Antinociceptive Efficacy of 15-Deoxy-Δ12,14-Prostaglandin J2 Therapy in Response to Experimentally Induced Temporomandibular Joint Arthritis: A Systematic Review of Studies in Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Registration in the International Database of Prospectively Registered Systematic Reviews (PROSPERO)
2.3. Inclusion and Exclusion Criteria
2.4. Literature Search
2.5. Risk of Bias Assessment
3. Results
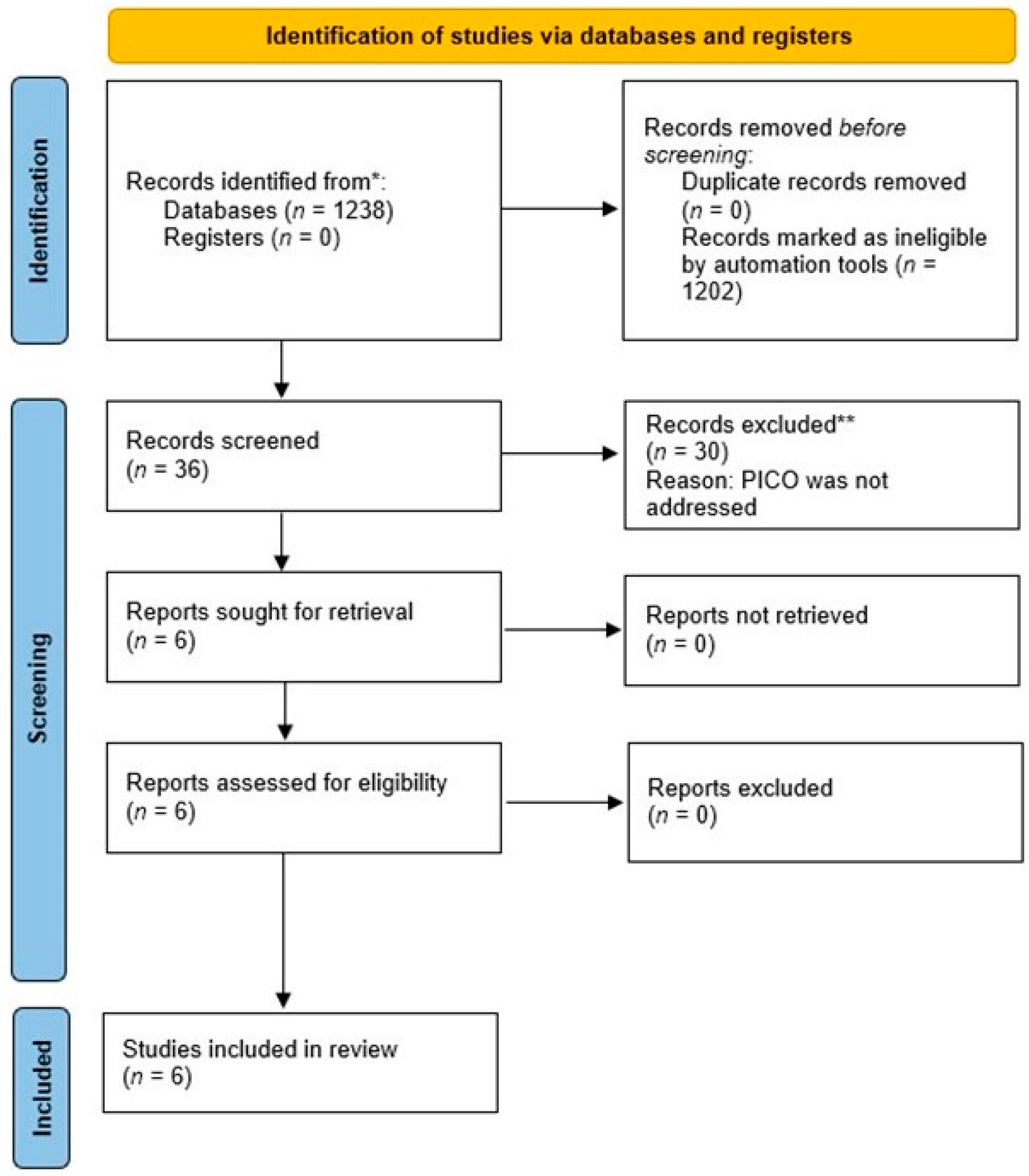
3.1. Literature Search
3.2. General Characteristics of Included Studies
3.3. 15-Deoxy-Δ12,14-Prostaglandin J2 Therapy
3.4. Other Parameters Assessed
3.5. Outcomes
3.5.1. Antinociceptive Effects of 15-Deoxy-Δ12,14-Prostaglandin J2
3.5.2. Effect of 15-Deoxy-Δ12,14-Prostaglandin J2 Leukocyte Migration, Plasma Extravasation, and Cytokine/Chemokine Profile
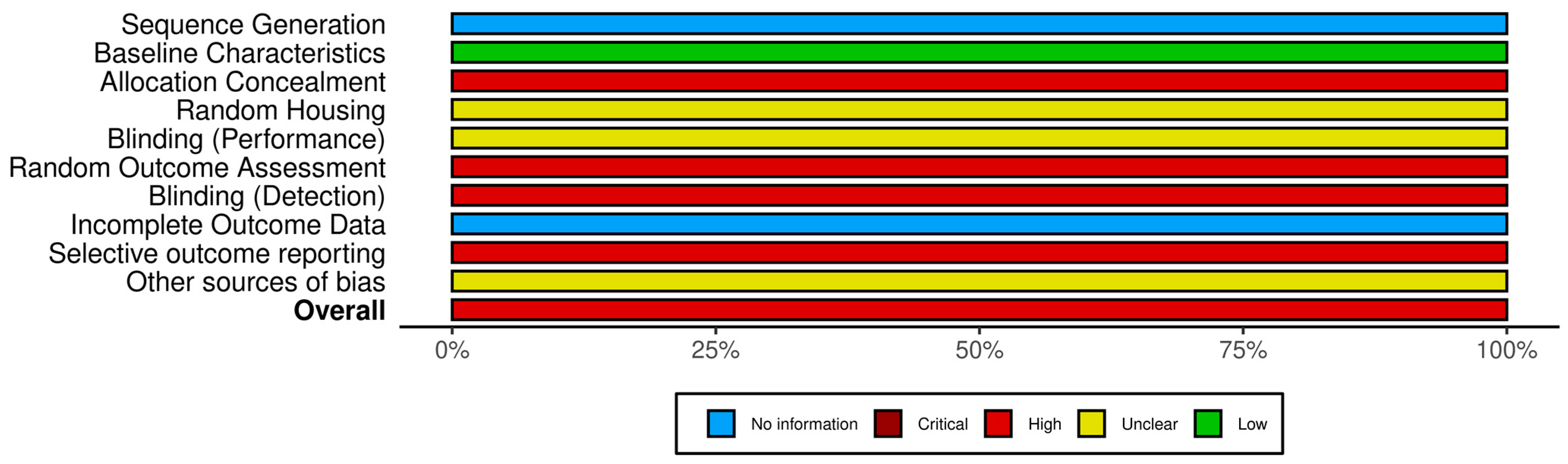
3.5.3. Risk of Bias Assessment and GRADE Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Loeser, J.D.; Treede, R.D. The Kyoto protocol of IASP Basic Pain Terminology. Pain 2008, 137, 473–477. [Google Scholar] [CrossRef]
- Kyrkanides, S.; Tallents, R.H.; Macher, D.J.; Olschowka, J.A.; Stevens, S.Y. Temporomandibular joint nociception: Effects of capsaicin on substance P-like immunoreactivity in the rabbit brain stem. J. Orofac. Pain 2002, 16, 229–236. [Google Scholar]
- Takeuchi, Y.; Zeredo, J.L.; Fujiyama, R.; Amagasa, T.; Toda, K. Effects of experimentally induced inflammation on temporomandibular joint nociceptors in rats. Neurosci. Lett. 2004, 354, 172–174. [Google Scholar] [CrossRef]
- Murphy, M.K.; MacBarb, R.F.; Wong, M.E.; Athanasiou, K.A. Temporomandibular disorders: A review of etiology, clinical management, and tissue engineering strategies. Int. J. Oral. Maxillofac. Implant. 2013, 28, e393–e414. [Google Scholar] [CrossRef]
- Scrivani, S.J.; Keith, D.A.; Kaban, L.B. Temporomandibular disorders. N. Engl. J. Med. 2008, 359, 2693–2705. [Google Scholar] [CrossRef]
- Manfredini, D.; Thomas, D.C.; Lobbezoo, F. Temporomandibular Disorders Within the Context of Sleep Disorders. Dent. Clin. N. Am. 2023, 67, 323–334. [Google Scholar] [CrossRef]
- Ananias, F.E.F.; Dos Santos, V.A.B.; Groppo, F.C.; Henriques, G.E.P.; Toledo, J.R.; da Silva Pais, R.; Figueroba, S.R. Inflammatory and degenerative effects of induced osteoarthritis/rheumatoid arthritis models on temporomandibular joint of rats. Arch. Oral. Biol. 2023, 150, 105693. [Google Scholar] [CrossRef]
