Pharmacokinetics and Toxicity of Sodium Selenite in the Treatment of Patients with Carcinoma in a Phase I Clinical Trial: The SECAR Study
Abstract
:1. Introduction
2. Experimental Section
2.1. Patient Eligibility
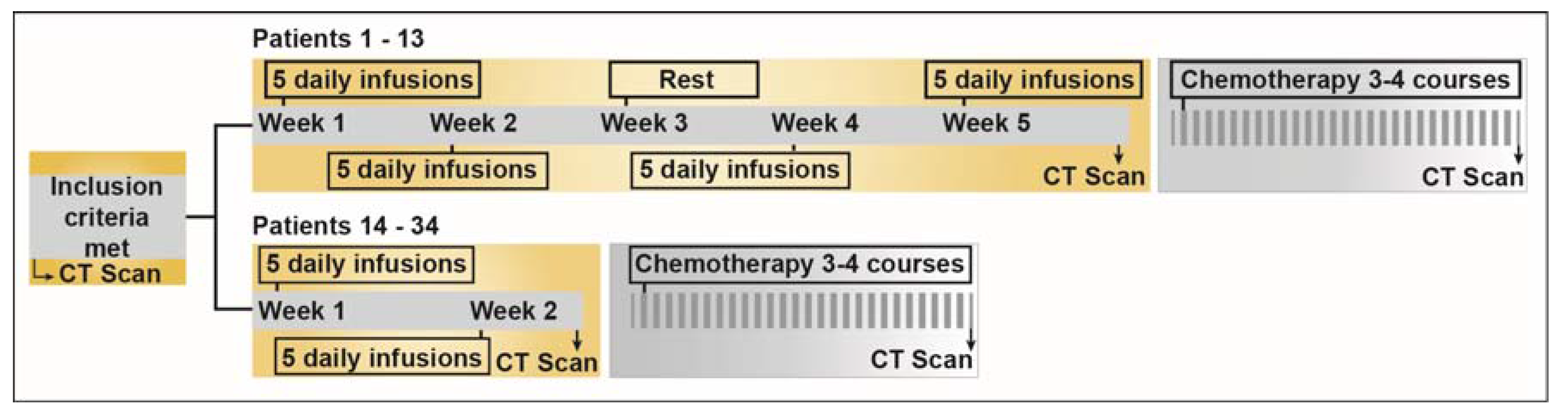
2.2. Study Design
| Cohort No. | No. of Patients | Daily Dose (mg/m2) | Treatment Schedule | Total Median dose (mg); (range) |
|---|---|---|---|---|
| 1 | 3 | 0.5 | OPD; 5 d/week; 4 weeks | 18.0 (17.5–18.0) |
| 2 | 3 | 1.0 | OPD; 5 d/week; 4 weeks | 36.8 (34.0–42.0) |
| 3 | 3 | 1.5 | OPD; 5 d/week; 4 weeks | 60.0 (50.0–62.0) |
| 4 | 4 | 2.0 | OPD; 5 d/week; 4 weeks | 72.5 (66.5–92.0) |
| Protocol amendment; 50% dose escalation in subsequent cohorts | ||||
| 5 | 4 | 3.0 | OPD; 5 d/week; 2 weeks | 49.0 (28.8–57.5) |
| 6 | 3 | 4.5 | OPD; 5 d/week; 2 weeks | 74.0 (62.0–98.0) |
| 7 | 3 | 6.8 | OPD; 5 d/week; 2 weeks | 117.0 (115.0–131.0) |
| 8 | 3 | 10.2 | OPD; 5 d/week; 2 weeks | 214.0 (176.0–225.0) |
| 9 | 6 | 15.3 | OPD; 5 d/week; 2 weeks | 77.7 (58.0–326.0) |
| 10 | 2 | 12.8 | OPD; 5 d/week; 2 weeks | 159.8 (107.6–212.0) |
2.3. Drug, Dose Escalation Design and Infusion Schedule
2.4. Toxicity Assessment
2.5. Chemotherapy
2.6. Pharmacokinetic Evaluation
2.6.1. Blood Sampling and Selenium Analysis
2.6.2. Pharmacokinetic Analyses
2.6.3. Statistical Analyses
3. Results
3.1. Patients
3.2. Dose Escalation, Toxicity and MTD
| Characteristic | Patients (N = 34) | |
|---|---|---|
| No. | % | |
| Age, Years | ||
| Mean | 59.7 | |
| SD | 11 | |
| Median | 61.5 | |
| Range | 37–79 | |
| Sex | ||
| Male | 19 | 56 |
| Female | 15 | 44 |
| WHO performance status | ||
| 0 | 9 | 26.5 |
| 1 | 19 | 55.9 |
| 2 | 6 | 17.6 |
| Primary tumor types | ||
| Non-small cell lung carcinoma | 21 | 61.8 |
| Small-cell lung carcinoma | 3 | 8.8 |
| Colon cancer | 4 | 11.8 |
| Rectal cancer | 2 | 5.9 |
| Malignant mesothelioma | 1 | 2.9 |
| Ethmoidal cancer | 1 | 2.9 |
| Tongue base cancer | 1 | 2.9 |
| Testicular teratoma | 1 | 2.9 |
| Stages | ||
| Stage I | 0 | 0 |
| Stage II | 0 | 0 |
| Stage III | 7 | 20.6 |
| Stage IV | 27 | 79.4 |
| Refractory to first line therapy | 34 | 100 |
