New Biscoumarin Derivatives: Synthesis, Crystal Structure, Theoretical Study and Antibacterial Activity against Staphylococcus aureus
Abstract
:1. Introduction
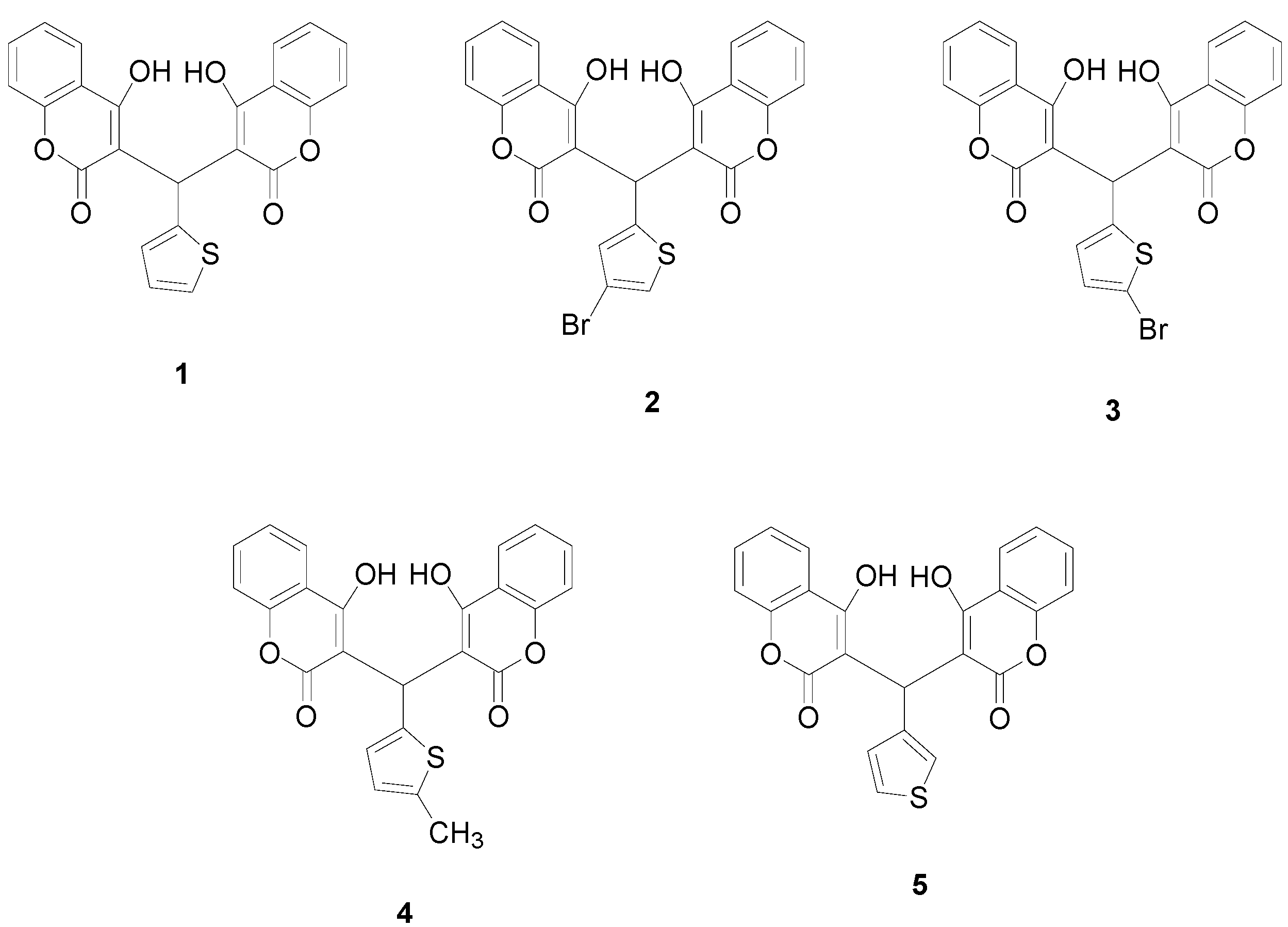
2. Results and Discussion
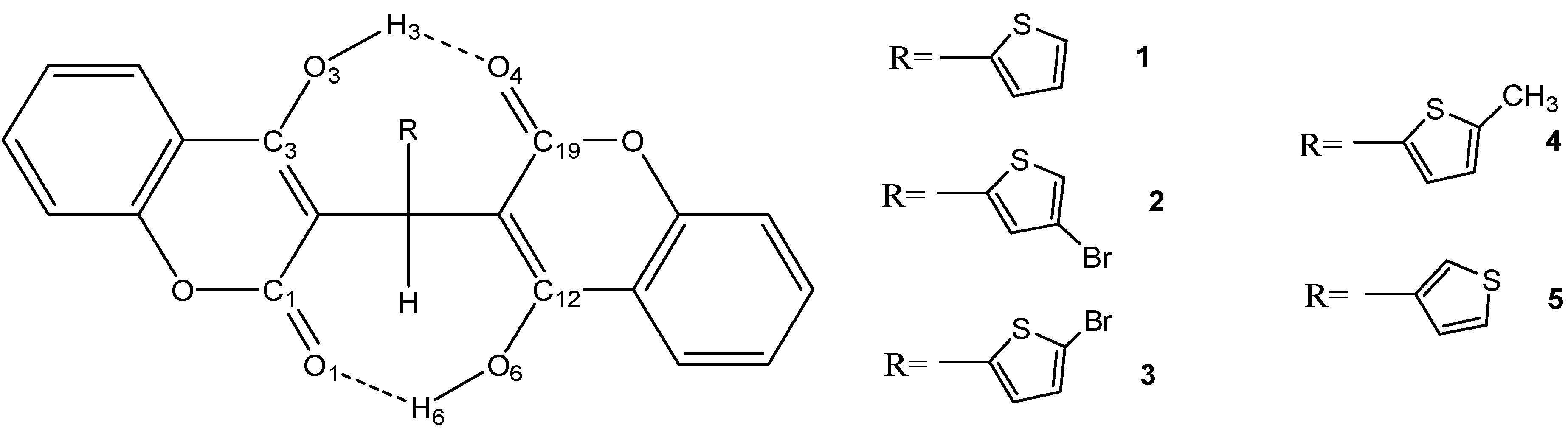
2.1. Molecular Structure
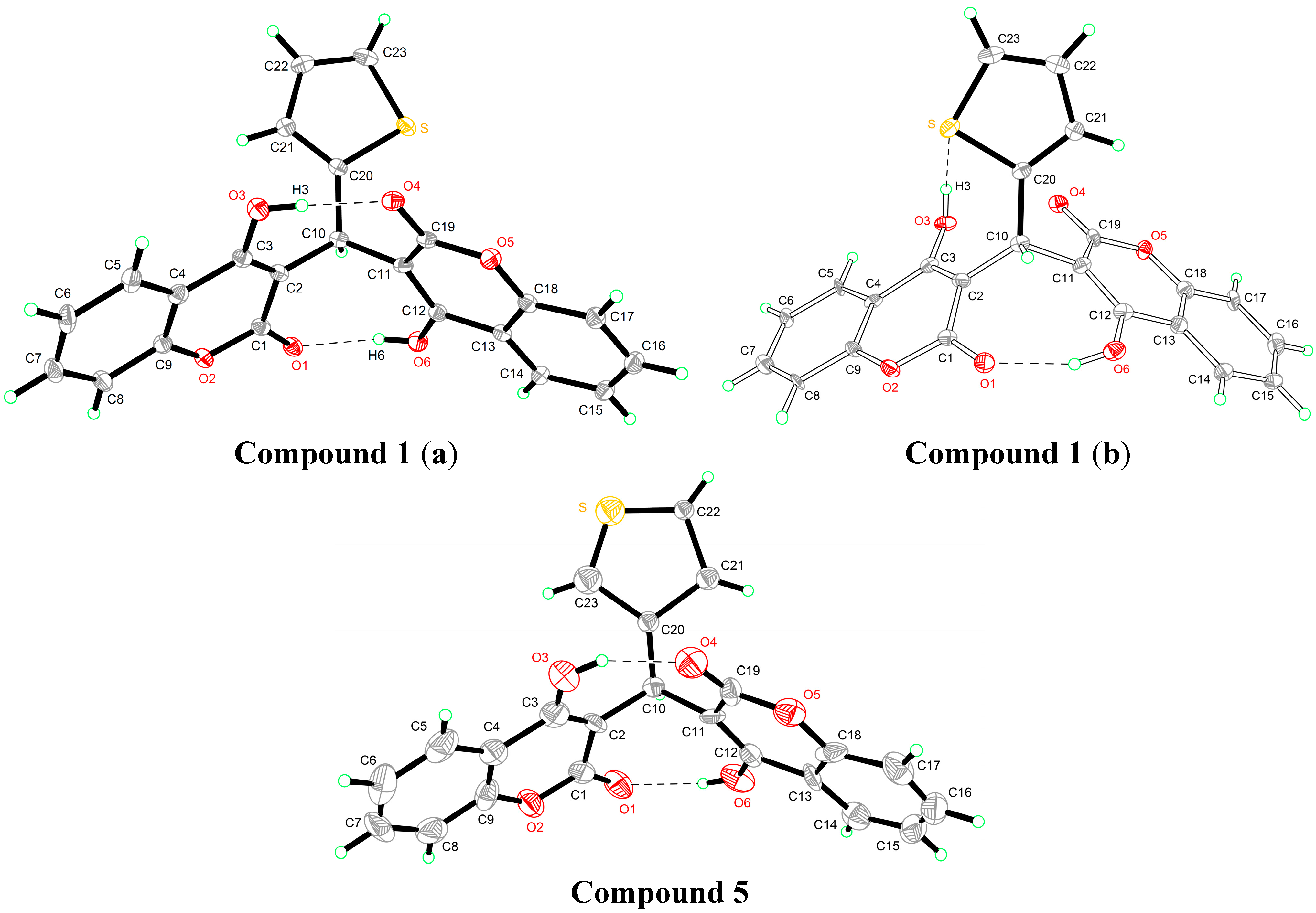
2.2. Quantum Chemical Calculations
2.2.1. Geometric Parameters of Compounds 1–5
| Name Definition | Compound 1 | Compound 5 | ||||||
|---|---|---|---|---|---|---|---|---|
| X-ray | 6-31G* | 6-31+G** | 6-311G* | X-ray | 6-31G* | 6-31+G** | 6-311G* | |
| O3···O4 | 2.592 | 2.639 | 2.614 | 2.643 | 2.587 | 2.643 | 2.621 | 2.648 |
| O1···O6 | 2.697 | 2.704 | 2.695 | 2.711 | 2.709 | 2.698 | 2.686 | 2.706 |
| C19=O4 | 1.234 | 1.229 | 1.232 | 1.222 | 1.192 | 1.229 | 1.232 | 1.222 |
| C1=O1 | 1.235 | 1.233 | 1.236 | 1.226 | 1.214 | 1.233 | 1.236 | 1.226 |
| C1-O2 | 1.361 | 1.372 | 1.370 | 1.371 | 1.309 | 1.373 | 1.371 | 1.372 |
| C9-O2 | 1.355 | 1.367 | 1.369 | 1.366 | 1.324 | 1.368 | 1.369 | 1.366 |
| C19-O5 | 1.352 | 1.376 | 1.373 | 1.375 | 1.318 | 1.377 | 1.375 | 1.377 |
| C18-O5 | 1.354 | 1.367 | 1.368 | 1.365 | 1.389 | 1.367 | 1.368 | 1.365 |
| C10-C20 | 1.514 | 1.521 | 1.522 | 1.520 | 1.412 | 1.529 | 1.529 | 1.528 |
| C1-C2-C10 | 113.63 | 114.14 | 114.12 | 113.94 | 113.38 | 114.62 | 114.65 | 114.40 |
| C3-C2-C10 | 126.92 | 126.33 | 126.55 | 126.52 | 126.59 | 125.76 | 125.91 | 125.96 |
| C10-C11-C19 | 119.17 | 118.92 | 119.07 | 118.71 | 115.55 | 119.12 | 119.37 | 118.90 |
