1. Introduction
The use of scientific management theory and methods is often emphasized in hospital management as it can give full play to the overall collaborative operational functions to allow for a full examination of hospital planning resources, such as staff, materials and information. The main purpose of such examinations is to provide patients with quality health care services and to meet the patient needs. However, medical institutions often suffer from a lack of adequate health care resources, have a lack of grading for collaborative work and have no clear guidelines for service provision, all of which make it difficult to achieve a scientific, rational and efficient use of the medical and health resources.
National health service sustainable development and hospital and medical management have been widely researched. Shusaku and Shoji used data mining methods to extract information stored in a hospital information systems and applied exploratory data analysis techniques and a generalized linear model to optimize the hospital’s management [
1]. From the perspective of improving patient satisfaction, Rozenblum, Lisby, Hockey
et al. conducted a survey in four academic hospitals in Denmark, Israel, the United Kingdom and the United States to analyze the relationship between hospital management and front-line clinicians, and demonstrated that patient satisfaction was influenced by clinician attitudes and the hospital construction management plan [
2]. Using an integration of genetic algorithms and a binary particle swarm optimization algorithm, Chiu
et al. proposed an RFID network layout method, and conducted optimization research on hospital management information transmission network issues [
3]. Inter-hospital ambulance transfer problems were analyzed by Nakamura
et al. using a discrete event simulation model, game theory and other research tools, the results from which showed that centralized resource sharing and collaboration had a significant impact on reducing hospital ambulance transfer times [
4]. Tianlin
et al. theoretically analyzed the necessity for hospital management innovations, and described hospital management innovation methods and basic practice principles [
5].
Management process research on collaborative synergy management is a mature field of study. Kapucu and Arslan based on research into leadership, decision-making and collaborative relationships between the government and aid organizations, found that synergy management using collaborative networks could improve emergency management efficiency through the effective use of emergency resources [
6]. Feng and Zhuowen conducted a comprehensive analysis of a multi-project collaborative management system, analyzed multi-project synergy generation and recommended measures to achieve enterprise-wide multi-project collaborative management using a multi-project collaborative management model [
7]. Comfort
et al. assessed the emergency response capacity of communities through the establishment of a dynamic simulation system model, and found that the transfer of and access to key information was helpful in improving community organizational network collaboration performance [
8].
Although there has been significant research and made a significant contribution in the aspect of improving patient satisfaction, advancing operational efficiency of the hospital and hospital management innovations in most cases, researchers have researched hospitals as independent individuals and from a theoretical or data driven perspective, so the issue of effective collaborative management between hospitals and medical services has not been fully tapped. In addition, although collaborative management thinking is quite mature, research on hospital collaborative management is rare, meaning that it is difficult to give an accurate picture of the situation in multi-level hospitals, or have definitive opinions about the administrative and collaborative performances between hospitals and health care providers. In view of this, and on the basis of previous studies, this paper analyzes hospital management from the perspective of collaborative management, and proposes a multi-level hospital management Synergy Entropy-House of Quality Measurement Model by introducing collaborative entropy theory. It is hoped that this model can provide a reference for improving hospital management and the coordination efficiency of organizations based on the synergy calculation.
