A Mobile Phone Based Method to Assess Energy and Food Intake in Young Children: A Validation Study against the Doubly Labelled Water Method and 24 h Dietary Recalls
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Total Energy Expenditure
2.3. Tool for Energy Balance in Children (TECH)
2.4. The 24 h Dietary Recalls
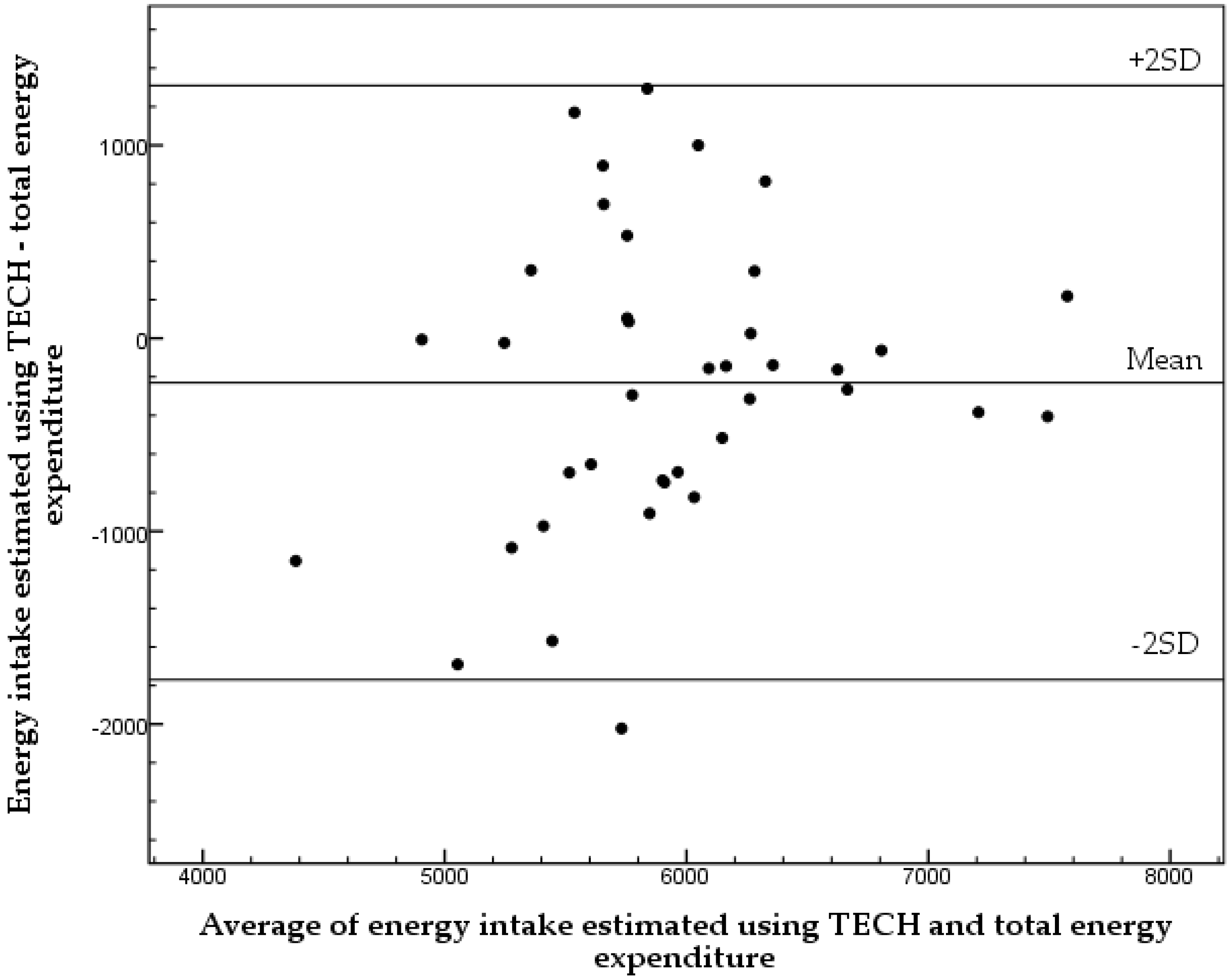
2.5. Statistical Analysis
2.6. Power Considerations and Dimensions of the Study
3. Results
| TECH 1,2 | 24 h Recall 3 | ||||
|---|---|---|---|---|---|
| Food Group | Intake 4 (g/Day) | Range (g/Day) | Intake 4 (g/Day) | Range (g/Day) | p 5 |
| Fruit | 103 ± 65 | 0–251 | 110 ± 76 | 0–293 | 0.307 |
| Vegetables | 64 ± 49 | 0–223 | 67 ± 52 | 0–196 | 0.255 |
| Fruit & Vegetables 6 | 230 ± 138 | 8–594 | 227 ± 148 | 0–782 | 0.655 |
| Fruit Juice | 56 ± 73 | 0–313 | 46 ± 89 | 0–488 | 0.087 |
| Sweetened Beverages | 77 ± 93 | 0–533 | 90 ± 93 | 0–467 | 0.161 |
| Candy | 19 ± 22 | 0–87 | 15 ± 16 | 0–63 | 0.290 |
| Ice Cream | 12 ± 19 | 0–75 | 11 ± 15 | 0–53 | 0.728 |
| Bakery Products | 19 ± 14 | 0–63 | 18 ± 16 | 0–59 | 0.369 |
| Food Group | ρ 1 | p |
|---|---|---|
| Fruit | 0.874 | <0.001 |
| Vegetables | 0.871 | <0.001 |
| Fruit & Vegetables | 0.896 | <0.001 |
| Fruit Juice | 0.665 | <0.001 |
| Sweetened Beverages | 0.711 | <0.001 |
| Candy | 0.744 | <0.001 |
| Ice Cream | 0.753 | <0.001 |
| Bakery Products | 0.786 | <0.001 |
4. Discussion
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| DLW | Double labelled water |
| EI | Energy intake |
| MINISTOP | Mobile-based intervention intended to stop obesity in preschoolers |
| TECH | Tool for energy balance in children |
| TEE | Total energy expenditure |
References
- World Health Association. Facts and Figures on Childhood Obesity. Available online: http://www.who.int/end-childhood-obesity/facts/en/ (assessed on 28 October 2015).
- Sanders, R.H.; Han, A.; Baker, J.S.; Cobley, S. Childhood obesity and its physical and psychological co-morbidities: A systematic review of australian children and adolescents. Eur. J. Pediatr. 2015, 174, 715–746. [Google Scholar] [CrossRef] [PubMed]
- Nader, P.R.; O‘Brien, M.; Houts, R.; Bradley, R.; Belsky, J.; Crosnoe, R.; Friedman, S.; Mei, Z.; Susman, E.J.; National Institute of Child Health and Human Development Early Child Care Research Network. Identifying risk for obesity in early childhood. Pediatrics 2006, 118, e594–e601. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J.; Bonataki, M.; Leary, S.D.; Wells, J.C.; Davey-Smith, G.; Emmett, P.; Steer, C.; Ness, A.R.; Sherriff, A. Progression from childhood overweight to adolescent obesity in a large contemporary cohort. Int. J. Pediatr. Obes. 2011, 6, e138–e143. [Google Scholar] [CrossRef] [PubMed]
