J. Clin. Med. 2022, 11(7), 2020; https://doi.org/10.3390/jcm11072020 - 4 Apr 2022
Cited by 11 | Viewed by 9971
Abstract
Since the prevalence of heart failure (HF) increases with age, HF is now one of the most common reasons for the hospitalization of elderly people. Although the treatment strategies and overall outcomes of HF patients have improved over time, hospitalization and mortality rates
[...] Read more.
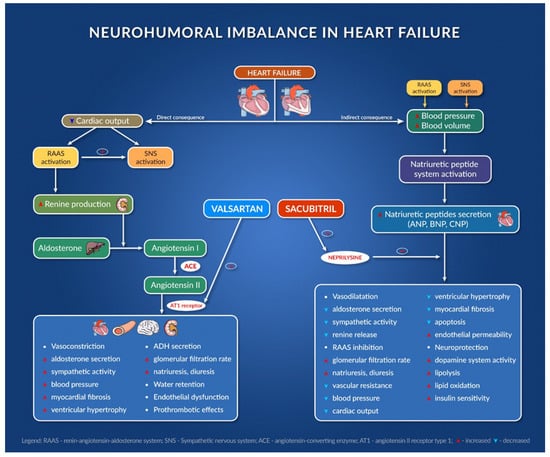
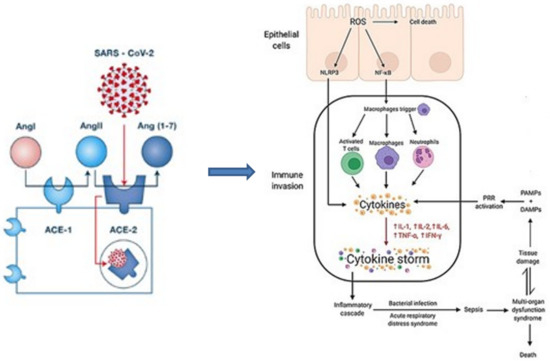
Since the prevalence of heart failure (HF) increases with age, HF is now one of the most common reasons for the hospitalization of elderly people. Although the treatment strategies and overall outcomes of HF patients have improved over time, hospitalization and mortality rates remain elevated, especially in developed countries where populations are aging. Therefore, this paper is intended to be a valuable multidisciplinary source of information for both doctors (cardiologists and general physicians) and pharmacists in order to decrease the morbidity and mortality of heart failure patients. We address several aspects regarding pharmacological treatment (including new approaches in HF treatment strategies [sacubitril/valsartan combination and sodium glucose co-transporter-2 inhibitors]), as well as the particularities of patients (age-induced changes and sex differences) and treatment (pharmacokinetic and pharmacodynamic changes in drugs; cardiorenal syndrome). The article also highlights several drugs and food supplements that may worsen the prognosis of HF patients and discusses some potential drug–drug interactions, their consequences and recommendations for health care providers, as well as the risks of adverse drug reactions and treatment discontinuation, as an interdisciplinary approach to treatment is essential for HF patients.
Full article
(This article belongs to the Special Issue Advances in the Management of Cardiovascular Disease)
►
Show Figures