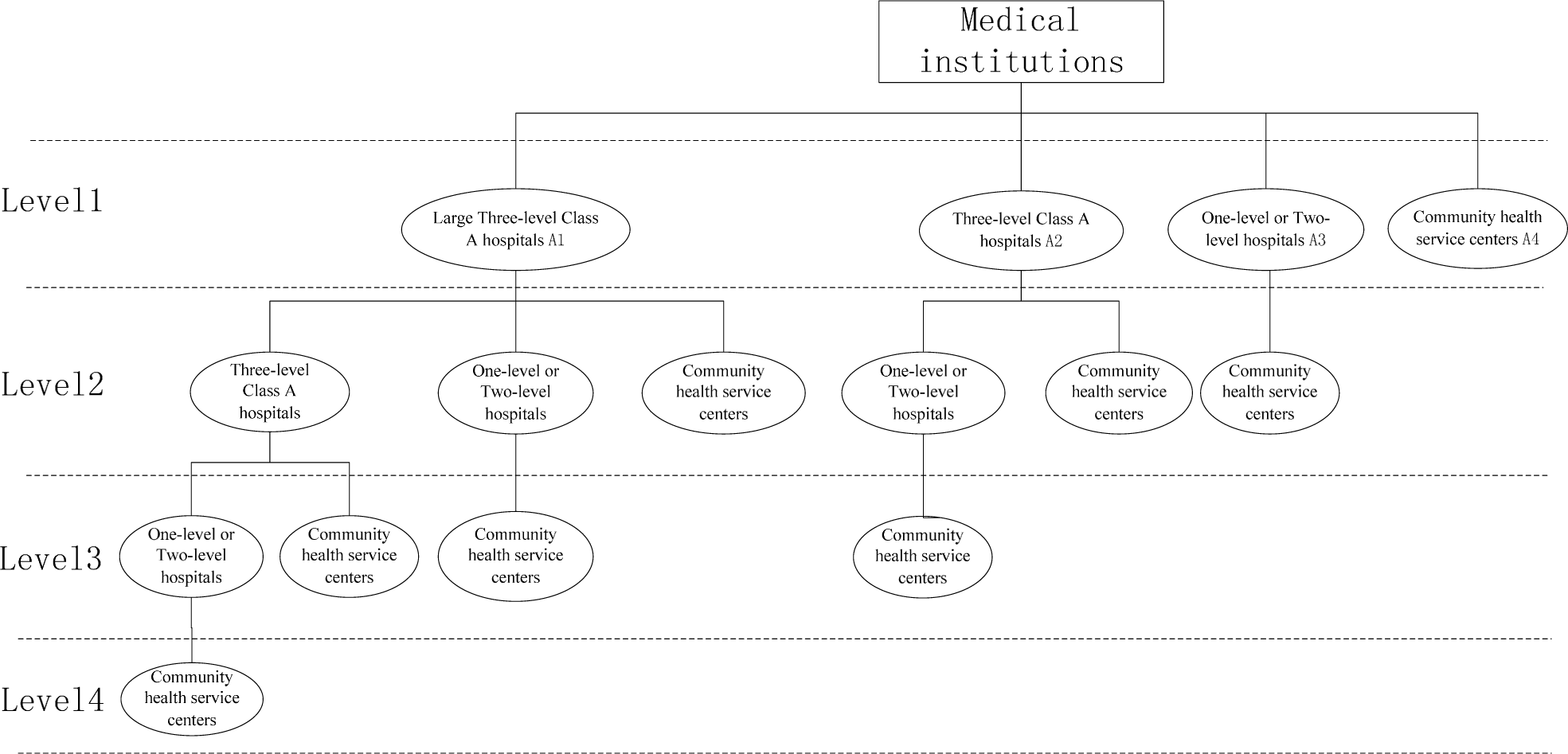
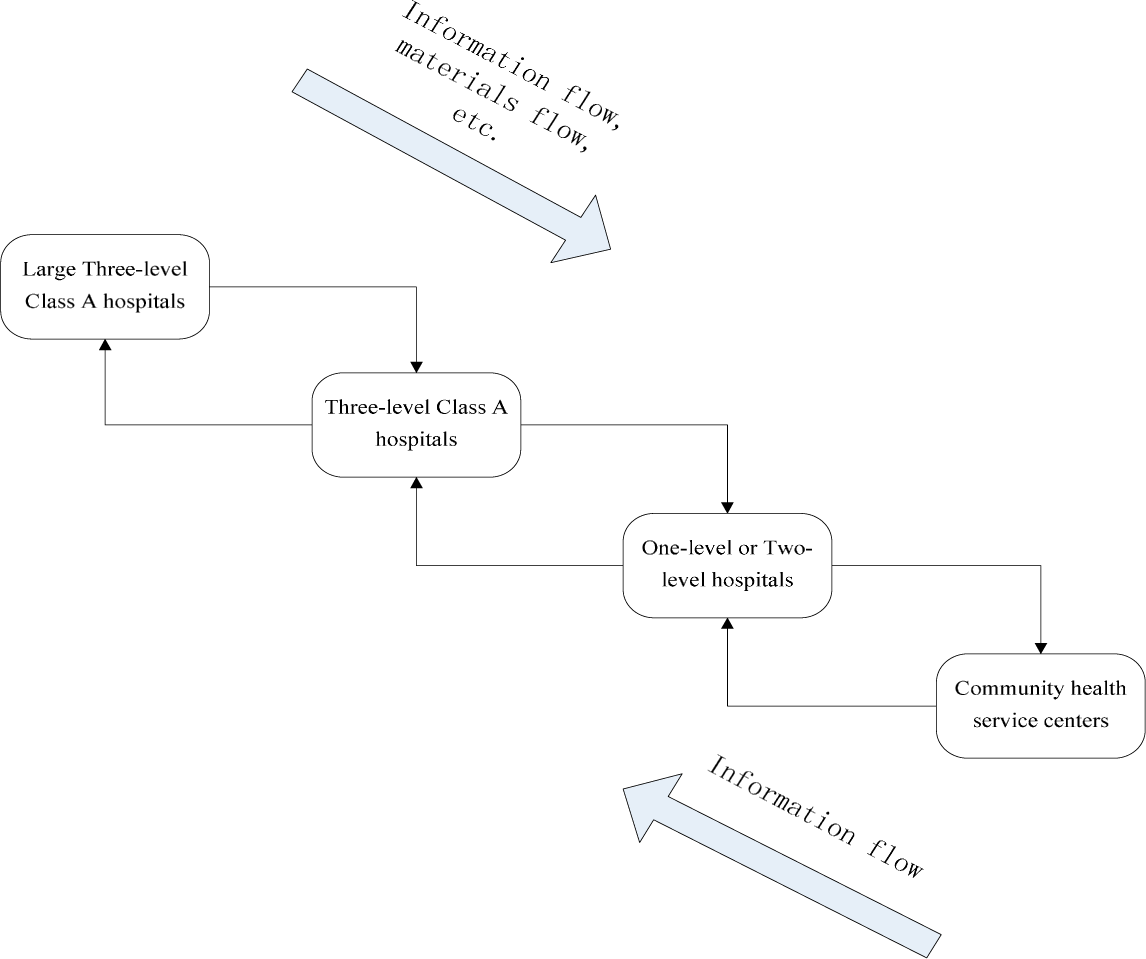
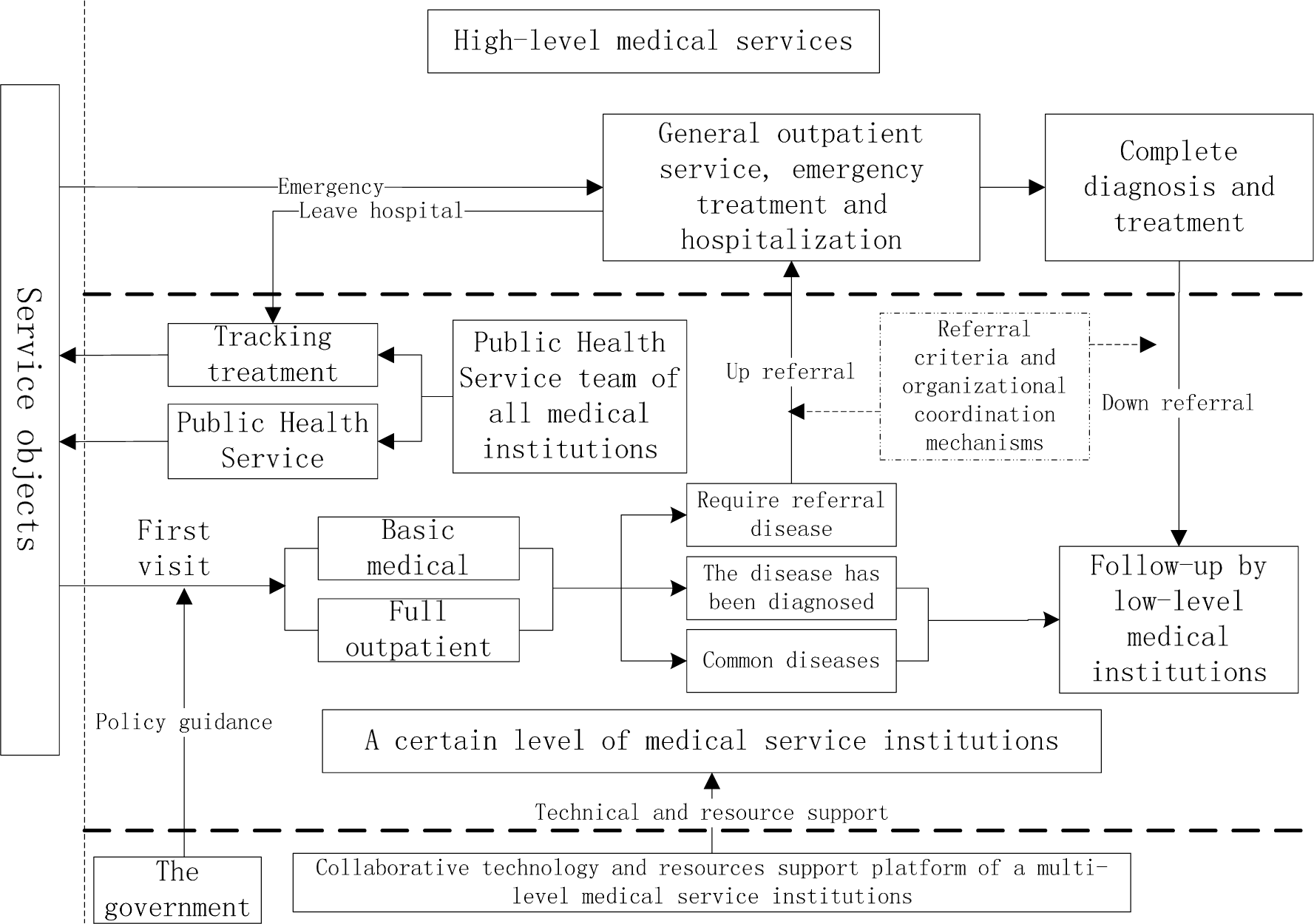
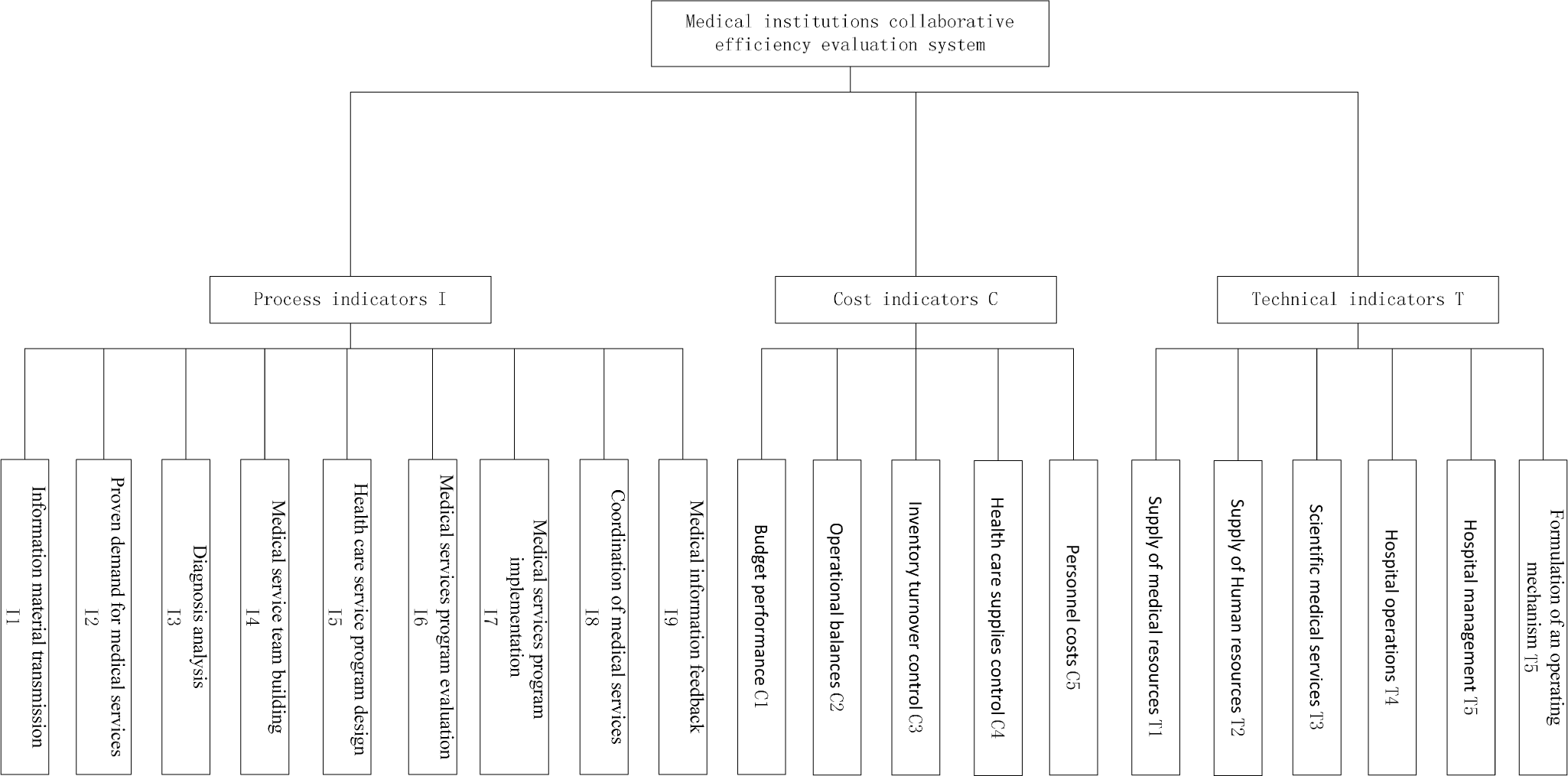
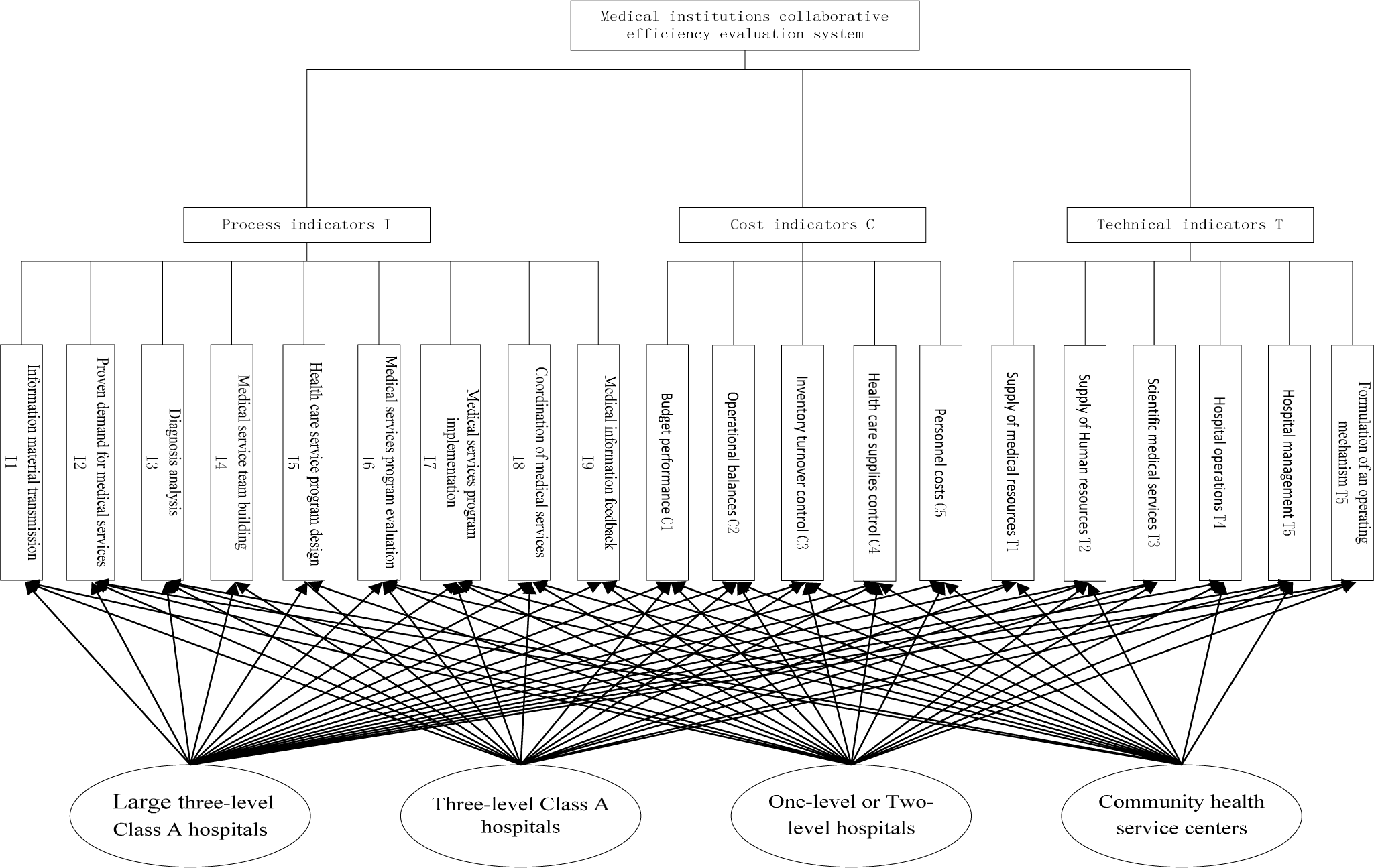
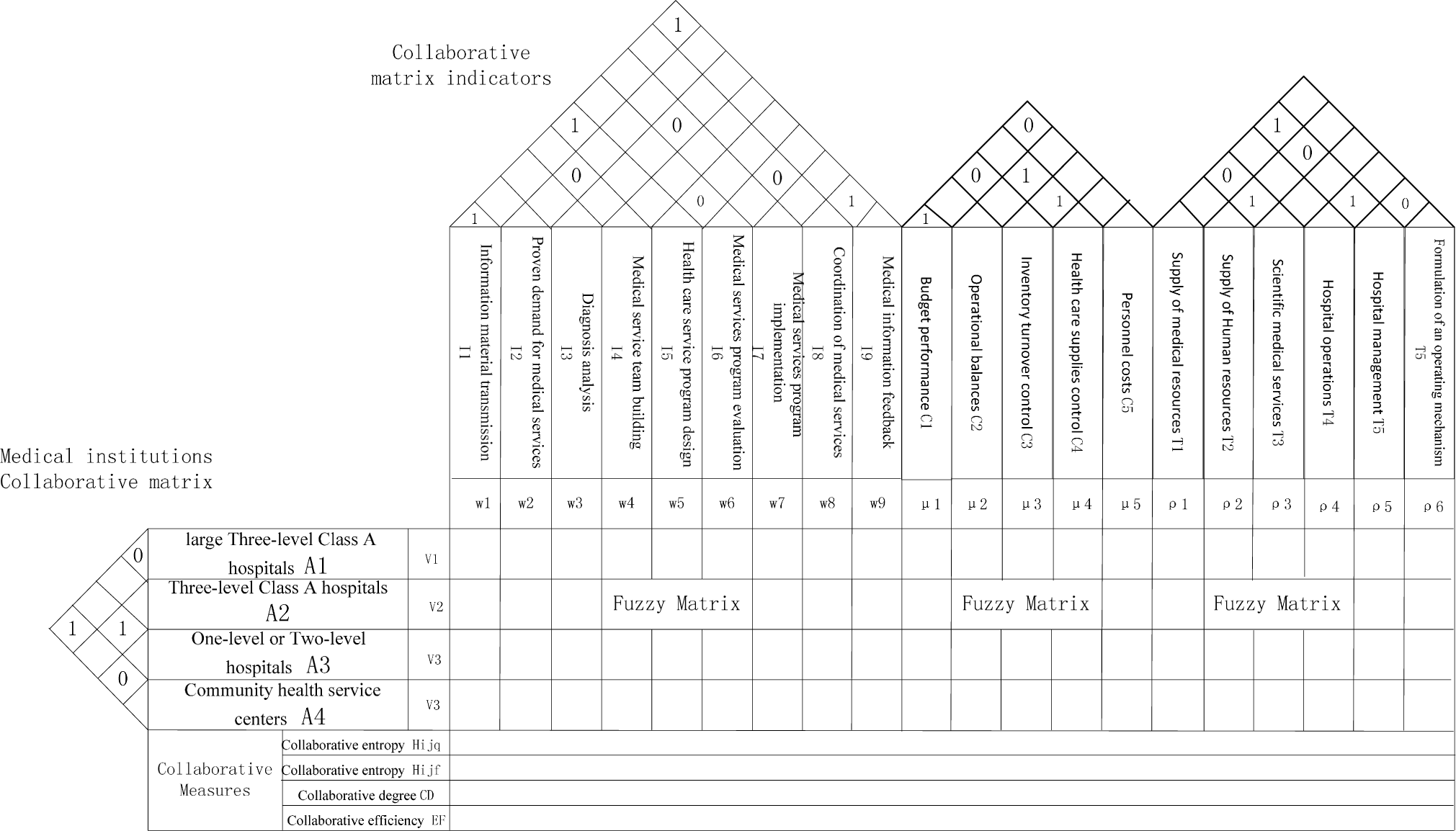
In Section 2, the paper establishes a structure of Multi-level medical institutions through on-the-spot investigation