- Bond, M.; Wyatt, K.; Lloyd, J.; Taylor, R. Systematic review of the effectiveness of weight management schemes for the under fives. Obes. Rev. 2011, 12, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Delisle, C.; Sandin, S.; Forsum, E.; Henriksson, H.; Trolle-Lagerros, Y.; Larsson, C.; Maddison, R.; Ortega, F.B.; Ruiz, J.R.; Silfvernagel, K.; et al. A web- and mobile phone-based intervention to prevent obesity in 4-year-olds (MINISTOP): A population-based randomized controlled trial. BMC Public Health 2015, 15, 95. [Google Scholar] [CrossRef] [PubMed]
- Manios, Y. The “ToyBox-study” obesity prevention programme in early childhood: An introduction. Obes. Rev. 2012, 13, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Sobko, T.; Svensson, V.; Ek, A.; Ekstedt, M.; Karlsson, H.; Johansson, E.; Cao, Y.; Hagstromer, M.; Marcus, C. A randomised controlled trial for overweight and obese parents to prevent childhood obesity—Early STOPP (Stockholm Obesity Prevention Program). BMC Public Health 2011, 11, 336. [Google Scholar] [CrossRef] [PubMed]
- Onnerfalt, J.; Erlandsson, L.K.; Orban, K.; Broberg, M.; Helgason, C.; Thorngren-Jerneck, K. A family-based intervention targeting parents of preschool children with overweight and obesity: Conceptual framework and study design of loops- lund overweight and obesity preschool study. BMC Public Health 2012, 12, 879. [Google Scholar] [CrossRef] [PubMed]
- Doring, N.; Hansson, L.M.; Andersson, E.S.; Bohman, B.; Westin, M.; Magnusson, M.; Larsson, C.; Sundblom, E.; Willmer, M.; Blennow, M.; et al. Primary prevention of childhood obesity through counselling sessions at swedish child health centres: Design, methods and baseline sample characteristics of the primrose cluster-randomised trial. BMC Public Health 2014, 14, 335. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.L.; Martin, R.J.; Collins, C.E. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J. Am. Diet. Assoc. 2010, 110, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- Stumbo, P.J. New technology in dietary assessment: A review of digital methods in improving food record accuracy. Proc. Nutr. Soc. 2013, 72, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Sharp, D.B.; Allman-Farinelli, M. Feasibility and validity of mobile phones to assess dietary intake. Nutrition 2014, 30, 1257–1266. [Google Scholar] [CrossRef] [PubMed]