- Sperry, M.M.; Ita, M.E.; Kartha, S.; Zhang, S.; Yu, Y.H.; Winkelstein, B. The Interface of Mechanics and Nociception in Joint Pathophysiology: Insights From the Facet and Temporomandibular Joints. J. Biomech. Eng. 2017, 139, 0210031–02100313. [Google Scholar] [CrossRef]
- Andre, A.; Kang, J.; Dym, H. Pharmacologic Treatment for Temporomandibular and Temporomandibular Joint Disorders. Oral. Maxillofac. Surg. Clin. N. Am. 2022, 34, 49–59. [Google Scholar] [CrossRef]
- Tăut, M.; Buduru, S.D.; Tălmăceanu, D.; Ban, A.; Roman, R.; Leucuța, D.; Barbur, I.; Ilea, A. Occlusal Splint Therapy Combined with Cranio-Temporomandibular Kinesiotherapy in Patients with Temporomandibular Disorders-A CBCT Study. Life 2022, 12, 2143. [Google Scholar] [CrossRef]
- Asquini, G.; Pitance, L.; Michelotti, A.; Falla, D. Effectiveness of manual therapy applied to craniomandibular structures in temporomandibular disorders: A systematic review. J. Oral. Rehabil. 2022, 49, 442–455. [Google Scholar] [CrossRef]
- Shroff, B. Malocclusion as a Cause for Temporomandibular Disorders and Orthodontics as a Treatment. Oral. Maxillofac. Surg. Clin. N. Am. 2018, 30, 299–302. [Google Scholar] [CrossRef]
- Silva Quinteiro, M.; Henrique Napimoga, M.; Gomes Macedo, C.; Furtado Freitas, F.; Balassini Abdalla, H.; Bonfante, R.; Trindade Clemente-Napimoga, J. 15-deoxy-Δ12,14-prostaglandin J2 reduces albumin-induced arthritis in temporomandibular joint of rats. Eur. J. Pharmacol. 2014, 740, 58–65. [Google Scholar] [CrossRef]
- Abdalla, H.B.; Napimoga, M.H.; Macedo, C.G.; Bonfante, R.; De Araujo, D.R.; de Mello, N.F.S.; Carvalho, L.B.; Fraceto, L.F.; Clemente-Napimoga, J.T. Poloxamer micellar system for intra-articular injection of 15-deoxy-(Δ12,14)-prostaglandin J(2) with improved bioavailability and anti-inflammatory properties in the temporomandibular joint of rats. Int. J. Pharm. 2020, 583, 119383. [Google Scholar] [CrossRef]
- Macedo, C.G.; Napimoga, M.H.; Rocha-Neto, L.M.; Abdalla, H.B.; Clemente-Napimoga, J.T. The role of endogenous opioid peptides in the antinociceptive effect of 15-deoxy(Δ12,14)-prostaglandin J2 in the temporomandibular joint. Prostaglandins Leukot. Essent. Fatty Acids 2016, 110, 27–34. [Google Scholar] [CrossRef]
