Abstract
Schools are key environments in which physical activity (PA) can be promoted. Various strategies and opportunities should be used to engage children in PA within schools. The aim of this study was to evaluate the effectiveness of the multi-component Active Schools: Skelmersdale (AS:Sk) pilot intervention on children’s PA and sedentary time (ST). The AS:Sk intervention was implemented for eight weeks in four schools with three control schools continuing normal practice. It consisted of eight components: active breaks, bounce at the bell, ‘Born To Move’ videos, Daily Mile or 100 Mile Club, playground activity challenge cards, physical education teacher training, newsletters, and activity homework. Child-level measures were collected at baseline and follow-up, including objectively measured PA. After accounting for confounding variables, the intervention had a significant effect on school day ST which was significantly less for the intervention children by 9 min per day compared to the control group. The AS:Sk pilot intervention was effective in reducing school day ST but significant changes in PA were negligible. To increase the efficacy of the current and future school-based interventions, authors should focus on implementation and process evaluations to better understand how schools are implementing intervention components.
1. Introduction
Children and young people engage in low levels of moderate to vigorous physical activity (MVPA) [1]. Worldwide data revealed 80% of 13–15 year olds do not meet the 60 min of MVPA per day guidelines [2]. Participation in physical activity (PA) during childhood years has a favourable relationship with adiposity, cardiometabolic biomarkers such as cholesterol and blood pressure, physical fitness, and bone health [3]. Psychological outcomes such as self-worth and self-esteem are also positively affected by participation in PA [4,5]. MVPA in particular is most important for health as relationships between health outcomes are most consistent and robust for PA of this higher intensity [3]. Moreover, in addition to low levels of activity, children’s sedentary time (ST) increases during the transition from primary/middle to secondary/high school [6]. Engagement in sedentary behaviours is detrimental to many aspects of health such as body composition, cardiorespiratory fitness (CRF), metabolic syndrome, and cardiovascular disease risk factors [7].
Many barriers can prevent children and young people from engaging in regular PA [8]. As a result, it has been suggested that schools are key environments for PA promotion regardless of the individual circumstances of a child [9]. Recent government recommendations state that half (at least 30 min) of the daily recommendation for MVPA should be accrued during school hours [10,11]. Recommendations for sedentary time are less prescriptive and specific, although efforts to reduce sedentary behaviours and minimise extended periods spent sedentary across the whole day and within schools are advocated [11,12,13,14].
Within comprehensive school PA programmes (CSPAP) [15] the use of a variety of strategies and opportunities is advocated to promote PA within schools, for example during the school day, before and after school, within physical education (PE), and with involvement from staff and family/community [15]. Results from a 2015 meta-analysis indicated that as the number of CSPAP components included in an intervention increased, the effect size associated with change in daily PA also increased [16].
A comprehensive intervention perspective with a focus on multiple-level factors exemplifies a socio-ecological approach [17]. Action Schools! BC (AS! BC) is an ongoing example of an intervention underpinned by the socio-ecological model [18], and which resulted in PA increasing through activities implemented across six different school components named ‘action-zones’ [19]. Literature reviews have further supported this approach to intervention design, stating that interventions targeting different levels of the socioecological model and those that are multi-component in nature can have a positive impact on PA levels [20,21,22,23].
That being said, multi-component interventions are not always successful at increasing PA [24,25]. Multi-component interventions are difficult to put into practice and a lack of implementation, with schools not implementing as intended has previously been reported [24]. More recently, a more pragmatic approach to PA promotion has been proposed which includes the expansion, extension, and enhancement of PA opportunities (theory of expanded, extended, and enhanced opportunities (TEO)) [26]. The use of this approach allows researchers to target various levels within an ecological model but additionally and importantly, identify appropriate targets [26].
The Active Schools: Skelmersdale (AS:Sk) pilot multi-component clustered randomised control trial (RCT) was designed to promote PA across the school day through multiple opportunities which could be integrated into every day school life and implemented by school staff. The aim of this study was to evaluate the impact of the AS:SK intervention on children’s MVPA and ST, and health indicators.
2. Materials and Methods
2.1. Participants
This study is the third phase of the AS:Sk project (ClinicalTrials.gov registration: NCT03283904). Seven primary schools within Skelmersdale, a low-income town, within West Lancashire, UK, participated in the project [27]. Using a sample size calculation that accounted for the pre-determined number of schools, 100 participants (50 per group) were required for a clustered RCT design with seven schools. This calculation was based on AS:Sk study 1 findings and assumed 15 participants per cluster, an intracluster correlation of 0.04, an alpha level of 0.05 and power of 90% [28,29]. Following ethical approval from the University Research Ethics Committee (ref #SPA-REC-2016-342), schools received the relevant paperwork to inform each Year 5 child (n = 239, age 9–10 years) about the study. Passive (“opt-out”) parental consent were obtained in six of the schools, one school chose to use active parental consent, and children completed informed assent forms prior to data collection. This process resulted in 232 participating children (97% recruitment rate).
2.2. Study Design
Following the collection of baseline measurements, schools were randomly assigned to either intervention or control groups by a member of the faculty unconnected to the study. This randomisation was not blinded due to the nature of the intervention. There was a one-week gap between the allocation of groups and the beginning of the intervention period to allow for the teachers to plan and organise intervention components into their future school plans. Control schools were informed via email of their selection and agreed to continue with their usual timetabled amount of playground breaks and PE lessons without any additional time allocated for PA participation. Details of the flow of participants through the study from baseline to follow up are shown in Figure 1.
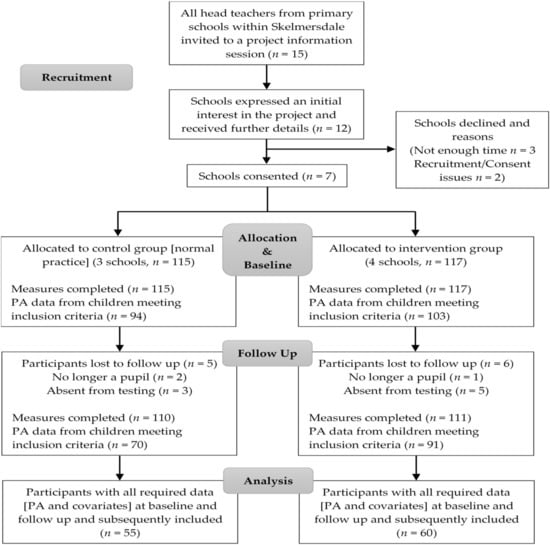
Figure 1.
