Antiosteoporotic Activity of Anthraquinones from Morinda officinalis on Osteoblasts and Osteoclasts
Abstract
:Introduction
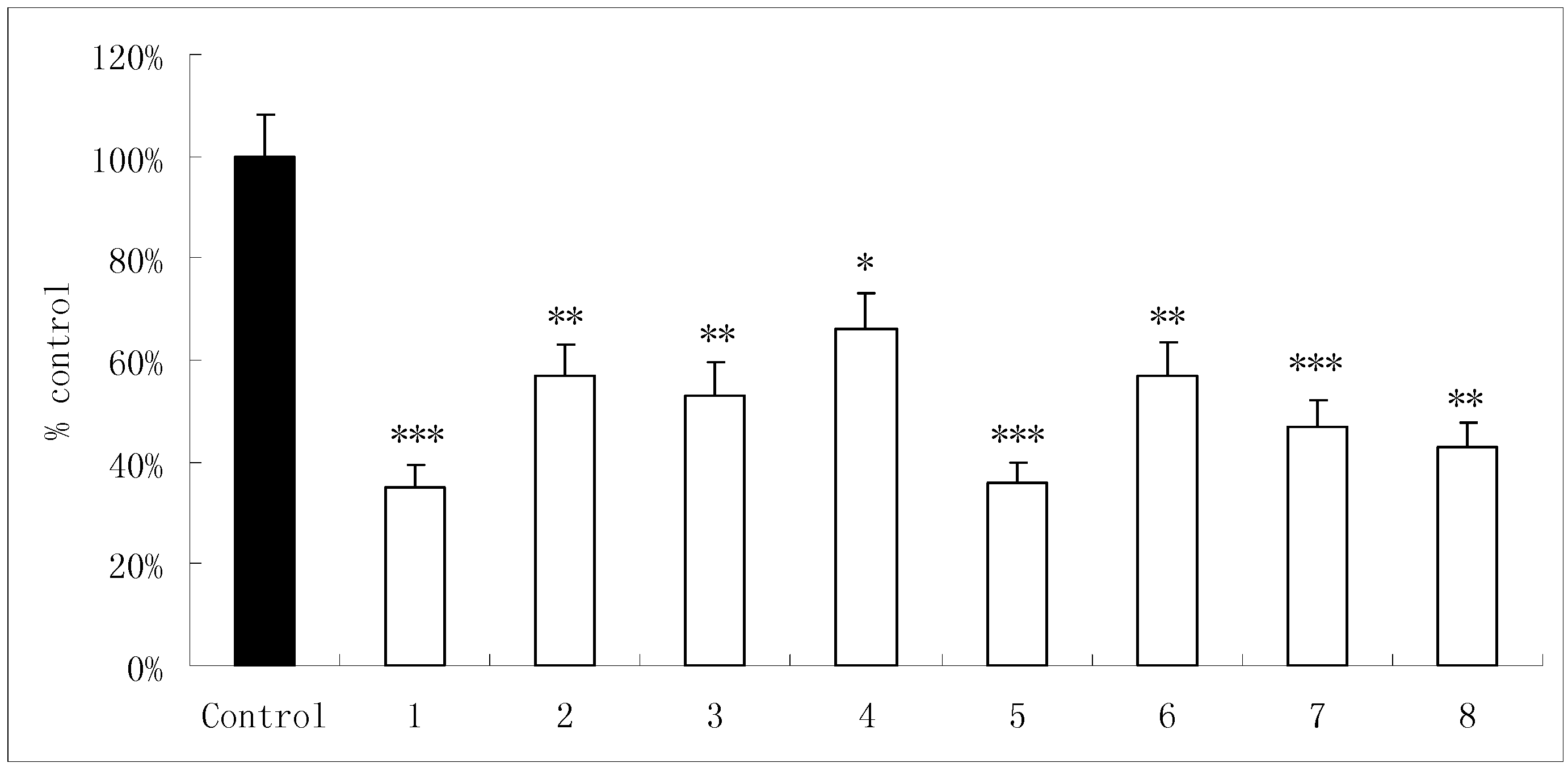
Results and Discussion
| Fractions | Conc. (µg/mL) | Osteoblast proliferation Absorbance (550nm) | Osteoblastic ALP activity (μmol/mg) | Osteoclastic TRAP activity (nmol/min/100 Osteoclastic cell ) |
|---|---|---|---|---|
| Control | 0.51±0.03 | 3.71±0.31 | 15.0±1.3 | |
| EMO extracts | 200 | 0.76±0.05** (49.1%) | 4.37±0.42** (17.8%) | 9.2±0.9** (38.7%) |
| 400 | 0.86±0.08** (68.6%) | 4.42±0.39** (19.1%) | 8.8±0.6** (41.3%) | |
| Petroleum ether fraction | 10 | 0.54±0.04 (5.8%) | 3.31±0.29 (49.1%) | 14.0±1.4 (-6.7%) |
| 20 | 0.51±0.02 (0%) | 3.38±0.32 (-1.6%) | 13.2±1.1 (-12.0%) | |
| Ethyl acetate fraction | 10 | 0.79±0.06** (54.9%) | 4.40±0.43** (18.6%) | 8.0±0.7** (90.1%) |
| 20 | 0.97±0.11** (90.1%) | 4.97±0.48** (33.9%) | 6.8±0.8** (55.0%) | |
| n-Butanol fraction | 10 | 0.61±0.04 (19.6%) | 3.38±0.29 (-8.9%) | 13.8±0.6 (-8.0%) |
| 20 | 0.58±0.01 (13.7%) | 3.39±0.32 (-8.6%) | 15.2±1.6 (1.3%) | |
| Aqueous fraction | 10 | 0.52±0.02 (1.9%) | 3.30±0.31 (-11.1%) | 16.1±1.3 (7.3%) |
| 20 | 0.56±0.06 (9.8%) | 3.41±0.33 (-8.1%) | 15.5±1.4 (3.3%) |
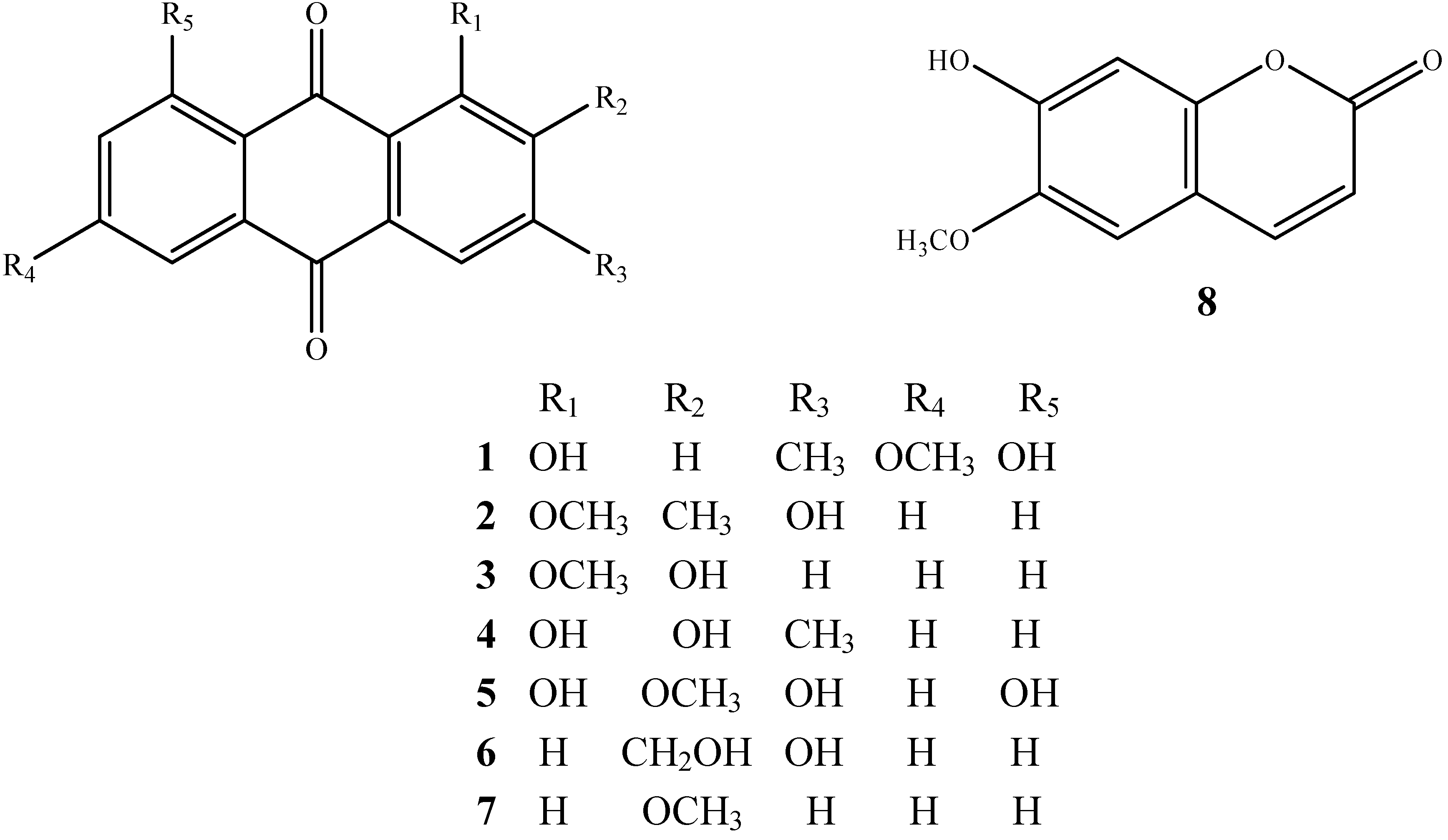
| Compound | Osteoblast proliferation absorbanc (550 nm) | Osteoblastic ALP activity (μmol/mg) | ||||
|---|---|---|---|---|---|---|
| 10-10mol/L | 10-9mol/L | 10-8mol/L | 10-10mol/L | 10-9mol/L | 10-8mol/L | |
| Control | 0.55±0.02 | 0.55±0.02 | 0.55±0.02 | 3.91±0.37 | 3.91±0.37 | 3.91±0.37 |
| 1 | 0.52±0.01 | 0.57±0.04 | 0.54±0.03 | 3.54±0.35 | 3.60±0.34 | 3.53±0.29 |
| 2 | 0.54±0.08 | 0.53±0.06 | 0.55±0.05 | 3.53±0.31 | 3.60±0.34 | 3.71±0.36 |
| 3 | 0.62±0.04* | 0.63±0.05* | 0.65±0.04* | 3.65±0.28 | 3.60±0.26 | 3.16±0.36 |
| 4 | 0.52±0.02 | 0.55±0.02 | 0.62±0.02* | 4.49±0.36** | 4.60±0.43** | 4.75±0.39** |