| C10-C11-C12 | 122.30 | 121.42 | 121.47 | 121.58 | 127.08 | 121.40 | 121.37 | 121.56 |
| C2-C10-C11 | 112.56 | 113.41 | 113.58 | 113.51 | 110.78 | 112.96 | 113.15 | 113.03 |
| C2-C10-C20 | 116.66 | 114.66 | 114.89 | 114.82 | 114.91 | 114.48 | 114.43 | 114.59 |
| C11-C10-C20 | 111.34 | 113.97 | 114.02 | 113.95 | 115.93 | 115.02 | 115.38 | 115.01 |
| C3-C2-C10-C11 | 84.78 | 83.91 | 83.52 | 84.56 | 88.12 | 87.60 | 87.46 | 88.20 |
| C2-C10-C11-C19 | 82.36 | 83.36 | 83.13 | 83.08 | 87.43 | 81.07 | 80.59 | 80.82 |
| C1-C2-C10-C20 | 136.87 | 134.30 | 133.69 | 134.30 | 134.62 | 135.07 | 134.21 | 135.02 |
| C19-C11-C10-C20 | 50.79 | 50.27 | 51.08 | 50.88 | 45.85 | 52.90 | 53.89 | 53.37 |
2.2.2. Estimation of the Single and Total HB Energies in Compounds 1–5
| System | Total Electronic Energies a | E(O6—H6···O1) | E(O3—H3···O4) | E(Total HB) |
|---|---|---|---|---|
| 1ab | −1734.116678 | −125.4805215 | ||
| 1a | −1734.096324 | −53.439427 | ||
| 1b | −1734.089239 | −72.0410945 | ||
| 2ab | −4305.229694 | −122.274786 | ||
| 2a | −4305.209554 | −52.87757 | ||
| 2b | −4305.203262 | −69.397216 | ||
| 3ab | −4305.225972 | −123.529775 | ||
| 3a | −4305.206014 | −52.399729 | ||
| 3b | −4305.19888 | −71.130046 | ||
| 4ab | −1773.408037 | −126.743387 | ||
| 4a | −1773.387526 | −53.8516305 | ||
| 4b | −1773.380274 | −72.8917565 | ||
| 5ab | −1734.116974 | −116.0287215 | ||
| 5a | −1734.097714 | −50.56713 | ||
| 5b | −1734.092041 | −65.4615915 |
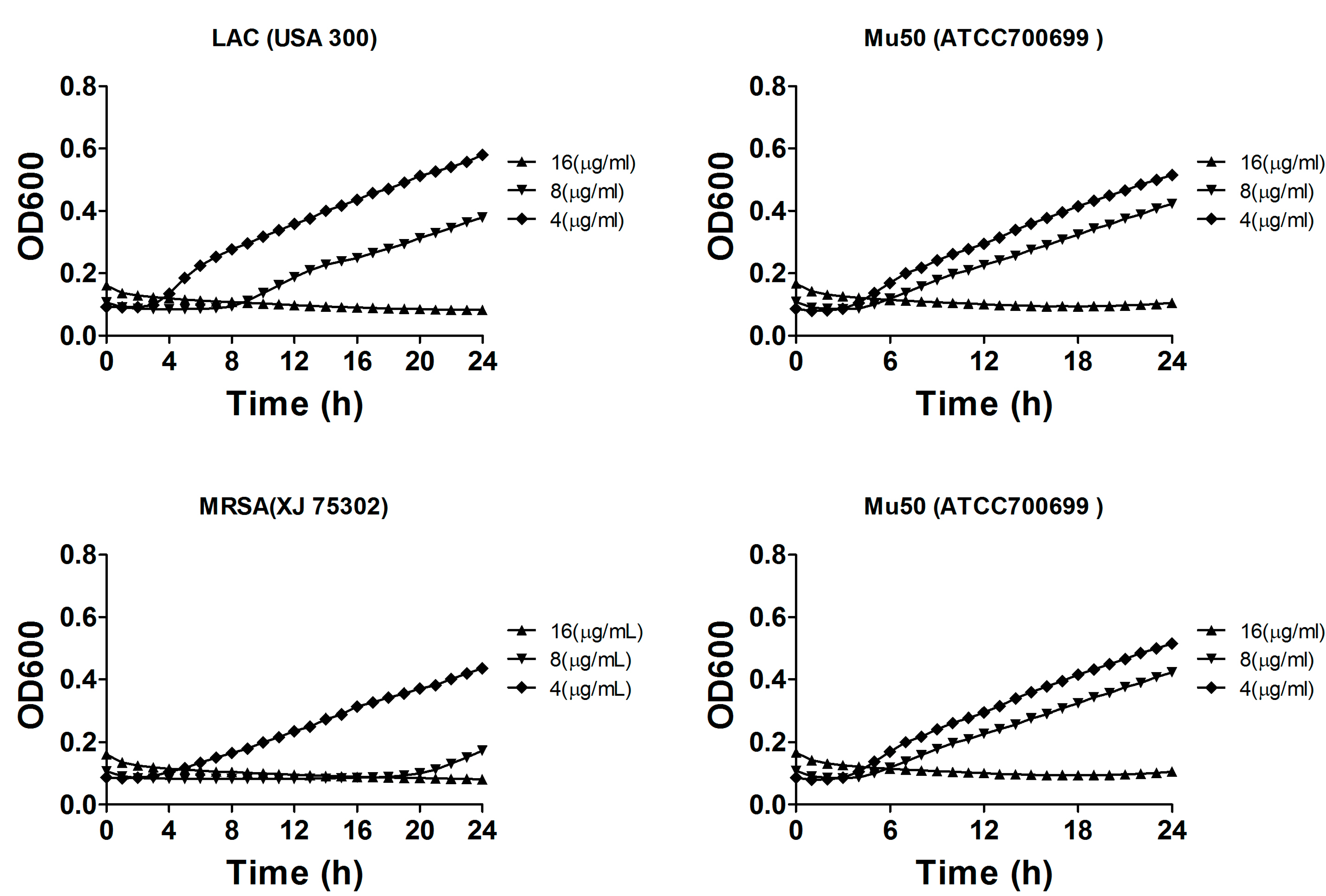
2.3. Minimal Inhibitory Concentration (MIC) Assay