| Preferred Terms | Grades 1–2 | Grades 3–4 | Any Grade | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Alopecia | 2 | 6 | 0 | 0 | 2 | 6 |
| Anorexia | 3 | 9 | 0 | 0 | 3 | 9 |
| Anxiousness | 0 | 0 | 1 | 3 | 1 | 3 |
| Arthralgia | 2 | 6 | 0 | 0 | 2 | 6 |
| Chest pain | 1 | 3 | 0 | 0 | 1 | 3 |
| Confusion | 0 | 0 | 1 | 3 | 1 | 3 |
| Cramps in legs and/or finger | 6 | 18 | 0 | 0 | 6 | 18 |
| Dyspnea | 2 | 6 | 1 | 3 | 3 | 9 |
| ECG change | 0 | 0 | 1 | 3 | 1 | 3 |
| Fatigue | 16 | 47 | 2 | 6 | 18 | 53 |
| Garlic smell of breath | 5 | 15 | 0 | 0 | 5 | 15 |
| Gastritis | 1 | 3 | 0 | 0 | 1 | 3 |
| Hallucination | 0 | 0 | 1 | 3 | 1 | 3 |
| Hot Flush | 1 | 3 | 0 | 0 | 1 | 3 |
| Nausea | 12 | 35 | 1 | 3 | 13 | 38 |
| Pain at infusion site | 2 | 6 | 0 | 0 | 2 | 6 |
| Peripheral sensory and motor neuropathy | 1 | 3 | 0 | 0 | 1 | 3 |
| Pressure on thorax | 0 | 0 | 1 | 3 | 1 | 3 |
| Pruritus legs | 1 | 3 | 0 | 0 | 1 | 3 |
| Stomach pain | 1 | 3 | 0 | 0 | 1 | 3 |
| Stomach swelling | 1 | 3 | 0 | 0 | 1 | 3 |
| Thrombopenia | 1 | 3 | 0 | 0 | 1 | 3 |
| Unconsciousness | 0 | 0 | 1 | 3 | 1 | 3 |
| Vertigo | 1 | 3 | 0 | 0 | 1 | 3 |
| Vomiting | 7 | 21 | 0 | 0 | 7 | 21 |

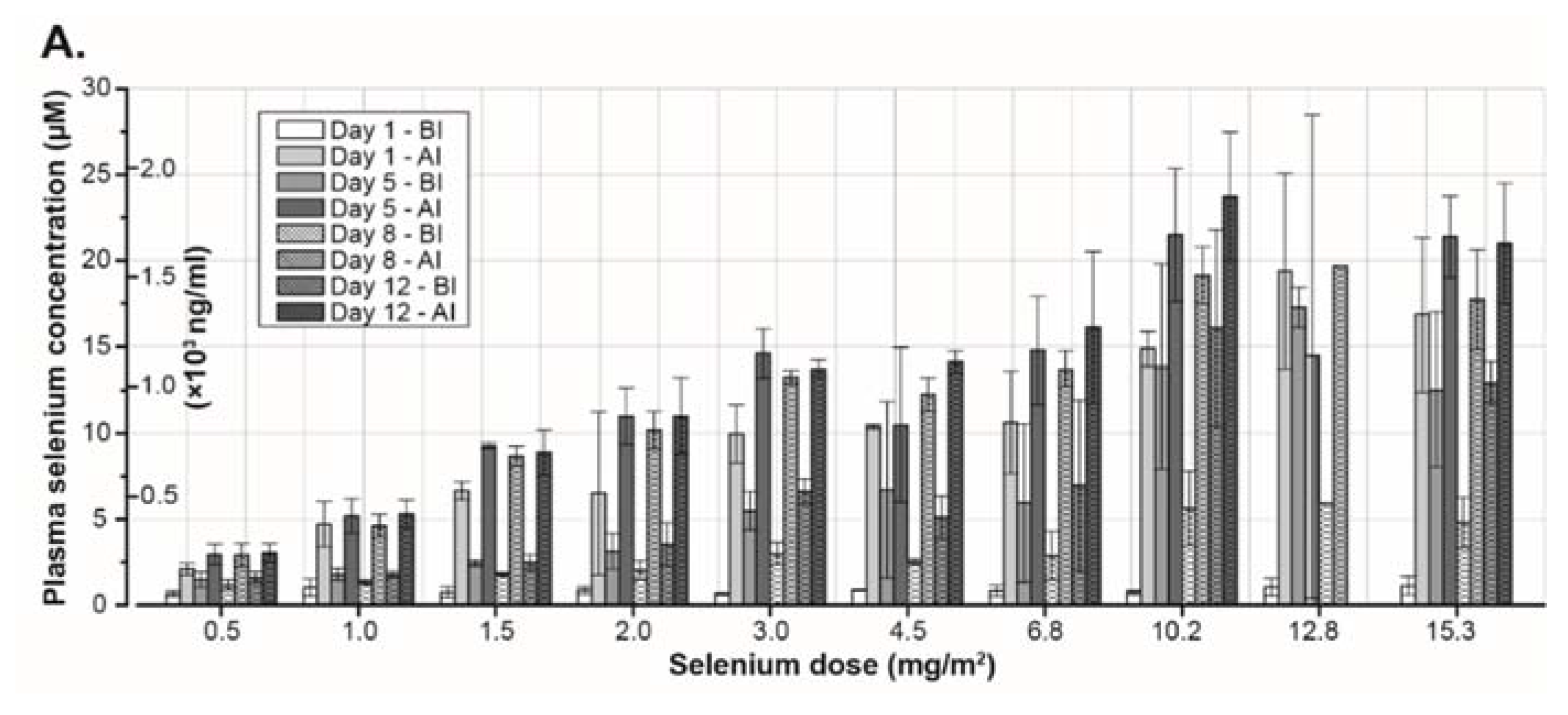

3.3. Pharmacokinetics
3.4. Clinical Assessment

4. Discussion
5. Conclusions
Supplementary Files
Supplementary File 1Acknowledgments
Author Contributions
Conflicts of Interest
References
- Yan, L.; Spallholz, J.E. Generation of reactive oxygen species from the reaction of selenium compounds with thiols and mammary tumor cells. Biochem. Pharmacol. 1993, 45, 429–437. [Google Scholar] [PubMed]
- Gorrini, C.; Harris, I.S.; Mak, T.W. Modulation of oxidative stress as an anticancer strategy. Nat. Rev. Drug Discov. 2013, 12, 931–947. [Google Scholar] [CrossRef] [PubMed]
- Trachootham, D.; Alexandre, J.; Huang, P. Targeting cancer cells by ros-mediated mechanisms: A radical therapeutic approach? Nat. Rev. Drug. Discov. 2009, 8, 579–591. