A Systematic Literature Review of Efficiency Measurement in Nursing Homes
Abstract
:1. Introduction
- Which methods have been used to measure productivity and efficiency of nursing homes?
- How did these studies measure quantities and prices of inputs and outputs, and how did they account for the different characteristics of nursing home operations?
- Did these studies adjust for quality of care and/or quality of life (of the residents)? If they did, how was quality measured? Did they appropriately reflect the outputs that a nursing home aims to produce?
2. Methods
2.1. Search Strategies
2.2. Study Selection
2.3. Data Extraction
3. Results
3.1. Summary of Included Studies
3.2. Estimation Methods and Model Specifications
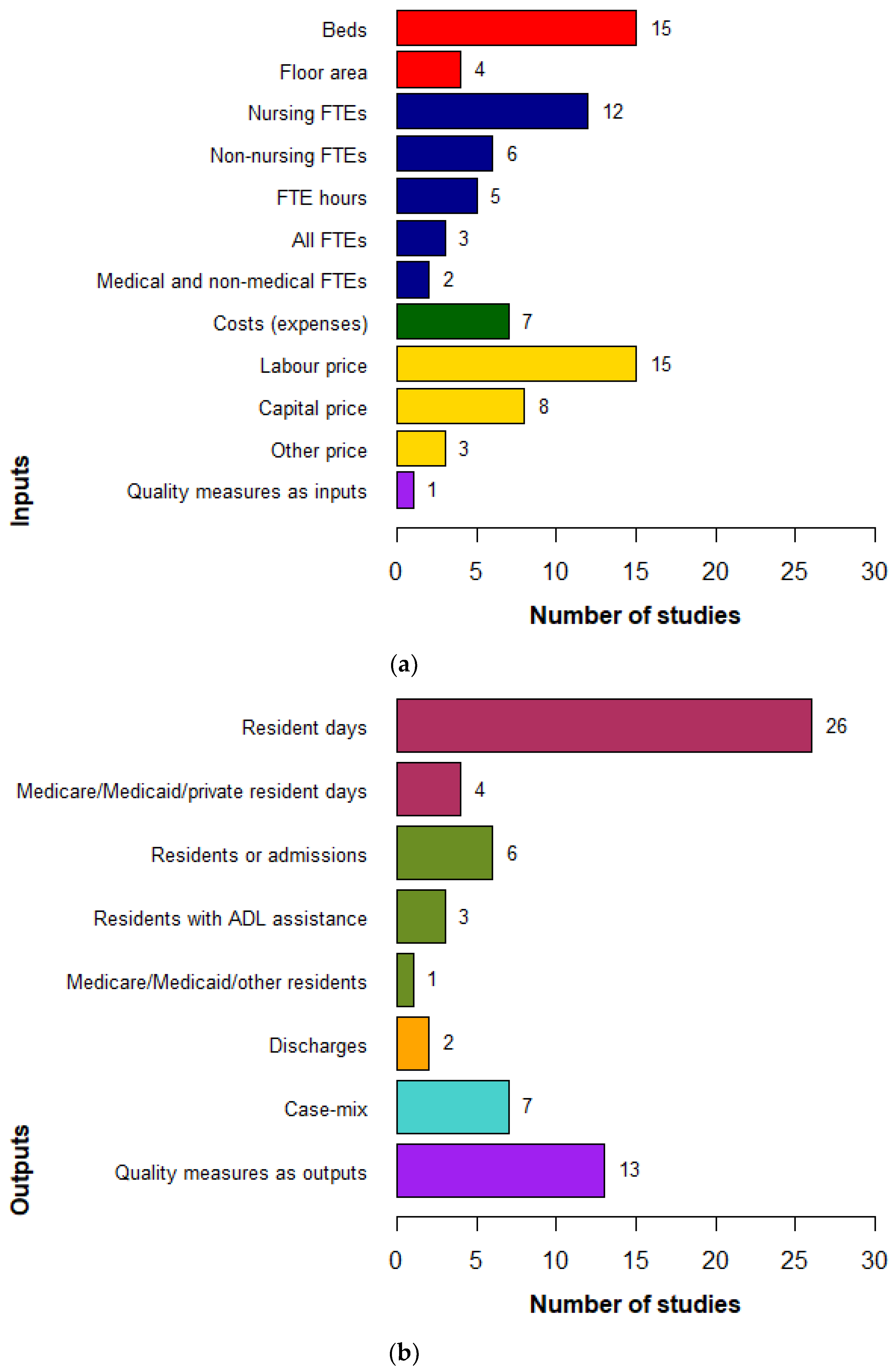
3.3. Input and Output Measures
3.4. Control Variables
3.5. Quality Measures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organisation. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Dulal, R. Technical efficiency of nursing homes: Do five-star quality ratings matter? Health Care Manag. Sci. 2018, 21, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Szczepura, A. Residential and nursing homes: How can they meet the challenge of an aging population? Aging Health 2011, 7, 877–887. [Google Scholar] [CrossRef]
- Australia Productivity Commission. Caring for Older Australians: Productivity Commission Inquiry Report; Productivity Commission: Canberra, Australia, 2011.