| Drug | MIC (ug/mL) | |||
|---|---|---|---|---|
| S. aureas (ATCC 29213) | MRSA (XJ 75302) | Mu50 (ATCC 700699) | LAC (USA 300) | |
| Compound 1 | 8 | 8 | 16 | 32 |
| Compound 2 | 64 | 64 | 64 | 128 |
| Compound 3 | 64 | 64 | 64 | 128 |
| Compound 4 | 32 | 32 | 32 | 32 |
| Compound 5 | >256 | >256 | >256 | >256 |
| Ceftazidime | 8 (S) | >256 (R) | 256 (R) | 64 (R) |
| Ceftriaxone | 2 (S) | >256 (R) | 256 (R) | 32 (R) |
| Gentamicin | 0.12 (S) | 64 (R) | 32 (R) | 0.25 (S) |
| Piperacillin | 2 (S) | >128 (R) | >128 (R) | 64 (R) |
2.4. Bacterial Growth Inhibition
3. Experimental Section
3.1. Apparatus and Materials
3.2. Synthesis and Characterization of Compounds 1–5
3.3. X-ray Crystallography
| Parameter | Compound 1 | Compound 5 |
|---|---|---|
| Formula | C23H14O6S | C23H14O6S |
| Mr | 418.40 | 418.40 |
| Temperature/K | 113(2) | 293(2) |
| Crystal system | Monoclinic | Monoclinic |
| Space group | P21/n | P21/n |
| a/Å | 7.7250(8) | 7.7983(4) |
| b/Å | 8.9250(10) | 8.9785(5) |
| c/Å | 26.537(2) | 26.6473(19) |
| α/° | 90 | 90 |
| β/° | 96.319(9) | 96.514(6) |
| γ/° | 90 | 90 |
| V/Å3 | 1818.5(3) | 1853.72(19) |
| Z | 4 | 4 |
| Dcalc/g·cm−3 | 1.528 | 3.009 |
| μ(Mo Kα)/mm−1 | 1.951 | 1.711 |
| θ range/° | 3.35 to 72.59 | 2.40 to 25.00 |
| Reflections collected | 15733 | 6656 |
| No. unique data[R(int)] | 3541[0.0619] | 3261[0.0307] |
| No. data with I ≥ 2σ(I) | 3242 | 1892 |
| R1 | 0.0603 | 0.2049 |
| ωR2(all data) | 0.1362 | 0.6273 |
| CCDC | 889260 | 1014707 |