Flow of schools and participants through the study.
2.3. Intervention
The Consolidated Standards of Reporting Trials (CONSORT) guidelines extension for clustered RCT were followed for reporting the results of the AS:Sk intervention [30]. The intervention duration was eight weeks and it consisted of eight components. These were active breaks (ABs), bounce at the bell, ‘Born To Move’ (BTM) videos, Daily Mile (DM) or 100 Mile Club (MC), playground activity challenge cards, PE teacher training, newsletters, and activity homework. All intervention approaches were designed to have no financial cost to the project or schools to implement. A description of each intervention component with the recommended implementation duration and frequency per school day or week was presented to each participating class teacher who was asked to adhere to this guidance. These details are presented in Table 1. Schools were given the freedom to implement the components during the school day when it best suited their own timetable, whilst adhering to the duration and frequency guidelines. The consultation of relevant school-based intervention literature and findings from phase two of the AS:Sk project which piloted three components (ABs, BTM videos, recess intervention; unpublished data), informed selection of the current components. The components aligned with elements of the socio-ecological model [17], the youth physical activity promotion model (YPAPM) [31], and TEO [26].

Table 1.
Detail of each intervention component.
2.4. Measures
The primary outcome for this study was school day MVPA. The secondary outcomes were achieving 30 min MVPA during the school day, school day ST, whole weekday ST and PA levels, CRF, and body size (BMI z-score). Measurement protocols at baseline and follow up were the same at both time points and took place within the school grounds. Baseline measures were taken in September 2017, with follow up measures taken in November and December 2017.
2.4.1. Physical Activity
Children wore an ActiGraph GT9X triaxial accelerometer (ActiGraph, Pensacola, FL, USA) which were each initialised to record raw accelerations at a frequency of 100 Hz. Children were instructed to wear the accelerometer for seven days at all times (24 h·day−1), except when engaging in water-based activities such as bathing and swimming. Data was downloaded using ActiLife version 6.11.9 (ActiGraph) and saved in raw format as GT3X files. Raw data files were processed in R (http://cran.r-project.org) using GGIR which converted the raw triaxial accelerometer signals into one omnidirectional measure of acceleration termed the Euclidean norm minus one (ENMO; vector magnitude taken from the three axes minus the value of gravity with negative values rounded up to zero) [45,46]. ENMO values were averaged per 1 s epoch over each of the seven monitored days [47]. Accelerometer non-wear was determined using the method of van Hees et al. [45], which has been applied previously in studies involving children [47,48,49]. Published ENMO prediction equations were used to identify cut-points for classifying activity as MVPA (3 metabolic equivalents (METs; child-specific); 201 mg) [50]. As there is no consensus as to the most appropriate ENMO ST cut-points [51], we also applied the Hildebrand et al. [50] regression equations using 1.5 METs, which resulted in values of 50 mg. Minimum wear time to be included in the analysis was set to 10 h for a minimum of three weekdays at both baseline and follow up [52]. The time periods explored in the analyses included the school day (defined by schools as between the time the timetable begins and the time children are dismissed) and also whole week day (defined as 7 am to 10 pm).
2.4.2. Anthropometrics
Stature was assessed to the nearest 0.1 cm using a portable stadiometer (Leicester Height Measure, Seca, Birmingham, UK). Body mass was assessed to the nearest 0.1 kg (813 scales, Seca). Body weight in kilograms divided by height in meters squared gave the body mass index (BMI) of each participant. BMI z-scores were assigned [53] and age and sex specific BMI cut-points established children as normal weight or overweight/obese (those who were underweight were grouped into the normal weight category) [54]. Waist circumference was measured to the nearest 0.1 cm using an anthropometric tape measure, and the percentage of waist circumference-to-height ratio (%WHtR) was calculated as a measure of central adiposity [55]. Gender-specific equations were used to predict children′s age from peak height velocity (APHV), as a proxy measure of biological maturation [56].
2.4.3. Cardiorespiratory Fitness (CRF)
The 20 m multistage shuttle run test was conducted to provide an estimate of CRF [57]. The total number of shuttles completed by each participant was recorded as a proxy measure of CRF. This test has been previously used with children of a similar age to those in the current study [43,58].
2.4.4. Psychological Constructs
A paper questionnaire pack was administered which included eight items measuring PA self-efficacy [59] and 16 items measuring PA enjoyment [60]. All items were scored using a 5-point scale ranging from 1 (“Strongly disagree”) to 5 (“Strongly agree”). These questionnaires have previously demonstrated strong factorial validity [59,60].
2.4.5. Socioeconomic Status (SES)
Neighbourhood-level socioeconomic status (SES) was calculated using the 2015 Indices of Multiple Deprivation (IMD) [61]. The IMD is a UK government-produced deprivation measure for England comprising income, employment, health, education, housing, environment, and crime. IMD rank scores were generated from parent-reported home post codes using the National Statistics Postcode Directory database. Every neighbourhood in England is ranked from one (most deprived area) to 32,844 (least deprived area).
2.5. Statistical Analysis
Descriptive statistics (mean and standard deviations) were calculated for the outcomes of all participants at baseline and follow-up. Multilevel modelling was performed using MLwiN Version 2.36 (Centre for Multilevel Modelling, University of Bristol, UK) [62] to determine the effects of the intervention. Multilevel modelling was appropriate for use in this study given the design of children clustered within the seven participating schools. Therefore, a 2-level data structure was used with children defined as the first level of analysis, and schools as the second level of analysis.