- Pena-dos-Santos, D.R.; Severino, F.P.; Pereira, S.A.; Rodrigues, D.B.; Cunha, F.Q.; Vieira, S.M.; Napimoga, M.H.; Clemente-Napimoga, J.T. Activation of peripheral kappa/delta opioid receptors mediates 15-deoxy-(Delta12,14)-prostaglandin J2 induced-antinociception in rat temporomandibular joint. Neuroscience 2009, 163, 1211–1219. [Google Scholar] [CrossRef]
- Quinteiro, M.S.; Napimoga, M.H.; Mesquita, K.P.; Clemente-Napimoga, J.T. The indirect antinociceptive mechanism of 15d-PGJ2 on rheumatoid arthritis-induced TMJ inflammatory pain in rats. Eur. J. Pain 2012, 16, 1106–1115. [Google Scholar] [CrossRef]
- Clemente-Napimoga, J.T.; Moreira, J.A.; Grillo, R.; de Melo, N.F.; Fraceto, L.F.; Napimoga, M.H. 15d-PGJ2-loaded in nanocapsules enhance the antinociceptive properties into rat temporomandibular hypernociception. Life Sci. 2012, 90, 944–949. [Google Scholar] [CrossRef]
- Carvalho, F.R.; Barros, R.Q.; Gonçalves, A.S.; Muragaki, S.P.; Pedroni, A.C.F.; Oliveira, K.; Freitas, P.M. Photobiomodulation Therapy on the Palliative Care of Temporomandibular Disorder and Orofacial/Cervical Skull Pain: Preliminary Results from a Randomized Controlled Clinical Trial. Healthcare 2023, 11, 2574. [Google Scholar] [CrossRef]
- Martenot, A.; Devoti, J.F.; Pons, M.; Meyer, C.; Brumpt, E.; Louvrier, A.; Bertin, E. Persistent myogenic temporomandibular disorders: Are navigation-guided botulinum toxin-A injections into the lateral pterygoid muscles effective? J. Stomatol. Oral. Maxillofac. Surg. 2023, 101715. [Google Scholar] [CrossRef]
- White, H.D.; Brown, L.A.; Gyurik, R.J.; Manganiello, P.D.; Robinson, T.D.; Hallock, L.S.; Lewis, L.D.; Yeo, K.T. Treatment of pain in fibromyalgia patients with testosterone gel: Pharmacokinetics and clinical response. Int. Immunopharmacol. 2015, 27, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Suh, J.Y.; Kim, D.H.; Na, H.K.; Surh, Y.J. 15-Deoxy-Δ(12,14)-prostaglandin J(2) Induces Epithelial-to-mesenchymal Transition in Human Breast Cancer Cells and Promotes Fibroblast Activation. J. Cancer Prev. 2020, 25, 152–163. [Google Scholar] [CrossRef] [PubMed]
- Surh, Y.J.; Na, H.K.; Park, J.M.; Lee, H.N.; Kim, W.; Yoon, I.S.; Kim, D.D. 15-Deoxy-Δ¹²,¹⁴-prostaglandin J₂, an electrophilic lipid mediator of anti-inflammatory and pro-resolving signaling. Biochem. Pharmacol. 2011, 82, 1335–1351. [Google Scholar] [CrossRef] [PubMed]
- de Jong, E.; Winkel, P.; Poelstra, K.; Prakash, J. Anticancer effects of 15d-prostaglandin-J2 in wild-type and doxorubicin-resistant ovarian cancer cells: Novel actions on SIRT1 and HDAC. PLoS ONE 2011, 6, e25192. [Google Scholar] [CrossRef] [PubMed]