3.4. Quantum Chemical Calculations
3.5. Minimal Inhibitory Concentration (MIC) Assay
3.6. Bacterial Growth Inhibition
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Taylor, A.R. Methicillin-resistant Staphylococcus aureus infections. Prim. Care 2013, 40, 637–654. [Google Scholar] [CrossRef] [PubMed]
- Xia, J.; Gao, J.; Kokudo, N.; Hasegawa, K.; Tang, W. Methicillin-resistant Staphylococcus aureus antibiotic resistance and virulence. Biosci. Trends 2013, 7, 113–121. [Google Scholar] [PubMed]
- Pottinger, P.S. Methicillin-resistant Staphylococcus aureus infections. Med. Clin. North Am. 2013, 97, 601–619. [Google Scholar] [CrossRef] [PubMed]
- Barber, M. Methicillin-resistant staphylococci. J. Clin. Pathol. 1961, 14, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Tarai, B.; Das, P.; Kumar, D. Recurrent challenges for clinicians: Emergence of methicillin-resistant Staphylococcus aureus, vancomycin resistance, and current treatment options. J. Lab. Phys. 2013, 5, 71–78. [Google Scholar]
- Hetem, D.J.; Bonten, M.J. Clinical relevance of mupirocin resistance in Staphylococcus aureus. J. Hosp. Infect. 2013, 85, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Cravotto, G.; Nano, G.M.; Palmisano, S.G.; Tagliapietra, S. The chemistry of coumarin derivatives. Part XIII. The reactivity of 4-hydroxycoumarin under heterogeneous high-intensity sonochemical conditions. Synthesis 2003, 8, 1286–1291. [Google Scholar]
- Atta-ur-Rahman; Shabbir, M.; Ziauddin Sultani, S.; Jabbar, A.; Choudhary, M.I. Cinnamates and coumarins from the leaves of Murraya paniculata. Phytochemistry 1997, 44, 683–685. [Google Scholar]