Continuous outcome variables were school day ST, light PA (LPA) and MVPA, whole weekday ST, LPA and MVPA, CRF and BMI z-score. The dichotomous outcome variable studied (thus logistic multilevel analysis) was achieving 30 min MVPA/school day. Regression coefficients for the group variables (‘0’ indicating control schools and ‘1’ indicating intervention schools) reflected between-group differences in the outcome measures (adjusted for baseline values and covariates). Initially, ‘crude’ interaction analyses were conducted with only the grouping variables and the outcome variable at baseline included in the model [63]. Potential confounding covariates were then added to ‘adjusted’ models whilst still controlling for baseline outcome variables. These potential confounding covariates were selected based on previous research which has deemed them to be influential to the outcomes and depending on the outcome, included gender [1,64], SES [65,66], body size [67,68], CRF [69,70], PA self-efficacy [31], PA enjoyment [31], accelerometer wear time, and whole weekday ST and MVPA [68,71,72]. Regression coefficients from the models were assessed for significance using the Wald statistic and the following equation, (regression coefficient/standard error)2. Statistical significance was set at p < 0.05.
The evaluation of potential effect modification was also carried out on several dichotomous covariates (gender, weight status, central obesity risk, and fitness status). These analyses determined whether the intervention effects were different for the subgroups. Interaction terms were added to the models, consisting of a multiplication of the main determinant (intervention) and the potential effect modifier [63]. Due to the reduced power which interaction terms have, statistical significance for this analysis was set at p < 0.1 [63].
3. Results
3.1. Preliminary Results
Descriptive statistics are displayed in Table 2 for all participants and by gender, for baseline and follow up measures.

Table 2.
Descriptive characteristics of participating children (control and intervention, baseline and follow up; mean (standard deviation) where applicable).
3.2. Intervention Effects
Table 3 shows the intervention effects on each outcome. In the adjusted models, time spent engaged in ST during the school day was significantly less for the intervention children compared to the control group (−9.0 min; p = 0.01). There were no intervention effects on any of the remaining outcome measures, although the trends for school day PA and CRF were in a favourable direction. The odds of achieving 30 min of MVPA per school day was 2.79 times higher in the intervention group compared to the control group, however this did not reach significance (p = 0.07).

Table 3.
Multilevel model analyses of the outcome measures.
3.3. Sub-Group Analyses
There were no post-intervention interaction effects in any of the dichotomous variables (sex, weight status, central obesity risk, fitness status) on the outcomes of school day ST and PA, whole day ST and PA, BMI z-score, and CRF.
4. Discussion
This study aimed to (1) assess the impact of the AS:Sk multi-component intervention on the primary outcome of school day MVPA, and (2) assess the impact of the AS:Sk multi-component intervention on the secondary outcomes of achieving 30 min MVPA/school day, school day ST, whole weekday ST and PA levels, CRF and body size. Overall, after accounting for confounding variables, the intervention had a significant effect on school day ST which was significantly less for the intervention children by 9 min per day compared to the control group. Trends were observed for favourable changes in school day LPA, PA, MVPA, achieving 30 min school day MVPA, and CRF, however these did not reach significance.
The AS:Sk intervention demonstrates school-based PA components which are novel in their ability to target various time points in the school day with no financial costs to the school. The significant effects that the intervention had on ST are consistent with previous research. For example, the Finnish Schools on the Move study, which allowed schools to plan their own interventions with strategies such as longer recess periods, increased use of equipment during the school day, and staff training, reported decreased ST at 1.5 year follow-up in children similar in age to those in AS:Sk [73]. In contrast, the Active Living multi-component school-based intervention, which used techniques to target PA in school, before, and after school with active transport, and also during leisure time observed a general increase in ST at 12 months follow-up (2.2% more daily time spent in sedentary behaviour), which the authors speculated could have been due to the participants increase in age [25]. Given the short follow up period in the current study, it is difficult to establish whether the initial positive impact on ST would be sustained long term, inhibiting the anticipated age-related increase. Project timescale and subsequent funding precluded the utilisation of a longer-term intervention period and follow up evaluations.
A significant intervention effect on school day ST has implications for both public health policy and child health outcomes. Public health guidelines in both the UK and other countries recommend that overall sedentary time should be limited in children and young people [12,13,14]. Moreover, research has explored the relationship between ST and health indicators, subsequently highlighting the detrimental effects that ST can have on child health. For example, time spent being sedentary is positively associated with BMI z-score, and negatively associated with fitness in children and youth (aged 6–17 years) [74].
Results indicated a modest and non-significant increase in school day MVPA of 1.5 min. Sutherland and colleagues also reported modest increases in MVPA after the implementation of their multi-component school-based programme, ‘PA 4 Everyone’ [41]. Differences to control students were significant, with 3.9 more minutes of MVPA per day accumulated by intervention students [41]. Conversely, the ‘Active Living’ multicomponent school-based PA intervention had no significant effect on MVPA per day and saw a general reduction in PA [25].
The addition of even small amounts of MVPA to the school day may be beneficial to physical health, particularly when compared to interventions which see negative outcomes and also when the age-related decline in MVPA is considered [75]. However, the meaningfulness of potential benefits could be questioned. The addition of MVPA does predict positive effects with decreased adiposity, whilst the replacement of MVPA with any other movement behaviour predicts negative effects with higher adiposity and lower CRF [76,77]. However, these results are based on 15 min reallocations of time which is considerably more than the intervention effect on MVPA in the current study. Researchers and practitioners should focus on developing sustainable strategies for increasing MVPA participation during the school day given its significant importance for physical health. Understanding how interventions are implemented within schools from the perspective of teachers and students alike, may help in the development of successful school-based techniques. The process evaluation of interventions is advocated by the UK Medical Research Council (MRC) and can play a crucial role in understanding and learning from findings [78,79]. Despite this, implementation data are rarely reported in the literature and a lack of standardised definitions and measurements of implementation contributes to this [79]. A review into the barriers and facilitators to the implementation of PA policies in schools concluded that the body of literature surrounding this topic area from a theoretical perspective was scarce [80]. Implementation of PA in the classroom setting has received more coverage in the literature recently, including perspectives from teachers which has provided useful and important considerations for future interventions [81,82].