- Vaarama, M.; Pieper, R.; Sixsmith, A. Care-Related Quality of Life in Old Age: Concepts, Models, and Empirical Findings; Vaarama, M., Pieper, R., Sixsmith, A., Eds.; Springer Science + Business Media: New York, NY, USA, 2008. [Google Scholar]
- Jacobs, R.; Smith, P.C.; Street, A. Measuring Efficiency in Health Care: Analytic Techniques and Health Policy; Cambridge University Press: Cambridge, UK, 2006. [Google Scholar]
- Coelli, T.; Rao, D.S.P.; O’Donnell, C.J.; Battese, G.E. An Introduction to Efficiency and Productivity Analysis; Springer: Boston, MA, USA, 2005. [Google Scholar]
- O’Donnell, C.J. Productivity and Efficiency Analysis: An Economic Approach to Measuring and Explaining Managerial Performance; Springer: Singapore, 2018. [Google Scholar]
- Nguyen, K.-H.; Coelli, T. Quantifying the Effects of Modelling Choices on Hospital Efficiency Measures: A Meta-Regression Analysis. The University of Queensland School of Economics. Available online: https://espace.library.uq.edu.au/view/UQ:369501 (accessed on 26 March 2019).
- WHO Regional Office for Europe. Health System Efficiency: How to Make Measurement Matter for Policy and Management; Cylus, J., Papanicolas, I., Smith, P.C., Eds.; WHO Regional Office for Europe: Copenhagen, Denmark, 2016. [Google Scholar]
- Donabedian, A. The Quality of Care: How Can It Be Assessed? JAMA 1988, 260, 743–748. [Google Scholar] [CrossRef]
- Donabedian, A. An Introduction to Quality Assurance in Health Care; Oxford University Press: Oxford, UK, 2003. [Google Scholar]
- Ayanian, J.Z.; Markel, H. Donabedian’s Lasting Framework for Health Care Quality. N. Engl. J. Med. 2016, 375, 205–207. [Google Scholar] [CrossRef] [PubMed]
- Quality of Care Amendment (Single Quality Framework) Principles 2018 (AU). Available online: https://www.legislation.gov.au/Details/F2018L01412/Download (accessed on 20 June 2019).