| 5 | 0.64±0.09 | 0.59±0.06 | 0.56±0.02 | 3.47±0.46 | 4.99±0.47** | 5.20±0.46** |
| 6 | 0.55±0.03 | 0.5±0.05 | 0.60±0.02 | 3.98±0.30 | 3.80±0.34 | 3.56±0.34 |
| 7 | 0.43±0.02 | 0.51±0.04 | 0.54±0.03 | 3.67±0.26 | 3.54±0.31 | 3.81±0.36 |
| 8 | 0.66±0.05* | 0.67±0.03* | 0.69±0.03** | 4.79±0.46** | 4.78±0.37** | 5.09±0.47** |
| Compound | Osteoclastic TRAP activity (nmol/min/100 osteoclastic cell ) | ||
|---|---|---|---|
| 10-7mol/L | 10-6mol/L | 10-5mol/L | |
| Control | 34.3±2.8 | 34.3±2.8 | 34.3±2.8 |
| 1 | 30.7±2.9* | 19.9±1.5** | 17.7±1.4** |
| 2 | 21.6±1.8** | 18.5±1.4*** | 13.8±1.3*** |
| 3 | 33.8±1.4 | 28.6±2.8* | 20.7±2.4** |
| 4 | 27.4±1.9** | 26.6±1.3** | 25.0±1.4** |
| 5 | 22.4±2.2** | 17.8±1.7*** | 9.8±1.0*** |
| 6 | 28.9±2.1* | 26.80±2.0** | 20.3±1.4** |
| 7 | 16.5±1.6*** | 16.0±1.5*** | 13.5±1.1*** |
| 8 | 28.4±2.1* | 25.1±1.9** | 17.6±1.7*** |
Conclusions
Experimental
General
Plant material
Extraction and isolation
Cell cultures
Assay for osteoblast proliferation and alkaline phosphatase (ALP) activity
Assay for osteoclastic TRAP activity
Determination of bone resorption pit
Acknowledgements
References
- Yang, Y.J.; Shu, H.Y.; Min, Z.D. Anthraquinones isolated from Morinda officinalis and Damnacanthusindicus. Acta Pharm. Sinica 1992, 27, 358–364. [Google Scholar]
- Seo, B.I.; Ku, S.K.; Cha, E.M.; Perk, J.H.; Kim, J.D.; Chol, H.Y.; Lee, H.S. Effect of Mornidae radix extracts on experimental osteoporosis in sciatic neurectomized mice. Phytother. Res. 2005, 19, 231–238. [Google Scholar] [CrossRef]
- Xie, H.G.; Zhang, H.W.; Zhang, J.; Xu, L.Z.; Zou, Z.M. Chemical constituents from Inula cappa. Chin. J. Nat. Med. 2007, 5, 193–196. [Google Scholar]
- Koumaglo, K.; Gbeassor, M.; Nikabu, O.; De, S.C.; Werner, W. Effects of three compounds extracted from Morinda lucida on Plasmodium falciparum. Planta Med. 1992, 58, 533–534. [Google Scholar] [CrossRef]