- Shan, Z.Z.; Masuko-Hongo, K.; Dai, S.M.; Nakamura, H.; Kato, T.; Nishioka, K. A potential role of 15-deoxy-delta(12,14)-prostaglandin J2 for induction of human articular chondrocyte apoptosis in arthritis. J. Biol. Chem. 2004, 279, 37939–37950. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s risk of bias tool for animal studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef]
- Zhang, X.; Hartmann, P. How to calculate sample size in animal and human studies. Front. Med. 2023, 10, 1215927. [Google Scholar] [CrossRef]
- Faber, J.; Fonseca, L.M. How sample size influences research outcomes. Dental Press J. Orthod. 2014, 19, 27–29. [Google Scholar] [CrossRef]
- Kapadia, R.; Yi, J.H.; Vemuganti, R. Mechanisms of anti-inflammatory and neuroprotective actions of PPAR-gamma agonists. Front. Biosci. A J. Virtual Libr. 2008, 13, 1813–1826. [Google Scholar] [CrossRef]
- Slade, G.D.; Conrad, M.S.; Diatchenko, L.; Rashid, N.U.; Zhong, S.; Smith, S.; Rhodes, J.; Medvedev, A.; Makarov, S.; Maixner, W.; et al. Cytokine biomarkers and chronic pain: Association of genes, transcription, and circulating proteins with temporomandibular disorders and widespread palpation tenderness. Pain 2011, 152, 2802–2812. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Bao, M.; Hou, C.; Wang, Y.; Zheng, L.; Peng, Y. The Role of TNF-α in the Pathogenesis of Temporomandibular Disorders. Biol. Pharm. Bull. 2021, 44, 1801–1809. [Google Scholar] [CrossRef] [PubMed]
- Grace, P.M.; Hutchinson, M.R.; Maier, S.F.; Watkins, L.R. Pathological pain and the neuroimmune interface. Nat. Rev. Immunol. 2014, 14, 217–231. [Google Scholar] [CrossRef] [PubMed]
- Straus, D.S.; Glass, C.K. Cyclopentenone prostaglandins: New insights on biological activities and cellular targets. Med. Res. Rev. 2001, 21, 185–210. [Google Scholar] [CrossRef]
- Maggi, L.B., Jr.; Sadeghi, H.; Weigand, C.; Scarim, A.L.; Heitmeier, M.R.; Corbett, J.A. Anti-inflammatory actions of 15-deoxy-delta 12,14-prostaglandin J2 and troglitazone: Evidence for heat shock-dependent and -independent inhibition of cytokine-induced inducible nitric oxide synthase expression. Diabetes 2000, 49, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Shane Anderson, A.; Loeser, R.F. Why is osteoarthritis an age-related disease? Best Pract. Res. Clin. Rheumatol. 2010, 24, 15–26. [Google Scholar] [CrossRef]