- Bowling, A.; Iliffe, S. Psychological approach to successful ageing predicts future quality of life in older adults. Health Qual. Life Outcomes 2011, 9, 13. [Google Scholar] [CrossRef] [PubMed]
- Bryant, C.; Bei, B.; Gilson, K.; Komiti, A.; Jackson, H.; Judd, F. The relationship between attitudes to aging and physical and mental health in older adults. Int. Psychogeriatr. Camb. 2012, 24, 674–683. [Google Scholar] [CrossRef]
- Carstensen, L.L.; Turan, B.; Scheibe, S.; Ram, N.; Ersner-Hershfield, H.; Samanez-Larkin, G.R.; Brooks, K.P.; Nesselroade, J.R. Emotional experience improves with age: Evidence based on over 10 years of experience sampling. Psychol. Aging 2010, 26, 21. [Google Scholar] [CrossRef]
- Hung, L.-W.; Kempen, G.I.J.M.; De Vries, N.K. Cross-cultural comparison between academic and lay views of healthy ageing: A literature review. Ageing Soc. 2010, 30, 1373–1391. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, 2535. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Ray, S.C. Technical, scale, and size efficiency in nursing home care: A nonparametric analysis of Connecticut homes. Health Econ. 1996, 5, 363–373. [Google Scholar] [CrossRef]
- Di Giorgio, L.; Filippini, M.; Masiero, G. Structural and managerial cost differences in nonprofit nursing homes. Econ. Model. 2015, 51, 289–298. [Google Scholar] [CrossRef] [Green Version]
- Farsi, M.; Filippini, M.; Kuenzle, M. Unobserved heterogeneity in stochastic cost frontier models: An application to Swiss nursing homes. Appl. Econ. 2005, 37, 2127–2141. [Google Scholar] [CrossRef]
- Farsi, M.; Filippini, M.; Lunati, D. Economies of Scale and Efficiency Measurement in Switzerland’s Nursing Homes. Swiss J. Econ. Stat. 2008, 144, 359–378. [Google Scholar] [CrossRef]
- Wang, Y.H.; Chou, L.F. The Efficiency of Nursing Homes in Taiwan: An Empirical Study Using Data Envelopment Analysis. Fu Jen Manag. Rev. 2005, 12, 167–194. [Google Scholar]
- Chang, S.-J.; Cheng, M.-A. The impact of nursing quality on nursing home efficiency: Evidence from Taiwan. Rev. Acc. Financ. 2013, 12, 369–386. [Google Scholar] [CrossRef]
- Chen, L.W.; Shea, D.G. The economies of scale for nursing home care. Med. Care Res. Rev. 2004, 61, 38–63. [Google Scholar] [CrossRef] [PubMed]
- DeLellis, N.O.; Ozcan, Y.A. Quality outcomes among efficient and inefficient nursing homes: A national study. Health Care Manag. Rev. 2013, 38, 156–165. [Google Scholar] [CrossRef]
- Dulal, R. Cost efficiency of nursing homes: Do five-star quality ratings matter? Health Care Manag. Sci. 2016, 20, 316–325. [Google Scholar] [CrossRef]
- Hsu, A.T.-M. An Investigation of Approaches to Performance Measurement: Applications to Long-Term Care in Ontario. Ph.D. Thesis, University of Toronto, Toronto, ON, Canada, 2015. [Google Scholar]
- Knox, K.J.; Blankmeyer, E.C.; Stutzman, J.R. Organizational Efficiency and Quality in Texas Nursing Facilities. Health Care Manag. Sci. 2003, 6, 175–188. [Google Scholar] [CrossRef]
- Knox, K.J.; Blankmeyer, E.C.; Stutzman, J.R. Comparative Performance and Quality among Nonprofit Nursing Facilities in Texas. Nonprofit. Volunt. Sect. Q. 2006, 35, 631–667. [Google Scholar] [CrossRef]
- Laine, J.; Linna, M.; Hakkinen, U.; Noro, A. Measuring the Productive Efficiency and Clinical Quality of Institutional Long-Term Care for the Elderly. Health Econ. 2005, 14, 245–256. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-R.; Chen, C.-Y.; Peng, T.-K. Study of the Relevance of the Quality of Care, Operating Efficiency and Inefficient Quality Competition of Senior Care Facilities. Int. J Environ. Res. Public Health 2017, 14, 1047. [Google Scholar] [CrossRef]
- Min, A.; Park, C.G.; Scott, L.D. Evaluating Technical Efficiency of Nursing Care Using Data Envelopment Analysis and Multilevel Modeling. West. J. Nurs. Res. 2016, 38, 1489–1508. [Google Scholar] [CrossRef]
- Rosko, M.D.P.; Chilingerian, J.A.P.; Zinn, J.S.P.; Aaronson, W.E.P. The Effects of Ownership, Operating Environment, and Strategic Choices on Nursing Home Efficiency. Med. Care 1995, 33, 1001–1021. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.J.; Unruh, L.; Wan, T.T.H. Has the Medicare prospective payment system led to increased nursing home efficiency? Health Serv. Res. 2008, 43, 1043–1061. [Google Scholar] [CrossRef] [PubMed]