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Yang, Y.; Huang, F.; Li, F.; Jiang, Q.; Shi, K.; Xu, C. Selenite induces apoptosis in colorectal cancer cells via akt-mediated inhibition of β-catenin survival axis. Cancer Lett. 2012, 315, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Q.; Wang, Y.; Li, T.; Shi, K.; Li, Z.; Ma, Y.; Li, F.; Luo, H.; Yang, Y.; Xu, C. Heat shock protein 90–mediated inactivation of nuclear factor-κb switches autophagy to apoptosis through becn1 transcriptional inhibition in selenite-induced nb4 cells. Mol. Biol. Cell 2011, 22, 1167–1180. [Google Scholar] [CrossRef] [PubMed]
- Hoefig, C.S.; Renko, K.; Köhrle, J.; Birringer, M.; Schomburg, L. Comparison of different selenocompounds with respect to nutritional value vs. Toxicity using liver cells in culture. J. Nutr. Biochem. 2011, 22, 945–955. [Google Scholar] [CrossRef] [PubMed]
- Wallenberg, M.; Misra, S.; Wasik, A.M.; Marzano, C.; Bjornstedt, M.; Gandin, V.; Fernandes, A.P. Selenium induces a multi-targeted cell death process in addition to ros formation. J. Cell Mol. Med. 2014, 18, 671–684. [Google Scholar] [CrossRef] [PubMed]
- Fico, M.E.; Poirier, K.A.; Watrach, A.M.; Watrach, M.A.; Milner, J.A. Differential effects of selenium on normal and neoplastic canine mammary cells. Cancer Res. 1986, 46, 3384–3388. [Google Scholar] [PubMed]
- Watrach, A.M.; Milner, J.A.; Watrach, M.A.; Poirier, K.A. Inhibition of human breast cancer cells by selenium. Cancer Lett. 1984, 25, 41–47. [Google Scholar] [CrossRef]
- Nilsonne, G.; Sun, X.; Nystrom, C.; Rundlof, A.K.; Fernandes, A.P.; Bjornstedt, M.; Dobra, K. Selenite induces apoptosis in sarcomatoid malignant mesothelioma cells through oxidative stress. Free Radical. Biol. Med. 2006, 41, 874–885. [Google Scholar] [CrossRef] [PubMed]
- Caffrey, P.B.; Frenkel, G.D. The development of drug resistance by tumor cells in vitro is accompanied by the development of sensitivity to selenite. Cancer Lett. 1994, 81, 59–65. [Google Scholar] [CrossRef]
- Caffrey, P.B.; Frenkel, G.D. Selenite cytotoxicity in drug resistant and non-resistant human ovarian tumor cells. Cancer Res. 1992, 52, 4812–4816. [Google Scholar] [PubMed]
- Björkhem-Bergman, L.; Jönsson, K.; Eriksson, L.C.; Olsson, J.M.; Lehmann, S.; Paul, C.; Björnstedt, M. Drug-resistant human lung cancer cells are more sensitive to selenium cytotoxicity. Effects on thioredoxin reductase and glutathione reductase. Biochem. Pharmacol. 2002, 63, 1875–1884. [Google Scholar] [CrossRef]