in medical institutions of Sichuan province. Furthermore, basic medical services and activities of medical institutions were analyzed, on this basis, the paper constructs the research framework of collaborative management research of multi-level medical institutions. In Section 3, this paper introduces the concept of Synergy Entropy and House of Quality, build a Synergy Entropy-House of Quality Measurement Model, and the specific steps and measure principle measure was introduced. Finally, through case analysis of a certain level of medical institutions in Sichuan province to verify the Synergy Entropy-House of Quality Measurement Model is scientific and effective.
5. Conclusions
It is vital to constantly improve hospital management and improve coordination to improve the provision of medical services, and to promote a rational flow of medical resources. In this paper, a Synergy Entropy and House of Quality analysis model was established based on collaborative entropy, which was used in the comprehensive analysis of the collaborative relationship between the different medical institution levels and various medical work stages. This allowed for the inherent synergies between the various elements of hospital management to be illuminated, the collaborative hospital management performance to be evaluated, and the circulation of medical resources to be promoted. From this analysis the following conclusions were made:
Using the concept of quality house and collaborative entropy principles, this paper transformed the qualitative analysis regarding hospital synergy performance management elements to quantitative calculations and established a quality house evaluation model for hospital management, providing a new method for the evaluation and optimization of hospital management collaborative performance.