- Knox, K.J.; Blankmeyer, E.C.; Stutzman, J.R. Technical Efficiency in Texas Nursing Facilities: A Stochastic Production Frontier Approach. J. Econ. Financ. 2007, 31, 75–86. [Google Scholar] [CrossRef]
- Crivelli, L.; Filippini, M.; Lunati, D. Regulation, ownership and efficiency in the Swiss nursing home industry. Int. J. Health Care Financ. Econ. 2002, 2, 79–97. [Google Scholar] [CrossRef]
- Farsi, M.; Filippini, M. An Empirical Analysis of Cost Efficiency in Non-profit and Public Nursing Homes. Ann. Public Coop. Econ. 2004, 75, 339–365. [Google Scholar] [CrossRef] [Green Version]
- Björkgren, M.A.; Fries, B.E.; Häkkinen, U.; Brommels, M. Case-mix adjustment and efficiency measurement. Scand. J. Public Health 2004, 32, 464–471. [Google Scholar] [CrossRef]
- Bjorkgren, M.A.; Hakkinen, U.; Linna, M. Measuring Efficiency of Long-Term Care Units in Finland. Health Care Manag. Sci. 2001, 4, 193–200. [Google Scholar] [CrossRef]
- Laine, J.; Finne-Soveri, U.H.; Björkgren, M.; Linna, M.; Noro, A.; Häkkinen, U. The association between quality of care and technical efficiency in long-term care. Int. J. Qual. Health Care 2005, 17, 259–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laine, J.; Linna, M.; Noro, A.; Hakkinen, U. The Cost Efficiency and Clinical Quality of Institutional Long-Term Care for the Elderly. Health Care Manag. Sci. 2005, 8, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Dervaux, B.; Leleu, H.; Nogues, H.; Valdmanis, V. Assessing French nursing home efficiency: An indirect approach via budget-constrained DEA models. Socio-Econ. Plan. Sci. 2006, 40, 70–91. [Google Scholar] [CrossRef]
- Shimshak, D.G. Managing Nursing Home Quality Using Dea with Weight Restrictions. In Applications in Multicriteria Decision Making, Data Envelopment Analysis, and Finance; Lawrence, K.D., Kleinman, G., Eds.; Emerald Group Publishing Limited: Bingley, UK, 2010; pp. 199–216. [Google Scholar]
- Shimshak, D.G.; Lenard, M.L. A Two-Model Approach to Measuring Operating and Quality Efficiency with DEA. Inf. Syst. Oper. Res. 2007, 45, 143–151. [Google Scholar] [CrossRef]
- Shimshak, D.; Lenard, M.; Klimberg, R. Incorporating quality into data envelopment analysis of nursing home performance: A case study. Omega 2009, 37, 672–685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozcan, Y.A.; Wogen, S.E.; Mau, L.W. Efficiency Evaluation of Skilled Nursing Facilities. J. Med. Syst. 1998, 22, 211–224. [Google Scholar] [CrossRef] [PubMed]
- Knox, K.J.; Blankmeyer, E.C.; Stutzman, J.R. Relative economic efficiency in Texas nursing facilities: A profit function analysis. J. Econ. Financ. 1999, 23, 199–213. [Google Scholar] [CrossRef]
- Anderson, R.I.; Lewis, D.; Webb, J.R. The efficiency of nursing home chains and the implications of non-profit status. J. Real Estate Portf. Manag. 1999, 5, 235–245. [Google Scholar]
- Garavaglia, G.; Lettieri, E.; Agasisti, T.; Lopez, S. Efficiency and Quality of Care in Nursing Homes: An Italian Case Study. Health Care Manag. Sci. 2011, 14, 22–35. [Google Scholar] [CrossRef]
- Luasa, S.N.; Dineen, D.; Zieba, M. Technical and scale efficiency in public and private Irish nursing homes—A bootstrap DEA approach. Health Care Manag. Sci. 2018, 21, 326–347. [Google Scholar] [CrossRef]
- Dormont, B.; Martin, C. Quality of service and cost-efficiency of French nursing homes. In Proceedings of the 9th European Conference on Health Economics, Zurich, Switzerland, 18–21 July 2012; p. 21. [Google Scholar]
- Duffy, J.A.M.; Fitzsimmons, J.A.; Jain, N. Identifying and studying “best-performing” services. Benchmarking 2006, 13, 232–251. [Google Scholar] [CrossRef]
- Filippini, M. Economies of scale in the Swiss nursing home industry. Appl. Econ. Lett. 2001, 8, 43–46. [Google Scholar] [CrossRef]
- Department of Health. 2017-18 Report on the Operation of the Aged Care Act 1997; Department of Health: Canberra, Australia, 2018.