- Schripsema, J.; Ramos, V.A.; Verpoorte, R. Robustaquinones, novel anthraquinones from an elicited Cinchona robusta suspension culture. Phytochemistry 1999, 51, 55–60. [Google Scholar] [CrossRef]
- Sittie, A.A.; Lemmich, E.; Olsen, C.E.; Hviid, D.; Kharazmi, A.; Nkrumah, F.K.; Christensen, S.B. Structure-activity studies: in vitro antileishmanial and antimalarial activities of anthraquinones from Morinda lucida. Pianta Med. 1999, 65, 259–261. [Google Scholar] [CrossRef]
- Burnett, A.; Thomson, R. Naturally occurring quinones. part x. The quinonoid constituents of tabebuia avellanedae (Bignoniaceae). J. Chem. Soc. C 1967, 2100–2104. [Google Scholar] [CrossRef]
- Owen, T.A.; Aronow, M.; Shalhoub, V.; Barone, L.M.; Wilming, L.; Tassinari, M.S.; Kennedy, M.B.; Pockwinse, S.; Lian, J.B.; Stein, G.S. Progressive development of the rat osteoblast phenotype in vitro: reciprocal relationship in expression of genes associated with osteoblast proliferation and differentiation during formation of the bone extracelluar matrix. J. Cell. Physiol. 1990, 143, 420–430. [Google Scholar] [CrossRef]
- Vaes, G. Celluar biology and biochemical mechanism of bone resorption. A review of recent developments on the formation, activation, and mode of action of osteoclasts. Clin. Orthop. Relat. Res. 1988, 231, 239–271. [Google Scholar]
- Lee, S.U.; Shin, H.K.; Min, Y.K.; Kim, S.H. Emodin accelerates osteoblast differentiation through phosphatidylinositol 3-kinase activation and bone morphogenetic protein-2 gene expression. Int. J. Immunopharmacol. 2008, 8, 741–747. [Google Scholar]
- Wang, L.; Mao, Y.J.; Wang, W.J. Inhibitory effect of diacere in on osteoclastic bone destruction and its possible mechan ism of action. Acta Pharm. Sinica 2006, 41, 555–560. [Google Scholar] [CrossRef]