- Al-Amiery, A.A.; Al-Bayati, R.I.H.; Saour, K.Y.; Radi, M.F. Cytotoxicity, antioxidant, and antimicrobial activities of novel 2-quinolone derivatives derived from coumarin. Res. Chem. Intermed. 2012, 38, 559–569. [Google Scholar] [CrossRef]
- Kontogiorgis, C.; Hadjipavlou-Litina, D. Biological evaluation of several coumarin derivatives designed possible anti-inflammatory/antioxidant agents. J. Enzym. Inhib. Med. Chem. 2003, 18, 63–69. [Google Scholar] [CrossRef]
- Smyth, T.; Ramachandran, V.N.; Smyth, W.F. A study of the antimicrobial activity of naturally occurring and synthetic coumarins. Int. J. Antimicrob. Agents 2009, 33, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Hua, J.; Zhou, J.; Zhang, H.; Zhu, H.; Cheng, Y.; Gust, R. Synthesis and in vitro antitumor activity of novel scopoletin derivatives. Bioorg. Med. Chem. Lett. 2012, 22, 5008–5012. [Google Scholar] [CrossRef] [PubMed]
- Iranshahi, M.; Askari, M.; Sahebkar, A.; Hadjipavlou-Litina, D. Evaluation of antioxidant, anti-inflammatory and lipoxygenase inhibitory activities of the prenylated coumarin umbelliprenin. DARU J. Pharm. Sci. 2009, 17, 99–103. [Google Scholar]
- Li, M.; Li, J.; Liu, B.; Zhou, Y.; Li, X.; Xue, X.; Hou, Z.; Luo, X. Synthesis, crystal structures, and anti-drug-resistant Staphylococcus aureus activities of novel 4-hydroxycoumarin derivatives. Eur. J. Pharmacol. 2013, 721, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Sheldrick, G.M. SHELXL-97, Program for Solution Crystal Structure and Refinement; University of Göttingen: Göttingen, Germany, 1997. [Google Scholar]