- Linna, M.; Häkkinen, U.; Magnussen, J. Comparing hospital cost efficiency between Norway and Finland. Health Policy 2006, 77, 268–278. [Google Scholar] [CrossRef] [PubMed]
- Medin, E.; Häkkinen, U.; Linna, M.; Anthun, K.S.; Kittelsen, S.A.C.; Rehnberg, C. International hospital productivity comparison: Experiences from the Nordic countries. Health Policy 2013, 112, 80–87. [Google Scholar] [CrossRef]
- Giancotti, M.; Guglielmo, A.; Mauro, M. Efficiency and optimal size of hospitals: Results of a systematic search. PLoS ONE 2017, 12, e0174533. [Google Scholar] [CrossRef] [PubMed]
- Leleu, H.; Al-Amin, M.; Rosko, M.; Valdmanis, V.G. A robust analysis of hospital efficiency and factors affecting variability. Health Serv. Manag. Res. 2018, 31, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-H.; Park, J.; Lim, S.; Park, S.-C. Has Competition Increased Hospital Technical Efficiency? Health Care Manag. 2015, 34, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Rosko, M.; Wong, H.S.; Mutter, R. Characteristics of High-and Low-Efficiency Hospitals. Med. Care Res. Rev. 2018, 75, 454–478. [Google Scholar] [CrossRef]
- Narcı, H.Ö.; Ozcan, Y.A.; Şahin, İ.; Tarcan, M.; Narcı, M. An examination of competition and efficiency for hospital industry in Turkey. Health Care Manag. Sci. 2015, 18, 407–418. [Google Scholar] [CrossRef]
- Anderson, R.I.; Weeks, H.S.; Hobbs, B.K.; Webb, J.R. Nursing home quality, chain affiliation, profit status and performance. J. Real Estate Res. 2003, 25, 43–60. [Google Scholar]
- Frijters, D.H.; Van Der Roest, H.G.; Carpenter, I.G.; Finne-Soveri, H.; Henrard, J.-C.; Chetrit, A.; Gindin, J.; Bernabei, R. The calculation of quality indicators for long term care facilities in 8 countries (SHELTER project). BMC Health Serv. Res. 2013, 13, 138. [Google Scholar] [CrossRef] [PubMed]
- Oliver-Baxter, J.; Brown, L.; Dawda, P. Should the healthcare compass in Australia point towards value-based primary healthcare? Aust. Health Rev. 2017, 41, 98. [Google Scholar] [CrossRef] [PubMed]
- Netten, A.; Burge, P.; Malley, J.; Potoglou, D.; Towers, A.; Brazier, J.; Flynn, T.; Forder, J.; Wall, B. Outcomes of social care for adults: developing a preference weighted measure. Health Technol. Assess. 2012, 16. [Google Scholar] [CrossRef] [PubMed]
- Netten, A.; Trukeschitz, B.; Beadle-Brown, J.; Forder, J.; Towers, A.-M.; Welch, E. Quality of life outcomes for residents and quality ratings of care homes: Is there a relationship? Age Ageing 2012, 41, 512–517. [Google Scholar] [CrossRef] [PubMed]
- interRAI. [QOL-LTCF] Interrai Self-Reported Quality of Life Survey for Long-Term Care Facilities (Nursing Homes) (QOL-LTCF) Interviewer Version-License to Print interRAI Catalog. 2009. Available online: https://catalog.interrai.org/QOL-LTCF-Self-Reported-Quality-of-Life-Survey-for-Long-Term-Care-Facilities-Interviewer-Version-PIY (accessed on 24 February 2019).
- interRAI. [QOL] interRAI Self-Reported Quality of Life (QOL) Surveys and User’s Manual, 9.3|interRAI Catalog. Available online: https://catalog.interrai.org/QOL-Quality-of-Life-Manual (accessed on 24 February 2019).
- Power, M.; Quinn, K.; Schmidt, S. WHOQOL-OLD Group. Development of the WHOQOL-Old Module. Qual. Life Res. 2005, 14, 2197–2214. [Google Scholar] [CrossRef] [PubMed]
- Ageing and Aged Care. Quality Indicators in Residential Aged Care; Department of Health: Canberra, Australia, 2019.
- Centers for Medicare & Medicaid Services. Design for Nursing Home Compare Five-Star Quality Rating System: Technical Users’ Guide; Centers for Medicare & Medicaid Services: Baltimore, MD, USA, 2019.