- Paulino, M.R.; Moreira, V.G.; Lemos, G.A.; Silva, P.; Bonan, P.R.F.; Batista, A.U.D. Prevalence of signs and symptoms of temporomandibular disorders in college preparatory students: Associations with emotional factors, parafunctional habits, and impact on quality of life. Cien Saude Colet. 2018, 23, 173–186. [Google Scholar] [CrossRef]
- Manfredini, D.; Piccotti, F.; Ferronato, G.; Guarda-Nardini, L. Age peaks of different RDC/TMD diagnoses in a patient population. J. Dent. 2010, 38, 392–399. [Google Scholar] [CrossRef]
- Lesnak, J.B.; Inoue, S.; Lima, L.; Rasmussen, L.; Sluka, K.A. Testosterone protects against the development of widespread muscle pain in mice. Pain 2020, 161, 2898–2908. [Google Scholar] [CrossRef]
| Parameters | Description |
|---|---|
| Patients/Subjects (P) | Patients/subjects with TMJ arthritis |
| Intervention (I) | Management of TMJ arthritis with 15d-PGJ2 therapy |
| Control (C) | Management of TMJ arthritis with placebo or no therapy |
| Outcome (O) | Change in TMJ nociception |
| Data Source | Database | PubMed | Scopus | Web of Science | Google Scholar |
| Vendor | NLM | Elsevier | Clarivate | ||
| Date searched | 5 June 2023 | 5 June 2023 | 5 June 2023 | 5 June 2023 | |
| Database Update | - | - | - | - | |
| Limiters | English only? | No | No | No | No |
| Time period searched | No restrictions | No restrictions | No restrictions | No restrictions | |
| Publication type | - | - | - | - | |
| Other | Not applicable | Not applicable | Not applicable | Not applicable | |
| Key words | Items found | 78 | 454 | 404 | 302 |
| Internal duplicates (within one database) | 0 | 0 | 0 | 0 | |
| External duplicates (between databases) | 0 | 0 | 0 | 0 | |
| Name of saved search | |||||
| 1 | Inflammation OR Nociception OR Pain AND | Inflammation OR Nociception OR Pain AND | Inflammation OR Nociception OR Pain AND | Inflammation OR Nociception OR Pain AND | |
| 2 | Prostaglandin J2 AND | Prostaglandin J2 AND | Prostaglandin J2 AND | Prostaglandin J2 AND | |
| 3 | Temporomandibular joint OR Temporomandibular disorders | Temporomandibular joint OR Temporomandibular disorders | Temporomandibular joint OR Temporomandibular disorders | Temporomandibular joint OR Temporomandibular disorders | |
| Authors et al. | Subjects (n) | Gender | Age | Weight Range | Study Groups | SSE |
|---|---|---|---|---|---|---|