- Frisch, M.J.; Trucks, G.W.; Schlegel, H.B.; Scuseria, G.E.; Robb, M.A.; Cheeseman, J.R.; Scalmani, G.; Barone, V.; Mennucci, B.; Petersson, G.A.; et al. Gaussian 09, Revision A.02 ed; Gaussian, Inc.: Wallingford, CT, USA, 2009. [Google Scholar]
- Hohenberg, P.; Kohn, W. Inhomogeneous Electron Gas. Phys. Rev. 1964, 136, B864–B871. [Google Scholar] [CrossRef]
- Kohn, W.; Sham, L.J. Self-Consistent Equations Including Exchange and Correlation Effects. Phys. Rev. 1965, 140, A1133–A1138. [Google Scholar] [CrossRef]
- Becke, A.D. Density-functional thermochemistry III. The role of exact exchange. J. Chem. Phys. 1993, 98, 5648–5652. [Google Scholar] [CrossRef]
- Lee, C.; Yang, W.; Parr, R.G. Development of the Colle-Salvetti correlation-energy formula into a functional of the electron density. Phys. Rev. B 1988, 37, 785–789. [Google Scholar] [CrossRef]
- Miehlich, B.; Savin, A.; Stoll, H.; Preuss, H. Results obtained with the correlation energy density functionals of becke and Lee, Yang and Parr. Chem. Phys. Lett. 1989, 157, 200–206. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing: Nineteenth Informational Supplement M100-S19; CLSI: Wayne, PA, USA, 2009. [Google Scholar]
- Motyl, M.; Dorso, K.; Barrett, J. UNIT 13A.3 basic microbiological techniques used in antibacterial drug discovery. Curr. Protoc. Pharmacol. 2006. [Google Scholar] [CrossRef]