There were no significant intervention effects on whole weekday movement behaviours (including out of school hours). A previous systematic review concluded that school-based interventions had no effect on leisure time PA [83]. Whilst results were not significant, intervention effects on whole weekday PA were in the negative direction. This could suggest that children compensated for the increased PA opportunities they were provided with during the school day by decreasing their leisure time PA. This theory has also been suggested by previous interventions in which increases in school day MVPA did not translate into positive effects across the day [73]. An intervention which increased the number of compulsory PE lessons found that the percentage of time spent in MVPA during school was greater; however, the percentage of time spent in MVPA out of school was lower when both time periods were compared to normal schools [84]. Further PA compensation research has also suggested that for every additional 10 min spent in MVPA, children engaged in 5 min less the following day [85]. That being said, not all interventions report compensation effects, for example a review of school-based interventions found five in total which were effective at increasing overall PA [86]. AS! BC is one of these interventions that was effective at increasing overall PA [87]. Activities implemented across six action zones in this intervention included extracurricular and family and community, these zones in particular may have been the important factor which limited PA compensation outside of the school day [87].
The CSPAP approach to PA promotion comprises of five different components or points of intervention which includes PA before and after school [15]. Whilst attempts were made to target the out of school period with the PA homework component of the AS:Sk intervention it would appear that more substantial efforts are needed, for example with school-based extracurricular PA opportunities, rather than PA that requires children to engage with in the home environment. Many barriers to participation in out of school PA exist, including parental reported barriers such as safety concerns [88]. Screen time has also been reported by parents as a barrier, particularly as it is seen as the ‘norm’ for children to engage and therefore parents struggle to limit it [88,89]. Parents have reported that engagement in family-based PA intervention programmes would be the most effective way to increase their child’s PA [88]. The out of school time period for PA participation requires more attention, even from interventions which are primarily designed as school-based, in which the out of school barriers to PA participation and the desired family-based sessions should be considered.
The AS:Sk intervention had several strengths. Firstly, it was developed through prior formative research and was theoretically underpinned by conceptual behaviour change models [17,26,31]. This approach adheres to MRC guidelines for the development of complex interventions [90]. In addition, school staff were provided with the flexibility to implement the PA components when it best suited their class or school. This approach is most feasible in the “real-world” school setting in which unpredictable changes to timetables can happen, thus programme flexibility has previously been reported by teachers as a facilitator to implementation [19]. There was also no financial cost to the schools or the project. This would suggest that the intervention can be self-sustained by schools alone and, therefore, has potential for long-term implementation, although the teacher burden relating to planning and implementation should not be understated. The use of objectively measured PA to assess the intervention effect is an important strength of the study. Furthermore, the use of raw accelerations avoids the uncertainty of pre-processed data such as counts and the possibility that signal-filtering methods alter study results [91,92]. A limitation of the study is the modest sample size, which may have resulted in a lack of power in the statistical test outcomes, particularly the positive outcomes which did not reach statistical significance. The number of children who met the accelerometer wear-time criteria at both baseline and follow up measures also impacted on the final sample size. A further limitation was the timing of the follow up measures in both control and intervention schools. By necessity, measures were taken at an atypical school period, in the final few weeks before Christmas. It is in this period that school timetables are often disregarded and festive activities sometimes replace usual practice. Thus, the activity of children may not be representative of the rest of the school year. Intervention schools in particular may not have implemented the intervention in these final school weeks as they may have done so earlier in the school term. Furthermore, given that intervention implementation was sustained by school staff only, without any external support, it is likely that there were differences in implementation between participating schools. Gaining an accurate and objective record of implementation frequency across the eight-week period within each participating school may require daily researcher visits during the intervention period, which was not possible due to the time constraints of the research staff. Alternatively, teacher logs could be used, but these may be more subject to bias. Quantitative data to illustrate implementation frequency across the eight-week period was, therefore, not available, and it is acknowledged that differences in implementation frequency between schools likely impacted the results. The lack of a more long-term follow up measurement period was also a limitation. Given that follow up measurements were taken only eight weeks after implementation it is difficult to understand the sustainability of the intervention. The overall short intervention implementation period of eight weeks is also a weakness of the study, as interventions of longer duration have been shown to be more effective [86].
5. Conclusions
The AS:Sk multi-component school-based PA intervention had a significant positive effect on school day ST. There were no significant intervention effects on any of the other outcome measures. The small sample size of the current study was an important limitation within the study and may have contributed to the analyses lacking power. The school day period should continue to be a priority. Its importance for PA participation has previously been highlighted, and this study indicates that positive effects on ST in particular are achievable across the school day. Modifications to out-of-school components would be beneficial to avoid any compensation effects on PA participation. The AS:Sk intervention has potential to be scaled up to a full trial following modifications based on the results of this pilot study. Future research should focus on exploring ways in which MVPA participation can be increased during the school day. This may be with the development of appropriate school-based techniques or, conversely, focusing on how to improve the implementation of established techniques (such as the components of the current intervention) through process evaluation research.
Author Contributions
S.L.T., B.M., W.B.C., and S.J.F. conceived and designed the study. S.L.T. collected the data with the contribution of M.B.O. S.L.T. conducted the analyses with the contribution of S.J.F. S.L.T. wrote the manuscript. R.J.N., Z.R.K., M.B.O., B.M., W.B.C., and S.J.F. provided comments on the manuscript and read and approved the final version of the manuscript. S.J.F. secured the study funding.
Funding
This study was funded by West Lancashire Sport Partnership UK, West Lancashire Community Leisure UK, and Edge Hill University Ormskirk UK.