- Savarino, L.; Benetti, D.; Baldini, N.; Tarabusi, C.; Greco, M.; Aloisi, R.; Frascarelli, S.; Fantozzi, R.; Dianzani, C.; Mian, M. A preliminary in vitro and in vivo study of the effects of new anthraquinones on neutrophils and bone remodeling. J. Biomed. Mater. Res. 2005, 75A, 324–332. [Google Scholar] [CrossRef]
- Zhang, J.; Munger, R.G.; West, N.A.; Cutler, D.R.; Wengreen, H.J.; Corcoran, C.D. Antioxidant intake and risk of osteoporotic hip fracture in Utah: an effect modified by smoking status. Am. J. Epidemiol. 2006, 163, 9–17. [Google Scholar]
- Hofbauer, L.C.; Lacey, D.L.; Dunstan, C.R.; Spelsberg, T.C.; Riggs, B.L.; Khosla, S. Interleukin-1β and tumor necrosis factor-α, but not interleukin-6 stimulate osteoprotegerin ligand gene expression in human osteoblastic cells. Bone 1999, 25, 255–259. [Google Scholar] [CrossRef]
- Tamura, T.; Shirai, T.; Kosaka, N.; Ohmori, K.; Takafumi, N. Pharmacological studies of diacerein in animal models of inflammation, arthritis and bone resorption. Eur. J. Pharmacol. 2002, 448, 81–87. [Google Scholar] [CrossRef]
- Ding, Y.; Zhao, L.; Mei, H.; Huang, Z.H.; Duan, Y.Y.; Ye, P. Exploration of emodin to treat alpha-naphthylisothiocyanate-induced cholestatic hepatitis via anti-inflammatory pathway. Eur. J. Pharmacol. 2008, 590, 377–386. [Google Scholar] [CrossRef]
- Daniel, A.B.; Roman, R.; Rafael, V.D.; Manuel, J.E. Peroxidase-mediated transformation of hydroxy-9,10-anthraquinones. Phytochemistry 2002, 60, 567–572. [Google Scholar] [CrossRef]
- Zin, A.M.; Abdulhamid, A.; Osman, A. Antioxidative activity of extracts from mengkudu (Morinda citrifolia L.) root, fruit and leaf. Food Chem. 2001, 78, 227–231. [Google Scholar]
- Liu, Z.D.; Zang, H.S.; Ou-Yang, Y.P. Biological study of growth pattern of newborn rat calvaria osteoblastic cell in vitro. Acta Anatom. Sin. 1995, 26, 157–159. [Google Scholar]