- Bassetti, M.; Merelli, M.; Temperoni, C.; Astilean, A. New antibiotics for bad bugs: Where are we? Ann. Clin. Microbiol. Antimicrob. 2013, 12. [Google Scholar] [CrossRef]
- Malani, P.N. Preventing postoperative Staphylococcus aureus infections. JAMA 2013, 309, 1408–1409. [Google Scholar] [CrossRef] [PubMed]
- Gordon, R.J.; Lowy, F.D. Pathogenesis of methicillin-resistant Staphylococcus aureus infection. Clin. Infect. Dis. 2008, 46, S350–S359. [Google Scholar] [CrossRef] [PubMed]
- Sample Availability: Samples of the compounds 1–5 are available from the authors.
© 2014 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qu, D.; Li, J.; Yang, X.-H.; Zhang, Z.-D.; Luo, X.-X.; Li, M.-K.; Li, X. New Biscoumarin Derivatives: Synthesis, Crystal Structure, Theoretical Study and Antibacterial Activity against Staphylococcus aureus. Molecules 2014, 19, 19868-19879. https://doi.org/10.3390/molecules191219868
Qu D, Li J, Yang X-H, Zhang Z-D, Luo X-X, Li M-K, Li X. New Biscoumarin Derivatives: Synthesis, Crystal Structure, Theoretical Study and Antibacterial Activity against Staphylococcus aureus. Molecules. 2014; 19(12):19868-19879. https://doi.org/10.3390/molecules191219868
Chicago/Turabian StyleQu, Di, Jing Li, Xiao-Hui Yang, Zi-Dan Zhang, Xiao-Xing Luo, Ming-Kai Li, and Xia Li. 2014. "New Biscoumarin Derivatives: Synthesis, Crystal Structure, Theoretical Study and Antibacterial Activity against Staphylococcus aureus" Molecules 19, no. 12: 19868-19879. https://doi.org/10.3390/molecules191219868