Acknowledgments
We would like to thank the participating schools, children and teachers for their participation, and Edge Hill University undergraduate students and West Lancashire Sport Partnership coaches for their assistance in data collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cooper, A.R.; Goodman, A.; Page, A.S.; Sherar, L.B.; Esliger, D.W.; van Sluijs, E.M.; Andersen, L.B.; Anderssen, S.; Cardon, G.; Davey, R.; et al. Objectively measured physical activity and sedentary time in youth: The International children’s accelerometry database (ICAD). Int. J. Behav. Nutr. Phys. Act. 2015, 12, 113. [Google Scholar] [CrossRef] [PubMed]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Poitras, V.J.; Gray, C.E.; Borghese, M.M.; Carson, V.; Chaput, J.P.; Janssen, I.; Katzmarzyk, P.T.; Pate, R.R.; Connor Gorber, S.; Kho, M.E.; et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41 (Suppl. 3), S197–S239. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.; Richards, J.; Hillman, C.; Faulkner, G.; Beauchamp, M.; Nilsson, M.; Kelly, P.; Smith, J.; Raine, L.; Biddle, S. Physical Activity for Cognitive and Mental Health in Youth: A Systematic Review of Mechanisms. Pediatrics 2016, 138, e20161642. [Google Scholar] [CrossRef] [PubMed]
- Reddon, H.; Meyre, D.; Cairney, J. Physical Activity and Global Self-worth in a Longitudinal Study of Children. Med. Sci. Sports Exerc. 2017, 49, 1606–1613. [Google Scholar] [CrossRef] [PubMed]
- Pearson, N.; Haycraft, E.; Johnston, J.P.; Atkin, A.J. Sedentary behaviour across the primary-secondary school transition: A systematic review. Prev. Med. 2017, 94, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.E.; Poitras, V.J.; Chaput, J.P.; Saunders, T.J.; Katzmarzyk, P.T.; Okely, A.D.; Connor Gorber, S. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Appl. Physiol. Nutr. Metab. 2016, 41, S240–S265. [Google Scholar] [CrossRef] [PubMed]
- Hesketh, K.R.; Lakshman, R.; van Sluijs, E.M.F. Barriers and facilitators to young children’s physical activity and sedentary behaviour: A systematic review and synthesis of qualitative literature. Obes. Rev. 2017, 18, 987–1017. [Google Scholar] [CrossRef] [PubMed]
- Burns, R.D.; Fu, Y.; Podlog, L.W. School-based physical activity interventions and physical activity enjoyment: A meta-analysis. Prev. Med. 2017, 103, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Childhood Obesity: A Plan for Action; HM Government: London, UK, 2016.
- Medicine, I.O. (Ed.) Educating the Student Body: Taking Physical Activity and Physical Education to School; The National Academies Press: Washington, DC, USA, 2013. [Google Scholar]
- Chief Medical Officer Department of Health. Start Active, Stay Active: A Report on Physical Activity from the Four Home Countries; Department of Health: London, UK, 2011.
- Tremblay, M.S.; Carson, V.; Chaput, J.P.; Connor Gorber, S.; Dinh, T.; Duggan, M.; Faulkner, G.; Gray, C.E.; Gruber, R.; Janson, K.; et al. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl. Physiol. Nutr. Metab. 2016, 41 (Suppl. 3), S311–S327. [Google Scholar] [CrossRef] [PubMed]
- Physical Activity Guidelines 2017; Health Council of the Netherlands: The Hague, The Netherlands, 2017.
- Erwin, H.; Beighle, A.; Carson, R.L.; Castelli, D.M. Comprehensive School-Based Physical Activity Promotion: A Review. Quest 2013, 65, 412–428. [Google Scholar] [CrossRef]
- Russ, L.B.; Webster, C.A.; Beets, M.W.; Phillips, D.S. Systematic Review and Meta-Analysis of Multi-Component Interventions Through Schools to Increase Physical Activity. J. Phys. Act. Health 2015, 12, 1436–1446. [Google Scholar] [CrossRef] [PubMed]
- Kenneth, R.M.; Daniel, B.; Allan, S.; Karen, G. An Ecological Perspective on Health Promotion Programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar]
- Naylor, P.-J.; Macdonald, H.M.; Reed, K.E.; McKay, H.A. Action Schools! BC: A Socioecological Approach to Modifying Chronic Disease Risk Factors in Elementary School Children. Prev. Chronic Dis. 2006, 3, A60. [Google Scholar] [PubMed]
- Naylor, P.-J.; Macdonald, H.M.; Zebedee, J.A.; Reed, K.E.; McKay, H.A. Lessons learned from Action Schools! BC—An ‘active school’ model to promote physical activity in elementary schools. J. Sci. Med. Sport 2006, 9, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Kellou, N.; Sandalinas, F.; Copin, N.; Simon, C. Prevention of unhealthy weight in children by promoting physical activity using a socio-ecological approach: What can we learn from intervention studies? Diabetes Metab. 2014, 40, 258–271. [Google Scholar] [CrossRef] [PubMed]
- Murillo Pardo, B.; García Bengoechea, E.; Generelo Lanaspa, E.; Bush, P.L.; Zaragoza Casterad, J.; Julián Clemente, J.A.; García González, L. Promising school-based strategies and intervention guidelines to increase physical activity of adolescents. Health Educ. Res. 2013, 28, 523–538. [Google Scholar] [CrossRef] [PubMed]
- Van Sluijs, E.M.F.; McMinn, A.M.; Griffin, S.J. Effectiveness of interventions to promote physical activity in children and adolescents: Systematic review of controlled trials. BMJ 2007, 335, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Owen, M.B.; Curry, W.B.; Kerner, C.; Newson, L.; Fairclough, S.J. The effectiveness of school-based physical activity interventions for adolescent girls: A systematic review and meta-analysis. Prev. Med. 2017, 105, 237–249. [Google Scholar] [CrossRef] [PubMed]
- Okely, A.D.; Lubans, D.R.; Morgan, P.J.; Cotton, W.; Peralta, L.; Miller, J.; Batterham, M.; Janssen, X. Promoting physical activity among adolescent girls: The Girls in Sport group randomized trial. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 81. [Google Scholar] [CrossRef] [PubMed]
- Van Kann, D.H.; Kremers, S.P.; de Vries, N.K.; de Vries, S.I.; Jansen, M.W. The effect of a school-centered multicomponent intervention on daily physical activity and sedentary behavior in primary school children: The Active Living study. Prev. Med. 2016, 89, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Beets, M.W.; Okely, A.; Weaver, R.G.; Webster, C.; Lubans, D.; Brusseau, T.; Carson, R.; Cliff, D.P. The theory of expanded, extended, and enhanced opportunities for youth physical activity promotion. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 120. [Google Scholar] [CrossRef] [PubMed]
- Collins, S. Seven Wards: A Focus on Skelmersdale; Lancashire, C.C., Ed.; Lancashire County Council: Preston, UK, 2015.