- Gemming, L.; Utter, J.; Ni Mhurchu, C. Image-assisted dietary assessment: A systematic review of the evidence. J. Acad. Nutr. Diet. 2015, 115, 64–77. [Google Scholar] [CrossRef] [PubMed]
- Rollo, M.E.; Ash, S.; Lyons-Wall, P.; Russell, A.W. Evaluation of a mobile phone image-based dietary assessment method in adults with type 2 diabetes. Nutrients 2015, 7, 4897–4910. [Google Scholar] [CrossRef] [PubMed]
- Henriksson, H.; Bonn, S.E.; Bergstrom, A.; Balter, K.; Balter, O.; Delisle, C.; Forsum, E.; Lof, M. A new mobile phone-based tool for assessing energy and certain food intakes in young children: A validation study. JMIR Mhealth Uhealth 2015, 3, e38. [Google Scholar] [CrossRef] [PubMed]
- Cadenas-Sanchez, C.; Nystrom, C.D.; Sanchez-Delgado, G.; Martinez-Tellez, B.; Mora-Gonzalez, J.; Risinger, A.S.; Ruiz, J.R.; Ortega, F.B.; Lof, M. Prevalence of overweight/obesity and fitness level in preschool children from the north compared with the south of Europe: An exploration with two countries. Pediatr. Obes. 2015. [Google Scholar] [CrossRef] [PubMed]
- Schoeller, D.A. Validation of habitual energy intake. Public Health Nutr. 2002, 5, 883–888. [Google Scholar] [CrossRef] [PubMed]
- Slinde, F.; Ellegård, L.-E.; Grönberg, A.; Larsson, S.; Rossander-Hulthen, L. Total energy expenditure in underweight patients with severe chronic obstructive pulmonary disease living at home. Clin. Nutr. 2003, 22, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Davies, P.S.; Coward, W.A.; Gregory, J.; White, A.; Mills, A. Total energy expenditure and energy intake in the pre-school child: A comparison. Br. J. Nutr. 1994, 72, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, B.; Prentice, A.; Coward, W.A.; Strain, J.; Black, A.; Davies, P.; Stewart, C.; McKenna, P.; Whitehead, R. Validation of estimates of energy intake by weighed dietary record and diet history in children and adolescents. Am. J. Clin. Nutr. 1992, 56, 29–35. [Google Scholar] [PubMed]
- Weir, J. New methods for calculating metabolic rate with special reference to protein metabolism. J. Physiol. 1949, 109, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Black, A.; Prentice, A.; Coward, W. Use of food quotients to predict respiratory quotients for the doubly-labelled water method of measuring energy expenditure. Hum. Nutr. Clin. Nutr. 1986, 40, 381–391. [Google Scholar] [PubMed]
- National Food Administration. Weights for Foods and Dishes; National Food Administration: Uppsala, Sweden, 1992. [Google Scholar]
- National Food Administration. 2014 Swedish Food Database. Available online: http://www.slv.se (assessed on 1 July 2015).
