation. UK J. Pharm. Biosci. 2014, 2, 1–4. [Google Scholar] [CrossRef]
- Jamerson, B.D.; Dukes, G.E.; Brouwer, K.L.R.; Dorm, K.H.; Messenheimer, J.A.; Powell, R.J. Venous irritation related to intravenous administration of phenytoin versus fosphenytoin. Pharmacotherapy 1994, 14, 47–52. [Google Scholar] [CrossRef] [PubMed]
- McPherson, M.L.; Cimino, N.M. Topical NSAID formulations. Pain Med. 2013, 14, S35–S39. [Google Scholar] [CrossRef] [PubMed]
- Fini, A.; Fazio, G.; Hervás, M.-J.F.; Holgado, M.A.; Rabasco, A.M. Factors governing the dissolution of diclofenac salts. Eur. J. Pharm. Sci. 1996, 4, 231–238. [Google Scholar] [CrossRef]
- Broh-Kahn, R.H. Choline salicylate: A new, effective, and well-tolerated analgesic, anti-inflammatory, and antipyretic agent. Int. Rec. Med. 1960, 173, 217–233. [Google Scholar] [PubMed]
- Duesel, B.F.; Berman, H.; Schachter, R.J. Substituted xanthines. I. Preparation and properties of some choline theophyllinates. J. Am. Pharm. Assoc. 1954, 43, 619–622. [Google Scholar] [CrossRef]
- Malek, P.; Kolc, J.; Herold, M.; Hoffman, J. Lymphotrophic antibiotics; antibiolymphins. Antibiot. Annu. 1957, 5, 546–551. [Google Scholar] [PubMed]
- Berge, S.M.; Bighley, L.D.; Monkhouse, D.C. Pharmaceutical salts. J. Pharm. Sci. 1977, 66, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Voelker, R. Extended-release ADHD drug. JAMA 2017, 318, 416. [Google Scholar] [CrossRef] [PubMed]
- Boger, W.P.; Strickland, S.C.; Gylfe, J.M. The penicillinate of benzhydrylamine; its oral administration. Antibiot. Med. Clin. Ther. 1955, 1, 372–376. [Google Scholar]
- Engel, J.; Kleemann, A.; Kutscher, B.; Reichert, D. Pharmaceutical Substances, 5th Edition, 2009: Syntheses, Patents and Applications of the Most Relevant APIs; Thieme: Stuttgart, Germany, 2014. [Google Scholar]
- Cusic, J.W. 8-Haloxanthine Salts of Dialkylaminoalkyl Type Antihistamine Bases. U.S. Patent 2534235A, 19 December 1950. [Google Scholar]
- Cusic, J.W. 8-Haloxanthine Salts of Diarylalkyl Dialkylaminoalkyl Ethers. U.S. Patent 2499058A, 28 February 1950. [Google Scholar]
- Seiler, D.; Doser, K.; Salem, I. Relative bioavailability of prasugrel free base in comparison to prasugrel hydrochloride in the presence and in the absence of a proton pump inhibitor. Arzneimittelforschung 2011, 61, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Song, C.H.; Han, J.-W. Patent cliff and strategic switch: Exploring strategic design possibilities in the pharmaceutical industry. SpringerPlus 2016, 5, 692. [Google Scholar] [CrossRef] [PubMed]
- Akazawa, M. Diclofenac, Hydroxyethyl-Pyrroldine or Piperidine. U.S. Patent 5607690A, 1 March 1997. [Google Scholar]
- Black, S.N.; Collier, E.A.; Davey, R.J.; Roberts, R.J. Structure, solubility, screening, and synthesis of molecular salts. J. Pharm. Sci. 2007, 96, 1053–1068. [Google Scholar] [CrossRef] [PubMed]
- Thorson, M.R.; Goyal, S.; Schudel, B.R.; Zukoski, C.F.; Zhang, G.G.Z.; Gong, Y.; Kenis, P.J.A. A microfluidic platform for pharmaceutical salt screening. Lab Chip 2011, 11, 3829–3837. [Google Scholar] [CrossRef] [PubMed]
- Nievergelt, P.P.; Babor, M.; Cejka, J.; Spingler, B. A high throughput screening method for the nano-crystallization of salts of organic cations. Chem. Sci. 2018, 9, 3716–3722. [Google Scholar] [CrossRef] [PubMed]

| Chemistry (Type of Ion) | Examples of Counterions | |
|---|---|---|
| Cations | Aluminum Arginine Benzathine Calcium Chloroprocaine Choline Diethanolamine Ethanolamine Ethylenediamine | Lysine Magnesium Histidine Lithium Meglumine Potassium Procaine Sodium Triethylamine Zinc |
| Anions | Acetate Aspartate Benzenesulfonate Benzoate Besylate Bicarbonate Bitartrate Bromide Camsylate Carbonate Chloride Citrate Decanoate Edetate Esylate Fumarate Gluceptate Gluconate Glutamate Glycolate Hexanoate Hydroxynaphthoate Iodide Isethionate Lactate | Lactobionate Malate Maleate Mandelate Mesylate Methylsulfate Mucate Napsylate Nitrate Octanoate Oleate Pamoate Pantothenate Phosphate Polygalacturonate Propionate Salicylate Stearate Acetate Succinate Sulfate Tartrate Teoclate Tosylate |
| Ibuprofen Counterion | Log P | Intestinal Flux (µg·cm−1·h−1) |
|---|---|---|
| Sodium | 0.92 | 3.09 |
| Ethylamine | 0.97 | 5.42 |
| Ethylenediamine | 1.11 | 15.31 |
| Diethylamine | 1.12 | 7.91 |
| Triethylamine | 1.18 | 48.4 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gupta, D.; Bhatia, D.; Dave, V.; Sutariya, V.; Varghese Gupta, S. Salts of Therapeutic Agents: Chemical, Physicochemical, and Biological Considerations. Molecules 2018, 23, 1719. https://doi.org/10.3390/molecules23071719
Gupta D, Bhatia D, Dave V, Sutariya V, Varghese Gupta S. Salts of Therapeutic Agents: Chemical, Physicochemical, and Biological Considerations. Molecules. 2018; 23(7):1719. https://doi.org/10.3390/molecules23071719
Chicago/Turabian StyleGupta, Deepak, Deepak Bhatia, Vivek Dave, Vijaykumar Sutariya, and Sheeba Varghese Gupta. 2018. "Salts of Therapeutic Agents: Chemical, Physicochemical, and Biological Considerations" Molecules 23, no. 7: 1719. https://doi.org/10.3390/molecules23071719