- interRAI, TAS. Definitions-interRAI Quality Indicators. Available online: https://www.interrai.co.nz/assets/Data/Quality-Indicators/Quality-Indicators-Definitions.pdf (accessed on 10 January 2019).

| DEA (22/39) | SFA (12/39) | Others (7/39) | Total (39/39) | |||||
|---|---|---|---|---|---|---|---|---|
| Number of stages(sum up to 100%) | ||||||||
| 1 stage | 32% | (7/22) | 67% | (8/12) | 57% | (4/7) | 43% | (17/39) |
| 2 stages | 64% | (14 /22) | 33% | (4/12) | 14% | (1/7) | 49% | (19/39) |
| 3 stages | 4% | (01/22) | 0% | (0/12) | 29% | (2/7) | 8% | (3/39) |
| Return to scale(not sum up to 100%) | ||||||||
| CRS | 68% | (15/22) | 17% | (2/12) | 0% | (0/7) | 44% | (17/39) |
| VRS | 59% | (13/22) | 83% | (10/12) | 100% | (7/7) | 72% | (28/39) |
| N/A | 0% | (0/22) | 0% | (0/12) | 0% | (0/7) | 0% | (0/39) |
| Orientation(not sum up to 100%) | ||||||||
| ITE | 86% | (19/22) | 83% | (10/12) | 71% | (5/7) | 85% | (33/39) |
| OTE | 5% | (1/22) | 0% | (0/12) | 0% | (0/7) | 3% | (1/39) |
| Profit orientation | 5% | (1/22) | 0% | (0/12) | 43% | (3/7) | 10% | (4/39) |
| N/A | 5% | (1/22) | 17% | (2/12) | 14% | (1/7) | 8% | (3/39) |
| Frontier(sum up to 100%) | ||||||||
| Cost frontier | 4% | (1/22) | 75% | (9/12) | 72% | (5/7) | 36% | (14/39) |
| Production frontier | 32% | (7/22) | 25% | (3/12) | 14% | (1/7) | 26% | (10/39) |
| Others | 64% | (14/22) | 0% | (0/22) | 14% | (1/7) | 38% | (15/39) |
| Input | Output | Control |
|---|---|---|
| Physical capital: No. of beds: 38% (15/39) Floor area: 10% (4/39) Human capital: Nursing FTEs: 31% (12/39) Non-nursing FTEs: 15% (6/39) Medical and non-medical FTEs: 5% (2/39) FTE hours: 13% (5/39) All FTEs: 8% (3/39) Input price: Labour price: 38% (15/39) Capital price: 21% (8/39) Other price: 8% (3/39) Other resource expenses: 18% (7/39) Quality measures: 3% (1/39) Outcome: 3% (1/39) (% non-ambulatory residents; % ambulatory and self-feeding residents) | Residential services produced: (Un)adjusted resident days: 67% (26/39) Medicare/Medicaid/private resident days: 10% (4/39) Residents or admissions: 15% (6/39) Medicare/Medicaid/other residents: 3% (1/39) Discharges: 5% (2/39) Casemix: 15% (6/39) Consequence of receiving the services: Residents with ADL assistance: 8% (3/39) Quality measures: 33% (13/39) Structure: 15% (6/39) Process: 3% (1/39) Outcome: 31% (12/39) | Structural characteristics: Ownership: 26% (10/39) For-profit status: 31% (12/39) Chain affiliation: 28% (11/39) Supervision: 3% (1/39) Medicare (Medicaid) admissions: 15% (6/39) Reimbursement per resident: 3% (1/39) Beds: 18% (7/39) Occupancy rate: 26% (10/39) Facility type: 23% (9/39) Ward’s specification: 5% (2/39) Others: 10% (4/39) Environmental factors: Location or urban/rural: 26% (10/39) HHI index: 15% (6/39) No. of agencies in area: 3% (1/39) Area average income: 8% (3/39) Wage index: 3% (1/39) % population aged 84+: 3% (1/39) County occupancy rate: 3% (1/39) Other control factors: Reimbursement (dummy): 8% (3/39) Policy change: 10% (4/39) Time trend: 28% (11/39) CM - age: 5% (2/39); discharge rate: 3% (1/39); - acuity/ADL index: 21% (8/39); others: 5% (2/39) Quality measures: 51% (20/39) Structure: 38% (15/39) Process: 0% (0/39) Outcome: 23% (9/39) |
| Impact on Efficiency | Approach 1 | Approach 2a | Approach 2b | |