| Silva Quinteiro et al. [13] | Wistar rats (NR) | Male | NR | 150–250 g | Test group: IA injection of 15d-PgJ2 Control group: IA vehicle injection | NR |
| Abdalla et al. [14] | Wistar rats (12) | Male | NR | 200–250 g | Test group: IA injection of a PL-407 micellar system of 15d-PgJ2 Control group: IA injection of 15d-PgJ2 without PL-407 micellar system | NR |
| Macedo et al. [15] | Male Wistar Rat (NR) | Male | 6–8 weeks old | 200–300 g | Test group: Intra-TMJ injection of 15d-PgJ2 Control group: IA 1.5% formalin injection | NR |
| Pena-dos-Santos et al. [16] | Wistar Rats (NR) | Male | NR | 150–250 g | Test group: IA injection of 15d-PgJ2 Control: IA vehicle injection | NR |
| Quinteiro et al. [17] | Wistar Rats (NR) | Male | NR | 150–250 g | Test group: Intra-TMJ injection of 15d-PgJ2 Control group: IA vehicle injection | NR |
| Clemente-Napimoga et al. [18] | Wistar Rats (NR) | Male | NR | 150–250 g | Test group: Intra-TMJ injection of 15d-PgJ2 Control group: IA vehicle injection | NR |
| Authors et al. | Induction of Arthritis | Mode of PgJ2 and Vehicle Administration | Concentration of PgJ2 | Control Group Injected with: | Other Parameters Assessed | Follow-Up |
|---|---|---|---|---|---|---|
| Silva Quinteiro et al. [13] | AIA (10 μg/TMJ) | IA injection | 100 ng/TMJ | mBSA |
| 48 h |
| Abdalla et al. [14] | 30 µL/TMJ Formalin | IA injection | 0.3 and 1.3 ng/TMJ | Vehicle Control Group |
| 14 days |
| Macedo et al. [15] | 1.5% Formalin Injection | IA injection | 100 ng (15 µL/TMJ) | 0.9% saline (45 µL/TMJ) |
| 45 min |
| Pena-dos-Santos et al. [16] | 1.5% Formalin | IA injection | 1, 10, 100 ng (15 µ/TMJ) | 0.9% saline |
| 45 min |
| Quinteiro et al. [17] | 0.5% Formalin | IA injection | 30, 100 and 300 ng/TMJ 15 µ/TMJ | PBS |
| 45 min |
| Clemente-Napimoga et al. [18] | 1.5% Formalin | Intra-TMJ 15d-PgJ2 Nanocapsules | 0.01, 0.1, 1 ng (15 µL/TMJ) | Saline nanocapsules (15 µ/TMJ) |
| 45 min |
| Authors et al. | Effects of 15d-PGJ2 on TMJ Nociception and Protein Expression in Peri-Auricular Tissues | Conclusion | ||||
|---|---|---|---|---|---|---|
| Experimental Nociception | LM and PE | Release of Proinflammatory Cytokines | CD55 Expression | Opioid Receptors | ||
| Silva Quinteiro et al. [13] | Inhibited | Inhibited | Reduced | NR | NR | 15d-PgJ2 administration inhibits TMJ nociception |
| Abdalla et al. [14] | Inhibited | Inhibited | Reduced | Increased | NR | 15d-PgJ2 administration inhibits TMJ nociception |