- Gibson, R.S. Principles of Nutrition Assessment, 2nd ed.; Oxford University Press: New York, NY, USA, 2005; pp. 41–44. [Google Scholar]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.E.; Burrows, T.L.; Truby, H.; Morgan, P.J.; Wright, I.M.; Davies, P.S.; Callister, R. Comparison of energy intake in toddlers assessed by food frequency questionnaire and total energy expenditure measured by the doubly labeled water method. J. Acad. Nutr. Diet. 2013, 113, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J.; Montgomery, C.; Jackson, D.; MacRitchie, J.; Armstrong, J. Energy intake by multiple pass 24 h recall and total energy expenditure: A comparison in a representative sample of 3–4-year-olds. Br. J. Nutr. 2001, 86, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Bornhorst, C.; Bel-Serrat, S.; Pigeot, I.; Huybrechts, I.; Ottavaere, C.; Sioen, I.; de Henauw, S.; Mouratidou, T.; Mesana, M.I.; Westerterp, K.; et al. Validity of 24-h recalls in (pre-)school aged children: Comparison of proxy-reported energy intakes with measured energy expenditure. Clin. Nutr. 2014, 33, 79–84. [Google Scholar] [CrossRef] [PubMed]
- O‘Connor, J.; Ball, E.J.; Steinbeck, K.S.; Davies, P.S.; Wishart, C.; Gaskin, K.J.; Baur, L.A. Comparison of total energy expenditure and energy intake in children aged 6–9 years. Am. J. Clin. Nutr. 2001, 74, 643–649. [Google Scholar] [PubMed]
- Kaskoun, M.C.; Johnson, R.K.; Goran, M.I. Comparison of energy intake by semiquantitative food-frequency questionnaire with total energy expenditure by the doubly labeled water method in young children. Am. J. Clin. Nutr. 1994, 60, 43–47. [Google Scholar] [PubMed]
- Flood, V.M.; Wen, L.M.; Hardy, L.L.; Rissel, C.; Simpson, J.M.; Baur, L.A. Reliability and validity of a short FFQ for assessing the dietary habits of 2–5-year-old children, Sydney, Australia. Public Health Nutr. 2014, 17, 498–509. [Google Scholar] [CrossRef] [PubMed]
- Vereecken, C.; Covents, M.; Huybrechts, I.; Kelly, C.; Maes, L. Changes in children’s food group intake from age 3 to 7 years: Comparison of a FFQ with an online food record. Br. J. Nutr. 2014, 112, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Bel-Serrat, S.; Mouratidou, T.; Pala, V.; Huybrechts, I.; Bornhorst, C.; Fernandez-Alvira, J.M.; Hadjigeorgiou, C.; Eiben, G.; Hebestreit, A.; Lissner, L.; et al. Relative validity of the children’s eating habits questionnaire-food frequency section among young European children: The idefics study. Public Health Nutr. 2014, 17, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Hill, R.J.; Davies, P.S. The validity of self-reported energy intake as determined using the doubly labelled water technique. Br. J. Nutr. 2001, 85, 415–430. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Heymsfield, S.B.; Kemnitz, J.W.; Klein, S.; Schoeller, D.A.; Speakman, J.R. Energy balance and its components: Implications for body weight regulation. Am. J. Clin. Nutr. 2012, 95, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Svensson, A.; Larsson, C.; Eiben, G.; Lanfer, A.; Pala, V.; Hebestreit, A.; Huybrechts, I.; Fernandez-Alvira, J.M.; Russo, P.; Koni, A.C.; et al. European children’s sugar intake on weekdays versus weekends: The idefics study. Eur. J. Clin. Nutr. 2014, 68, 822–828. [Google Scholar] [CrossRef] [PubMed]