|---|---|---|---|---|
| Facility characteristics | ||||
| For-profit | Positive (n = 9) | [30,35,37,49] | [28] | [2,34,36,50] |
| Negative (n = 2) | [29] | [27] | ||
| Private-owned | Positive (n = 3) | [25,36,51] | ||
| Negative (n = 3) | [29] | [27,52] | ||
| Mixed impacts depends on models (n = 2) | [31] | [53] | ||
| Insignificant or no impact (n = 3) | [21,38] | [24] | ||
| Chain affiliation | Positive (n = 3) | [49] | [34,36] | |
| Negative (n = 2) | [28] | [50] | ||
| Mixed impacts depends on models (n = 3) | [30,31] | [36] | ||
| Insignificant or no impact (n = 3) | [29] | [2,27] | ||
| Occupancy rate | Positive (n = 8) | [30,31] | [24,25,32,34,35,48] | |
| Negative (n = 1) | [33] | |||
| Mixed impacts depends on models (n = 1) | [36] | |||
| Size (number of beds) | Positive (n = 5) | [29] | [34,35,36,52] | |
| Negative (n = 1) | [24] | |||
| Insignificant or no impact (n = 1) | [51] | |||
| Environmental factors | ||||
| Competition (measured by HHI index) | Positive (n = 2) | [27,36] | ||
| Insignificant or no impact (n = 3) | [29,35] | [24] | ||
| Urban | Positive (n = 3) | [29,30,31] | ||
| Mixed impacts depends on models (n = 2) | [53] | [52] | ||
| Insignificant or no impact (n = 2) | [49] | [48] | ||
| Structure (19/39) | Process (1/39) | Outcome (20/39) | |
|---|---|---|---|
| Inputs (1/39) | 1. % Non-ambulatory: 3% (1/39) 2. % resident not self-feeding: 3% (1/39) (These patient conditions as quality measures incorporated as inputs in Duffy et al.’s study [54] to reflect opportunity for patient co-production) | ||
| Outputs (13/39) | 1. Rating for health inspection (deficiencies): 10% (4/39) 2. FTEs contributing to QOC (e.g., RN) per resident: 3% (1/39) 3. FTEs contributing to QOL (e.g., activity professionals and staff) per resident (used as QOL measure): 3% (1/39) 4. Administrative service performance: 3% (1/39) 5. Life care performance: 3% (1/39) 6. Health care performance: 3% (1/39) 7. Extra nursing hours: 3% (1/39) | 1. Degree of involvement in the provision of organized groups for its residents and their families QOL (used as QOL index): 3% (1/39) | 1. % ADL decline: 8% (3/39) 2. % pressure ulcers: 21% (8/39) 3. % restraints: 18% (7/39) 4. % UTI: 8% (3/39) 5. % depression without treatment: 3% (1/39) 6. % pain: 8% (3/39) 7. % (no) falls: 10% (4/39) 8. Catheterisation: 15% (6/39) 9. % drug error: 3% (1/39) 10. Accident rate (or emergencies): 5% (2/39) 11. Out-of-pocket charges (as residential satisfaction—Willing to pay): 3% (1/39) |
| Control variables (20/39) | 1. Staffing (RN hours/total nursing hours perresident day): 8% (3/39) 2. Nursing staff ratio (Nurses employed/nurses that should be employed according to the guidelines): 10% (4/39) 3. High quality facility (Care person per resident): 8% (3/39) 4. Nursing home rating: 8% (3/39) 5. Qualification of medical staff: 5% (2/39) 6. % RNs: 3% (1/39) 7. % rooms with own toilet: 3% (1/39) 8. % single rooms: 3% (1/39) 9. Average assistance time: 3% (1/39) | 1. ADL severity level: 13% (5/39) 2. Acuity index: 3% (1/39) 3. Pressure sores: 10% (4/39) 4. Catheterisations: 8% (3/39) 5. Restraints: 10% (4/39) 6. Bedfast: 5% (2/39) 7. Unplanned weight change: 5% (2/39) 8. Depression: 8% (3/39) 9. Antipsychotic, anti-anxiety/hypnotic use: 8% (3/39) 10. Behavioural symptoms: 3% (1/39) 11. Cognitive impairment: 3% (1/39) 12. % use ≥ 9 medications: 3% (1/39) 13. Bowel incontinence: 3% (1/39) 14. Bladder incontinence: 3% (1/39) 15. % UTI: 3% (1/39) 16. % injury, fall, fracture: 3% (1/39) 17. Pneumococcal vaccination: 3% (1/39) 18. Influenza vaccination: 3% (1/39) 19. On pain management: 3% (1/39) 20. Adjusted mortality rate: 3% (1/39) |