| Macedo et al. [15] | Inhibited | NR | NR | NR | Activated * | 15d-PgJ2 administration inhibits TMJ nociception |
| Pena-dos-Santos et al. [16] | Inhibited | Inhibited | NR | NR | Activated * | 15d-PgJ2 administration inhibits TMJ nociception |
| Quinteiro et al. [17] | Inhibited | Inhibited | Reduced | NR | NR | 15d-PgJ2 administration inhibits TMJ nociception |
| Clemente-Napimoga et al. [18] | Inhibited | NR | Reduced | NR | NR | 15d-PgJ2 administration inhibits TMJ nociception |
| Domains | Silva Quinteiro et al. [13] | Abdalla et al. [14] | Macedo et al. [15] | Pena-dos-Santos et al. [16] | Quinteiro et al. [17] | Clemente-Napimoga et al. [18] |
|---|---|---|---|---|---|---|
| Sequence Generation | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Baseline Characteristics | Yes | Yes | Yes | Yes | Yes | Yes |
| Allocation Concealment | No | No | No | No | No | No |
| Random Housing | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Blinding (Performance) | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Random Outcome Assessment | No | No | No | No | No | No |
| Blinding (Detection) | No | No | No | No | No | No |
| Incomplete Outcome Data | Yes | Yes | Yes | Yes | Yes | Yes |
| Selective Outcome Reporting | Yes | Yes | Yes | Yes | Yes | Yes |
| Other Sources of Bias | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Overall Bias Rating | High | High | High | High | High | High |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hart, F.; Michelogiannakis, D.; Rossouw, P.E.; Javed, F. Antinociceptive Efficacy of 15-Deoxy-Δ12,14-Prostaglandin J2 Therapy in Response to Experimentally Induced Temporomandibular Joint Arthritis: A Systematic Review of Studies in Rats. Prosthesis 2024, 6, 63-73. https://doi.org/10.3390/prosthesis6010005
Hart F, Michelogiannakis D, Rossouw PE, Javed F. Antinociceptive Efficacy of 15-Deoxy-Δ12,14-Prostaglandin J2 Therapy in Response to Experimentally Induced Temporomandibular Joint Arthritis: A Systematic Review of Studies in Rats. Prosthesis. 2024; 6(1):63-73. https://doi.org/10.3390/prosthesis6010005
Chicago/Turabian StyleHart, Fraser, Dimitrios Michelogiannakis, P. Emile Rossouw, and Fawad Javed. 2024. "Antinociceptive Efficacy of 15-Deoxy-Δ12,14-Prostaglandin J2 Therapy in Response to Experimentally Induced Temporomandibular Joint Arthritis: A Systematic Review of Studies in Rats" Prosthesis 6, no. 1: 63-73. https://doi.org/10.3390/prosthesis6010005