- Caffrey, P.B.; Frenkel, G.D. Sensitivity of melphalan-resistant tumors to selenite in vivo. Cancer Lett. 1997, 121, 177–180. [Google Scholar] [CrossRef]
- Milner, J.A. Effect of selenium on virally induced and transplantable tumor models. Fed. Proc. 1985, 44, 2568–2572. [Google Scholar] [PubMed]
- Ip, C.; Medina, D. Current concepts of selenium and mammary tumorigenesis. In Cellular and Molecular Biology of Mammary Cancer; Medina, D., Kidwell, W., Heppner, G., Anderson, E., Eds.; Springer US: New York, NY, USA, 1987; pp. 479–494. [Google Scholar]
- Milner, J.A. Selenium and the transplantable tumor. J. Agric. Food Chem. 1984, 32, 436–442. [Google Scholar] [CrossRef]
- Novoselov, S.V.; Calvisi, D.F.; Labunskyy, V.M.; Factor, V.M.; Carlson, B.A.; Fomenko, D.E.; Moustafa, M.E.; Hatfield, D.L.; Gladyshev, V.N. Selenoprotein deficiency and high levels of selenium compounds can effectively inhibit hepatocarcinogenesis in transgenic mice. Oncogene 2005, 24, 8003–8011. [Google Scholar] [CrossRef] [PubMed]
- Watson-Williams, E. A preliminary note on the treatment of inoperable carcinoma with selenium. Br. Med. J. 1919, 2, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Todd, A.T. The selenide treatment of cancer. Br. J. Surg. 1934, 21, 619–631. [Google Scholar] [CrossRef]
- Manzanares, W.; Biestro, A.; Torre, M.H.; Galusso, F.; Facchin, G.; Hardy, G. High-dose selenium reduces ventilator-associated pneumonia and illness severity in critically ill patients with systemic inflammation. Intensive Care Med. 2011, 37, 1120–1127. [Google Scholar] [CrossRef] [PubMed]
- Forceville, X.; Laviolle, B.; Annane, D.; Vitoux, D.; Bleichner, G.; Korach, J.M.; Cantais, E.; Georges, H.; Soubirou, J.L.; Combes, A.; et al. Effects of high doses of selenium, as sodium selenite, in septic shock: A placebo-controlled, randomized, double-blind, phase ii study. Crit Care 2007, 11, R73. [Google Scholar] [CrossRef] [PubMed]
- Mosteller, R.D. Simplified calculation of body-surface area. N. Engl. J. Med. 1987, 317, 1098. [Google Scholar] [PubMed]