| No. | Quality Measures | Approach 1 | Approach 2a | Approach 2b | ||
|---|---|---|---|---|---|---|
| (10/39) | (2/39) | (8/39) | ||||
| Structure | ||||||
| 1 | Staffing (RN hours/total nursing hours per resident day) | 8% | (3/39) | [23] | [28] | [2] |
| 2 | Nursing staff ratio (Nurses Employed/nurses that should be employed according to the guidelines) | 10% | (4/39) | [21,22,39,55] | ||
| 3 | High quality facility (Care person per resident) | 8% | (3/39) | [23,38] | [53] | |
| 4 | Nursing home rating | 10% | (4/39) | [28,30,31] | [33] | |
| 5 | Qualification of medical staff | 3% | (1/39) | [52], * Not as quality measure [25] | ||
| 6 | % RNs | 3% | (1/39) | [42] | ||
| 7 | % rooms with own toilet | 3% | (1/39) | |||
| 8 | % single rooms | 3% | (1/39) | |||
| 9 | Average assistance time | 3% | (1/39) | [38] | ||
| Outcome | ||||||
| 1 | ADL severity level | 15% | (6/39) | [21,22,39,55] * Not as quality measure [20,26,30,31] | * Not as quality measure [53] | [27,42] * Not as quality measure [34,35] |
| 2 | Acuity index | 3% | (1/39) | [27] | ||
| 3 | Pressure sores | 10% | (4/39) | [27,32,35,42] | ||
| 4 | Catheterisations | 8% | (3/39) | [27,35,42] | ||
| 5 | Restraints | 10% | (4/39) | [27,35,42,43] | ||
| 6 | Bedfast | 5% | (2/39) | [27,42] | ||
| 7 | Unplanned weight change | 5% | (2/39) | [27,42] | ||
| 8 | Depression | 8% | (3/39) | [27,32,42] | ||
| 9 | Antipsychotic, anti-anxiety/hypnotic use | 8% | (3/39) | [32,42,43] | ||
| 10 | Behavioural symptoms | 3% | (1/39) | [42] | ||
| 11 | Cognitive impairment | 3% | (1/39) | [42] | ||
| 12 | % use >= 9 medications | 3% | (1/39) | [42] | ||
| 13 | Bowel incontinence | 5% | (2/39) | [27,42] | ||
| 14 | Bladder incontinence | 3% | (1/39) | [27] | ||
| 15 | % UTI | 3% | (1/39) | [42] | ||
| 16 | % injury, fall, fracture | 3% | (1/39) | [42] | ||
| 17 | Pneumococcal vaccination | 3% | (1/39) | [27] | ||
| 18 | Influenza vaccination | 3% | (1/39) | [27] | ||
| 19 | On pain management | 3% | (1/39) | [27] | ||
| 20 | Adjusted mortality rate | 3% | (1/39) | [29] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, A.; Nguyen, K.-H.; Gray, L.; Comans, T. A Systematic Literature Review of Efficiency Measurement in Nursing Homes. Int. J. Environ. Res. Public Health 2019, 16, 2186. https://doi.org/10.3390/ijerph16122186
Tran A, Nguyen K-H, Gray L, Comans T. A Systematic Literature Review of Efficiency Measurement in Nursing Homes. International Journal of Environmental Research and Public Health. 2019; 16(12):2186. https://doi.org/10.3390/ijerph16122186
Chicago/Turabian StyleTran, Alice, Kim-Huong Nguyen, Len Gray, and Tracy Comans. 2019. "A Systematic Literature Review of Efficiency Measurement in Nursing Homes" International Journal of Environmental Research and Public Health 16, no. 12: 2186. https://doi.org/10.3390/ijerph16122186