- Hemming, K.; Girling, A.J.; Sitch, A.J.; Marsh, J.; Lilford, R.J. Sample size calculations for cluster randomised controlled trials with a fixed number of clusters. BMC Med. Res. Methodol. 2011, 11, 102. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.L.; Curry, W.B.; Knowles, Z.R.; Noonan, R.J.; McGrane, B.; Fairclough, S.J. Predictors of Segmented School Day Physical Activity and Sedentary Time in Children from a Northwest England Low-Income Community. Int. J. Environ. Res. Public Health 2017, 14, E534. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.K.; Piaggio, G.; Elbourne, D.R.; Altman, D.G. Consort 2010 statement: Extension to cluster randomised trials. BMJ 2012, 345, e5661. [Google Scholar] [CrossRef] [PubMed]
- Welk, G.J. The Youth Physical Activity Promotion Model: A Conceptual Bridge Between Theory and Practice. Quest 1999, 51, 5–23. [Google Scholar] [CrossRef]
- Watson, A.; Timperio, A.; Brown, H.; Hesketh, K.D. A primary school active break programme (ACTI-BREAK): Study protocol for a pilot cluster randomised controlled trial. Trials 2017, 18, 433. [Google Scholar] [CrossRef] [PubMed]
- Carlson, J.A.; Engelberg, J.K.; Cain, K.L.; Conway, T.L.; Mignano, A.M.; Bonilla, E.A.; Geremia, C.; Sallis, J.F. Implementing classroom physical activity breaks: Associations with student physical activity and classroom behavior. Prev. Med. 2015, 81, 67–72. [Google Scholar] [CrossRef] [PubMed]
- McKay, H.; MacLean, L.; Petit, M.; MacKelvie-O’Brien, K.; Janssen, P.; Beck, T.; Khan, K. “Bounce at the Bell”: A novel program of short bouts of exercise improves proximal femur bone mass in early pubertal children. Br. J. Sports Med. 2005, 39, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, H.M.; Kontulainen, S.A.; Khan, K.M.; McKay, H.A. Is a school-based physical activity intervention effective for increasing tibial bone strength in boys and girls? J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2007, 22, 434–446. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, S.J.; McGrane, B.; Sanders, G.; Taylor, S.; Owen, M.; Curry, W. A non-equivalent group pilot trial of a school-based physical activity and fitness intervention for 10–11 year old english children: Born to move. BMC Public Health 2016, 16, 861. [Google Scholar] [CrossRef] [PubMed]
- Sacheck, J.M.; Wright, C.; Amin, S.; Anzman-Frasca, S.; Chomitz, V.; Chui, K.; Nelson, M.; Economos, C. The Fueling Learning Through Exercise (FLEX) Study: Short-term Findings On Sedentary Time In Lower-income Schoolchildren778 May 31 445 PM–500 PM. Med. Sci. Sports Exerc. 2017, 49, 200–201. [Google Scholar] [CrossRef]
- Lubans, D.R.; Lonsdale, C.; Cohen, K.; Eather, N.; Beauchamp, M.R.; Morgan, P.J.; Sylvester, B.D.; Smith, J.J. Framework for the design and delivery of organized physical activity sessions for children and adolescents: Rationale and description of the ‘SAAFE’ teaching principles. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 24. [Google Scholar] [CrossRef] [PubMed]
- Brazendale, K.; Chandler, J.L.; Beets, M.W.; Weaver, R.G.; Beighle, A.; Huberty, J.L.; Moore, J.B. Maximizing children’s physical activity using the LET US Play principles. Prev. Med. 2015, 76, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.R.; Morgan, P.J.; Weaver, K.; Callister, R.; Dewar, D.L.; Costigan, S.A.; Finn, T.L.; Smith, J.; Upton, L.; Plotnikoff, R.C. Rationale and study protocol for the supporting children’s outcomes using rewards, exercise and skills (SCORES) group randomized controlled trial: A physical activity and fundamental movement skills intervention for primary schools in low-income communities. BMC Public Health 2012, 12, 427. [Google Scholar]
- Sutherland, R.; Campbell, E.; Lubans, D.R.; Morgan, P.J.; Okely, A.D.; Nathan, N.; Wolfenden, L.; Wiese, J.; Gillham, K.; Hollis, J.; et al. ‘Physical Activity 4 Everyone’ school-based intervention to prevent decline in adolescent physical activity levels: 12 month (mid-intervention) report on a cluster randomised trial. Br. J. Sports Med. 2016, 50, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Vander Ploeg, K.A.; Maximova, K.; McGavock, J.; Davis, W.; Veugelers, P. Do school-based physical activity interventions increase or reduce inequalities in health? Soc. Sci. Med. 2014, 112, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, S.J.; Hackett, A.F.; Davies, I.G.; Gobbi, R.; Mackintosh, K.A.; Warburton, G.L.; Stratton, G.; van Sluijs, E.M.F.; Boddy, L.M. Promoting healthy weight in primary school children through physical activity and nutrition education: A pragmatic evaluation of the CHANGE! randomised intervention study. BMC Public Health 2013, 13, 626. [Google Scholar] [CrossRef] [PubMed]
- Kriemler, S.; Zahner, L.; Schindler, C.; Meyer, U.; Hartmann, T.; Hebestreit, H.; Brunner-La Rocca, H.P.; van Mechelen, W.; Puder, J.J. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: Cluster randomised controlled trial. BMJ 2010, 340, c785. [Google Scholar] [CrossRef] [PubMed]
- Van Hees, V.T.; Gorzelniak, L.; Dean Leon, E.C.; Eder, M.; Pias, M.; Taherian, S.; Ekelund, U.; Renstrom, F.; Franks, P.W.; Horsch, A.; et al. Separating movement and gravity components in an acceleration signal and implications for the assessment of human daily physical activity. PLoS ONE 2013, 8, e61691. [Google Scholar] [CrossRef] [PubMed]