- Zambonin, Z.A.; Teti, A.; Primavera, M.V. Isolated osteoclasts in primary culture: first observation on structure and survival in culture media. Anat. Embryol. 1982, 165, 405–413. [Google Scholar] [CrossRef]
- Bradford, M.M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 1976, 72, 248–254. [Google Scholar] [CrossRef]
- Qin, L.P.; Zhang, Q.Y.; Tian, Y.P.; Zheng, H.C.; Huang, M.; Huang, B.K. Total coumarins from fruits of Cnidium monnieri (TCFC) inhibit the formation and differentiation of multinucleated osteoclasts derived from rat marrow cells. Acta Pharmacol. Sin. 2003, 24, 181–186. [Google Scholar]
- Sample Availability: Contact the authors.
© 2009 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Wu, Y.-B.; Zheng, C.-J.; Qin, L.-P.; Sun, L.-N.; Han, T.; Jiao, L.; Zhang, Q.-Y.; Wu, J.-Z. Antiosteoporotic Activity of Anthraquinones from Morinda officinalis on Osteoblasts and Osteoclasts. Molecules 2009, 14, 573-583. https://doi.org/10.3390/molecules14010573
Wu Y-B, Zheng C-J, Qin L-P, Sun L-N, Han T, Jiao L, Zhang Q-Y, Wu J-Z. Antiosteoporotic Activity of Anthraquinones from Morinda officinalis on Osteoblasts and Osteoclasts. Molecules. 2009; 14(1):573-583. https://doi.org/10.3390/molecules14010573
Chicago/Turabian StyleWu, Yan-Bin, Cheng-Jian Zheng, Lu-Ping Qin, Lian-Na Sun, Ting Han, Lei Jiao, Qiao-Yan Zhang, and Jin-Zhong Wu. 2009. "Antiosteoporotic Activity of Anthraquinones from Morinda officinalis on Osteoblasts and Osteoclasts" Molecules 14, no. 1: 573-583. https://doi.org/10.3390/molecules14010573
APA StyleWu, Y.-B., Zheng, C.-J., Qin, L.-P., Sun, L.-N., Han, T., Jiao, L., Zhang, Q.-Y., & Wu, J.-Z. (2009). Antiosteoporotic Activity of Anthraquinones from Morinda officinalis on Osteoblasts and Osteoclasts. Molecules, 14(1), 573-583. https://doi.org/10.3390/molecules14010573