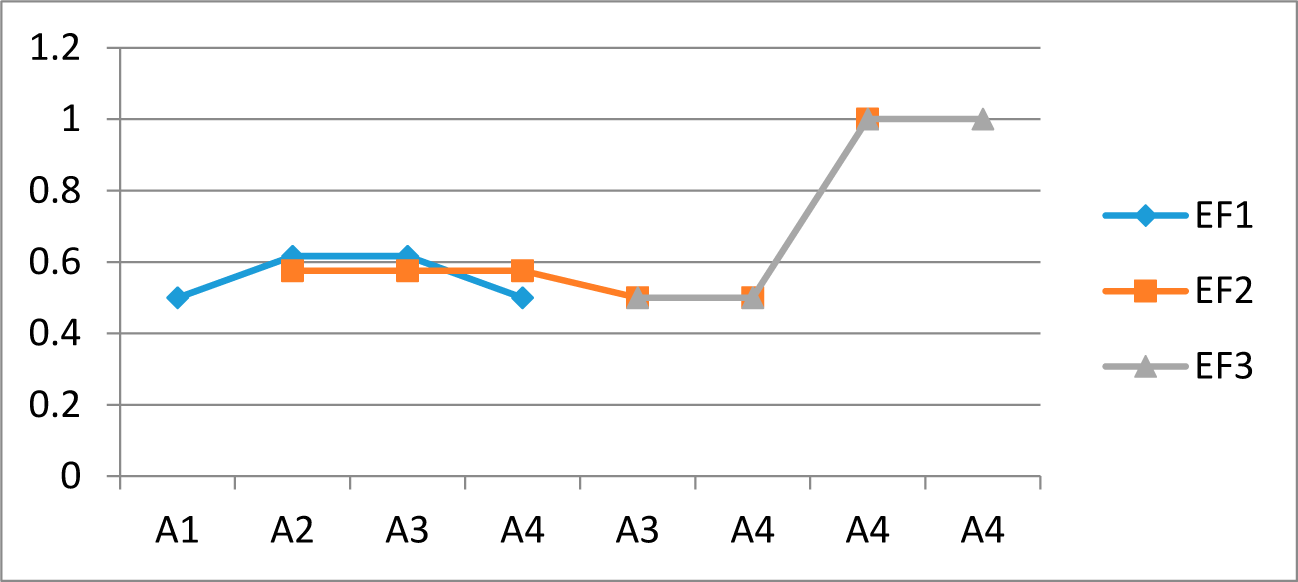
Using the collaborative calculation principle from the House of Quality analysis model, this paper evaluated hospital management effectively, rationally analyzed the synergies between the multi-level medical institutions and the medical work and also more efficiently reflected the hospital management synergy between the various elements using a cooperative and collaborative degree concept.
The analyses for the overall coordination degree and collaboration efficiency of each hospital management element was consistent with the detailed analysis of the results between the various elements, indicating that the quality of the housing cooperative evaluation model evaluation results had a better consistency, but also reflected the higher effectiveness of the collaborative entropy principle compared to traditional qualitative analysis, thereby providing a more persuasive evaluation for the performance of hospital management collaborative research.
In this paper, the synergy entropy and House of Quality principle was used to investigate hospital management collaborative performance. This paper transformed traditional qualitative analysis into quantitative values, and compared the importance parameters for all medical institution levels and medical work stages with the entropy results, allowing for an improved calculation of the overall coordination and synergistic efficiency of the various elements. The use of the triangular fuzzy function reduced the subjective influence of the evaluation process to some extent. However, some subjectivity still exists, so the evaluation process still has room for improvement. Therefore, further improvement in the accuracy of hospital collaboration performance evaluation and the development of a stronger synergy entropy and House of Quality analysis model are key directions for the future.