- Van Hees, V.T.; Fang, Z.; Langford, J.; Assah, F.; Mohammad, A.; da Silva, I.C.M.; Trenell, M.I.; White, T.; Wareham, N.J.; Brage, S. Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: An evaluation on four continents. J. Appl. Physiol. 2014, 117, 738–744. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, S.J.; Noonan, R.; Rowlands, A.V.; Van Hees, V.; Knowles, Z.; Boddy, L.M. Wear Compliance and Activity in Children Wearing Wrist- and Hip-Mounted Accelerometers. Med. Sci. Sports Exerc. 2016, 48, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, A.V.; Cliff, D.P.; Fairclough, S.J.; Boddy, L.M.; Olds, T.S.; Parfitt, G.; Noonan, R.J.; Downs, S.J.; Knowles, Z.R.; Beets, M.W. Moving Forward with Backward Compatibility: Translating Wrist Accelerometer Data. Med. Sci. Sports Exerc. 2016, 48, 2142–2149. [Google Scholar] [CrossRef] [PubMed]
- Noonan, R.J.; Boddy, L.M.; Kim, Y.; Knowles, Z.R.; Fairclough, S.J. Comparison of children’s free-living physical activity derived from wrist and hip raw accelerations during the segmented week. J. Sports Sci. 2017, 35, 2067–2072. [Google Scholar] [CrossRef] [PubMed]
- Hildebrand, M.; van Hees, V.T.; Hansen, B.H.; Ekelund, U.L.F. Age Group Comparability of Raw Accelerometer Output from Wrist- and Hip-Worn Monitors. Med. Sci. Sports Exerc. 2014, 46, 1816–1824. [Google Scholar] [CrossRef] [PubMed]
- Hildebrand, M.; Hansen, B.H.; van Hees, V.T.; Ekelund, U. Evaluation of raw acceleration sedentary thresholds in children and adults. Scand. J. Med. Sci. Sports 2017, 27, 1814–1823. [Google Scholar] [CrossRef] [PubMed]
- Rich, C.; Geraci, M.; Griffiths, L.; Sera, F.; Dezateux, C.; Cortina-Borja, M. Quality Control Methods in Accelerometer Data Processing: Defining Minimum Wear Time. PLoS ONE 2013, 8, e67206. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Freeman, J.V.; Preece, M.A. Body mass index reference curves for the UK, 1990. Arch. Dis. Child. 1995, 73, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.K. Waist circumference to height ratio in children and adolescents. Clin. Pediatr. 2015, 54, 652–658. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.A.; McKay, H.A.; Macdonald, H.; Nettlefold, L.; Baxter-Jones, A.D.; Cameron, N.; Brasher, P.M. Enhancing a Somatic Maturity Prediction Model. Med. Sci. Sports Exerc. 2015, 47, 1755–1764. [Google Scholar] [CrossRef] [PubMed]
- Léger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Boddy, L.M.; Fairclough, S.J.; Atkinson, G.; Stratton, G. Changes in cardiorespiratory fitness in 9- to 10.9-year-old children: SportsLinx 1998–2010. Med. Sci. Sports Exerc. 2012, 44, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Motl, R.W.; Dishman, R.K.; Trost, S.G.; Saunders, R.P.; Dowda, M.; Felton, G.; Ward, D.S.; Pate, R.R. Factorial Validity and Invariance of Questionnaires Measuring Social-Cognitive Determinants of Physical Activity among Adolescent Girls. Prev. Med. 2000, 31, 584–594. [Google Scholar] [CrossRef] [PubMed]
- Motl, R.W.; Dishman, R.K.; Saunders, R.; Dowda, M.; Felton, G.; Pate, R.R. Measuring enjoyment of physical activity in adolescent girls. Am. J. Prev. Med. 2001, 21, 110–117. [Google Scholar] [CrossRef]
- The English Indicies of Deprivation 2015; Ministry of Housing, Communities & Local Government: Wetherby, UK, 2015.
- Rabesh, J.; Charlton, C.; Browne, W.J.; Healy, M.; Cameron, B. MLwiN Version 2.10.; Centre for Multilevel Modelling, University of Bristol: Bristol, UK, 2009. [Google Scholar]
- Twisk, J.W.R. Applied Multilevel Analysis; Cambridge University Press: Cambridge, UK, 2006. [Google Scholar]
- Zaqout, M.; Vyncke, K.; Moreno, L.A.; De Miguel-Etayo, P.; Lauria, F.; Molnar, D.; Lissner, L.; Hunsberger, M.; Veidebaum, T.; Tornaritis, M.; et al. Determinant factors of physical fitness in European children. Int. J. Public Health 2016, 61, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Baquet, G.; Ridgers, N.D.; Blaes, A.; Aucouturier, J.; Van Praagh, E.; Berthoin, S. Objectively assessed recess physical activity in girls and boys from high and low socioeconomic backgrounds. BMC Public Health 2014, 14, 192. [Google Scholar] [CrossRef] [PubMed]
- Borraccino, A.; Lemma, P.; Iannotti, R.J.; Zambon, A.; Dalmasso, P.; Lazzeri, G.; Giacchi, M.; Cavallo, F. Socioeconomic effects on meeting physical activity guidelines: Comparisons among 32 countries. Med. Sci. Sports Exerc. 2009, 41, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Richmond, R.C.; Davey Smith, G.; Ness, A.R.; den Hoed, M.; McMahon, G.; Timpson, N.J. Assessing Causality in the Association between Child Adiposity and Physical Activity Levels: A Mendelian Randomization Analysis. PLoS Med. 2014, 11, e1001618. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.; Mota, J.; Okely, A.D.; Pratt, M.; Moreira, C.; Coelho-e-Silva, M.J.; Vale, S.; Sardinha, L.B. The independent associations of sedentary behaviour and physical activity on cardiorespiratory fitness. Br. J. Sports Med. 2014, 48, 1508–1512. [Google Scholar] [CrossRef] [PubMed]
- Grund, A.; Dilba, B.; Forberger, K.; Krause, H.; Siewers, M.; Rieckert, H.; Müller, M.J. Relationships between physical activity, physical fitness, muscle strength and nutritional state in 5- to 11-year-old children. Eur. J. Appl. Physiol. 2000, 82, 425–438. [Google Scholar] [CrossRef] [PubMed]
- Silva, G.; Andersen, L.B.; Aires, L.; Mota, J.; Oliveira, J.; Ribeiro, J.C. Associations between sports participation, levels of moderate to vigorous physical activity and cardiorespiratory fitness in childrenand adolescents. J. Sports Sci. 2013, 31, 1359–1367. [Google Scholar] [CrossRef] [PubMed]