- Sepp, H.; Lennernas, M.; Pettersson, R.; Abrahamsson, L. Children’s nutrient intake at preschool and at home. Acta Paediatr. 2001, 90, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Garemo, M.; Lenner, R.A.; Strandvik, B. Swedish pre-school children eat too much junk food and sucrose. Acta Paediatr. 2007, 96, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Fomon, S.J.; Haschke, F.; Ziegler, E.E.; Nelson, S.E. Body composition of reference children from birth to age 10 years. Am. J. Clin. Nutr. 1982, 35, 1169–1175. [Google Scholar] [PubMed]
- Roberts, S.B.; Young, V.R. Energy costs of fat and protein deposition in the human infant. Am. J. Clin. Nutr. 1988, 48, 951–955. [Google Scholar] [PubMed]
- Coward, W.A.; Cole, T.J. The double labeled water method for the measurement of energy expenditure in humans: Risks and benefits. In New Techniques in Nutritional Research, 9th ed.; Whitehead, R.G., Prentice, A., Eds.; Academic Press, Inc.: San Diego, CA, USA, 1991; Volume 9, pp. 139–176. [Google Scholar]
- Speakman, J.R. Doubly Labelled Water. Theory and Practice, 1st ed.; Chapman & Hall: London, UK, 1997. [Google Scholar]
- Reilly, J.J.; Kelly, L.A.; Montgomery, C.; Jackson, D.M.; Slater, C.; Grant, S.; Paton, J.Y. Validation of actigraph accelerometer estimates of total energy expenditure in young children. Int. J. Pediatr. Obes. 2006, 1, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Wikland, K.A.; Luo, Z.C.; Niklasson, A.; Karlberg, J. Swedish population-based longitudinal reference values from birth to 18 years of age for height, weight and head circumference. Acta Paediatr. 2002, 91, 739–754. [Google Scholar] [CrossRef] [PubMed]
- Public Health Agency of Sweden. 2014 Overweight and Besity National Statistics. Available online: http://www.folkhalsomyndigheten.se/ (assessed on 2 November 2015).
- Statistics Sweden. 2014 Educational Attainment of the Population. Available online: http://www.scb.se/ (assessed on 2 November 2015).
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delisle Nyström, C.; Forsum, E.; Henriksson, H.; Trolle-Lagerros, Y.; Larsson, C.; Maddison, R.; Timpka, T.; Löf, M. A Mobile Phone Based Method to Assess Energy and Food Intake in Young Children: A Validation Study against the Doubly Labelled Water Method and 24 h Dietary Recalls. Nutrients 2016, 8, 50. https://doi.org/10.3390/nu8010050
Delisle Nyström C, Forsum E, Henriksson H, Trolle-Lagerros Y, Larsson C, Maddison R, Timpka T, Löf M. A Mobile Phone Based Method to Assess Energy and Food Intake in Young Children: A Validation Study against the Doubly Labelled Water Method and 24 h Dietary Recalls. Nutrients. 2016; 8(1):50. https://doi.org/10.3390/nu8010050
Chicago/Turabian StyleDelisle Nyström, Christine, Elisabet Forsum, Hanna Henriksson, Ylva Trolle-Lagerros, Christel Larsson, Ralph Maddison, Toomas Timpka, and Marie Löf. 2016. "A Mobile Phone Based Method to Assess Energy and Food Intake in Young Children: A Validation Study against the Doubly Labelled Water Method and 24 h Dietary Recalls" Nutrients 8, no. 1: 50. https://doi.org/10.3390/nu8010050
APA StyleDelisle Nyström, C., Forsum, E., Henriksson, H., Trolle-Lagerros, Y., Larsson, C., Maddison, R., Timpka, T., & Löf, M. (2016). A Mobile Phone Based Method to Assess Energy and Food Intake in Young Children: A Validation Study against the Doubly Labelled Water Method and 24 h Dietary Recalls. Nutrients, 8(1), 50. https://doi.org/10.3390/nu8010050