- Olm, E.; Fernandes, A.P.; Hebert, C.; Rundlöf, A.-K.; Larsen, E.H.; Danielsson, O.; Björnstedt, M. Extracellular thiol-assisted selenium uptake dependent on the xc− cystine transporter explains the cancer-specific cytotoxicity of selenite. Proc. Natl. Acad. Sci. USA 2009, 106, 11400–11405. [Google Scholar] [CrossRef] [PubMed]
- Turan, B.; Koc, E.; Hotomaroglu, O.; Kiziltan, E.; Yildirim, S.; Demirel, E. Tissue and concentration-dependent effects of sodium selenite on muscle contraction. Biol. Trace Elem. Res. 1998, 62, 265–280. [Google Scholar] [CrossRef] [PubMed]
- Caffrey, P.B.; Frenkel, G.D. Prevention of carboplatin-induced resistance in human ovarian tumor xenografts by selenite. Anticancer Res. 2013, 33, 4249–4254. [Google Scholar] [PubMed]
- De Haas, E.C.; di Pietro, A.; Simpson, K.L.; Meijer, C.; Suurmeijer, A.J.H.; Lancashire, L.J.; Cummings, J.; de Jong, S.; de Vries, E.G.E.; Dive, C.; et al. Clinical evaluation of m30 and m65 elisa cell death assays as circulating biomarkers in a drug-sensitive tumor, testicular cancer. Neoplasia 2008, 10, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brodin, O.; Eksborg, S.; Wallenberg, M.; Asker-Hagelberg, C.; Larsen, E.H.; Mohlkert, D.; Lenneby-Helleday, C.; Jacobsson, H.; Linder, S.; Misra, S.; et al. Pharmacokinetics and Toxicity of Sodium Selenite in the Treatment of Patients with Carcinoma in a Phase I Clinical Trial: The SECAR Study. Nutrients 2015, 7, 4978-4994. https://doi.org/10.3390/nu7064978
Brodin O, Eksborg S, Wallenberg M, Asker-Hagelberg C, Larsen EH, Mohlkert D, Lenneby-Helleday C, Jacobsson H, Linder S, Misra S, et al. Pharmacokinetics and Toxicity of Sodium Selenite in the Treatment of Patients with Carcinoma in a Phase I Clinical Trial: The SECAR Study. Nutrients. 2015; 7(6):4978-4994. https://doi.org/10.3390/nu7064978
Chicago/Turabian StyleBrodin, Ola, Staffan Eksborg, Marita Wallenberg, Charlotte Asker-Hagelberg, Erik H. Larsen, Dag Mohlkert, Clara Lenneby-Helleday, Hans Jacobsson, Stig Linder, Sougat Misra, and et al. 2015. "Pharmacokinetics and Toxicity of Sodium Selenite in the Treatment of Patients with Carcinoma in a Phase I Clinical Trial: The SECAR Study" Nutrients 7, no. 6: 4978-4994. https://doi.org/10.3390/nu7064978