- Mann, K.D.; Howe, L.D.; Basterfield, L.; Parkinson, K.N.; Pearce, M.S.; Reilly, J.K.; Adamson, A.J.; Reilly, J.J.; Janssen, X. Longitudinal study of the associations between change in sedentary behavior and change in adiposity during childhood and adolescence: Gateshead Millennium Study. Int. J. Obes. 2017, 41, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, H.J.; Standage, M.; Gillison, F.B.; Cumming, S.P.; Katzmarzyk, P.T. Correlates of intensity-specific physical activity in children aged 9–11 years: A multilevel analysis of UK data from the International Study of Childhood Obesity, Lifestyle and the Environment. BMJ Open 2018, 8, e018373. [Google Scholar] [CrossRef] [PubMed]
- Haapala, H.L.; Hirvensalo, M.H.; Kulmala, J.; Hakonen, H.; Kankaanpää, A.; Laine, K.; Laakso, L.; Tammelin, T.H. Changes in physical activity and sedentary time in the Finnish Schools on the Move program: A quasi-experimental study. Scand. J. Med. Sci. Sports 2017, 27, 1442–1453. [Google Scholar] [CrossRef] [PubMed]
- Carson, V.; Tremblay, M.S.; Chaput, J.P.; Chastin, S.F. Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl. Physiol. Nutr. Metab. 2016, 41 (Suppl. 3), S294–S302. [Google Scholar] [CrossRef] [PubMed]
- Dumith, S.C.; Gigante, D.P.; Domingues, M.R.; Kohl, H.W. Physical activity change during adolescence: A systematic review and a pooled analysis. Int. J. Epidemiol. 2011, 40, 685–698. [Google Scholar] [CrossRef] [PubMed]
- Dumuid, D.; Stanford, T.E.; Pedišić, Ž.; Maher, C.; Lewis, L.K.; Martín-Fernández, J.-A.; Katzmarzyk, P.T.; Chaput, J.-P.; Fogelholm, M.; Standage, M.; et al. Adiposity and the isotemporal substitution of physical activity, sedentary time and sleep among school-aged children: A compositional data analysis approach. BMC Public Health 2018, 18, 311. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, S.J.; Dumuid, D.; Taylor, S.; Curry, W.; McGrane, B.; Stratton, G.; Maher, C.; Olds, T. Fitness, fatness and the reallocation of time between children’s daily movement behaviours: An analysis of compositional data. Int. J. Behav. Nutr.Phys. Act. 2017, 14, 64. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef] [PubMed]
- Naylor, P.J.; Nettlefold, L.; Race, D.; Hoy, C.; Ashe, M.C.; Wharf Higgins, J.; McKay, H.A. Implementation of school based physical activity interventions: A systematic review. Prev. Med. 2015, 72, 95–115. [Google Scholar] [CrossRef] [PubMed]
- Nathan, N.; Elton, B.; Babic, M.; McCarthy, N.; Sutherland, R.; Presseau, J.; Seward, K.; Hodder, R.; Booth, D.; Yoong, S.L.; et al. Barriers and facilitators to the implementation of physical activity policies in schools: A systematic review. Prev. Med. 2018, 107, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Routen, A.C.; Johnston, J.P.; Glazebrook, C.; Sherar, L.B. Teacher perceptions on the delivery and implementation of movement integration strategies: The CLASS PAL (Physically Active Learning) Programme. Int. J. Educ. Res. 2018, 88, 48–59. [Google Scholar] [CrossRef]
- Dyrstad, S.M.; Kvalø, S.E.; Alstveit, M.; Skage, I. Physically active academic lessons: Acceptance, barriers and facilitators for implementation. BMC Public Health 2018, 18, 322. [Google Scholar] [CrossRef] [PubMed]
- Dobbins, M.; De Corby, K.; Robeson, P.; Husson, H.; Tirilis, D. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6–18. Cochrane Database Syst. Rev. 2009, 28, CD007651. [Google Scholar]
- Møller, N.C.; Tarp, J.; Kamelarczyk, E.F.; Brønd, J.C.; Klakk, H.; Wedderkopp, N. Do extra compulsory physical education lessons mean more physically active children—Findings from the childhood health, activity, and motor performance school study Denmark (The CHAMPS-study DK). Int. J. Behav. Nutr. Phys. Act. 2014, 11, 121. [Google Scholar] [CrossRef] [PubMed]
- Ridgers, N.D.; Timperio, A.; Cerin, E.; Salmon, J.O. Compensation of Physical Activity and Sedentary Time in Primary School Children. Med. Sci. Sports Exerc. 2014, 46, 1564–1569. [Google Scholar] [CrossRef] [PubMed]
- Kriemler, S.; Meyer, U.; Martin, E.; Sluijs, E.M.; Andersen, L.B.; Martin, B.W. Effect of school-based interventions on physical activity and fitness in children and adolescents: A review of reviews and systematic update. Br. J. Sports Med. 2011, 45, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Naylor, P.J.; Macdonald, H.M.; Warburton, D.E.R.; Reed, K.E.; McKay, H.A. An active school model to promote physical activity in elementary schools: Action schools! BC. Br. J. Sports Med. 2008, 42, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Noonan, R.J.; Boddy, L.M.; Fairclough, S.J.; Knowles, Z.R. Parental perceptions on childrens out-of-school physical activity and family-based physical activity. Early Child Dev. Care 2017, 187, 1909–1924. [Google Scholar] [CrossRef]
- Solomon-Moore, E.; Matthews, J.; Reid, T.; Toumpakari, Z.; Sebire, S.J.; Thompson, J.L.; Lawlor, D.A.; Jago, R. Examining the challenges posed to parents by the contemporary screen environments of children: A qualitative investigation. BMC Pediatr. 2018, 18, 129. [Google Scholar] [CrossRef] [PubMed]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.; Bowles, H.R.; Troiano, R.; Haskell, W. Assessment of physical activity using wearable monitors: Recommendations for monitor calibration and use in the field. Med. Sci. Sports Exerc. 2012, 44 (Suppl. 1), S1–S4. [Google Scholar] [CrossRef] [PubMed]
- Peach, D.; Van Hoomissen, J.; Callender, H.L. Exploring the ActiLife((R)) filtration algorithm: Converting raw acceleration data to counts. Physiol. Meas. 2014, 35, 2359–2367. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).