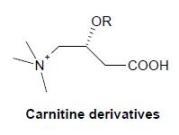
Carnitine Conjugate of Nipecotic Acid: A New Example of Dual Prodrug
Abstract
:Introduction
Results and Discussion

| Treatment | Latency to convulsions (s) |
|---|---|
| Control (saline + PTZ) | 677 ± 51 |
| Nipecotic acid + PTZ | 645 ± 50 |
| L-carnitine + PTZ | 664 ± 62 |
| 4 + PTZ | 1021 ± 55a |

| Treatment | Nipecotic acid (nmol/g)a |
|---|---|
| Control (saline) | n.d. |
| Nipecotic acid | n.d. |
| Compound 4 | 600 |
Conclusions
Experimental Section
General
Effects of the drugs on pentylenetetrazol-induced seizures
Determination of nipecotic acid in mouse brains
Statistical evaluation
Acknowledgments
References
- Hansch, C.; Bjorkroth, J.P.; Leo, A. Hydrophobicity and central nervous system agents: On the principle of minimal hydrophobicity in drug design. J. Pharm. Sci. 1987, 76, 663–687. [Google Scholar]
- Testa, B.; Carrupt, P.A.; Gaillard, P.; Billois, F.; Weber, P. Lipophilicity in molecular modelling. Pharm. Res. 1996, 13, 335–343. [Google Scholar] [CrossRef]
- Tamai, I.; Tsuji, A. Transporter mediated permeation of drugs across the blood-brain barrier. J. Pharm. Sci. 2000, 89, 1371–1388. [Google Scholar] [CrossRef]
- Manfredini, S.; Pavan, B.; Vertuani, S.; Scaglianti, M.; Compagnone, D.; Biondi, C.; Scatturin, A.; Tanganelli, S.; Ferraro, L.; Prasad, P.; Dalpiaz, A. Design, synthesis and activity of ascorbic acid prodrugs of nipecotic, kynurenic and diclophenamic acids, liable to increase neurotropic activiy. J. Med. Chem. 2002, 45, 559–562. [Google Scholar] [CrossRef]
- Bahl, J.J.; Bressler, R. The pharmacology of carnitine. Ann. Rev. Pharmacol. Toxicol. 1987, 27, 257–277. [Google Scholar] [CrossRef]
- Brass, E.P. L-Carnitine and Its Role in Medicine: From Function to Therapy; Ferrari, R., DiMauro, S., Sherwood, G., Eds.; Academic Press Limited: London, UK, 1992; pp. 21–36. [Google Scholar]
- Virmani, M.A.; Rossi, S.; Conti, R.; Spadoni, A.; Arrigoni, -Martelli, E.; Calvani, M. Structural, metabolic and ionic requirements for the uptake of L-carnitine by primary rat cortical cells. Pharm. Res. 1996, 33, 19–27. [Google Scholar]
- Dalpiaz, A.; Pavan, B.; Vertuani, S.; Vitali, F.; Scaglianti, M.; Bortolotti, F.; Biondi, C.; Scatturin, A.; Tanganelli, S.; Ferraro, L.; Marzola, G.; Prasad, P.; Manfredini, S. Ascorbic and 6-Br-ascorbic acid conjugates as a tool to increase the therapeutic effects of potentially central active drugs. Eur. J. Pharm. Sci. 2005, 24, 259–269. [Google Scholar]
- Frey, H.H.; Popp, C.; Loscher, W. Influence of inhibitors of the high affinity GABA uptake on seizure tresholds in mice. Neuropharmacology 1979, 18, 581–590. [Google Scholar] [CrossRef]
- Yu, Z.; Iryo, Y.; Matsuoka, M.; Igisu, H.; Ikeda, M. Suppression of pentylenetetrazol-induced seizures by carnitine in mice. Naunyn Schmiedebergs Arch. Pharmacol. 1997, 355, 545–549. [Google Scholar] [CrossRef]
- Kim, Y.C.; Zhao, L.X.; Kim, T.H.; Je, S.M.; Kim, E.K.; Choi, H.; Chae, W.G.; Park, M.; Choi, J.; Jahng, Y.; Lee, E.S. Design and synthesis of anticonvulsive agents γ-vinyl GABA-based potential dual acting prodrugs and their biological activities. Bioorg. Med. Chem. Lett. 2000, 10, 609–614. [Google Scholar] [CrossRef]
- Nassereddine-Sebaei, M.; Crider, A.M.; Carrol, R.T.; Hinko, C.N. Determination of m-nitrophenol and nipecotic acid in mouse tissues by high-performance liquid chromatography after administration of anticonvulsant m-nirophenyl-3-piperidinecarboxylate hydrochloride. J. Pharmaceut. Sci. 1993, 82, 39–43. [Google Scholar] [CrossRef]
- Sample Availability: Contact the authors.
© 2009 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Napolitano, C.; Scaglianti, M.; Scalambra, E.; Manfredini, S.; Ferraro, L.; Beggiato, S.; Vertuani, S. Carnitine Conjugate of Nipecotic Acid: A New Example of Dual Prodrug. Molecules 2009, 14, 3268-3274. https://doi.org/10.3390/molecules14093268
Napolitano C, Scaglianti M, Scalambra E, Manfredini S, Ferraro L, Beggiato S, Vertuani S. Carnitine Conjugate of Nipecotic Acid: A New Example of Dual Prodrug. Molecules. 2009; 14(9):3268-3274. https://doi.org/10.3390/molecules14093268
Chicago/Turabian StyleNapolitano, Carmela, Martina Scaglianti, Emanuela Scalambra, Stefano Manfredini, Luca Ferraro, Sarah Beggiato, and Silvia Vertuani. 2009. "Carnitine Conjugate of Nipecotic Acid: A New Example of Dual Prodrug" Molecules 14, no. 9: 3268-3274. https://doi.org/10.3390/molecules14093268